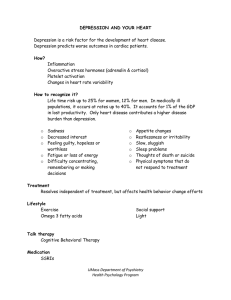
Depression The common features of all the depressive disorders are the presence of: sadness, despair, emptiness Anhedonia (loss of the ability to experience any pleasure) Low self-esteem Apathy, low motivation, and social withdrawal Excessive emotional sensitivity Negative, pessimistic thinking Irritability Suicidal ideas accompanied by somatic and cognitive changes that significantly affect the individual’s capacity to function. Issues of duration, timing, or presumed etiology differ among them. Psychological Symptoms of Depression Appetite disturbance – decreased or increased, with accompanying weight loss or gain Fatigue Decreased sex drive Restlessness, agitation, or psychomotor retardation Diurnal variations in mood – usually feeling worse in the morning Impaired concentration and forgetfulness Pronounced anhedonia – total loss of the ability to experience pleasure Sleep disturbance – early morning awakening, frequent awakenings throughout the night; occasionally hypersomnia (excessive sleeping). Note that initial insomnia (difficulty falling asleep) may be seen as depression, but it is not diagnostic of a major depressive disorder. Initial insomnia can be seen in anyone experiencing stress in general. Initial insomnia alone is more characteristic of anxiety disorders than of depression. Facts... Lifetime prevalence for depressive disorders is 17% Suicide rate for patients with major depression is 9% 18 million people per year suffer from major depression in the US; another 7.5 million experience chronic low-grade depression The incident of depression ratio of women to men is 2:1 Only 50% of Americans who suffer a bout of major depression will seek treatment; yet treatment can be effective in up to 80% of depressed clients – even those suffering with very severe depressions. For the most part, antidepressants are categorized into 6 main groups: 1. Tricyclic 2. Selective serotonin reuptake inhibitors (SSRIs). 3. Monoamine oxidase inhibitors 4. Serotonin and norepinephrine reuptake inhibitors (SNRIs). 5. Norepinephrine reuptake inhibitors (NRIs). 6. Atypical Choosing an antidepression 1. Symptomatic presentation may point toward preferred first-line medication choices. If main symptoms are: anxiety agitation, obsession symptoms, rumination, irritability aggression, and/or pronounced suicidality - serotonin reuptake inhibitors are the first-line treatment strategy. If main symptoms are: apathy, low energy, anhedonia, and/or low motivation dopamine or noradrenergic reuptake inhibitors are preferred (bupropion). 2. Second major factor in choosing an antidepressant is the side effect profile. Even slight side effect often leads to noncompliance. 3 phases: acute treatment- begins with first dose and extends until the patient is asymptomatic (in good case this may be from 6-8 weeks but often takes longer) continuation treatment- to avoid acute relapse, it is strongly suggested that patient continues treatment for a minimum of six months beyond the acute phase. Also, maintain on the same dose used during the acute phase. Maintenance treatment- relapse prevention is an important aspect of treatment, especially once with recurrent episodes (70-80% will experience chronic or recurrent episodic depression). Continued (lifelong)treatment provide the best outcome for such individuals. It experience some additional episodes (albeit, with decreased frequency and severity). The following guidelines are offered: 1. First episode: at the end of the continuation phase, gradually reduce the dose (over a period of 4-6 weeks to avoid acute discontinuation withdrawal symptoms) and assuming to return of depressive symptoms, discontinue. Talk to the patient any signs of recurrence to contact. 2. Second episode: a. With “risk factors” which include family history of mood disorder, first episode occurring prior to the age of 18, and/or most recent episode has severe symptoms: recommend life-long medication treatment to prevent recurrence. 3. Third or later episode: recommend life-long medication treatment. Increase in dose can be made if there is a failure to show a positive response after 4-5 weeks. If the patient had first episode prior to the age of 18, is experiencing a recurrent episode, and/or has been depressed for more than two months, this often requires 4-6 weeks to show first signs of a clinical response. Take age into consideration with dosage.