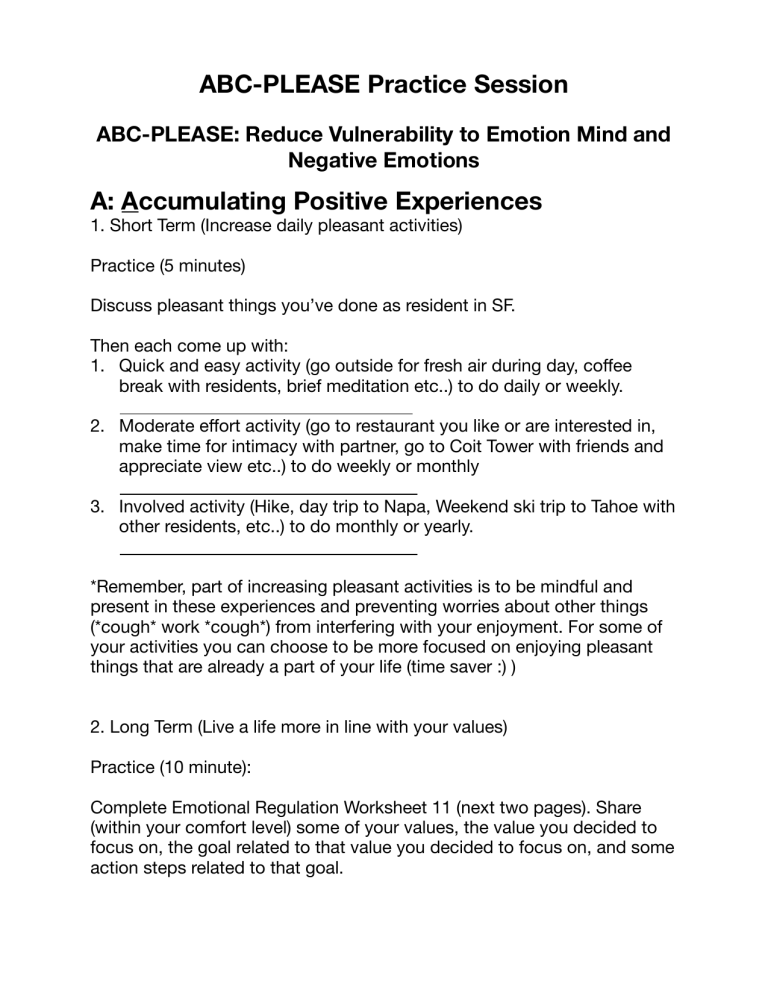
ABC-PLEASE Practice Session ABC-PLEASE: Reduce Vulnerability to Emotion Mind and Negative Emotions A: Accumulating Positive Experiences 1. Short Term (Increase daily pleasant activities) Practice (5 minutes) Discuss pleasant things you’ve done as resident in SF. Then each come up with: 1. Quick and easy activity (go outside for fresh air during day, co ee break with residents, brief meditation etc..) to do daily or weekly. 2. Moderate e ort activity (go to restaurant you like or are interested in, make time for intimacy with partner, go to Coit Tower with friends and appreciate view etc..) to do weekly or monthly 3. Involved activity (Hike, day trip to Napa, Weekend ski trip to Tahoe with other residents, etc..) to do monthly or yearly. *Remember, part of increasing pleasant activities is to be mindful and present in these experiences and preventing worries about other things (*cough* work *cough*) from interfering with your enjoyment. For some of your activities you can choose to be more focused on enjoying pleasant things that are already a part of your life (time saver :) ) 2. Long Term (Live a life more in line with your values) Practice (10 minute): ff ff Complete Emotional Regulation Worksheet 11 (next two pages). Share (within your comfort level) some of your values, the value you decided to focus on, the goal related to that value you decided to focus on, and some action steps related to that goal. B: Building Mastery 3. Have something in your life that challenges you and provides opportunity for growth, mastery, and sense of accomplishment. Increases feelings of control, competence, self-con dence. You want it to be di cult but possible. Examples: learn/practice another language, a musical instrument, yoga/ sur ng, learn something outside of psychiatry (history, philosophy, computer engineering), read great literature Practice (5 min): Discuss things in your life (not psychiatry/medicine/science!) that may give you this opportunity. What is something you have been interested in learning or getting better at? Commit to providing space to do this thing at least weekly (or a smaller portion of time daily if possible). I will provide at least an hour this week for C: Coping Ahead 4. Prepare/plan for possible future stressful event. Mentally rehearse being in the situation and coping e ectively. Practice while you are in wise mind. Example stressful events in residency: First LPPI call with 11 consults, Monday morning on inpatient with 3 new patients, Having upcoming SWIP with no progress made on your scholarly project, meeting with Weston about your QI project and you still aren’t completely sure what QI stands for, acute patient tells you they are suicidal in outpatient visit, wake up Monday to 10 MyChart messages with various requests, 5:05 7L admit, 3am nursing page about miralax PRN (patient is asleep and has not complained of any constipation) Practice (8 min): ffi fi ff fi Come up with a stressful experience (or choose one above) and mentally rehearse to yourself. Discuss your experiences afterwards and what was helpful (or not). Your situation: PLEASE: Take care of your body to take care of your mind PL: Treat Physical ILlness 5. Address chronic illness, (back pain, carpal tunnel, STIs, migraines for instance). Take prescribed medicines. Keep up with routine medical care (have a PCP, get twice yearly dental cleanings). Practice (5 min): Discuss what gets in the way of treating physical illness in residency and strategize ways to overcome them. Commit to doing one thing in next few days to work towards dealing with illness or medical care. Write it down (only share what it is if you want) I will l E: Balanced Eating (and hydrating Enough!) 6. Both binging and excessive dieting are associated with dysphoria, emotionality (hangry anyone?) and distraction. Some ‘unhealthy’ foods (chocolate, cheese, steak etc..) can be bene cial in moderation, and contribute to negative emotions when beyond that. Increasing green vegetables can be an e ective start to healthier eating. Don’t forget hydration as well (get a water bottle?) Practice (5 min): Discuss foods that make you feel happy, calm, or energized. Are there foods that make you crash in a few hours? What are the di culties of eating healthy in residency (i.e. limited healthy options in our cafeteria, the di culty of cooking for ourselves given how busy we are, the feeling of ‘starving’ at the end of a long workday followed by inhaling the nearest comfort food we can get, stress eating etc…). One thing you could do this week to have more balanced eating: ffi fi ff ffi l A: Avoid Mood-Altering Substances 7. Alcohol, marijuana, and other mood-altering substances lower your resistance to negative moods. Use in moderation if at all. Ca eine is a hidden anxiogenic that can also lead to crashes hours later. Be mindful of how alcohol and marijuana may e ect your mood. Imagine the patient(s) you have that struggles to admit the negative e ects of these substances on their mood. Having insight into this is di cult. Is there a trusted friend whose opinion you can elicit? Practice (5 min): Discuss the role of ca eine in your lives now or in the past. How does it make you feel? Do you crash later in the day? Do you notice increased anxiety? Have you been increasing your intake over time? Do you get withdrawal headaches? Go over the substance use disorder criteria using CAFFEINE for yourself as the example. If you don’t use ca eine, what about non-substances like Net ix or video games? Circle the severity (or not). 1. 2. 3. Taking the substance in larger amounts or for longer than you're meant to Wanting to cut down or stop using the substance but not managing to Spending a lot of time getting, using, or recovering from use of the substance 4. Cravings and urges to use the substance 5. Not managing to do what you should at work, home, or school because of substance use 6. Continuing to use, even when it causes problems in relationships 7. Giving up important social, occupational, or recreational activities because of substance use 8. Using substances again and again, even when it puts you in danger 9. Continuing to use, even when you know you have a physical or psychological problem that could have been caused or made worse by the substance 10. Needing more of the substance to get the effect you want (tolerance) 11. Development of withdrawal symptoms, which can be relieved by taking more of the substance . ) . . . ff ff . ffi ff . ff ff . . . . . fl Circle One: None (0-1 criteria), Mild (2-3), Moderate (4-5), Severe (6+ S: Balanced Sleep 8. We know the importance of sleep and the value of sleep hygiene. Do we follow our own advice? Practice (5 min): Discuss the amount of sleep people feel leaves them rested. Have you been able to manage to get this during residency? What gets in the way (reading the news on your phone in bed, Instagram scrolling mindlessly, ruminating about a patient, erratic hours, young child, addicted to moonlighting in PES or the money that comes from it?). How do you deal with sleep with overnight call? What has been e ective or not so e ective? Any sleep hygiene tips have you tried yourself and found helpful? Sleep hygiene tip I will work on starting tonight: l E: Exercise 9. Goal used in most studies is 4-7 days/week of aerobic exercise, at least 20 minutes long. This can be a very e ective antidepressant and reduce anxiety. In addition it can help with chronic pain (PL) and provide an opportunity to Build Mastery. Practice (5 min): Discuss ways to make consistent exercise a part of your routine. What has been successful? What hasn’t worked? What do you enjoy doing? Anyone need an exercise buddy? l ff ff ff Small step to increasing exercise I will do this week: