Neuro Exam Notes: Brain Anatomy, Function, and Assessment
advertisement

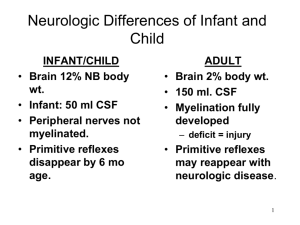
Exam 3 notes slide - Neuroglial function alteration slide-CNS – Brain and spinal cord – outside layer ( dura mater(between the cerebral hemispheres and the cerebellum is the Tentorium( protect the layer of the brain when trauma occurs – balance the two hemisphere)), subdural space, and arachnoid – most inner layer Pia mater is the subarachnoid space ( CSF location) – epidural space outer layer of the dura mater. Reference to a tumor: o Supratentorial – tumor above the tentorium – monitor decorticate positioning - is seen with interruption in the corticospinal pathway. This finding is abnormal and is a sign that the client’s condition has deteriorated. o e charge o nurse, and other health care team members should be notified immediately of this change in status. Decerebrate o posturing consists of external rotation and extension of the extremities. o Hyperreflexes present as increased reflex responses. o Infratentorial – tumor below the tentorium Brain division of the cerebral cortex o cerebrum- for balance o Frontal motor strip ot cortex( mobility) broca’s speech center on the dominant side – speech but not comprehend voluntary eye movement, sensory perception, past information ; experience, affective response of the situation behavior regulation, cognition, judgment, reasoning, concertation o o abstraction. Personality change. Temporal lobe Auditory center for sound interpretation complicated memory patterns Wernicke area for language comprehension – pt understand but cannot speak. the processing of words into coherent thought as well as the understanding of written or spoken words. The temporal lobe also is responsible for the auditory center’s interpretation of sound and complicated memory patterns. any complication – can cause - . Memory loss, Difficulty with sound interpretation, Speech difficulties Right-sided paralysis indicates a left-brain stroke, which will lead to difficulty with comprehension and use of language. parietal lobe sensory input – texture, size, shape, spatial three-dimensional ( Spatial) perception – singing, playing musical instruments, and processing nonverbal visual experiences perception of body part and position aweraness taste impulses for interpretation. - Impaired taste o occipital lobe primary for vision Brainstem function Medulla o cardiac -slowing center o respiratory center o cranial nerve nuclei XV glossopharyngeal, X vegus, XI ( accessory) XII(hypoglossal), and parts of cranial nerves VII (facial) and VIII ( vestibulocochlear)- Damage to these nerves causes-impaired swallowing, inability to shrug shoulders, and loss of the gag reflex. pons o cardiac acceleration and vasoconstriction centers o neurotoxic center the helps control raspatory ( pattern and rate ) o cranial nerve nuclei ( V trigeminal, VI (abducens) VII( facial, and VIII ( vestibulocochlear) Midbrain o contains the cerebral aqueduct, of aqueduct of Silvius o location of periaqueductal gray, which may abolish pain when stimulated o cranial nerve nuclei III ( oculomotor) and IV (trochlear) the cercle of Willis – joint together the posterior and the anterior by small communicating arteries from the ring base of the brain. I -Olfactory - small II- Optic- vision III- Oculomotor- motor eye muscle – lateral rectus and inferior and superior rectus muscle – lip elevation via the elevator muscle = PNS ( feed and Breed) IV- trachea V- trigeminal VI- abducens VII- facial VIII – vestibulocochlear IX- glossopharyngeal X- Vagus XI- spinal accessories XII hypoglossal Blood supply Diagnosis assessment the brain receives 750 ml/min or 15 to 20% of cardiac output can ony used sugar for energy – ( it takes 5 min for the brain to have irreversible brain damage) -the brain need O2 – no med goes to the brain blood- brain barrier – molecules must be enter the brain by active transportendocytosis, exocytosis, creating highly selective barrier the guards the neurons CSF – analysis -colorless, clear, no blood or bacterial, white cells (0-5 – glucoses 40-80 mg protein (1645mg Computed tomography (CT): Uses a narrow X-ray beam to scan the body part in successive layers Positron emission tomography (PET): A nuclear imaging technique that produces images of actual organ functioning Single photon emission computed tomography (SPECT): Uses radionuclides and instruments to detect single photons, and captures a moment of cerebral blood flow - Caffeine-containing liquids and foods are central nervous system stimulants and may alter the test results. No contrast is used; therefore, the client does not need to increase fluid intake. The client should take cardiac medications as prescribed. Magnetic resonance imaging (MRI): Uses a magnetic field to obtain images of different areas of the body- Allergies to iodine and/or shellfish need to be explored because the client may have a similar reaction to the dye used in the procedure. In some cases, the client may need to be medicated with antihistamines or steroids before the test is given.- Metal devices such as internal pumps, pacemakers, and prostheses interfere with the accuracy of the image and can become displaced by the magnetic force generated by an MRI procedure Cerebral angiography: An x-ray study of the cerebral circulation - it is a high risk monitor Vs every 15 to 30 for 2 hr- 1 hr for 6 hr – 2 hr for 24 Myelogram: An X-ray of the spinal subarachnoid space Noninvasive carotid flow studies: Use ultrasound to evaluate carotid and deep orbital circulation Electroencephalogram (EEG): Represents a record of the electrical activity generated in the brain- Hyperventilation produces cerebral vasoconstriction and alkalosis, which increases the likelihood of seizure activity. The client is asked to breathe deeply 20 to 30 times for 3 minutes. ◦ Avoid caffeine on day of test ◦ Wash hair, but no sprays or oils after shampoo accurate. Electromyogram (EMG): Uses needle electrodes to measure changes in the electrical potential of the muscles and the nerves leading to them Lumbar puncture (spinal tap): Carried out to withdraw CSF- insertion of the needle between the subarachnoid space between the L3 and L4 , and sometimes L4-L5 – still position proper positioning for Lumbar puncture – fetal side-lying position to separate the vertebrae and move the spinal nerve roots away from the area to be accessed. – local anesthesia – slight pressure after the procedure assess the site for CSF leak and infection - An LP should not be performed if the client has a skin infection at or near the puncture site because of the risk of infection monitor VS, Headache, ------increased fluid intake – report and HA to HCP if medication does not relieve pain. - d immediately contact the provider if the client experiences a severe headache, nausea, vomiting, photophobia, or a change in level of consciousness after an LP, which are all signs of increased intracranial pressure. rest----may position fat – bed rest and maintain flat cheek neurological status o complication > ICP cause by ( severe HA, nausea, vomiting, photophobia, and change in LOC o serious complications – brain hernation formation, infection, CSF leakage hematoma formation Altered cerebral function o Manifestation of altered cerebral function occur as a result of illness or injury Loc may be altered by the process that affect the arousal function of the brainstem, the cognitive function of the cerebral hemisphere or both- Loc is a primary indicator of Neuro PB – if lethargic – cannot answer – call HCP – request for CT scan Glasgow coma Scale ***** 15-13 – mild impairment 12-9- moderate impairment loss of consciousness greater than 30 minutes physical and cognitive impairment with or may not resolve benefit from rehabilitation 3-8- sever impairment- candidate for organ doner -cannot be less than 3 coma, unconscious state; no meaningful response, no voluntary activities best response to eyes opening **** 1- no eye opening 2- eye opening to pain 3- eye opening to verbal commands 4- eyes open spontaneously vegetative state ( less than 3) sleep wake cycles Arousal, but no interaction with environment – the 1 sign of anything going wrong is change LOC damage to RAS impairs the ability to maintain wakefulness and arousal- action suppressed at the brainstem – which proceeds edema and ischemia – may be due to tumors, hematomas or hemorrhaged oe aneurysm no location response to pain Patterns of breathing are impaired as the respiratory center becomes compressed Diencephalon: Cheyne-stokes respiration – getting worse Midbrain- neurogenic hyperventilation uninhibited stimulation of the respiratory centers – breathing a lot pons- apneustic respirations, characterized by sighing on mild inspiration or prolonged inhalation and exhalation ( excessive stimulation of the respiratory center) medulla ---Ataxic/apna respirations (total uncoordinated and irregular probably as a result of loss of responsiveness to CO2 – COPD- unresponsiveness to CO2 they cannot take too much O2 thay can stop breathing Diabetes insipidus – deficiency in production of ADH cause by organic lesion of damage to hypothalamus – and decrease renal response the ADH – cause increase in urination > 800 ml/HR and increased in plasma osmolarity _ > dehydration o Sx with DI o increased in quantities of the urine with very loe specific gravity occurs suddenly after the heat injury, CNS infection or tumoe\r Tx hormone of ADH or fluid replacement ( hypotonic saline is given), DDAVP-demoopressin acetate ( po, IV, nasal spray) best for DI – hope that it will solve the PB N/I > fluid intake and give DDAVP – accurate I/O o Pupillary responses – as LOC deteriorates, a predictable progression of pupillary response occurs, o if the lesion localized – the affects may be seeing in the same side – ipsilateral purpil)- if generalized the p=pupils is affect equally. with compression of CN III the pupil may change shape or off =center -is responsible for dilated ad constriction of the pupils – assess when shining light to the eye as impairment continuous it become fixed ( nonreactive) and dilated – brain damage ( poor prognostic sign, patient with his problem are sometimes referred to as having a “Blown “pupils as neuro condition further deteriorates, the eye movement is lost, and the ocular reflexes are altered Locked -in syndrome – different from vegetable state in the client is alert and fully aware of the environment – unable to communicated through speech or movement because of blocked efferent pathways from the brain – motor paralysis affects all voluntary muscle. presence of restlessness and confusion more combative Doll’e eyes -your eye go to another direction – route through brain damage o o o cannot done on the pt with possible cervical trauma, until it rules out the procedure is performed by holding the pt eyes open briskly and turn side by side if the reflex is u=intake the eye will turn the opposite side from with the eye is turned it the reflexes is absent 1- remain in the midline or move with the head – this brainstem injury o 2- eyes move to opposite direction from one another – some degree of brain stem injury Nystagmus – an involuntary condition in which the eyes make repetitive uncontrolled movements. to a big deviation of the eyes – Is associated with specific lesion or chemical intoxication – don’t know affect ICP if both reflex lost brain function as deteriorated Coma and brain death. o o o irreversible coma-(vegetative state)-permanent state of complete unawareness result from death of the cerebral hemispheres- with continued function of the brainstem and cerebellum Usually, the result of severe head injuries and anoxia myasthenia gravis/ ALS Brain death o cessation and irreversible of all brain function, including the brainstem neurologic tests are not required to confirm brain death in some state or province example test are – cerebral angiography, EEG, CTA, transcramial Doppler ultrasonography o criteria way from state to state but generally recognized criteria are: unresponsiveness coma – no reflex movement no spontaneous movement ( apnea test) pupils fixed and dilated -potential brain death absent of ocular movement and cold calories Flat EEG negative brain flow study o nursing management – ineffective airway clearance, risk for aspiration o loss of cough and gag reflexes 1. assess ability to clear secretion – don’t stop taking care 2. monitor breathing sound 3. period suctioning --- maintain open airway – suction – if not able to breath – put o2 on 4. turn side to side every 2 hr with HOB at 30 degree – help to grain fluid o impaired skin integrity r/t mobility assess skin evry shift reposition every 2 hr prevent skin breakdown ( bathe daily. keep linens, clean and free wrinkle free, good mouth care keep cornea moist- Avascular – used tape gently o impaired physical mobility o maintain extremities in function position by providing adequate support devices o Use of splints. pillows, rolled wash cloths, ROM drug therapy – o Mannitol, an osmotic diuretic – used to treat cerebral edema by pulling Ho2 from the brain – more effective when given bolus – give it with Iv filter to eliminate microscopic crystals strict o output Avery 1 hr – serum osmolarity 310 to 320 goal every day. risk for dehydration acute renal failure weakness, edema, and change in urine output. furosemide – incidence from rebound from mannitol – enhance therapeutic and reduce edema and blood volume- < sodium intake at the brain- < the production of csf from choroid plexus. Increased intracranial pressured ( IICP) o o o defined the rise in pressure of CSF between skull and brain ----15 mmhg ( normal 0=15 mmHg) significant increased called intracranial hypertension causes – neoplasms, cerebral edema, trauma, infraction, infection, abscess, hemorrhage, hematoma, increased CSF , decreased absorption IICP pathology ( insult to brain, tissue edema, > ICP, compression of the ventricle, compression of the blood vessels, decreased cerebral blood flow, decreased O2, edema around the necrotic tissue, increased in ICP with compression of brain and the respiratory center, accumulation of CO2, vasodilation, increased in ICP resulting from increase blood volume. death. o o o o o o o o o o o o o o o o monro-kelli hypothesis –volume of one component ( tissue, blood, CSF > voulume of another cerebral blood flow normal 750ml/minute – brain tissue 78% blood 12% maximum compensation -----then ICP increased - elevate BP influence ( HTN) hypercarbia ---PaCO2 > 45 mmHg = vasodilation with increased volume => ICP hypercarbia ---PaCO2 <25 mmHg = rebound cerebral vasodilation and loss of autoregulation ( ability to keep constant blood flow to brain) normal cerebral perfusion pressure (CPP) 60-100mmGh --- determine CSF CPP> 100mmHg = hyper perfusion and high> hCP CPP< 60 mmHg = hypoperfusion / cerebral Ischemia ( irreversible/ infraction <40mmHg) CPP -40 mmHg = brain death compensatory mechanisms kick in with increase in ICP balance / protect brain CSF changes via shunting into subarachnoid space to reduce pressure decreased secretion / increased absorption of CSF. failure to compensate mechanism = hypoxia, ischemia- herniation, brain death when ICP nears systemic arterial [pressure CPP CBF decreased when ICP is equal systemic arterial pressure stop --- brain death occurs impact of elevated on circulation determined by CPP with mean arterial pressure (MAP) the prime influence. Manifestation of IICP o o change in Loc is most reliable indication for IICP – as pressure increased, decrease in LOC rt to impairment of circulatory blood flow earliest sign – blurred vision ( diplopia), severe headache, papilledema/ swelling of optic disk, and projectile vomiting – then dilated or pinpoint pupils – Cheyenne stokes raspatory, decerebration, decorticate flaccid – late sign Cushing triad ( wide pulse pressure, bradycardia , irregular respiration, later tamp change) o change in motor ability, as contralateral ( opposite side of the mass lesion hemiparesis hemiplegia may develop – pain stimuli 5/6 motor response withdrawal 4/6 Alteration brain activity definitions seizure-uncontrolled discharge of neurons in cerebral cortex, interfere with normal function epilepsy-recurrent paroxysmal – cerebral function – sudden short attack – alter in consciousness motor and sensory phenomena Type of seizure si precipitated factors o o o o o o seizure -physical exhaustion -sound odors, fever, sleep deprivation, malnutrition, stress, ETOH, shock, drug bacterial meningitisviral meningitis encephalitis brain abscess herniated intervertebral Stroke – brain attack or CVA o Type of stroke Hemorrhagic stroke o TIA- brief interruption in the cerebral or inadequate blood flow to a part of the brain o o Thrombotic Embolic Risk factor of stroke o hypertension o metabolic syndrome o Heart disease o heavy alcohol consumption o poor diet- diabetes o drug abuse o o o o sleep apnea obesity physical inactivity smoking blood supplies to the brain Internal carotid arteries o frontal lobe o Parietal lobe o temporal lobe CNS neoplasms brain tumor primary originated in the brain secondary – original in other place then the brain due to metastatic 65 % id gliomas -originates in the astrocytes- the most common glioblastoma multiforme – very malignant and invasive Sx/S headache- more in the norming nausea vomiting – cognitive pb- memory -sign of brain- frontal lobe– personality change and judgment seizure seizure mood and personality change sensory loss. increased ICP specific SX – frontal ( seizure) cognitive pb- memory personality change and judgment parietal speech disruption writing struggle spatial disorder occipital seizure blindness temporal - dysphagia seizure cerebellar- headache, papilledema, > ICP, ataxic, gait, vertigo, tinnitus, deafness Tumor in the pituitary transsphenoidal ( hypophysectomy) -upper lip and gingiva are cut and access is obtained through the floor of the nose and sphenoid sinuses nursing care- neuro check per order – check nasal for sign of CSF halo in the white gauze. instruct the pt do not blow the nose ot brush the teeth. Tx hormone replacement – vasopressin dacaton) ti < icp- dilantin antiemertic dx histologic study and endocrine study. will be indicated Spinal cord tumors most common cause Motor vehicle collisions (MVC) 42%, fall, violence, sport injury. and miscellaneous 8 % o falling object, diving, sking,boating, football, penetrating trauma ( gunshot, stabling) o LMN – lower motor neurons- skeletal muscle of the eyes, mouth, throat – segment of the brain – any lesion – weekends paralysis, denervation , atrophy hyporeflexia, or areflexia – decrease muscle tone ( flaccidity )0,1 o UMNs (upper motor neurons) – from the cerebral cortex downward – increased muscle tone( spasticity) – irritation restlessness, agitation, tachypnea, bradycardia, oliguria, diarrhea, borborygmi. reflexes 3, 4 o Basal ganglia – both cerebral – control and vacillated learned of automatic movement risk factors – age gender, and alcohol or drug use ( young male ( 18-30) most common is cervical, least thoracic. paraplegia – lower extremities ( T1-S5) tetraplegia – paralysis in arms, legs trunk, pelvis- injury of the C-spine- total sensory loss C7 Spinal shock o decrease reflexes-0,1 o sensory loss o flaccid below the injury site o bowel and bladder dysfunction o loss of sensation of pain, touch temperature, below the level of the injury. o begin immediately after the complete transection of the cord – connection between the brain and the cord in interrupted. o last day and month – then reflex activity returns. Neurogenic shock – c-spine from C7 higher plan on ventilation support – BP<80 HR<40 everythings slow down. more cervical assess for respiration statute o o o Shock cause by > PNS or parasympathetic stimulation or inhibit SNS or sympathetic stimulation of muscle of the blood vessels. loss of vasomotor tone vasodilation, hypotension, bradycardia, warm and dry extremities, < CO Autonomic dysreflexia – occurs in T6 and higher injury – seen after the spinal shock when the stimulus cannot ascend the spinal cord. o o o o is an exaggeration sympathetic response when this happened – massive vasoconstriction above the injury and vasodilation below the injury fecal impaction – constipation – stool softener all the time symptoms – early-sx SCI- back pain that worsen with activity. bounding headache- check BP bradycardia hypertension flushed warm skin with perfusion sweating above the lesion and pale cold dry skin below ( skin Flushed, worm and wait above the injury and cold and dry below the injury). Dilation above the eight - sitting for the blood to go dependent. complication SCI stress ulcer paralytic ileus ( constipation) decubitus – stage stool impaction decreased venous return fracture r/t bone demyelination joint contracture – PT, OT Nursing care c-spine C7 – ABC Brown-Sequard syndrome – complete motor and sensory loss below C7 ( ipsilateral and contralateral) monitor LOC – maintain the head in the neutral position – sbrserve spontaneous movement compare data – more breathing assess foe sexual activity – women can still have sex suction carefully to avoid vagus nerve stimulation – bradycardia cardiac arrest. percussion and chest PT for weak cough breathing exercise hydrate/ humidity to thin secretion fecal impaction ( autonomic dysreflexia) rise HOB / removed compression hose to decrease venous return and BP report any deterioration ASP neuro monitoring – 1 hour ROM – 2hr UAP PT, monitor BP, cv for dysrhythmia assess DVT, emboli maintain skin integrity- massage. barriers cream promote urinary elimination with inter-mitten catherization ( to keep the bladder empty) used the indwelling catheter for acute phase pour arm water in the perineal area, follows all this with catheterization if need it ---<80 residual is acceptable. – no foley catheter promote bowel function with feel tube followed bt residual check offer high calory diet, > protein. > fiber used bowel retrain process – stool softener, rectal suppository, digital stimulation after meals. halo brace care – infection prevention by shaving hair. around pins – clean with ½ H2O2 and 1/2NaCL. topical ABOs, Diagnostic test spine Xrays myelogram CT scan CBC, lytes, ABCs, glucose H&h, UA,EMG MEDs – stool softener, H2 antagonist - or antacids. low dose anticoagulant, corticosteroid NSAID antispasmodics, antidepressant, topical ABOs prn Seizure- resulting from metabolic disturbances - clinical manifestation Simple partial seizure – consciousness – motor sx, one part of the body- sensory symptoms tingling numbness, visual, auditory, hearing, taste =- vertigo spells Complex partial seizure – repetitive movement like lips smacking antisocialist/ aggressive behavior - - - - characteristic psychomotor seizure with repetition beaver and lips smacking altered memory, sexual sensations and disorder of visual or auditory sensations often involves behavioral, emotional and cognitive behavior that altered LOC Absent seizure( petite mal) – short period – 5-30 secs up tp 100days -eye fluttering, lips smacking – more in children ( typical absence seizure staring spell, daydreaming that last a few minutes and unnoticed ) if untreated it can go 100 time a day.atypical – staring spell accompanied by the s/sx brief warnings, peculiar behavior during seizures and confusion after seizure more longer. Generalizes seizure – or grand- mal seizure is a bilateral synchronous epileptic discharge affecting the whole brain at the onset seizure – tonic-clonic, tonic, absence, myoclonic(single jark just for a second) cause by sudden abnormal bursts of electrical brain activity tonic-clonic – grand mal – most common type ( stiffness-jerking( eye roll ) – postictal phase ( unconscious and unresponsive to stimuli)- relaxed- rapid breathing – sleeping ( let them sleep)***- fatigue – often accompanied by incontinence and tongue biting – breathing ceases 15 s to 1 min during the tonic phase- may be hyperventilated eyes rolling on the colonic phase- cyanosis exercise salivation - atonic seizure (drop attack)– paroxysmal loss of muscle tone and sudden falling on the ground and return of consciousness, - risk of heard injury – often were protective helmets, - Tonic sudden unset of maintained increased tone in the extensor muscles and fall result. - clonic begins with loss LOC and sudden loss of muscle tone. and jerking movement. status epilepticus – ER – continues tonic-clonic cycle- interference with respiration ( hypoxia, hyperthermia, hypoglycemia, exhaustion ( if not stop in 30 minutes can cause brain damage)- tx give adtivant( larasepam)**** or Dilantin ( bolus) and prepare for intubation – more prone to death. they don’t stop seizing – no breathing – give adtivant – O2, be ready to intubate – anesthesia - epileptic – gliosis is a scar tissue around the area of the brain epilepsy occurs – interfere with normal brain neuron function. - the astrocytes may be a key role in recurring of the seizure Nursing intervention for seizure record all the aspect of the seizure note the time in wish the seizure occurs and the duration the event proceeds the seizure the priority intervention is to maintain airway during seizure - promote drainage secretion without aspiration; suction, O2 no oral object in the mouth. no restrain during injury, place padding under the head. - take the pt out of bed, NPO nothing in the mouth, time it, what type of seizure tonic-clonic, medication, notified the hcp protect the pt head for injury and turn the pt on the side, loosen constructive close ease pt on the floor do not restrain the patient do not place any object in the pt mouth. after seizure, reposition the pt and maintain airways suctioning, and oxygen. Focus assessment monitor pupils size reaction, cyanosis, sweating, salivation, LOC, incontinence during surgery monitor time of the seizure and duration activity, movement thrigger Aura monitor poetical period (30-90 min) for confusion sleepiness, arousal issues, muscle aches, headache, weakness, aphasia, partial paralysis. inpesct foe injury especially the tongue – anything in the mouth. turn to the side to maintain airway meds. dilantin, Depakote, Tegretol, neurotin, klonopin, Lamictal, also valium or phenobarbital status epilepticus. teach ID alert , trigger and support. headaches – intracranial source origin. - type of HA primary cause by disease ( tension, migraine, cluster) - secondary cause by condition or disorder( sinus disorder, neck, injury, stroke hemorrhagic ). Cluster- it is a most sever and repeated HA that occurs for months a at time following the period of remission. – abrupt onset usually, 2-3 hours after falling as sleep in spring or fall-cause by trigeminal(tic douloureux) (CNV) that conduct pain – the imagery shows hypothalamic at the onset of the cluster HA, alcohol the only trigger - it is shaped and stabbing – pain is in around the eye and radiated to the forehead cheek, nose, or gums and swelling around the eyes. may be accompanied by unilateral ptosis or lacrimation. dx – keep a headache diary can be useful. CT and MRI may rule out aneurysm Migraine- unknown cause -recurring and unilateral- steady throbbing pain with synchronous pulse- autonomic more femalerisk factors – education family hx- type common(without aura and classic( aura such as headache for hours or days prodrome ( photophobia, psychologic, hyperactivity, irritability, and food craving )- subjective hyperexcitability. associated with seizure, ischemic stroke, Asthma, depression, anxiety, myocardial infraction Raynaud’s syndrome and irritable bowel syndrome. may last 72 hours. hibernate to color, light, odors, and the presence of people) Aura is neurologic neuro symptoms ( bright light, scotomas( patchy blindness) visual distortion ( zigzag line) weakness, paralysis, feeling of limbs are moving) precedes HA 10 to 30 minutes. diagnosis – pt history CT, MRI drug triptan (sumatriptan) is a specific serotonin agonist that cause vasoconstriction _ pt with heart disease and stroke should avoid it – used for cluster HA Frontal-type(migraine and tension) -the Dx is trough thorough family hx Tension type - Stress HA- bilateral location, pressing and tightening quality(last day and night). episode and chromic – constant dull pressing or bandlike headache associated with neck pain and increased in tone in the cervical and neck muscle. involve in the light and sound photophobia – activity does not aggravated symptoms. dx history assessment most important and electromyogram (EMG) Restless leg syndrome (Willis-Ekbom diseases) – unpleasant sensory ( paresthesia) and motor abnormally on one or both leg – primary (idiopathic)– abnormal iron metabolism secondary- metabolic abnormality r/t iron deficiency, renal failure, polyneuropathy associated with DM, RA, pregnancy. amenia is related to dysfunction in the brain ganglia circuits that used neurotransmitter dopamine, which controls movement.- cause the urge to move the legs clinical manifestations paresthesia, numbness, tingling,subjective- sensation of bugs creeping or crawling on the legs , pain localizes on the cap muscles sleep disturbance- pins and needle sensation to severe pain motor abnormalities voluntary restlessness periodic involuntary movement DX – CBC serum ferritin and renal function test – hx od DM pt, polysomnography studies (apnea) encourage -non drug encourage sleep and exercise more then one drug therapy – Sinemet( cardopa/levodopa), permax, , Neurontin, Depakote, clonidine. dopamine agonist ( ropinirole (requip), Mirapex(pramipexole) benzodiazepine, low dose oxycodone eliminated – aggravating factors – such caffeine, alcohol, certain drugs, ( neuroleptics, lithium, antihistamines, antidepressant) Alzheimers diseases- over production of B amyloid protein o stage 1- healthy and alert, restlessness, forgetful uncoordinated o stage 2 –memory deficits become more apparent, language deficit (wrong word and repetition of words or phrases), lose ability to complete simple tacks. sleep disturbances. depression, sundowning reaction is agitation, disorientation and wandering behaviors in late evening or night. o Stage 3 - increased dependence, inability to communicate, loss of continence and progressive loss of cognitive abilities o 7 years od life expectancy. o dx EEG, MRI, PET, psychometric evaluation ( Folstein mini mental exam) o meds – cholinesterase inhibitor ( mild to moderate) Aricept(donepezil), Exelon(rivastigmine) , razadyne ) > ADL, decreased agitation, and hallucinations o Namenda SR(Mentatine (NMDA) ) – protect brain cells from people that experience decrease in cognitive. o depression med lorazepam (Ativan), risperidone (risperidone), and sertraline (Zoloft) o nursing care – lifeline program. reminder ( alarm clock, pocket computer, simple yes or no question in the early stage 1 o constant reorientation- stage 1 o sundowning is a disruption in circadian rhythms – daylight will help to restablish a more normal circadian pattern Parkison’s disease o basal ganglia – down in initiated and execute movement - > muscle tone, tremor, at rest , impaired pasture reflexes o show degeneration of dopamine – product by substantia nigra the mid brain. Sign start after 80% of the neuro is lost – before you start getting the symptoms o sign - ESP + tremors at rest - onset is gradual and insidious - than mild tremor, a slight limb, decrease arm swing - later sever – short shuffering gait , propulsive gait with arm flex and lost of posture reflexes. rigidity is typical by jerky motion and slowness of movement - o o o o o o o Bradykinesia – loss od autonomic movement such as blinking, swallowing, of salivation, self-expression with facial and hand movement. - stooped posture = blank mask like facial expression, drooling of saliva, and suffering gait- care full when the eat – risk for aspiration. Complication progressive deterioration with the loss of spontaneity movement swallowing difficulty severe debilitation leads to pneumonia UTI and skin breakdown decreased mobility - gait is slow and shuffling - head and trunk and bent forward and legs are constantly flexed Diagnosis is base on solely on hx and clinical features - two/three of tremor, rigidity, bradykinesia ( slowed movement) - positive to response to antiparkinson’s med – is the ultimate confirmation of the disease - dementia 40 % o o o o o o Meds is to correct the imbalance neurotransmitter with the CNS to > dopamine and < cholinergic to brain levodopa – cross the brain- barrier and convert to DA in the basal ganglia levodopa cabidopa ( Sinemet) is the drug od choice) – inhibit enzyme od dopamine in the prereferral and help to enter the brain. o MAO inhibitor selegeline – to control rigidity and bradykinesia movement. o surgery is to provide an arm relive o Ablation surgery tx PD and it replace by deep brain stimulation (DBS) - placing electrode In the thalamus, globus pallidus, or subthalamic connect the generator with upper chest deliver specific electricity to the brain - transplantation of fetal neural tissue into the basal ganglia provides DA in the brain still on experimentation. NI- cut into small size – several small meals provid time to eat levodopa impaired protein _ decreased intake in protein- decreased the abruption of dopamine in the brain. Multiple sclerosis – SNS – everything go Up o chronic -muelin and nerve axon in brain/spinal cord destroyed lead to interruption of the nerve impulse. o plaque formation of the write matter after C,T,L spinal cord cause inflammation and scaring lead to disability. o benign relapse collapse remission – progressive primary and secondary o exacerbated y stress fever, fatigue, pregnancy o o o o o o unknown cause -auto/ genetic. viral manifestation- visual disturbance - sudden progressive weakness- early weakness in the leg start first - spasticity Spasm, tremors, gait inability, - bladder/bowel dysfunction incontinence - depression Diagnosis - lumbar puncture for CSF – clonal IgG bands - > protein > WBC - MRI , CT, Muscle testing hx physical meds - corticosteroids- ACTH, prednisone - immunomodulators glatiramer acetate copaxone, avonex- teach how to draw-up and administer med - immunosuppressant novantrone - prostigmine, Urecholine- cholinergic - Ditropan, damtrium, lioresol- anticholinergic - antibitotics ( UTI) - check the creatine before give fampridine (Ampyra) N/I rest period, prevent fatigue, fluid intake 2000ml /day minimum, promote independence teach the pt for crede method for flaccid bladder. to improve bladder emptying Myasthenia gravis - autoimmune anti body destroyer the cholinergic receptor at the neuromuscular junction - chronic progression of PNS ( everything will go down) r/t to nerve transmission to voluntary muscle = fluctuating weakness, fatigue on exertion and relive with rest. - unknown cause – autoimmune disorder thyroid ( lack of tyrosine kinase- tymus tissue ) - autoantibodies , between receptors =wider gap between axon ending and muscle in neuromuscular junction. - Muscle contraction hindered; receptors dis - the onset is slow; precipitated by stress, hormonal change r/t pregnancy, menses, thyroid disorder, infection, vaccination trauma, surgery, extreme temperature excess, in exercise, meds that bock the neurotransmitter, opioid, sedative, bars, ETOH, - diagnosis test ABCs, PFT EMG, - Tensilon test= IV administration with promote voluntary muscle contraction by allowing acetylcholine to bind with receptors to improve symptoms , weakness, returns after tension effects gone. after injection tension if there is an improve in muscle contraction ( pt has MG) -if the worsening of the Sx the cholinergic crisis and should have atropine ready when testing. - positive test finding confirms diagnosis MG - Manifestations mild diplopia; unilateral ptosis, constricted pupils. muscle weakness of the face, jaw, neck, hip muscle related to chewing, swallowing, respirations serious -are the most serious bowel and bladder incontinence paresthesia pain myasthenic crisis( under medicated) sudden motor weakness, risk for respiratory failure and aspiration. – positive Tensilon test cholinergic crisis (over medicated) sevre mucle weaknes with cramps, diarrhea, bradycardia, bronchial spasm. - nursing care focus maintain airway/effective respiration assess for respiratory infection. monitor meal time bent forward slightly to avoid meal aspiration provide adequate nutrition small frequent meals 30 to 45 mins per meals for peak muscle strength at meals ; IV flds, NG promote mobility = PT, OT , eye care = artificial tears. patch, sunglasses meds=pyridostigmine, Mestinon, steroids, Imuran, Cytoxan, teach to take the med 30 minute prior to meals. educate about rest energy conservation, activity with peak med effects. avoid extremes hot/cold exposure to infection; stress’ meds, that precipitate exacerbation like ETOH, sedative, local anesthetics signs of crisis; med alert ID communication options =flash cards/boards. Amyotrophic lateral sclerosis (ALS)(lou Gehrig’s disease) quinidine/anesthetics and thymus disorders. - destruction of the motor neuron in the brainstem and spinal cord gradually degenerated – motor neurons last with axon degeneration that causes demyelination. lack in transfer signal to the brain. - affected the cranial nerve III, IV, VI - lead to death with 3 to 5 years - cause is unknow – viral, metabolic, trauma, familial. - UMN= spasticity weakness muscle > in reflexes - LMN- muscle atrophy, flaccid paralysis, - loss muscle innervation=muscle atrophy=disease muscle mass= increased fatigue - typical symptoms – limb weakness, dysarthria, and dysphagia - - others sleep disturbance, pain, spasticity, drooling, emotional lability, depression, constipation, and esophageal. - death result from respiratory infection r/t compromise on respiratory function. - no cure riluzole slow the prohression by decreasing the glutamate( excitatory neurotransmitter) in the brain - meds – steroids, ABO’s anticholinesterase (neostigmine), muscle relaxants. - discuss the artificial method of ventilation and advance director. go to be on ventilation - Diagnosis test > CRP and protein in CSF- show muscle damage CT scan Myelography muscle biopsy EMG – for muscle recirculation. nursing focus – airways-O2, suction. vent support PRN, cardiac status VS, Guillain-barre syndrome (GBS) -CN(III, V, VI, VII, X, XII) full recovery is expected paralysis of the ascending to the nerves that stimulated the thoracic area Huntington disease hereditary disorder – autosomal dominant trait at the time of conception – (congenital )- form both men and women. – offspring have 50 % of chance to have movement disorder characterized by both neurologic and behavioral symptoms. - the pathogen of HD is involved in the basal ganglia and extrapyramidal motor system cause deficiency in DA the neurotransmitter Ach and yaminobutyric ( GABA) and in DA ( dopamine) that lead to symptoms opposite with is excess in DA parison’s diseases - tx tetrabenazine (xenazine) to tx chorea and decreased DA at the synapses of the brain. more palliative care - used antibiotic to tx infections and guardianship gradually clinical onset of mental status change, leading to dementia and choreiform (chorea) excursive writhing and twitching movement of the limbs, trunk, and facial muscles( chewing and swallowing -lead to aspiration and malnutrition) gaits and ambulation become impossible due to chorea calory requirement is elevated 4000 to 5000 calories /day to maintain body weightdifficulty to hold the head still as a disease progressed presence of swallowing difficulty. three stage the last 5 years for the total of 15 years. death is possible ( 10 to 20 years of the onset of the problem) due to pneumonia followed by suicide. management no know cause – genetic counseling antipsychotic med such as med for anxiety, depression, Obsessive compulsive behavior monoamine-depleting agents to management the movement abnormalities and disabling or interfere with ADLs. and safety bell’s -CN(VII)- or facial paralysis unilateral paralysis of the facial muscle -Affects the motor branches of the facial nerve. for expression foe one side of the face. the sensory portion innervates the anterior two-thirds of one side of the tongue. unknown cause the onset is sudden is almost involve one side of the face. pain behing the ear and jaw may precede the paralysis. – some cannot blink---may need artificial tears uncreased tearing on the affected side – no lb study or meds ( steroid) Manifestation- numbness ant stiffness on one side of the face facial paralysis causes the entire face to droop- private place when eating pt believe they have stroke because they cannot wrinkle forehead, close the eye or pucker lips on the affected side. precipitation factors herpes simplex virus complete recovery few weeks or months – but permanent paralysis can occurs with older and diabetes pt treatment – corticosteroid, moist heat, gentle massage, electrical stimulation of the nerve – exercise inability to close the eyelid, with an upward movement of the eyeball, when closure is attempted protect eye with sunglass, artificial tearing, tape the eyelid close at night, oral hygiene Trigeminal - CN (V) tic douloureaux- chronic disease that affect more women than men with unknow cause characterized by brief repetition of severe facial pain- over the surface of the skin that often begins near one side of the mouth and continuous ear, eye or nutrition the same side of the face. and subjective as stabbing pain. decrease in pain is the higher priority pain is initiated by many factors -light touch, eating, swallowing, talking, sneezing, shaving, chewing gum, brushing, teeth or washing the face. change in temperature cold and wind can cause pain. more pain in winter Treatment – anticonvulsant –Tegretol, Dilantin (level 10- 20), Neurontin may be used.to decrease paroxysmal afferent impulse and stop pain – SE- dizziness, drowsiness, bone marrow function. monitor the drug surgery intervention- rhizotomy – surgical reserving of the nerve route o glycerol rhizotomy -less danger, less sensory aberration ( pain) o Gamma knife radiosurgery -radiation to reduce pain o microvascular decompression- greater relieve of pain o percutaneous radiofrequency rhizotomy- greater relieve of pain - post-surgery numbness but no residual paralysis – will have loss of facial sensation to temperature and touch nursing care pain management Tegretol o o improving nutrition – refused to eat during period of the attacks. teach to prevent injury and disease process. Tetanus or lockjaw – (SNS) provide by wound contamination tonic spasm or seizure can be prevent by vaccination disorder of the nerve system characterized by neurotoxin clostridium tetani. when the spore of the neurotoxin inters the open wound, they germinated and produce toxin incubation 8-12 days or longer toxin- peripheral nerve- spinal cord- uncontrolled muscle spasm.- make sure the vaccine is up to date ( 10 years) ICU on ventilator Manifestation o Pain at the side ( lockjaw) o stiffness of the jaw and neck’ o dysphagia o profuse perspiration and drooling o hyperreflexia o rigidity and spams on the abdomen neck and back muscle. o general seizure – typical opisthotonos position- head retracted, back arched and feet are extended. o unable to breathe intubation/ ventilator o urinary retention o nursing intervention -promote safety, nutrition, cv pulmonary - place the pt in the dark and quiet to decrease stimulation - maintain oxygenation trough mechanical ventilation. - clean the wound with soap and water only- and keel all bacterial o nursing management - maintain IV access - administrate adequate antibiotics - monitor fluid electrolyte status / UO - teach for immunization – wound care – wash thoroughly with soap and water Botulism food poisoning cause by indigestion of food contaminated with toxin of bacillus clostridium botulinum. – anaerobic and does not need o2 found in the soil can have it by eating uncooked foods- especially home – canned vegetables and fruitd smoked meats, and vacuum-packed fish. manifestation – GI tract bound to nerve tissue blocked the relieve of acetylcholine from nerve endings and cause respiratory paralysis due to the paralyses of skeletal muscle – after 12-6 hours of indigestion. o visual disturbance – diplopia, loss of accommodation and fixed, dilation pupils ( CNIII, VI,IV) o ptosis o Gi N/V/D and dry mouth – cathartics enemas gastric lavage o o o o o paralysis of all muscle of the body respiratory paralysis cause death if not placed on mechanical ventilation no effect on mental statute. alert and oriented CDC notification – located and observe all people nursing management - ICU- ventilator tracheostomy / suctioning , rehydration, NPO, I/O, education ( if the ventilation id maintain the pt can recover without deficits) Infection of the brain o o Meningitis – inflammation cause by pathogen – IICP ( brain damage – death)- decrease cerebral perfusion main cause is infection. inflammation of pia-matter arachnoid subarachnoid place Meningitis Bacterial most common - bacterial - Neisseria meningitis, meningococcal, streptococcus, pneumoniae( mild ear infection), haemophilus influenzae and E-coli. - Manifestation – Up – - early -restlessness, agitation, and irrigation( nuchal rigidity ( stiff neck) - severe HA - chills and high fever - confusion and alteration in LOC - photophobia - sign late – seizures - of increased IICP( Cushing trail)- widened pulse pressure ,bradycardia , irregular respiration, decreased in loc HA and vomiting projectile. - petechial rash ( meningococcal) isolation for droplet( N95) until lab comes back – increased risk of contagious – other type need standard precautions (mask, glove, gown) - Dx lumbar puncture o complication- arthritis, CNS damage , CNIII- hearing loss , DVT ( infraction cerebral blood vessel) o prevention – vaccination – 11-12 repeated 16 yo – if unvaccinated 13-18one dose if first dose 16yo - bexsero - trumba o o Meningitis Virus – or aseptic meningitis - may be cured - cause by viruses – herpes simplex, zoater, Epstein-barr-viruss or cytomegalovirus ( CMV) - manifestation – mild HA- with malaise, V?N and lethargy = mild flu like illnss prior to the onset of meningitis - > protein and < glucose >WBC Encephalitis acute inflammation of the parenchyma of the brain always cause by virus ma may bacteria, fungi ( antifungal med ( amphotericin B or difuran) or other organism may be progressive to coma Brain Abscess purulent material in the brain ( cerebrum and cerebellar) cause open wound, infection of the mastoid and the middle ear, nasal cavity or nasal sinuses secondary in infection from cancer / metastatic spread from the lung and heard result microorganism of the brain tissues Sx of infection: fever, chills, malaise, anorexia late seizure and alteration on LOC-sing of < LOC – comatose Treatment broad spectrum antibiotics for unknow organism ( bacterial_rifampin, or vancomycin, claforan, give foe7-21 days + steroids to suppressed infalmation. interventional method (Ommoya reservoir) – implanted in the lateral part of the brain. diagnostic test. - bacterial -lumbar puncture turbid fluid ( cloudy) and < glucose - gram- stain for bacterial infection - CT – increased in contraction surrounding show low density care with brain abscess. - MRI-hemorrhage N/I - monitor LOC - assess foe seizure precaution - ABC - cranial nerve assessment - IICP symptoms. herniated intervertebral disk or rupture disk is the rupture of the protrusion of the nucleus pulposus that surrounding the cartilage between the inner and outer collar of the intervertebral disk? more in the lower back pain(L4-5 or S1) and in men more often( 30 to 50 yo) surgery if the conservation measure if not working bone graft done if pt has spinal fusion ‘laminectomy an artificial disk replacement order morphine for decreased in pain. N/I up right the way monitor DVT monitor CSF halo turn cough and deep breath to prevent otosclerosis or pneumonia Discharge after surgery limited stair climbing limit driving no lighting object more than 5 lb restrict pushing and pulling activity avoid bending or twisting at waist take a daily work. head trauma Review – caring with pati with seizure – safety – O2 whan cane of seizure how long if last, incotinant – call the doctor – no restrain, any thing on the mouthe med – takedon – steroid ( < swelling) mannitol – asmolatiti < fluid > UO ASA- TIA – keep the platelet from tiking together baby asa 81 mg – going TIA ( iskemic stroke – go away in the coup a day spinal injury shock (Spasticity and hyperactive reflexes, Lack of movement and sensation below the level of injury) neurogenic shock ( hypotension, bradycardia, warm extremities) , Autonomic dysreflexia ( T6 -bowel assessment, hypertension, bradycardia, throbbing headache, and diaphoresis. ) ( they can feel) _ > HTN – transition that noting can ascent – know the difference IICP – sx _ <LOC, restleness , and confusion – awake, and 2 hrs later very lathegic – cuching triad ( widen pulse peruse ) shyn staoc long period of apnea epidural hematomas – is arterial – is ER – uncouscouis then wake up – don’t see immmediated medical tx – subdural is veonus – slow – need a let of timw older people – the brain shweng – no sx for 2 or 3 days and lathalgy – bc the have more room CN III< IV< VI delegated qieustion LPN – can not do primary assess no IV push, they can give grug CAN= set the room for isolation eyes disordie glucama detached reine muscular disorder – no > temperature in stroke pt - > metabolic demanded -> ICP put the catheter into the ventricle – sterile technique Aneurysm sx meningitis bacterial – isolation droplet – cloudy, <glocuse > protein test the ring around gauze blood Halo –for sugar maysimax – graives tenseltong - too much monotir respiration status retrain – midtens – reatelness put the IV ICU propofol – short minute , brain injury- < propofal make the pt wake weakness in the leg. status epilatus – make the seizure stop - > HR, death O2 intubation ( drugs larazepain (adtivent ) broca’s /winkes ( they can speak but they can understand speck 85 questions