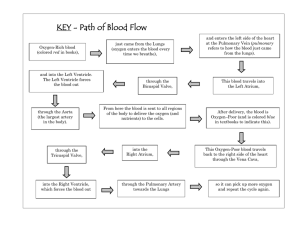
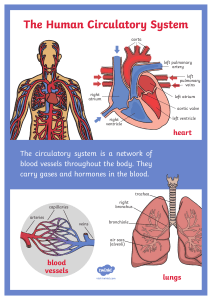
Patho II: 10/11/21 Cardiac Pathophysiology: Heart: - - Heart Structure: - - - Blood Flow through the Heart: - Size of a fist o Base: upper portion o Apex: pointed end Acute Coronary Syndrome (ACS) o Due to ischemia (low oxygen to cardiac muscle) Myocardial Infarction (MI) o Prolonged ischemia leading to cell death Tissue Layers: o Epicardium – outer layer o Myocardium – cardiac muscle o Endocardium – inner lining of heart Coronary circulation: o Right coronary artery: supplies right side of heart (right atrium and ventricle, SA and AV nodes) o Left coronary artery: supplies blood to the left side of heart LAD (left anterior descending): branches from left coronary; supplies blood to front of left side of heart Four chambers: o Atria: receiving chambers Right atrium: receives blood from superior/ inferior vena cava and coronary sinus >> tricuspid valve Left atrium: receives blood from pulmonary veins >>> mitral valve (bicuspid valve) o Ventricles: pumping chambers (pump blood outside the heart to lungs or systemic circulation) Right ventricle: pumps blood to lungs Left ventricle: pumps blood to body Ventricular walls thicker than atrial walls DEOXYGENATED blood enters from systemic circulation to RIGHT side of heart from SUPERIOR/ INFERIOR VENA CAVA Blood empties into RIGHT ATRIUM RIGHT ATRIUM pumps blood through TRICUSPID VALVE to RIGHT VENTRICLE RIGHT VENTRICLE pumps blood through PULMONIC VALVE to PULMONARY ARTERIES PULMONARY ARTERIES carry blood to lungs for gas exchange OXYGENATED blood returns from lungs to heart through PULMONARY VEINS PULMONARY VEINS empty into LEFT ATRIUM LEFT ATRIUM pumps blood through MITRAL VALVE to LEFT VENTRICLE LEFT VENTRICLE pumps blood through AORTIC VALVE to AORTA AORTA carries blood to rest of body Circulation Cont.: - Cardiac Muscle Action Potential: - Two Circuits: o Pulmonary: low pressure; Right ventricle to Left atrium o Systemic: high pressure; Left ventricle to Right Atrium Systolic: contraction (SBP) Diastolic: relaxation (DBP) Phase 0: fast SODIUM channels open and increased potential from -90mV to 20mV Phase 1: PEAK, abrupt CLOSURE of fast SODIUM channels Phase 2: PLATEAU, slow SODIUM-CALCIUM channels Phase 3: REPOLARIZATION, K+ channels open Phase 4: RESTING POTENTIAL, Na+/ K+ PUMP Refractory Period: - Allows heart to relax w/o being reactivated Allows heart to fill with blood Protects against fatal arrhythmias Absolute Refractory Period: cells cannot be restimulated; phases 0-2 (part of 3) Dysrhythmias (Arrhythmias): - Disruption in electrical signal o Supraventricular: SA node, AV node, atria o Ventricular: Bundle of His, Purkinje fibers, ventricles o Tachyarrhythmia: rapid heartbeat that may be regular or irregular, but is out of proportion to age and level of exertion or activity o Bradyarrhythmia: slower-than-expected heart rate, generally beating fewer than 60 beats per minute Block o Most commonly at AV node Ectopic pacemaker o Outside normal conduction pathway PVC (premature ventricular contraction) – extra heartbeats that begin in one of your heart’s ventricles Symptoms: fluttering, skipped/ missed beats, pounding Causes: heart disease or bodily changes can make cells electrically unstable; scarring may also cause electrical impulses to be misrouted Risk factors: caffeine, tobacco, alcohol; hypertension; anxiety; heart disease; risk increases if taking ANTIHISTAMINES or DECONGESTANTS Complications: cardiomyopathy (weaking of heart muscle); arrhythmias Electrical activity of the heart: - Electrocardiogram: - - Coronary Circulation: - - - o X-axis: time (duration) o Y-axis: millivolts (voltage) Standard waveforms: o P wave: atrial depolarization o QRS complex: ventricular depolarization o T wave: ventricular repolarization 12-Lead ECG: provides twelve diff. vies of electrical activity of the heart Cardiac muscle requires constant supply of O2 and nutrients to function properly Blood flow is GREATEST during DIASTOLE o REDUCED during SYSTOLE (due to contraction and compression of cardiac vessels) Collateral circulation will form if an artery becomes obstructed o offers an important alternative source of blood supply when the original vessel fails to provide sufficient blood; may avoid MI SA node supplied by the RCA (right coronary artery) and LCA (left coronary artery) AV node supplied by RCA (blockage of RCA can lead to conduction issues > dysrhythmias Blockage of LCA can lead to LV dysfunction and possible CHF