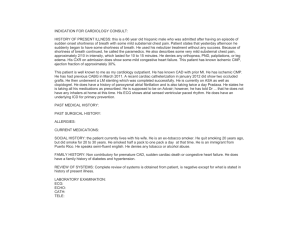
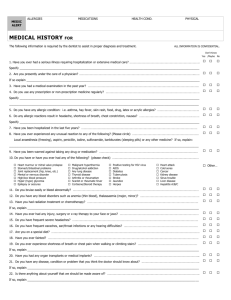
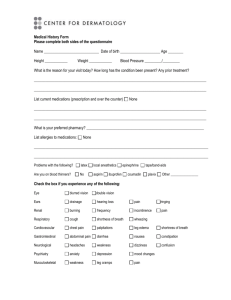
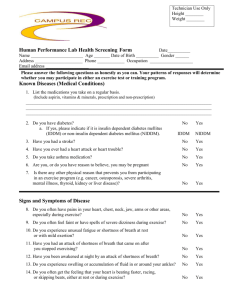
This week for discussion please read the case study and answer one of the questions in the discussion forum. Feel free to add or comment on other classmate's discussion. Case Study: Cognition HPI: Ruth is a 70 year old widowed female brought to the doctor’s office by her daughter who reports her mother has not been herself lately. She doesn’t take part in activities with her friends as often and seems to pay less attention to her hygiene or housekeeping. The house is dirty but Ruth doesn’t see it. Ruth seems down and is less interested in what is happening to her family. Ruth has begun repeating the same stories and asking the same questions repeatedly. She has been more forgetful, losing her house keys in the last few months. Previously an avid reader, she no longer attends book club and can’t concentrate sufficiently to complete her stories. Daughter wonders if Ruth’s vision is impaired as she is finding soiled clothing throughout the house. Ruth is staying home most of the time, watching TV. Ruth states she is feeling just fine and her daughter is a worrier. Self-Care Deficit r/t cognitive impairment AEB pay less attention to her hygiene or housekeeping. Social Isolation r/t cognitive decline and loss of loved one AEB widowed 2 years ago, she doesn’t take part in activities with her friends as often, less interested In what is happening to her family, no longer attends book club, staying home most of time watching TV. Chronic Confusion r/t cognitive impairment AEB repeating the same stories and asking the same questions repeatedly, she has been more forgetful, losing her house keys, can’t concentrate sufficiently to complete her stories, soiled clothing throughout the house. Risk for injury r/t HTN, age 70, forgetful, losing keys, visual changes. PMH: HTN, HLD since age 62 Depression treated in the past with sertraline. No recent therapy for depression SH: Widowed 2 years ago. Had been married for 45 years. Medications: Lisinopril 10 mg PO daily Simvastatin 20 mg PO HS Allergies: PE: NKDA VS: 98.4-68-16 132/84 CV: RRR, nl S1S2 HT: 5’4” WT: 135lbs BMI: 23.2 Resp: CTA Question 1: What tests could you perform in the office? Question 2:· What do you think could be wrong with this woman? List possibilities. What would cause these symptoms? Question 3: What would you recommend for lab tests that might be helpful in narrowing your search Question 4: What do you think is happening to this patient? Question 5: What are the medications for this condition, What are the dosages, side effects? Common interactions? Question 6: Nursing DX Case study 1 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4269302/ Case Study/ Comments or questions about lecture Case Study: Dyspnea HPI: 67 year old female, Ann, arrives at the emergency department complaining of shortness of breath for the past five days which has gotten progressively worse. Her shortness of breath is worse when lying down and with exertion. She complains of a cough, especially at night. The patient also notes increased swelling in her legs bilaterally and well as mild substernal chest pressure. PMH: Hypertension, Diabetes type II, Prior Myocardial Infarction SH: Married X 40 years, Retired teacher, 2 grown children living far away Medications: Metformin 500 mg PO BID, Lisinopril 10 mg PO daily, Simvastatin 20 mg PO HS, Metoprolol 50 mg Daily, Nitro 0.5 mg SL PRN Allergies: NKDAPE: BP 210/106, HR 118, RR 26, T 98.2. Height: CV: 5‘4“ Weight: 175 lbs RRR Lungs: Crackles in the lung bases bilaterally EXT: 1+ pitting edema in the lower extremities bilaterally Question 1: What tests/assessments could you perform in the ED? Question 2: What do you think could be wrong with this woman? List possibilities. What would cause these symptoms? What are potential causes of dyspnea. Question 3: What would you recommend for lab tests that might be helpful in narrowing your search Question 4: What do you think is happening to this patient? Question 5: What are the medications for this condition? What are the dosages, side effects? Common interactions? Question 6: Nursing DX/ Differential DX Ineffective breathing pattern r/t cardio-pulmonary impairment secondary to heart failure AEB HR 118, RR 26, Crackles in the lung bases bilaterally , complaining of shortness of breath for the past five days which has gotten progressively worse. Her shortness of breath is worse when lying down and with exertion. She complains of a cough, especially at night. Activity Intolerance r/t imbalance between o2 supply/demand AEB dyspnea, complaining of shortness of breath for the past five days which has gotten progressively worse. Her shortness of breath is worse when lying down and with exertion. She complains of a cough, especially at night. Excess fluid volume r/t decreased cardiac output AEB BP 210/106, HR 118, RR 26,crackles in the lung bases bilaterally , increased swelling in her legs bilaterally and well as mild substernal chest pressure. 1+ pitting edema in the lower extremities bilaterally. Ineffective tissue perfusion r/t decreased cardiac output AEB difficulty breathing complaining of shortness of breath, BP 210/106 HR 118, RR 26, 1+ pitting edema in the lower extremities bilaterally. Anxiety r/t Breathlessness from inadequate oxygenation AEB complaining of shortness of breath for the past five days which has gotten progressively worse, She complains of a cough, especially at night. 2 grown children living far away Risk for impaired skin integrity r/t 1+ pitting edema in the lower extremities bilaterally Risk for https://nurseslabs.com/heart-failure-nursing-care-plans/16/