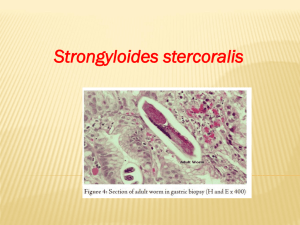
STRONGYLOIDIASIS Strongyloides stercoralis Stool specimen Tissue specimen STRONGYLOIDIASIS 1. 2. 3. Strongyloidiasis in humans is caused by Strongyloides stercoralis a nematode of Superfamily- Rhabdiasoide Common in Asia, Africa Tropical & template areas. Transmission- Filariform larvae through skin penetration – Interaction with contaminated soil or water – The disease is most prevalent in areas of poor sanitation such as those which have poor sewage disposal sites. – Strongyloides is classified as a soil-transmitted helminth. This means that the primary mode of infection is through contact with soil that is contaminated with free-living larvae. Morphology and Life cycle Strongyloidiasis occurs in three phases: a) invasive, b) pulmonary, c) and intestinal. • Filariform larvae that penetrate the skin cause itching at the entry site. • Slight hemorrhage and swelling may appear • bacteria may get into the site, • inflammtion is likely. Morphology & Life cycle •Adults of Strongyloides stercoralis may be found in the human host or soil. • In the human host there are no parasitic males. •Parasitic females are long, slender 2.03.0 mm in length. •In the environment, rhabditoid larvae may develop into • infective filariform (larvae (direct cycle) or •free-living adults that contain both males and females •(indirect cycle)--Can produce freeliving rhabditoid larvae Adult free-living female Adult free-living female S. stercoralis alongside a smaller rhabditoid larva. Notice the developing eggs in the adult female. • Background • Strongyloidiasis is an intestinal infection caused by 2 species of the parasitic nematode Strongyloides. • The most common and clinically important pathogenic species in humans is S stercoralis (see the following image). S fuelleborni is found sporadically in Africa and Papua New Guinea. • Distinctive characteristics of this parasite are its ability to persist and replicate within a host for decades while producing minimal or no symptoms (individuals with an intact immune system) and its potential to cause life-threatening infection • (hyperinfection syndrome, disseminated strongyloidiasis) in an immunocompromised host (60-85% mortality rate).[1, 2, 3] • Rhabditiform larva of Strongyloides stercoralis in stool specimen (wet mount stained with iodine). The symptoms related to strongyloidiasis may reflect the Strongyloidiasis • (hyperinfection syndrome, disseminated strongyloidiasis) in an immunocompromised host (60-85% mortality rate).[1, 2, 3] • Rhabditiform larva of Strongyloides stercoralis in stool specimen (wet mount stained with iodine). The symptoms related to strongyloidiasis may reflect the nematode's systemic passage, its local cutaneous involvement, or both. During chronic uncomplicated infections, the larvae may migrate to the skin, where they can cause cutaneous strongyloidiasis, known as larva currens because of the quick migratory rate of the larva. Infection is clinically characterized by watery diarrhea, abdominal cramping, and urticarial rash. In malnourished children, strongyloidiasis remains an important cause of chronic diarrhea, cachexia, and failure to thrive. Strongyloidiasis • This condition can also be a health consequence of captivity. During the World War II, allied military personnel held by the Japanese experienced deprivation, malnutrition, and exposure to tropical diseases.[4] Certain tropical diseases have persisted in these survivors, notably infections with S stercoralis, with studies 30 years or more after release documenting overall infection rates of 15%. Chronic strongyloidiasis may produce a linear urticarial larva currens rash, with such individuals at risk of fatal hyperinfection if immunity is suppressed. • Patient Education • Travelers to endemic areas should wear footwear when walking on the beach and other areas with soil. Community education in endemic areas should include sewage management, avoidance of soil contaminated with feces or use of feces for fertilizer, wearing of protective clothing when handling sewage or contaminated soil, and wearing of shoes while outdoors. Strongyloidiasis • Strongyloides is classified as a soil-transmitted helminth. This means that the primary mode of infection is through contact with soil that is contaminated with free-living larvae. • When the larvae come in contact with skin, they are able to penetrate it and migrate through the body, eventually finding their way to the small intestine where they burrow and lay their eggs. • Unlike other soil-transmitted helminths such as hookworm and whipworm whose eggs do not hatch until they are in the environment, the eggs of Strongyloides hatch into larvae in the intestine. • Most of these larvae will be excreted in the stool, but some of the larvae may molt and immediately re-infect the host either by burrowing into the intestinal wall, or by penetrating the perianal skin. • This characteristic of Strongyloides is termed auto-infection. The significance of auto-infection is that unless treated for Strongyloides, persons may remain infected throughout their lifetime.