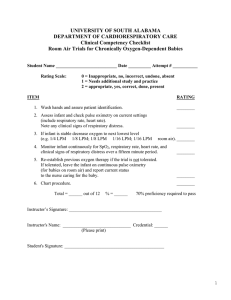
EMT Practice Final Exam 1 You are treating a patient in severe shock who is breathing at a rate of 20 times per minute. Besides rate, which of the following assessments would you need to help determine the proper type of oxygen administration devices to use? A: The adequacy of the airway. B: The volume of each breath. C: The patient’s blood pressure. D: The patient’s heart rate. 2 You are treating a patient in severe shock who is breathing at a rate of 20 times per minute. Assume this patient has adequate chest rise and fall and is moving a sufficient quantity of air. Which of the following oxygen delivery devices would be most appropriate? A: A bag-valve-mask device. B: A flow-restricted, oxygen-powered device. C: A nasal cannula at 6 LPM. D: A non-rebreather mask at 12-15 LPM. 3 You are treating a patient experiencing a diabetic emergency who opens her eyes upon loud verbal stimuli and has an intact gag reflex. You have performed a head-tilt/chin-lift maneuver on the patient; however, the patient is still exhibiting snoring sounds with each breath. Which of the following would be the most appropriate method to alleviate the snoring sounds? A: Perform abdominal thrusts. B: Place a nasopharyngeal airway. C: Place an oropharyngeal airway. D: Suction the nose with a flexible catheter. 4 You arrive to find a 62-year-old male complaining of difficulty breathing. The patient is sitting forward in a chair and is obviously anxious. Upon assessment, respiratory rate is 36, shallow and labored. The patient’s heart rate is 120, weak and irregular. You also note that the patient’s skin is slightly cyanotic centrally and significantly cyanotic peripherally. Of the following, which is the most critical assessment you should perform on this patient? A: Assess lung sounds bilaterally. B: Assess the patient’s temperature. C: Obtain the pulse oximetry reading. D: Obtain a blood pressure reading. r.20190312 EMT Practice Final Exam 5 You are assessing a patient who has complained of difficulty breathing. You have just begun listening for lung sounds by auscultating the left upper chest. You should next listen to the: A: Heart sounds. B: Left lower chest. C: Right lower chest. D: Right upper chest. 6 You have responded to a patient who has a history of COPD. The patient tells you she has asthma and is on home oxygen at 2 LPM. She has called you today because she has twisted her ankle. You note some swelling and bruising in the right ankle area. The patient has no other injuries or complaints. Which of the following would be the most appropriate oxygen delivery device to administer to the patient while transporting to the hospital? A: Assist ventilations with a bag valve mask. B: A non-rebreather mask at 12-15 LPM. C: A partial rebreather mask at 10 LPM. D: A nasal cannula at 2 LPM. 7 You are called to the scene of a cardiac arrest, where a 16-year-old patient was discovered in a pool face down. The family has him taken out of the pool, started CPR and called 911. The patient is pale, cold and clammy. There are pulses with CPR but no pulses without CPR. Which of the following should you do next? A: Dry the patient’s chest, attach the AED, turn it on, and follow the directions of the machine. B: Fully immobilize the patient on a backboard and then resume CPR at a 30 to 2 ratio. C: Remove all of his clothing, dry him off completely, and then attach the AED. D: Turn the patient on his side, decompress the stomach, and then return to CPR. 8 You are transporting a patient to a local hospital when the patient suddenly develops nausea and vomiting, cold sweats, and a drop in systolic blood pressure. The patient also states that she has some pressure in her chest. Which of the following treatments should be initiated first? A: Administer nitroglycerin. B: Administer high flow oxygen. C: Place the patient in an upright position. D: Place an oral airway and assist ventilations. r.20190312 EMT Practice Final Exam 9 Your ambulance is called to the scene of a cardiac patient. He is pale, diaphoretic, and is not answering questions appropriately. The patient’s blood pressure is 60 systolic, and he has a pulse of 130, weak and thready. The patient’s wife informs you he is an insulin dependent diabetic and also has suffered a heart attack six months ago. Since that time he has been prescribed a water pill to help control the amount of fluid in his lungs. Which of the following would be most important in providing treatment to this patient? A: High flow oxygen by non-rebreather mask. B: Auscultation of lung sounds bilaterally. C: Collection of a list of medications. D: Administration of nitroglycerin. 10 You are called to treat a 74-year-old female who is complaining of generalized weakness and tightness in her chest. She smokes 2 packs of cigarettes a day and is a diabetic. Vital signs are pulse 120 and irregular, breathing 22 labored and shallow, blood pressure 100/60, and her skin is mottled and moist. What treatment should you provide this patient? A: Apply oxygen through a non-rebreather mask and reassure the patient. B: Assist her in the administration of her insulin medication. C: Have her drink some sweetened beverage as her sugar is low. D: Place her on 2 LPM nasal cannula as she probably has COPD. 11 You are called to treat a patient who lost control of his bicycle and ended up in a bush. While assessing the patient, you notice that he has a stick impaled in his cheek and blood is flowing into the airway. Select the best choice to deal with this situation: A: Apply pressure to the temporal artery in an effort to control the bleeding. B: Place the patient on his side and allow the blood to drain from his airway. C: Remove the stick from the cheek and control bleeding both inside and out. D: Stabilize the stick in place and immobilize the patient on a long board. 12 You are called to a residence where a 30-year-old female was thrown from her house after an explosion. She is supine, unresponsive, and has some notable burns. There is no obvious bleeding. She is breathing at 30 times per minute, and has a weak radial pulse at 130 beats per minute. Which of the following should also be included in a rapid secondary assessment (rapid trauma survey)? A: Assessing the trachea and neck veins. B: Obtaining a blood pressure and history. C: Determining the percentage of burn area affected. D: Evaluating the upper extremities for deformities. r.20190312 EMT Practice Final Exam 13 You are called to the scene of a single motor vehicle accident where a 19-year-old male has lost control of his vehicle and hit a tree. The patient is still seated in the driver’s seat and is speaking incoherently. You are holding cervical spine control while opening the airway and notice a fruity odor on his breath. You notice a small bump on the left side of the patient’s head and a minor laceration to his forehead. The patient’s pulse is 40 and respirations are irregular at 6. Once you have finished your primary assessment, you should proceed with your assessment by performing a: A: Rapid secondary assessment (rapid trauma survey). B: Complete secondary assessment (detailed physical exam). C: Modified secondary assessment (focused exam) of the head. D: Diabetic history evaluation. 14 You are attempting to stabilize a 17-year-old male who has been stabbed in the chest just under the right arm. You find a sucking sound in the area of the stab wound. The sucking chest wound requires what type of special care? A: A bulky dressing to stabilize the chest. B: Placement of an occlusive dressing. C: Sterile gauze to control bleeding. D: Leaving the wound exposed. 15 You are called to a long term nursing facility for an elderly female that complains of shortness of breath. She has been a patient for years and the staff tells the EMT that she is coughing up blood and needs transport to the hospital to rule out tuberculosis. What care should you provide? A: Check the patient’s medical records for a DNR order and if present, refuse to transport. B: Oxygen by non-rebreather mask at 10-15 LPM and isolation precautions. C: Place the patient in a Trendelenburg position to treat for hypovolemic shock and give oxygen. D: Use a rigid suction catheter to suction the blood from the airway and begin assisting ventilations. 16 You are called to the scene of a 64-year-old female who is complaining of a severe headache that occurred immediately after she got out of bed this morning. She is also having a difficult time formulating sentences. She tells you she takes a “blood thinner” as a result of her irregular heart condition. The patient’s level of consciousness has decreased. Your assessment reveals a blood pressure of 210/120. Pulse is 60 and respirations are 12/minute and decreasing. Which of the following is the most appropriate treatment option? A: Place an NPA and supplemental oxygen with a nasal cannula at 2-4 LPM. B: Place an OPA and begin assisting ventilations at 30 times per minute. C: Place a non-rebreather mask at 15 LPM and prepare to assist ventilations. D: Place a nasal cannula at 6 LPM and position her in a supine position. r.20190312 EMT Practice Final Exam 17 You are dispatched to a school playground where a 15-year-old male has fallen from a bicycle and has a deformed lower right arm. The patient tells you he has a condition called hemophilia. What other critical assessments should you perform on this patient relative to his condition and hemophilia history? A: Ascertain whether the patient can move his injured arm or not. B: Ask the patient what his last oral intake was today. C: Assess sensation and pulses below the injury site. D: Determine if there is a possibility of internal bleeding. 18 You are called to a restaurant where a 36-year-old male has begun walking around the restaurant acting confused. The patient’s wife meets you at the entrance and indicates that her husband has been under a lot of stress lately and is now acting strangely. The wife tells you he has had one beer while waiting for his meal and is disoriented. His skin is moist, pulse is rapid, and breathing is normal. His past medical history is high blood pressure, heart problems and diabetes. Which of the following is most appropriate? A: Administer activated charcoal by mouth after contacting medical control. B: Prepare restraints, as the patient will likely become hostile towards the crew. C: Attempt to administer oral glucose to the patient by mouth. D: Try to orient the patient and have him discuss his stressors. 19 You are called to assess a 5-year-old male who is unresponsive. The mother tells you that her son has been vomiting and had diarrhea for the past two days. The skin is pale, cool, and clammy, and the child is only responsive to painful stimuli. What other assessments would you expect to find with this patient? A: An increased respiratory rate and an increased pulse rate. B: A non-purposeful stare to the right and a sunken fontanel. C: Instant capillary refill time on the hands of the patient. D: An increased auscultated blood pressure. 20 You have a male patient with difficulty breathing. Your exam reveals the following: breath sounds are wheezing bilaterally. The patient has a prescription for an inhaler. His respirations are 32 and labored, pulse 104 and regular, and he is alert and oriented. He tells you that this is the worst asthma attack he’s ever had and he fears dying. As you are writing your report for this patient, which is the least important to include for purposes of documentation? A: The patient’s history of asthma and what he did for relief from the attack. B: The patient’s description that this is the worst asthma attack he has ever experienced. C: The patient’s blood pressure before and after the inhaler treatments were given. D: The presence of pulse, motor function, and sensation after transport to the hospital. r.20190312 EMT Practice Final Exam ANSWER KEY 1-B When selecting an oxygen device, first evaluate for the need for ventilation support (tidal volume). 2-D This patient has adequate tidal volume and is in shock. Position supine, give high flow O2, keep warm. 3-B The tongue is the problem causing snoring. An OPA would gag this patient while an NPA will not. 4-A You already have the tidal volume. Lung sounds would allow you to focus your treatment the most. 5-D Compare lung sounds side to side at the same height. After left upper is right upper. 6-D The complaint is trauma, not medical. The oxygen given is only to maintain what the patient uses at home. 7-A Prioritize CPR and AED use over backboarding, removing clothing, and stomach decompression. 8-B High flow oxygen is indicated; NTG relies on BP; airway/ventilations not needed; place the patient supine. 9-A High flow oxygen is indicated regardless of lung sounds; NTG contraindicated; medications not important 10-A Insulin administration not in EMT scope; labored breathing requires higher LPM; assume cardiac cause 11-C Impalements may be removed by EMTs when they endanger the airway. 12-A Rapid trauma assessment contains significant findings from the head to the pelvis. 13-A This is a trauma patient with a suspected diabetic cause. Perform a rapid trauma survey. 14-B Sucking chest wounds need occlusive (airtight) dressings to prevent the development of pneumothorax. 15-B Complaints of SOB get oxygen; suspected TB requires isolation precautions and a respirator for you. 16-C Altered LOC requires higher LPM O2; ventilation is not indicated at the current time but may be soon. 17-D Hemophilia is a bleeding disorder; evaluate the possibility of internal bleeding; everything else unimportant. 18-C Altered LOC with known diabetic problems should be assumed as hypoglycemia with this presentation. 19-A Vomiting and diarrhea, suspect dehydration; this results in increased HR and RR and decreased BP. 20-D Distal pulse, motor, sensation (trauma assessments) are unimportant on this medically focused call. r.20190312