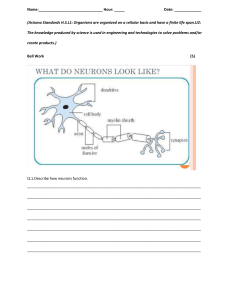
GNMD 6044 Final study guide CNS, PNS, Amyloidosis 1. Acute pyogenic meningitis (bacterial) – E, Age related, CF, M, C a. It is an inflammatory process of the leptomeninges (aka thin meninges: pia & arachnoid is csf) and CSF within the subarachnoidal space b. Etiology (in the test) E. coli, group B streptococci (neonates) H. influenzae (infants, children) N. meningitidis (adolescents, young adults), epidemic Streptococcus pneumoniae, Listeria monocytogenes (adults, elderly) Klebsiella or anaerobics (immunosuppressed) c. Clinically Starts with Fever, headache, N/V, photophobia, irritability, clouding of consciousness, and neck and back stiffness. Kerning and Brudzinski positive. CSF – cloudy or purulent, increased pressure, 90,000 neutrophils/mm3, elevated protein level, marked reduced glucose. Presence of bacteria in smears or cultures. Lumbar puncture, smear, culture, immunoelectrophoresis, CT. Extravasation of fluid plasma protein, increased pressure Extravasation of cells neutrophils in CSF Glucose is reduced because the bacteria eats the glucose d. Morphology exudate within the leptomeninges, located at the base of brain (H. influenzae), h. Flu can cause meningitis in children around the base of the brain…or at cerebral convexities near sagittal sinus (Pneumococcus). Pneumococcus in convexities more common in adults Purulent Meningitis – A creamy exudate opacifies the leptomeninges. Probably Neisseria meningitides or step pneumo Histology – neutrophils fill the subarachnoid space 2. Brain abscess – E, CF, M a. It is an acute focal suppurative infection of the brain. Severe b. Etiology Direct implantation (trauma, direct infection), local extension (mastoiditis, paranasal sinuses), hematogenous spread (heart, lungs, bones, tooth extraction) Risk factors – acute bacterial endocarditis, congenital heart disease with right-to-left shunt, chronic pulmonary sepsis with bronchiectasis. Verrucae in the valves may detach and go to brain causing an infarct but accumulation of the bacteria will cause the abscess--Tetralogy of falot Streptococci and staphylococci (common) c. Morphology – lesions with central liquefactive necrosis, surrounded by fibrosis, and edema. Common in frontal, parietal lobes and cerebellum Clinically – focal deficits, raised intracranial pressure w/ N/V. CSF – increased pressure, increased WBC and proteins, normal sugar content because it’s not in csf but in the area of abscess d. Complications – Abscess may open up in the ventricles causing ventriculitis, meningitis, sinus thrombosis e. Prognosis – mortality rate 10% 3. Syphilis – M, a. It is developed during tertiary stage of syphilis in 10% of patients left untreated. Patients with HIV are at increased risk b. Morphology Meningovascular neurosyphilis – is a chronic meningitis involving the base of the brain, cerebral convexities, and spinal leptomeninges. It may be associated with obliterative endoarteritis and cerebral gummas (tumor like). Inflammation of the arteries with thrombosis. Seizure, hemiparesis, hemiplegia. Paretic neurosyphilis – Damage to the substance of the brain due to an inflammatory processMemory mood and behavioral changes arriving to severe dementia: invasion of the brain by Treponema pallidum, progressive loss of mental and physical functions, memory disturbances, mood alterations, disturbed speech, optic nerve atrophy, and severe dementia. Histology – inflammatory meningeal lesions and parenchymal damage located at frontal lobe (loss of neurons, proliferation of microglia and astrocytes, gliosis (around the dying neurons), iron deposits, presence of spirochetes, granular ependymitis) Tables dorsalis damage by the spirochetes to the sensory nerves in the dorsal roots complicated with ataxia, loss of pain sensation, skin and joint damage (Charcot joints), “lightning pains”, loss of deep tendon reflexes, urinary and fecal incontinence. Histology – loss of axons and myelin in the dorsal roots, and atrophy in the dorsal columns of the spinal cords. 4. Viral encephalitis – E, M, CF a. Arthropod-borne (Arbo) Viral Encephalitis It is an epidemic encephalitis most in tropical regions of the world. In the Western hemisphere, it is caused by Eastern and Western equine, Venezuelan, St. Louis, and California types of arboviruses b. c. d. e. f. Clinically – reflex asymmetry, ocular palsies, seizure, confusion, delirium, stupor or coma. CSF – colorless, slightly elevated pressure, neutrophilic and lymphocytic pleocytosis, elevated protein levels, normal sugar content Morphology – lymphocytic meningoencephalitis, multiple foci of necrosis of gray and white matter, viral antigens inside the neurons, perivascular cuff, neuronophagia, gliosis (proliferation of microglia around neuron). Herpes Simplex Virus Type 1 It causes encephalitis in children and young adults Clinically - alteration in mood, memory, and behavior. Subacute manifestations – weakness, lethargy, ataxia, seizure Morphology – encephalitis involves the temporal lobes, orbital gyri of the frontal lobes. Histology – necrotizing (arteritis) and hemorrhagic lesions with intranuclear viral inclusion bodies in neurons and glia. Herpes Simplex Virus 2 It causes severe encephalitis in 50% of neonates born by vaginal delivery to women with active primary HSV genital infection In AIDS, it results in acute, hemorrhagic, necrotizing encephalitis Varicella-Zoster Virus (Herpes Zoster) No neurologic manifestation with chickenpox Reactivation of virus in adults causes shingles – painful, self-limited, vesicular skin eruption in the distribution of the dermatome, complicated with postherpetic neuralgia syndrome (10%) In AIDS patient (12%) - acute encephalitis, with early demyelination, necrosis, and inclusion bodies in neurons and glia Cytomegalovirus Common in fetuses (periventricular necrosis, microcephaly, periventricular calcifications) and AIDS patients (15-20%) with subacute encephalitis. Histology – ependymal and subependymal regions of the brain are involved. Severe hemorrhagic necrotizing ventriculoencephalitis, and chorioid plexitis. Prominent cytomegalic cells with intranuclear and intracytoplasmic inclusions CMV antigens demostrate intranuclear and intracytoplasmic inclusions in Purkinje cells of the cerebellum. Poliomyelitis It is caused by poliovirus a member of picorna group of enteroviruses In nonimmunized individuals it causes a subclinical or mild gastroenteritis, and in a small fraction it involves the nervous system Clinically Subclinical (95%) Gastroenteritits, nonparalytic (meningitis), paralytic (post polio syndrome) Meningeal irritation (fever, malaise, and headache) Paralysis (m. neck, trunk, four limbs, respiratory muscles); mild cases – asymmetric and patchy paralysis in lower limbs; CSF – aseptic meningitis. Postpolio syndrome – it is developed 25-35 years after the resolution of the initial illness with progressive weakness, decreased muscle bulk, and pain Morphology Loss of motor neurons with flaccid paralysis, muscle wasting, hyporeflexia, which are permanent. Histology – mononuclear cell in perivascular cuffs and neuronophagia of the anterior horn motor neurons of the spinal cord, with the presence of poliovirus inside the cells Complications – mortality 5-25% - paralysis of respiratory muscles, myocarditis g. HIV-1 Meningoencephalitis. Subacute encephalitis Clinically – dementia, mental slowing, memory loss, mood disturbances, apathy and depression. Motor abnormalities, ataxia, Bladder and bowel incontinence, and seizure. X-ray – diffuse cortical atrophy, focal abnormalities in the white matter, ventricular dilation Morphology – meninges are clear, dilation of ventricles, sulcal widening, abnormal cortical thickness. Symetric demyelination in corona radiata Histology – infiltrates of microglial nodules with multinucleated giant cells, tissue necrosis, gliosis, located in subcortical white matter, diencephalon, and brain stem. Presence of HIV in CD4 lymphocytes and multinucleate macrophages, diffuse astrogliosis 5. Rabies – M, L, CF a. It is transmitted to humans by the bite of a rabid dog, or exposure to bats. Virus enter the CNS by ascend along the peripheral nerves from the wound site. Incubation period 1-3 mo b. Clinically- malaise, headache, fever, local paresthesias around the wound (diagnostic). Sometimes, severe encephalitis with CNS excitability, painful touch, violent motor responses, convulsions. Contracture of pharyngeal muscles on swallowing with foaming at the mouth (hydrophobia), meningismus, flaccid paralysis, alternating mania and stupor, coma and death (respiratory center failure) c. Morphology Brain edema and vascular congestion. Histology – neuronal degeneration, inflammatory reaction in the basal ganglia, midbrain, floor of the fourth ventricle, and medulla. Negri bodies – cytoplasmic, round to oval, eosinophilic inclusions – in pyramidal neurons of the hypocampus and Purkinje cells of cerebellum. Presence of rabies virus within Negri bodies 6. Encephalitis (measles, JC virus, etc) – L, M a. It is a viral encephalitis caused by polyomavirus (JC virus), characterized by demyelination (virus infects oligodendrocytes) b. It is present in immunocompromised individuals c. Clinically – focal and progressive neurologic symptoms and signs. CT and MRI - multifocal lesions in the hemispheric or cerebellar white matter. d. Morphology – patches of irregular, ill-defined destruction of the white matter from mm to cm, located in the cerebrum, brain stem, cerebellum, and spinal cord. e. Histology – patch of demyelination, with lipid-laden macrophages, reduced number of axons, bizarre giant astrocytes, and oligodendrocytes that contain viral antigens in the periphery. 7. Subacute sclerosing panencephalitis – measles a. It occurs in children or young adults, months or years after an initial infection with measles. It represents a persistent but nonproductive infection of CNS by altered measles virus. Koplik spots are only found in early stage rubeola exposure, not as a sequelae b. Clinically – cognitive decline, spasticity of limbs, seizures. c. Morphology – widespread gliosis, myelin degeneration, viral inclusions with measles virus within the nucleus of oligodendrocytes and neurons, inflammation of white and gray matter, neurofibrillary tangles,. 8. Cerutzfeldt-Jacob’s – E, CF, M a. Transmissible Spongiform encephalopathy (Prion disease) b. It is characterized by “spongiform change” caused by intracellular vacuoles in neural cells, dementia, and the presence of prion protein PrP. c. Pathogenesis - PrP is a normal protein in neurons. It becomes pathogenic when is changed from -helix isoform PrPc to an abnormal -pleated sheet isoform PrPsc that is resistant to digestion with proteases. This change occurs spontaneously and slowly (sporadic cases) or at a higher rate caused by mutations (familial cases). PrPsc can corrupt the integrity of normal cellular components. CJD - point mutation in PrPN gene (D178N) and Val at codon 129. Fatal familial insomnia - point mutation in PrPN gene (D178N) and Met at codon 129. Aggregates of PrPsc protein inside the cell cause the neuronal death. d. Morphology– spongiform transformation (gray matter) of the cerebral cortex, putamen, and caudate nuclei. e. Histology – small, apparently empty, microscopic vacuoles in the perikaryon/cytoplasm of the neurons. Neuronal loss, reactive gliosis, no inflammation. f. Fatal familial insomnia – not spongiform pattern, neuronal loss, reactive gliosis in thalamus. g. Clinical rapidly progressive dementia with changes in memory, and behavior, involuntary jerking muscle contractions, ataxia. Sporadic 85% peak incidence 7th decade iatrogenic transmission – cornel transplantation, deep implantation electrodes, contaminated preparations of GH. Fatal within 7 mo. h. Variant CJD vCJD – young adults , like CJD, related with the ingestion of beef from cows with bovine spongiform encephalopathy. i. GSS – inherited disease with mutation of PrPN gene, chronic cerebellar ataxia, and progressive dementia. Fatal in several years j. Fatal familial insomnia – sleep disturbances, ataxia, autonomic disturbances, stupor, coma, fatal within 3 y. 9. Multiple sclerosis – CF, M a. It is characterized by episodes of neurologic deficit, separated in time, and white matter lesions (sclerotic plaques), separated in space. Incidence 1/1000 individuals. b. Female/male 2:1, 20-30y/o c. Relapse and remission that last for many year (time) d. Lesions (WM) Spread in brain an SpC (space) e. Pathogenesis Environmental (infection roseola virus, trauma, pregnancy), genetic, and immune factors. 15fold higher risk in HLA-DR2 individuals, and in first-degree relatives. Cell-mediated immunity (Autoimmunetype 4 HS) with infiltration of CD4+ and CD8+ lymphocytes and macrophages that induce oligodendrocyte injury. Antibody-mediated damage of myelin (type 2 HSR) Genetic: Pregnancy may awaken the dz Morphology Multiple, well-circumscribed, depressed, glassy, irregular plaques associated with surrounding sclerosis of the white matter throughout the CNS (lateral ventricles, optic nerve and chiasm, brain stem, cerebellum, spinal cord) Clinical Unilateral visual impairment for a few days (optic neuritis, retrobulbar neuritis), ataxia, nystagmus, weakness, numbness, tingling (sensorimotor), spasticity (central), dysarthria, difficulty in controlling of bladder, dementia CSF – mildly elevated proteins, gamma globulin is increased showing oligoclonal bands, moderate pleocytosis (B cells)- b cells are basically producing the G globulins (antibodies against myelin) Complications respiratory paralysis, UTI Variants Devic disease (RAPID progression), neuromyelitis optica - bilateral optic neuritis and prominent spinal cord involvement. It is rapidly progressive, with more destructive lesions Acute MS, Marburg form – young individuals, fulminant course in several months. Large and numerous plaques 10. Alzheimer’s disease – M, CF, P a. Degenerative diseases are characterized by progressive loss of neurons in patients without previous neurologic deficit b. Alzheimer’s is a degenerative disease affecting the Cerebral cortex c. It is the most common cause of dementia in the elderly, starting after 50y; 5-10% familial; in Down syndrome after 45y/o d. Clinically alteration in mood and behavior (sleeplessness, agitation, wandering, anxiety, and depression), progressive disorientation, memory loss, language deficit, loss of mathematical skills, loss of learned motor skills, aphasia, Dementia, and after 5-10y – pts becomes incontinent, mute, and immobile. Pneumonia causes death. Accurate dx only in 80-90% Neurons that produce Acetylcholine are lost (important to know for test perhaps) MMB-Mood Memory Behavior Atherosclerosis can cause dementia e. Morphology Cortical atrophy, narrow gyri, widening of cerebral sulci in frontal, temporal (hippocampus), and parietal lobes, and ventricular enlargement f. Histology – neurofibrillary tangles (bundles of filaments in the cytoplasm of the neurons that displace or encircle the nucleus. Paired helical filaments, protein tau, ubiquitin, and amyloid -peptide) senile (neuritic) plaques (focal, spherical collections of dilated, tortuous silver-staining neuritic processes surrounding a central amyloid core. The dominant component of plaque core is A-peptide that derives from APP) amyloid angiopathy (amyloid deposition around the blood vessels)- brain becomes malnourished Granulovacuolar degeneration – small intraneuronal vacuoles which contain an argyrophilic granule Hirano bodies – rod like, elongated, glassy, eosinophilic bodies containing actin in hypocampal pyramidal cells, red/pin color from stain g. Pathogenesis Amyloid -peptide – Amyloid precursor protein APP is a transmembrane protein with unknown function. APP is broken down by - and -secretases which generate A-peptide from APP. Apeptide aggregates and generates the amyloid that is found in the brain and is neurotoxic for the neurons Hyperphosphorylated Tau protein (also neurotoxic) Presenilins – in familial Alzheimer disease, there is mutation in genes for presenilin-1 and presenilin-2 that are responsible for increased production of A- peptide, and they are target for cleavage by caspase proteases, playing a role in apoptosis of neurons Apolipoprotein E – mutation in 4 loci of Apo E gene increases the risk (early onset) for Alzheimer disease. Apo E is present in plaques Mutation in 2-macroglobulin increases the risk of Alzheimer disease 11. Parkinson’s – CF, M, P a. Parkinsonism is a syndrome characterized by diminished facial expression stooped posture slowness of voluntary movements progressively shortened, accelerated steps rigidity “pill-rolling” tremor b. There is damage to nigro-striated dopaminergic system c. Idiopathic Parkinson Disease (Paralysis agitans) It shows an autosomal dominant inheritance Pathogenesis – Mutation in the gene for -synuclein, a protein in the presynaptic terminal, causes accumulation of it in inclusions characteristic for IPD, the Lewy bodies Morphology pallor of the substantia nigra and locus ceruleus loss of the pigmented, dopaminergic neurons in the above regions with gliosis Lewy bodies – single or multiple intracytoplasmic, eosinophilic inclusions with a dense core and a pale halo - inside the neurons; located - cerebral cortex, amygdala, and brain stem neurons Clinically- Parkinson syndrome, dementia 12. Huntington’s chorea – Inheritance, Etiology E, morphology M, clinical features CF, Complications C, Pathology P a. Not congenital but inherited in Autosomal dominant pattern b. characterized by progressive movement disorders, dementia, and degeneration of striatal neurons c. Pathogenesis the loss of striatal inhibitory output from the degeneration of GABA-containing neurons, to the external portion of the globus pallidus. The gene responsible for the disease is located on chrom.4, and it shows unstable CAG trinucleotide repeats. Protein Huntingtin. Increased number of repeats – anticipation d. Morphology – small brain with atrophy of the caudate nucleus, and putamen, and dilation of the third and fourth ventricles. Histology – severe loss of striatal neurons – GABA, enkephalin, and substance P neurons e. Clinically – the disease starts at the 3rd or 4th decade; dementia and chorea (jerky, hyperkinetic or dystonic movements affecting all parts of the body); later – parkinsonism, bradykinesia, and rigidity. Increased risk of suicide and infections. Death within 15y. 13. Amyotrophic lateral sclerosis – CF, M, a. Degenerative Diseases affecting Motor Neurons b. It is characterized by problems in the nerve that causes atrophy of muscle, cortex and spinal cord affected. c. Neuronal muscle atrophy (amyotrophy) and hyperreflexia due to loss of lower motor and upper motor neurons in the anterior horns of the spinal cord and corticospinal tracts, respectively. Men, fifth decade. 5-10% familial with autosomal dominant inheritance d. Pathogenesis – cause unknown. In familial cases, missense mutation in copper-zinc superoxide dismutase gene on chrom.21 which causes and accumulation of oxide free radicals (it’s usually an antioxidant) e. Morphology: Ventral root is motor neurons f. Clinical Asymmetric weakness of the hands, dropping objects, difficulty performing fine motor movements, cramping, and spasticity of the arms and legs. Later, diminished muscle strength, and mass Respiratory infections due to involvement of respiratory muscles In some pts, anomalies of deglutition and phonation dominate 14. Chronic alcoholism – M a. Niacin deficiency- pellagra Features - dermatitis (exposed areas: face, hands, knees), diarrhea, dementia - psychosis, glossitis - inflammation and edema cause a large, red tongue b. Thiamine (B1) deficiency, Beriberi Wernicke-Korsakoff syndrome (dry Beriberi) – ataxia, ophthalmoplegia, polyneuropathy, retrograde amnesia and confabulations. Common in Chronic alcoholism Morphology – petechial hemorrhage and necrosis in mammillary bodies, and paraventricular regions: third and fourth ventricles c. Wernicke encephalopathy, because of thiamine deficiency. Mental confusion, ataxia, abnormal ocular motility, polyneuropathy d. Korsakoff psychosis - retrograde amnesia, confabulatory symptoms e. Alcoholic cerebellar degeneration: unsteadiness of gait, ataxia, incoordination, there is destruction of Purkinje cells in the (upper) cerebellum f. Central pontine myelinolysis - progressive weakness of bulbar muscles that causes dysphagia and dysarthria, and inability to swallow. Quadriparesis, coma, death g. Polyneuropathy - deficiency of thiamine and other B vitamins, Numbness, paresthesias, pain, weakness, ataxia 15. Gliomas (most common brain tumors) – types T, L a. Brain tumors in general: 20% of cancer of childhood, and 70% arise in posterior fossa, while in adults, in cerebral hemispheres. Gliomas Neuronal tumors Poorly differentiated neoplasms Meningiomas b. Gliomas: They include astrocytomas, oligodendrogliomas, and ependymomas Astrocytomas: Fibrillary Astrocytoma and Glioblastoma Multiforme 80% of adult primary tumors; in cerebral hemispheres; 4-6 decade Clinically – seizures, lethargies, headache, and focal neurologic deficit. They become more anaplastic with time Fibrillary astrocytoma, mostly benign but if it stays there for too long becomes more aggressive (gliobastoma multiforme) Morphology ◊ Diffuse Fibrillary Astrocytoma is well-differentiated (less cells and bv), or evolves to less differentiated (more cell, bv)Anaplastic astrocytoma and Glioblastoma multiforme Genetics ◊ low grade astrocytoma - inactivation of p53 gene, and overexpression of PDGF-A and its receptor genes; higher grade astrocytomas – mutation in Rb gene; glioblastomas – amplification of EGFR gene Pilocytic Astrocytoma: Common in children and young adults; located in cerebellum; Morphology – cystic tumor with a nodule in the wall of the cyst. Prognosis – slow grow; pts survive for 40y after total resection Pleomorphic Xanthoastrocytoma: Children and young adults; temporal lobe; history of seizure. Morphology – neoplastic astrocytes, with abundant reticulin deposits, and inflammatory infiltrate Oligodendroglioma 5-15% of gliomas; located in cerebral hemispheres; present in 4-5th decade Clinically – several years of neurologic complaints, and seizure Morphology – well-circumscribed, gelatinous, gray mass with cysts, hemorrhage, and calcifications Prognosis – better prognosis than astrocytomas. 5-10y survival rate Ependymomas 5-10% of tumors in 2nd decade; located near the fourth ventricle. Morphology – solid or papillary masses extended from the floor of the ventricle. Clinically – hydrocephalus, N/V, CSF dissemination. Prognosis – poor, 4y survival rate Myxopapillary ependymomas – occur in filum terminale of the spinal cord Subependymomas – solid, calcified, slow growing nodules attached to the ventricular lining and protruding into the ventricle Choroid plexus papillomas – in children in lateral ventricles, in adults in 4th ventricle. Hydrocephalus. 16. Medulloblastoma – M, location L, age A a. common in children; b. located in midline of cerebellum; vermis c. well-circumscribed, gray, friable tumor composed of sheets of d. anaplastic cells forming Homer-Wright rosettes. e. Very malignant, disseminates through CSF; radiosensitive 17. Meningiomas – L, A a. Benign tumors of adults b. Morphology – well-defined, encapsulated tumor masses arising from meningothelial cells of arachnoid, with their base on dura compressing the brain (pushing the brain down, not in the brain. Psammoma bodies (calcifications) are present c. Clinically – slow growing, express progesterone receptors and grow during pregnancy d. Metastatic tumors Primary tumor is located in the lungs, breast, skin (melanoma), kidney, GI tract 18. Schwannoma – L, M a. Schwann Cells, line axons and responsible for the production of myelin b. Well circumscribed, encapsulated masses that are attached to the nerves. Tumors show cellular areas with Verocay bodies, and looser, myxoid regions c. Clinically – common location in the cerebellopontine angle involving the eight nerve – tinnitus, hearing loss (acoustic neuroma), trigeminal nerve, and dorsal roots. Associated with neurofibromatosis type 2. 19. Guillain-Barre syndrome – E, M, CF, C a. Disease of the Peripheral Nerves: Inflammatory Neuropathies: b. (Acute Inflammatory Demyelinating Polyradiculoneuropathy) c. It is the most common life-threatening disease of PNS, characterized by ascending paralyses, inflammation and demyelination of peripheral nerves and spinal nerve roots (radiculoneuropathy) d. Autoimmune disease type 4 hsrxn e. Type 2 association with circulating myelin antobodies f. Pathogenesis Preceded by a viral infection (Campylobacter jejuni, cytomegalovirus, Epstein-Barr virus, and Mycoplasma pneumoniae), vaccines, surgery T cell-mediated immune response is generated – segmental demyelination of axon by macrophages and lymphocytes. Circulating antibodies (Anti-GM1) are present g. Morphology Inflammation of peripheral nerve – perivenular and endoneurial infiltration by lymphocytes, macrophages, and plasma cells located in the spinal and cranial motor roots. Segmental demyelination. Oligoclonal bands involved h. Clinical course Ascending paralysis (legs, arms, face), weakness, disappearance of deep tendon reflexes; Sensory (Pain, parasthesias, dysesthesias); Autonomic (tachycardia, hypo/ hypertension, flushing, sweating, sphinchters); elevation of CSF protein due to inflammation i. Complications Respiratory paralysis, autonomic instability, complications of tracheostomy j. Prognosis – Most (good recovery), 10-20% disability, 3% relapses, mortality rate 2-5% 20. Diabetic neuropathy - type, M a. Diabetes in bv’s induces atherosclerosis b. In small bv’s –hyaline arteriosclerosis c. Several patterns: distal symmetric sensory or sensor-motor neuropathy, autonomic neuropathy, focal or multifocal asymmetric neuropathy d. Most common is distal symmetric sensorimotor neuropathy characterized by decreased sensation in distal extremities, loss of pain sensation, ulcers, less evident motor neuropathy e. Morphology Segmental demyelination, relative loss of axon fibers. Arteriolo-hyalinization of Endoneural vessels (vaso nervorum) f. Clinically Peripheral neuropathy involves 50% of diabetics after 25y of diabetes. 100% have conduction abnormalities, autonomic neuropathy in 20-40% 21. Carpal tunnel syndrome – E, CF, a. Compression neuropathy – a nerve is compressed or entrapped within an anatomic compartment b. Carpal tunnel syndrome – compression of median nerve at the level of wrist by transverse carpal ligament c. Predisposing factors – pregnancy, osteoarthritis, hypothyroidism, amyloidosis, excessive usage of the wrist d. Clinically – Mostly sensory, numbness and paresthesias of the tip of the thumb and first two fingers e. Pathology - ischemia, edema of myelin sheath, demyelination 22. Bell’s palsy paralysis no wrinkles form, in stroke paralysis wrinkles form 23. Thoracic outlet syndrome - E, M, CF, C a. Compression of blood vessels/nerves in the space between clavicle and first rib b. Neurogenic Brachial plexus - spasm/hypertrophy of scalene m. Paresthesia in arm/fingers, pain in neck/shoulder/hand, weakening grip, atrophy of thenar/hypothenar eminences c. Vascular Subclavian vein/artery Veins - arm swelling, cyanosis, pain Arteries - muscle cramping, coldness/blanching of hand d. Unknown/nonspecific Chronic pain in the area of thoracic outlet that worsens with activity, but specific cause of pain cannot be determined e. Etiology a. Anatomical defects, posture, trauma, repetitive activity, overweight, pregnancy 24. Amyloidosis – primary, secondary, familial, isolated, types of proteins, morphology, clinical a. It is a disease that is characterized by deposition of Amyloid protein in different organs b. Common components of Amyloid Amyloid P Laminin, collagen IV, proteoglycans Apo E c. Two types of Amyloid AL – Primary amyloidosis, MM, B-cell lymphoma Ig light chain excess production of immunoglobulin and abnormal assembly in MM, and B cell lymphoma (excess light chains) AA – Secondary amyloidosis (RA, Ankylosing Sp, SLE, Lung abscess, TB, osteomyelitis), FMF, Cancer (Hodgkin’s, renal cell ca) AA from serum amyloid protein d. Stain red w/Congo red e. Beta-pleated sheet f. Diagnosis – biopsy Gingiva Rectum Abdominal subcutaneous fat Usually deposited in the framework of tissues in b/w cells, in the connective tissue that forms the framework of tissue. Dentists can dx because of swelling of tongue g. Clinical Classification of Amyloidoses Systemic deposition Primary Secondary FMF - pyrin Isolated Single organs – heart, kidney, GI, skin, joints, etc Aorta atherosclerosis – medin derives from lactadherin, produces by SMC ◊ Medin is the amyloid material produced in smooth muscle cells Alzheimer disease – Aß amyloid (peptide) derived from AßPP in the cell membrane ◊ AB peptide deposited in the neurons, (neurofibrillary tangles Alzheimers)- forming to so called senile plaques near BV’s amyloid angiopathy DM type 2 – amylin a variant of calcitonin ◊ Deposition of amyloid material in between beta cells in the islets of langherhan’s, damage to islets= more severe diabetes Senile cardiac amyloidoses – tranthyretin secreted by liver, transports T3, T4 Spongiform Encephalopathy – PrP protein ◊ Spongiform prions inside vacuoles in neurons. Dementia chorea Medullary carcinoma of thyroid gland – amyloid is procalcitonin ◊ Pink material in cancer from procalcitonin medullary AL amyloid - Ig light chain AA amyloid ◊ Derives from Serum amyloid A SAA ◊ SAA is acute phase protein produced by the liver in acute/chronic inflammation ◊ Amyloid enhancing factor AEF promotes formation of amyloid (found inside Macrophages) h. Morphologic features of Amyloidoses Amyloid is deposited in the stromal network of the tissues. It increases the size of organs Deposition around blood vessels causes ( lower O2 and block nutrition/nourishment) atrophy (Alzheimer) Blocks blood supply to the cells Intoxicate cells; Death of cells i. Clinical features of Amyloidoses Kidney MM, Chronic inflammation, FMF complicated with nephrotic syndrome may have Amyloidosis It progresses to renal failure Heart Amyloidoses causes restrictive cardiomyopathy, arrhythmia, sudden death ◊ Heart doesn’t fill with blood as well- amyloidosis and hemochromatosis are the most common cause of restrictive myopathy Ganglia, BV, SMC of submucosa – reduces motility and absorption Constipation, diarrhea, malabsorption Enlarged tongue - dysphagia, dysarthria GI