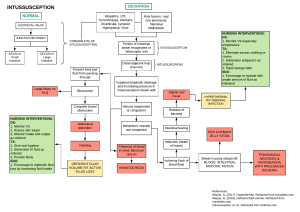
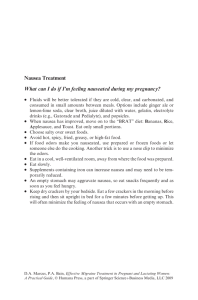
Laboratory Results: Lab WBC RBC Hgb Hct MCV Platelets Glucose BUN Creatinine Sodium Potassium Client Value Normal Value H/L 4.8-10.8 4.7-6.1 14-18 42-52% 82-92 130-400 70-109 8-25 0.7-1.3 135-145 3.5-5 Interpretation Bowel Obstruction Causes: * Hernia, Strangulation, fistula * Perforated Bowel, complete blockage * Peritonitis, cancer, IBD, Crohn’s *Hemorrhage, PUD, ileostomy, colostomy * Ileus. Impaction, necrosis, Surgical Procedure/Treatments: NG tube for Suctioning/decompression to prevent aspiration, Fluid resuscitation, Enemas, Surgical interventions (Stents to open blockages, Ileostomy/colostomy, Resection) Pathophysiology/Clinical Manifestations: A bowel obstruction happens when the small or large intestine is partly or completely blocked. The blockage prevents food, fluids, and gas from moving through the intestines in the normal way possibly from a blockage caused by tumors, scar tissue, or twisting or narrowing of the intestines. In the small intestine, scar tissue is most often the cause. Other causes include hernias and Crohn's disease, which can twist or narrow the intestine, and tumors, which can block the intestine. A blockage also can happen if one part of the intestine folds like a telescope into another part, which is called intussusception. In the large intestine, cancer is most often the cause. Other causes are severe constipation from a hard mass of stool,and narrowing of the intestine caused by diverticulitis or inflammatory bowel disease. Medications: - IV Resuscitation: NS or LR - ABx: gram (-) or anaerobic Cefazolin (Ancef)-cephalosporin - Analgesic: Morphine Sulfate (MS Contin) - Antiemetic: Promethazine (Phenergan) Ondansetron (Zofran) Diagnostics/Labs: V/S & Nursing Physical Assessment, ABGs-Acid/Base balance (R/T: N/V/D), CBC, CMP, WBC w/ DIFF, Chem Panel, UA, BUN, Serum, Creatinine, Lactate dehydrogenase tests (tissues damage), Abd. X-Ray (may show blockages in sm or lrg intestines), CT Scan to detect blockages, Ultrasound, Type & Cross match for surgical intervention, R/O hepatic obstruction with AST, ALT, Occult blood- stool sample, Stool culture, 12 Lead ECG R/T arrhythmias Secondary to Electrolyte imbalances. ND 1: Deficient Fluid Volume R/T vomiting and decreased fluid absorption in colon secondary to Bowel Obstruction AEB low blood pressure, increased HR, decreased urinary output, decreased skin turgor, dry mucous membranes, and change in LOC. ND#1 Goals: STG: Client will be A&Ox4 by noon. LTG: Client will be increasing urinary output to at least 30ml/hr by end of shift. ND 2: Risk for Aspiration R/T entry of secretions from gastric acid into lungs secondary to Bowel Obstruction. ND 3: Nausea R/T wavelike sensation in back of throat, epigastrium, or throughout the abdomen with or without vomiting secondary to Bowel Obstruction AE sour taste in mouth, reports of being “sick to stomach”, aversion to food, and increased salivation. ND#2 Goals: STG: Client will state 2 ways to ND#3 Goals: STG: Client will verbalize1 way to prevent aspiration by noon. decrease noxious stimuli that cause nausea by noon. LTG: Client will maintain a patent airway by end of shift. LTG: Client will report elimination of nausea by end of shift. Interventions STG: Interventions STG: Interventions STG: * Obtain a patient history to ascertain the probable cause of the fluid disturbance. R: Such information can help guide interventions. Causes may include acute trauma and bleeding, reduced fluid intake from changes in cognition, large amount of drainage after surgery, or persistent diarrhea/vomiting. * Monitor and document BP & HR. R: Reduction in blood volume can cause hypotension/tachycardia. *Monitor for changes in mental status. R: Dehydration may alter mental status, esp in older adults. May include: restlessness, anxiety, lethargy, and confusion. *Monitor active fluid loss from wound drainage, tubes, diarrhea, bleeding, vomiting, insensible loss and maintain an accurate I & O record. R: Fluid loss can cause decreased fluid volume and dehydration. *Monitor V/S and temp. R: Febrile states decrease body fluids through perspiration and increased respirations. * Monitor LOC. R: A decreased LOC is a prime risk factor for aspiration. *Assess the presence of cough and gag reflexes. R: The lungs are normally protected against aspiration by reflexes such as cough and gag. *Evaluate swallowing ability by assessing for the following: Coughing, choking, throat clearing, gurgling or “wet” voice during or after swallowing. If there is residual food after eating. Regurgitation of flood/fluid through nares. R: Impaired swallowing increases r/f aspiration. *Auscultate bowel sounds to evaluate bowel motility, and assess for and distention and firmness. R: Decreased GI motility increase r/f aspiration. *Assess for presence of N/V. R: N/V increases risk, pt should get antiemetics to prevent gastric regurg. * Assess the cause of the Nausea. R: Determining the cause will guide the choice of interventions, such as removing stimulus. *Assess the nausea characteristics: Hx, duration, Freq, Severity, Precipitating factors, Medications, Measures to alleviate the problem. R: A comprehensive assess. Of the nausea can help determine interventions or alleviate problems. *Keep an emesis basin within easy reach of the Pt. R: N is often associated with V. *Offer or assist with oral hygiene Q2-hrs. R: N is often related to anorexia and increased salivation. Oral hygiene helps promote comfort *Remove noxious odors from the room. R: Strong or noxious odors can promote nausea. LTG: * Assess skin turgor and mucous membranes for signs of dehydration. R: Loss of interstitial fluid causes loss of skin turgor. Skin turgor assessed over the sternum or forehead is best. *Assess the color and amount of urine. Report urine output of less than 30mls/hr for 2 consecutive hours. R: Concentrated Urine denotes fluid deficits. *Monitor serum electrolytes and urine osmolality, and report abnormal values. R: Elevated BUN suggest fluid deficit. Urine specific gravity is likewise increased. *Insert IV catheter and maintain IV access. R: Parental fluid replacement is indicated to prevent or treat hypovolemic complications. *Administer parental Fluids as ordered. R: Fluids are needed to maintain hydration states. LTG: * Assess for S/S of aspiration by auscultation of breath sounds for development of wheezes or crackles. Monitor CXR as ordered. R: Aspiration can occurs with sm amounts. CXR will show infiltrates. *Pts with NG Tubes or gastronomy tubes: check placement before feeding, using tube markings, x-ray study, pH of gastric contents, and color of aspirate as guides. R: A displaced tube can tube feeding into airway. *Keep suction available and use as needed. R: Tracheal suction may be needed to maintain an airway. *Position Pts with decreased LOC supine on side. R: Rescue positioning decreases r/f aspiration. *Elevated HOB 30-45 degrees. R: Upright positioning reduces r/f aspiration by decreasing gastric reflux. LTG: * Maintain fluid balance for pts at risk for nausea. R: Adequate hydration before surgery or Chemo reduces nausea. *Teach pt to use nonpharmacological nausea control techniques: relaxation, guided imagery, music therapy, distraction, deep breathing. R: helps patient manage their nausea. *Administer Antiemetic’s as ordered. R: Antiemetic’s raise threshold of chemoreceptor trigger zones to stimulation. *Teach pt to change positions slowly. Sudden or gross movement can increase nausea. *Teach patient to avoid greasy, fried, or spicy foods. R: These foods exacerbate nausea. DIABETES Pathophysiology Diabetes mellitus is a syndrome with disordered metabolism and inappropriate hyperglycemia due to either a deficiency of insulin secretion or a combination of insulin resistance and inadequate insulin secretion to compensate. Type I diabetes is due to pancreatic islet B cell destruction predominantly by an autoimmune process, and these persons are prone to ketoacidosis, while type 2 diabetes is the more prevalent form and results from insulin resistance with defect in compensatory insulin secretion. Treatments and Medication: Glimepiride, metformin, repaglinide, Nateglinide, Acarbose, Actos, Avandia, Javia, Humalog. Lantas Insulin Therapy, diet changes and exercise. Diagnostics and Labs Hemoglobin AIC test, Glycated hemoglobin tests. Fasting plasma glucose (FPG), Random plasma glucose (RPG) Nursing Interventions Assess for signs of hyperglycemia, Assess blood glucose level before meals and at bedtime. Assess for signs of avoidance to learn. Identify client's support person that may need information about the planned diabetes regimen Set up patient witch a dietician to promote healthier diet. Patient Education Patient Education Teach Pt proper way to give and store insulin. Provide written information or guidelines and selfleaning modules, especially about the proper diet essential for diabetic patients Provide positive reinforcements and evaluate the learning of skills Educate about nearby community resources or support groups Expected Outcomes Improved nutritional status, maintenance of integrity Ability to perform basic diabetes self-care skills Patient maintains normal glucose levels RISK FACTOR URINARY CATHETER USAGE PREGNANCY PREMATURE NOWBORNS DM NEUROGENIC BLADDER SEXUAL INTERROUSE LOWER URINARY TRACK INFECTION Bacteria is introduced. Pathogens ascends through the urethra toward bladder colonizing in the urethra (urethritis), Bladder (cystitis), or prostate (prostatis) Bacteria multiply and overwhelms the hosts defense system reproducing rapidly by uropathic bacteria attracting to the uroepithelium. These bacteria such as E. Coli have pili adhesions that allow them to bind to mucosal cellular receptors and enter uroepithelial cells and resist flushing during urination. Labs and diagnostics: -urine dipstick and microscopy Urine culture of fresh urine McCance, K.L,& Huther, S.E. (2005). Pathophysiology: the biologic basis for disease in adults and children (5th ed.) St. Louis, MO: Elsevier Mosby. Hasdungan, A (2019). UTI. Retrived from https://armandoh.org/ October 17. 2019. Bacteria KEEPS Keisiella E. coli Enterobacteria Proteus Staph Inflammatory response and Neutrophil infiltration promoting inflammation and edema in the bladder wall, which discharge stretch receptors. Pathogens use enzymes to reduce nitrate to nitrite Pathogens ascends toward kidney and colonizes and spreading infection. Dissemination also occurs by way of bloodstream. Upper Urinary tract infection (Pyelonephritis) Medullary infiltration of WBC with renal parenchyma and capsule inflammation, renal edema, necrosis of renal papillae. Cytokines released systemically Bacteremia Bacteria spread to circulation via renal vein and leads to septic shock if left untreated Treatment: -3 to 4 week’s microorganism specific Antibiotic Lots of fluid -Dysuria -Frequency -Urgency Treatment: 3 to 7 days Microorganism Specific antibiotic Hematuria Foul smelling urine (+) bacterial culture Increase WBC (+) Nitrites -Malaise Fever vomiting Rigors Flank Pain