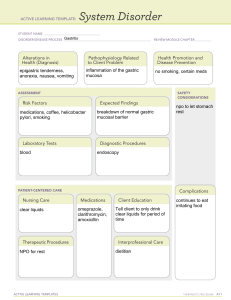
AGA Abstracts raises a question about possibility that bacteria other than H.pylori may contribute to carcinogenesis of gastric cancer. However, little is known about the effects of other gastric microbiome on the occurrence of gastric cancer in human. In this study, based on the hypothesis that certain microbiome may affect the progression of gastric cancer, we intend to observe the differences in the distribution of microbiomes in gastric cancer patients and normal patients. Methods: In this study, gastric mucosa collected by biopsy during ensophagogastroduodenoscopy (EGD) from seven patients with advanced gastric cancer (AGC) and from six noncancerous patients(control group). Gastric biopsies were obtained from the margin of cancer in cancer patients. In control group, biopsies were done from antrum with normal gastric mucosal morphology. DNA was extracted from the gastric tissues and 16s rRNA genes were amplified. They were analyazed by using the molecular profiling approach terminal restriction fragment length polymorphism (T-RFLP) and cloning and sequencing of 16S rRNA genes was performed. Results: Higher number of species was detected in control group, average of 102 species, compared to the cancer group, average of 72 species. The gastric cancer microbiome was characterized by reduced microbial diversity compared to that of control group. Many different bacterial species were found in both groups but distribution was quite different between the two groups. Fusobacteria was more dominant in cancer group and Rhodoacterales was found more prominent in control group. The gastric H.pylori was detected only in one patient from each group. Conclusion: More diverse gastric microbiome was observed in non-cancerous patients and composition of species was different between the two groups. These results suggest that microbial dysbiosis may be involved in gastric carcinogenesis, but it is not yet clear that microbial transition accelerates carcinogenesis. Further studies should include more detailed analysis of spatial and temporal composition of gastric microbiome. Better understanding of microbial differences and changes in healthy and gastric cancer patients could verify the carcinogenesis of gastric cancer. in LPS-induced inflammation of colon cancer cell line. Methods: L. johnsonii was isolated from a human fecal sample, and it was cultured under anaerobic conditions. After cultivation, the EV was separated and concentrated. WST-1, Nitric Oxide concentrations, and ELISA were used to measure whether the EV effectiveness. Result: The anti-inflammatory effect of EV isolated from L. johnsonii was confirmed in Caco-2 cell line. All experiments about EV treatment were under conditions of LPS-stimulation. When the pre-stimulated colon cancer cells were treated with the EV, the concentration of NO, inflammatory factor, was significantly reduced than control. The EV (1ug/ml) treatment group (37.2±6.56 mM/L) had a 34% lower NO value than the positive control group (55.8±4.70 mM/L). Also, EV (1ug/ ml) treatment group showed significantly reduced the TNF (tumor necrosis factor) level (15%) and IL-8 (interleukin-8) level (24%). In these conditions, cell viability was not different between EV treatment group and control group. Conclusion: EV isolated from L. johnsonii had an anti-inflammatory effect in the LPS-induced inflammation of colon cells. These results suggested the potential that just EV alone without whole live form probiotics could help suppress the inflammation of colon. Su535 LACTOBACILLUS REUTERI AND LACTOBACILLUS RHAMNOSUS GG DIFFERENTIALLY AFFECT GUT MICROBIOTA AND PLASMA METABOLITES IN MICE WITH TREG-DEFICIENCY Yuying Liu, Thomas K. Hoang, Christopher M. Taylor, Evelyn S. Park, Jasmin Freeborn, Meng Luo, Stefan Roos, J. Marc Rhoads Background: Treg-deficiency causes a lethal, CD4+ T cell-driven autoimmune disease called IPEX syndrome in humans and called the scurfy (SF) phenotype in a mouse model of the disease. Feeding Lactobacillus reuteri DSM 17938 (LR) to SF mice reprograms gut microbiota, markedly reduces disease progression, and prolongs lifespan. However, the efficacy and mechanism of LR, compared to other probiotics, in producing these effects is unknown. Probiotic Lactobacillus rhamnosus GG (LGG) is one of the most widely used and welldocumented probiotic strains, often used to prevent or treat gastrointestinal infections, antibiotic-associated diarrhea, respiratory infections, and allergies. Objective: To further our understanding of the specificity of probiotics in modulating autoimmunity, gut microbiota and plasma metabolites in well-characterized model of Treg-deficiency (SF mice). Methods: We gavage fed 107 CFU/day of LR or LGG to SF mice daily; starting on d13 after the SF phenotype was identified. Cecal contents and blood were collected on d22 (before weaning) for microbiota analysis by 16s rRNA gene sequencing and for plasma global metabolomics by liquid chromatograpny-mass spectrometry which analyzes 696 metabolites (Metabolon). Results: LR was more effective than LGG in prolonging survival. Both probiotics increased the percentage of tolerogenic dendritic cells in the intestinal mucosa, while only LR reduced inflammatory CD44+ T cells in the mesenteric lymph nodes and circulating blood. Both probiotics restored the fecal microbial alpha diversity, but they produced distinct fecal bacterial clusters and differentially modulated microbial relative abundance (RA). LR increased the RA of Firmicutes, g_Oscillospira while reducing Bacteroidetes, g_Bacteroides and g_Parabacteroides, reversing changes attributed to the SF phenotype. LGG reduced primarily the RA of g_Bacteroides. Both LR and LGG reduced the potentially pathogenic taxon c_Gammaproteobacteria. Plasma metabolomics revealed similar changes of many clusters of metabolites in SF mice associated with treatment with either LR or LGG. However, some unique effects of LR included increased inosine metabolites, central energy metabolismglycolysis-tricarboxylic acid (TCA) cycle intermediates, as well as alterations in redox homeostasis, while LGG heavily affected bile acid metabolism. Conclusions: 1) Different probiotics produce distinct signatures in the fecal microbial community in mice with Treg deficiency. 2) There are many similarities of LR compared to LGG in global plasma metabolites. However, there are strain-specific microbial products with different anti-inflammatory properties, reinforcing the concept that “one size does not fit all” in the treatment of autoimmune disease. Su536 MIXTURES OF LACTOBACILLUS ACIDOPHILUS, LACTOBACILLUS PLANTARUM, AND BIFIDOBACTERIUM LACTIS MITIGATE a-AMYLASE INHIBITION BY EXTRACTS OF NON-GLUTEN WHEAT PROTEINS Tom Fairlie, Anh Do, Ayesha Shah, Mark Morrison, Gerald J. Holtmann Background:Gluten is associated with food hypersensitivity in adults, however non-gluten components such as a-Amylase Trypsin Inhibitors (ATI) are known to induce an immune response, and various bacteria can degrade these ATI’s and reduce inflammatory activity[1]. We explored the interaction between bacterial and non-gluten wheat proteins in pursuit of development of therapeutic options such as probiotic-containing functional foods. Methods:Non-gluten soluble proteins of plain wheat flour (WE) were extracted with salt solution following described methods[2]. Saliva from a single volunteer was collected and processed according to standard protocols[3]. A commercial mixture containing Lactobacillus acidophilus, Lactobacillus plantarum, and Bifidobacterium lactis was used. For the assays, saliva was diluted (1/1500.PBS), and then 0.025ml transferred to individual wells of a microtitre plate. Then 0.025ml of either PBS (control, saliva); WE alone (8μg/ml final concentration, WE); or the probiotic mixture from one capsule resuspended in 2ml PBS (ProB). In parallel, volumes of WE and the probiotic mixture were mixed and incubated for 12h at 37oC, then 0.025 ml of this mixture was added to 0.025ml saliva (Saliva+ProB+WE). The a-amylase activity in these preparations was measured immediately via coupled enzymatic assay using commercially available kits. Two biological replicates using the same source of saliva were performed. Results:Figure 1 shows the a-amylase activity of different mixtures (% of controls). The added WE reduced a-amylase activity to 8.1%±8.0. Coincubation with the probiotic mixture mitigated the effect, as the a-amylase activity was 83.3%±2.1. Saliva a-amylase activity was not altered by the probiotic mixture alone (88.3%±2.7). As such, neither the WE nor the probiotic mixture has detectable a-amylase activity. Conclusions:Soluble non-gluten proteins from wheat inhibit saliva a-amylase activity, but the coincubation of this extract with a commercial probiotic mixture for 12h appears to mitigate these inhibitory effects. Our findings suggest the ATI in WE were inactivated on exposure to specific probiotic bacterial Su534 ANTI-INFLAMMATORY EFFECT OF EV (EXTRACELLULAR VESICLES) ISOLATED FROM LACTOBACILLUS JOHNSONII IN COLON CELL Dong Ho Lee, Jung-Hyun Kim, Ki Sung Kang, wonsuk Lee, Young Soo Park, Cheol Min Shin, Hyuk Yoon, Nayoung Kim, Eun Ji Lee, Yoo Jin Kim Aim: Lactobacillus johnsonii along with other bacterial and mammalian cells releases extracellular membrane vesicles (EV). EV is involved in cell-cell communications in various biological systems. Cell-cell interactions, especially microbiota-host cell crosstalk are multifunctional that implicate complex interactions between cells and cellular factors; many of these cellular factors such as lipids, proteins, nucleic acids, polysaccharides, and various soluble factors are associated with EVs. It was also reported EVs from Lactobacillus sp. can stimulate the host immune and nervous systems, enhance the host immune responses against other bacteria. In this study, we tested whether EV isolated from L. johnsonii has an anti-inflammatory effect AGA Abstracts S-730