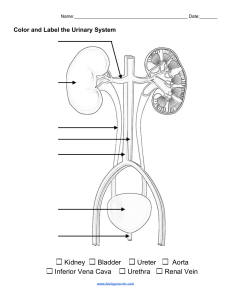
CH24 Urinary System Most regulatory function 2. Juxtamedullary nephrons 15% Long nephron loop extending deep into medulla Essential to produce concentrated urine Urinary system organs Kidneys: rcv 25% of cardiac output, major excretory organs) Ureters Urinary bladder Urinary tract Urethra 5 functions of urinary system 1. Adjusting bld volume and bp 2. Regulating bld plasma concentration of sodium, potassium, chloride, or other ions 3. Stabilize bld pH 4. Conserving valuable nutrients by preventing loss in urine 5. Removing drugs and toxins from bldstream 2 components of nephron 1. Renal corpuscle: BP forces water and solutes out of glomerular capillaries (filtration) → produce filtrate (protein free solution, bld plasma) in surrounding capsular space Glomerular capsule (bowman’s capsule): cup shaped chamber Glomerulus: capillary network 2. Renal tubule: tubular passageway upto 50mm long, rcv filtrate and modifies it to create urine Proximal convoluted tubule (PCT) i. rcv tubular fluid = filtrate ii. Lining cells reabsorb nutrients iii. Reabsorb 60-70% water (108-116L/day), 99100% organic substrates, 60-70% Na+, Cl- in original filtrate Nephron loop (loop of henle) i. osmotic gradient for water reabsorption. ii. Each limb has thin segment/thick segment. iii. 25% of water (45L/day) and 20-25% Na,Cl reabsorption. iv. Creates concentration gradient in renal medulla Distal convoluted tubule (DCT) i. adjust tubular fluid composition by reabsorption and secretion ii. 5%, 9L/day water reabsorption under ADH, variable amount of Na reabsorption under aldosterone Kidney structure: paired retroperitoneal organs Reddish brown, 4” L x 2.2” w x 1.2” thick / ~150g (5.25oz) Hilum: medial indentation, point of exit/entry for renal artery, nerves, vein and ureter Location: btwn muscle wall and parietal peritoneum, protected by organs & body musculature & 11,12th ribs, L is superior than R Positioned by 1. overlying peritoneum 2. adjacent visceral organs 3. supporting connective tissues Connective tissues: Fibrous capsule (collagen fiber layer): outer surface, project fibers into perinephric fat to renal fascia Perinephric fat (perinephric fat capsule): thick fat tissue Renal fascia (dense, fibrous outer layer): anchors to surrounding structure Major structure of kidney Fibrous capsule: lines renal sinus Renal cortex: superficial region, outer most Renal medulla: inner region, includes belos; 1. Renal pyramid: conical structure 2. Renal papilla: tip of pyramid 3. Renal column: separates adjacent pyramids Kidney lobe: pyramid, cortex and columns. 6-18 lobes each Hilum Minor calyx: collect urine from single kidney lobe Major calyx: form from fusion of 4-5 minor calyces Renal pelvis: funnel shaped collects urine from major calyces, continuous with ureter Collecting system: tubes carrying tubular fluid away from nephrons 1. Collecting duct: fluid from many nephrons, carry fluids through renal medulla. Reabsorption variable amount of water (9%, 16.8L/day) under ADH and Na reabsorption under aldosterone. 2 lining cells: intercalated cells (secrete, reabsorb hydrogen and bicarbonate ions) Principal cells (reabsorb water and secrete potassium) 2. Papillary duct: fluid from collecting ducts, deliver to ureter 2 types of nephrons (microscopic functional units) 1. Cortical nephrons 85% of all nephrons Primarily in cortex Arterial system 1 CH24 Urinary System Renal artery → segmental arteries → interlobar arteries → arcuate arteries → cortical radiate arteries (=interlobular arteries) → afferent arterioles → glomerulus (pedicels) that wrap around glomerular capillaries, gap between pedicels are filtration slits Filtration membrane: fenestrated glomerular capillaries → dense layer basement membrane → filtration slits Efferent arteriole < Afferent arteriole (increase BP in glomerular capillaries) Juxtaglomerular complex: secretes renin when glomerular bp decreases Intraglomerular mesangial cells: supporting cells, btwn adjacent glomerular capillaries, control capillary diameter and bld flow rate Glomerular filtration rate: amount of filtrate produced each minute. Net filtration pressure (NFP) being positive and filtrate move into capsular space 2. Reabsorption Transport water and solutes from tubular fluid across tubular epithelium into peritubular fluid and the peritubular capillaries Predominates in proximal convoluted tubule (PCT) i. >99% of glucose, amino acids, organic nutrients ii. Sodium, potassium, bicarbonate, magnesium, phosphate, sulfate ions iii. Water (108L /day); solute concentration of tubular fluid↓, water moves into peritubular fluid 3. Secretion Transport of solutes from peritubular fluid across tubular epithelium into tubular fluid Mvmt of water and solutes (peritubular fluid → tubular fluid) 15-20% of initial filtrate volume reaches DCT Venous system Cortical radiate veins → arcuate veins → interlobar veins → segmental vein → renal vein Bld flow in cortical nephron Afferent arteriole → glomerulus → efferent arteriole → peritubular capillaries (surround entire renal tubule, surrounded by peritubular fluid, reabsorb water and solutes drain into cortical radiate veins) Bld flow in juxtamedullary nephron Same until after peritubular capillaries Vasa recta: connected to distal end of peritubular capillaries. Long, straight capillaries parallel to nephron loop. Transport & redistribute water and solutes within medulla; stabilize concentration gradient of medulla. Drain into cortical radiate veins Nephron innervation 1.25 M nephrons each kidney Cortical and juxtamedullary nephrons innervated by renal nerves (enter at hilum, follow renal artery) Mostly sympathetic postganglionic fibers from celiac plexus and inferior splanchnic nerves that provides… o Sympathetic stimuli adjusting bld flow and bp at glomeruli o Stimulate release of renin Renal physiology and homeostasis By regulating volume and composition of bld Concentrates urine to 855-1355mOsm/L Excretes solutes and metabolic wastes Metabolic wastes (much higher in Urine than Bld plasma) Urea: abundant organic waste, by product of amino acid breakdown Creatinine: byproduct of creatine phosphate breakdown in muscles Uric acid: recycling of nitrogenous bases of RNA Functions of nephron segment Filtration only in renal corpuscle (180L/day) Balance btwn reabsorption and secretion varies in remaining nephron segments Final volume and concentration regulation is btwn collecting system and nephron loops 3 processes in urine formation 1. Filtration BP forces water and solutes across the membrane of glomerular capillaries into capsular space (btwn layers of glomerular capsule) Glomerular capsule: receiving container i. parietal layer (outer capsule) ii. Visceral layer: cover capillary, composed of podocytes, large cells with food processes Normal urine 1200mL/day with osmotic concentration of 1000 mOsm/L Differ from person and day; kidney alter function for homeostasis 2 CH24 Urinary System Shunts (silicone rubber tubes) connect bld vessels with machine Renal failure treatment Dialysis relieves symptoms but not a cure; kidney transplant is only real cure for severe renal failure >90% survival at 2yrs after transplant Close relative donor increases success rate Immunosuppressive drugs are necessary to reduce rejection Urinary tract: transports, stores, eliminates urine Visualized by pyelogram; x-ray image taken after an intravenous radiopaque dye administration Ureters: muscular tube about 30cm o retroperitoneal and attached to posterior abdominal wall o penetrate posterior bladder wall at oblique angle Bladder: hollow, muscular organ, ~1L, outside of peritoneal cavity o Supporting ligaments (lateral umbilical ligaments, middle umbilical ligaments) o Rugae: folds in lining for expansion o Ureteric orifices: slit-like shape prevent backflow of urine into ureters with bladder contraction o Trigone: triangular area bounded by ureteral opening and entrance to urethra o Neck of urinary bladder: surrounds urethral opening, internal urethral sphincter (involuntary smth muscle) o External urethral sphincter: located where urethra passes through urogenital diaphragm, voluntary control (must relax to urinate) Urethra: neck of bladder to exterior of the body Renal failure: kidney cannot remove wastes. Results in Decrease in urine production BP ↑ Anemia from decline erythropoietin production Central nerve system problems (sleeplessness, seizures, delirium, coma) Chronic renal failure: function deteriorate gradually over time. slow progression, irreversible condition Manage by restricting water, salt, protein intake → reduce strain by minimizing V of urine produced and amount of nitrogenous waste generated Acidosis: common problem with renal failure. Countered by ingesting bicarbonate ions Lining of ureters 1. Inner mucosa: transitional epithelium and surrounding lamina propria 2. Middle muscular layer: bands of smth muscle creating peristaltic waves to move urine 3. Outer connective tissue layer: continuous with fibrous capsule and peritoneum Acute renal failure: rapid deteriorates of kidney function in few days; may be impaired for wks Sudden slowing or sopping of filtration caused by toxic drugs, renal ischemia, urinary obstruction, trauma, allergic response to antibiotics or anesthetics in sensitized individuals Partial or complete recovery is possible; ~50% survival rate with supportive treatment Wall of bladder 1. Mucosa 2. Submucosa 3. Muscularis layer: form detrusor muscle, 3 layers Inner longitudinal Circular Outer longitudinal Dialysis: process of passive diffusion across selectively permeable membrane Hemodialysis: Regulates composition of bld using dialysis machine with artificial membrane Dialysis fluid containing specific concentrations of solutes in the other side of membrane Wall of urethra 3 CH24 Urinary System Thick & elastic lamina propria, longitudinal folds in mucous membrane (mucin secreting cells in epithelial pocket) Stratified epithelium that varies by location 1. Transitional at neck 2. Stratified columnar at mid 3. Stratified squamous near external urethral orifice Dysuria: painful or difficult urination. Ex. Cystitis, urethritis, urinary obstructions (enlarged prostate in male) <clinical signs of urinary system disorders> Edema(swelling): renal disorders lead to proteinuria (protein in urine). Facial swelling especially around eyes Fever: when urinary system is infected with pathogens Cystitis: bladder infection; low-grade fever Pyelonephritis: kidney infection; very high fever Micturition reflex (urinary reflex) Coordinates process of urination by both 1. Local reflex pathway 2. Central pathway through cerebral cortex Urine storage reflex: stretch receptors of bladder wall → a. In vertebrae, sympathetic stimulation to detrusor and contraction of internal urethral sphincter b. Pontine storage center: parasympathetic activity↓, somatic motor nerve activity of external urethral sphincter↑ Urine voiding reflex: by pontine micturition center→ Interneuron relays sensation of bladder fullness to thalamus Projection fibers relay info to cerebral cortex Voluntary relaxation of external urethral sphincter (causes relaxation of internal urethral sphincter) leads urination due to increased pressure Urinary disorders <volume and appearance change> Polyuria: excessive urine production from H or metabolic problems, possibly diabetes or glomerulonephritis Oliguria: reduced urine production (50-500mL/day) Anuria: severely reduced urine production (0-50mL/day) Oliguria and anuria indicate serious kidney problems and potential renal failure <frequency change> Increased urgency or frequency can be caused by irritation of the lining of ureter or bladder Incontinence: inability to control urination voluntarily Periodic involuntary leakage = stress incontinence Inability to delay = urge incontinence Continual trickle of urine from full bladder = overflow incontinence Urinary retention: initially normal renal function, urination does not occur (commonly by enlarged prostate gland, compression of prostatic urethra) <pain> Superior pubic region: urinary bladder disorders Superior lumbar or flank region radiating to right or left upper quadrants: kidney infection (pyelonephritis) or kidney stones (renal calculi) 4