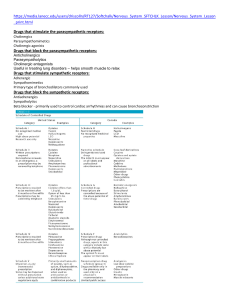
Cardiac Medications Chapter 15: Adrenergic Agonists and Adrenergic Blockers Nervous System 101: Autonomic Nervous System Sympathetic Parasympathetic Fight or Flight Rest and Digest Epinephrine, Dopamine, Norepinephrine Alpha 1, Alpha 2, Beta 1, Beta 2 Acetylcholinesterase Muscarinic and nicotinic Sympathetic Receptors Alpha Receptors: o Alpha 1: Blood vessels: vasoconstriction (raise our BP), increased BP increased contractibility of the heart Eyes: mydriasis (pupil dilation) We need to see better in the fight-or-flight response Bladder: relaxation Bladder is pretty much shut down Prostate: contraction At this time, it is not time for the prostate to be active o Alpha 2: more narrowly focused; inhibits norepinephrine release Blood vessels: decreased blood pressure Smooth muscle (GI tract): decreased GI motility and tone Beta Receptors: o Beta 1: located within the kidneys, but predominately in the heart itself Heart: increased heart contraction, increased HR, increase blood pressure Kidney: increased renin secretion, increased angiotensin, increased blood pressure RAAS System o Beta 2: Smooth muscle (GI tract): decreased GI motility and tone Lungs: bronchodilation Uterus: relaxation of uterine smooth muscle Liver: activation of glycogenolysis, increased blood sugar Breakdown of glycogen use carefully with diabetic patients Dopaminergic Receptors o Located in the renal. mesenteric, coronary, and cerebral arteries o Causes vasodilation increased blood flow o Dopamine is the only neurotransmitter/medication that can activate this receptor Dopamine is a normal neurotransmitter found in the body, but there is also synthetic dopamine that is made in a lab that can activate the receptor sites when concentrations of dopamine in the body o Given when patients are septic because they are hypotensive increases blood flow increase in blood pressure Classification of Adrenergic Agonists/Sympathomimetics Direct acting o Epinephrine (Epi) and norepinephrine (NE) o Directly stimulates adrenergic receptor Mimic normal neurotransmitters o Stimulates normal neurotransmitters o Main focus Indirect Acting o Amphetamine o Stimulates the release of norepinephrine from terminal nerve endings o The “middleman” Mixed Acting o Ephedrine o Stimulates adrenergic receptor sites and stimulates the release of NE from terminal nerve endings o Lazier has people do work for them then decides to do work themselves Catecholamines Catecholamines o Chemical structures of a substance o Produce a sympathetic response Structures we have produced in a lab to mimic the synthetic receptors o Endogenous or sympathetic Endogenous: epinephrine, norepinephrine, dopamine Can be produced in the body, but can also be created in the lab Sympathetic: isoproterenol and dobutamine (synthetic version of dopamine) Cannot be found in the body, so they have to be created in a lab Noncatecholamines o Stimulate adrenergic receptors Act on the receptor sites themselves Work like catecholamines, but work on the receptor sites o Most often have a longer duration than endogenous and synthetic versions o Examples: Phenylephrine Can be found in Sudafed Metaproterenol Albuterol Inhaler Epinephrine (Medication) Non-Selective o Excites 3 different receptor sites equally Alpha 1, Beta 1, Beta 2 o Gets into the body quickly Action o Increase blood pressure (Alpha 1) Given during CPR (cardiac rescue medication) o Increase heart rate (Beta 1) o Bronchodilation (Beta 2) This is why we give medication in respiratory emergencies and anaphylactic reactions helps open up airways Contraindications/caution o Dysrhythmias, HTN Due to increase in heart rate and blood pressure Can put people into a lethal arrhythmia Could induce stroke-like symptoms If patient already has high blood pressure o Hyperthyroidism (thyroid storm), DM Excites Beta 2 receptorsglycogenolysis which causes an increase in blood sugar (closely monitor blood sugar) o Pregnancy When they are pregnant, mom shares circulatory system with babies When the mothers heart rate and blood pressure are increased, the baby’s is as well Only given when absolutely critical cardiac arrest or anaphylactic reactions Action: o Inotropic Positive inotropic effect strengthen the force of the heartbeat o Vasoconstrictor o Bronchodilator o Oral or lip swelling could also indicate airway constriction Uses: o Anaphylaxis/anaphylactic shock o Bronchospasms Bad asthmatic attacks o Cardiogenic shock/cardiac arrest (CPR) Side effects: o Cardiac o Decreased renal perfusion Due to increase in blood pressure and heart rate The faster the heart pumps, the less blood coming out with each pump, thus reducing the amount of blood perfusing the kidneys Interactions: o Beta-blockers Beta-blockers block the receptor sites; therefore, Epi cannot reach its target site; they work against each other o Digoxin Antiarrhythmic will interact with Epi Chart 15.1 on page 202 Nursing interventions: o Monitor BP, HR, and urine output Monitoring urine output due to decrease in renal perfusion o Report rhythm changes, tremors, dizziness, HTN, and palpations Sinus tachycardia want to be cautious about and notify HCP Teach that they may feel tremor or shakes heart will be pumping and they will not know why Dizziness due to increase in heart rate o Monitor IV site for infiltration Especially if giving an Epi drip Antidote: phentolamine mesylate Will do the opposite of epinephrine If reaching subcutaneous tissue o Avoid cold medications/diet pills CONTAIN CAFFEINE will go into tachycardia Recommended for elderly patients OTC cold medications; safe if taking any heart medications (if they have a heart on the label) o Avoid when breastfeeding Pump and dump Pumping breast milk and dumping it out Will reach the baby’s bloodstream and cause increase in blood mediations o Avoid continuous use of adrenergic nasal sprays Adrenergic: does the same thing as epinephrine Other Cardiac Adrenergic Agonists Dobutamine o Synthetic catecholamine o Increases myocardial force and cardiac output Increases contractions and strength of contractions providing more blood to the rest of the body o Used with heart failure and bypass surgery o Not normally produced in the body synthetic catecholamine Dopamine o The SYNTHETIC dopamine o Increases BP and cardiac output (CO), and increases renal blood flow o Used to treat mild kidney failure due to low CO Stage 1 renal disease Norepinephrine o Not given as often as epinephrine given if Epi doesn’t seem to be working o Stimulates the heart in cardiac arrest o Vasoconstricts and increases blood pressure in hypotension and shock (septic shock, cardiac shock, etc.) Albuterol Selective o Acts on Beta 2 receptors o Bronchodilation Used for respiratory distress and asthma o Glycogenolysis (liver) NEED TO MONITOR BLOOD SUGAR Uses o Asthma, COPD, bronchospasm, chronic bronchitis Side effects/adverse reactions o Restlessness (agitated), nervousness, restless o Tachycardia, dizziness, hallucinations (in severe cases; can see auras or different colors) Drug interactions o May increase other sympathomimetics and tricyclic antidepressants Want to be VERY cautious when given with tricyclic antidepressants o Beta blockers due to the blockage of beta receptors Chart 15.2 (p. 204) WE USE ALBUTEROL BECAUSE IT WORKS ON THE BETA 2 RECEPTORS Central Acting Alpha Adrenergic Agonists Alpha receptor; adrenergic agonist WORKS WITH THE SYMPATHETIC NERVOUS SYSTEM Clonidine o Primarily used to treat hypertension o Selective Alpha 2 agonist Only will work on Alpha 2 receptor sites o Contraindication in liver disease Works on liver and causes glycogenolysis Make the liver pick up in production o Side effects Edema, bradycardia Drowsiness/dizziness Dry mouth Number one complaint Stimulates alpha receptors dries up secretions Suck on ice chips, chew on sugar-free gum or candy, or spongy oral swabs if NPO Educate that this is a side effect, not a reason to stop taking the medication o Nursing interventions Monitor BMP and I&Os Clonidine will retain sodium and water Assess and monitor VS Used to treat hypertension Blood pressure and heart rate before and after administration Treat c/o dry mouth Heavy machinery educate! Due to drowsiness effect Know how medication affects them before driving or operating machinery Adrenergic Antagonists Works against or neutralizes effects of sympathetic nervous system Blocks the effect of the adrenergic neurotransmitter o Blocks the receptor site or inhibits the release of epinephrine and norepinephrine Works on both alpha and beta receptor sites o Normally on one or the other, but does not rule out that it will not work on both o Classified based on their target receptor site o Alpha 1 antagonist: vasodilation, decreased BP, pupil constriction, and reflex tachycardia For male patients, prostate will relax which will suppress ejaculation will be more difficult or inhibited entirely; EDUCATE o Beta 1 antagonist: reduces cardiac contractility, decreases pulse o Beta 2 antagonist: bronchoconstriction, contracts uterus, inhibits glycogenolysis Medications o TABLE 15.4 Alpha Blockers (-zosin) Selective o Blocks alpha 1 receptors Non-selective o Blocks both alpha receptor sites Action o Promotes vasodilation want more blood flow Use o Decreases symptoms of benign prostatic hyperplasia (BPH) and peripheral vascular disease (PVD) Medications o Prazosin and Terazosin o These drugs are contraindicated or used with caution in cases of asthma, bradycardia, HF, severe renal or hepatic disease, hypothyroidism, or if the patient has had a previous stroke Beta Blockers (-lol) Selective o Blocks beta 1: decreased BP and HR o Blocks beta 2: bronchoconstriction Non-selective o Blocks both beta receptor sites Action o Decreases CO and blocks the release of Epinephrine and Norepinephrine Use o Mild to moderate hypertension, angina, migraines, mild dysrhythmias, and heart failure Used in conjunction with other heart medications when used to treat heart failure Contraindications/caution o Patients with COPD/asthma Because of bronchoconstriction may make it harder for these patients to breathe Nursing considerations: o Because beta blockers decrease heart rate HAVE TO HAVE A HEART RATE BEFORE ADMINISTERING BETA BLOCKERS IF HEART RATE IS LESS THAN 50, DO NOT GIVE THIS MEDICATION o Always monitor vital signs (BP) and lung sounds o Teach our patients to NEVER discontinue medication abruptly Can cause tachycardia, rebound blood pressure higher than before, can cause a stroke or dysrhythmias If not tolerating, taper off over a 1-2 week period o Avoid postural hypotension Have patients rise or stand up slowly Dangle feet on edge of bed for 20-30 seconds o Make sure patients don’t operate vehicles or heavy machinery until they know how it affects them because it can cause dizziness Propranolol Uses o Angina, dysrhythmias, hypertension, heart failure Contraindications o Asthma and COPD patients Side effects/adverse reactions o Dizziness, low blood pressure, low heart rate o Male patients: will cause impatience, decrease libido and alopecia (reversible) Can cause them to be noncompliant or stop medication MUST EDUCATE Drug interactions o Decreased effect of phenytoin, NSAIDs, caffeine, and theophylline o Heart block may occur when used with CCB and Digoxin Atenolol Selective o Blocks beta 1 only, decreases blood pressure and heart rate with fewer side effects Uses o High blood pressure and angina Side effects/adverse reactions o HA, dizziness, hypoglycemia, fatigue, depression, and blood dyscrasias Drug interactions o Decreased effects with NSAIDs o Decreased effects with alpha blockers, atropine, and anticholinergics Anticholinergics block the cholinergic/parasympathetic nervous system o Increased risk of hypoglycemia with insulin and sulfonylureas Monitor blood sugar levels Chapter 16: Cholinergic Agonists and Antagonists Cholinergic Agonists Stimulates the PNS o Rest and digest o Muscarinic and nicotinic receptor sites o Mimics the PNS neurotransmitter acetylcholine/acetylcholinesterase Cholinergic Receptors o Muscarinic receptors Affects smooth muscles o Nicotinic Receptors Affects skeletal muscles Works in the eye, lungs, heart, blood vessels, GI, bladder, and salivary glands Also known as parasympathomimetics, muscarinic agonists, or cholinesterase inhibitors Effects of Cholinergic Agonists Heart o Decreases heart rate and blood pressure, vasodilation, slows AV conduction Rest and digest state Eyes o Constricts pupils, increases accommodation, increases lacrimation We no longer need more light let in to see better Lungs o Bronchial constriction, increases secretions Urinary o Stimulates urination by allowing bladder to relax GI o Increases gastric secretions/emptying Muscles o Maintains muscle strength and tone Will not contract like we need in fight or flight, but will maintain tone and strength Direct Acting Cholinergic Agonists Selective to muscarinic receptors o Smooth muscle receptor sites Located in the smooth muscles o Heart, GI, GU, glands Medications o Metoclopramide Increases gastric emptying Used a lot in GI disorders o Pilocarpine Constricts pupils o Bethanechol Increases urination Used in patients that have issues emptying the bladder Side Effects/Adverse Reactions o Blurred vision, miosis o Hypotension, bradycardia o Increased secretions, GI distress (stomach is ramping up) o Bronchoconstriction Contraindications o Bradycardia, hypotension, COPD, peptic ulcer, Parkinsonism, hyperthyroidism Not used to cure, but used to help in Parkinsonism and hyperthyroidism Bethanechol Cholinergic agonist will lower blood pressure and heart rate o Due to decrease in blood pressure, bethanechol can cause postural hypotension Interventions o Monitor heart rate and blood pressure o Teach patient to rise slowly (to prevent orthostatic hypotension) o Record/monitor I&Os o Assess and monitor lung sounds bronchoconstriction o Give 1 hour before meals (ac) or 2 hours after meals (pc) o Assess/monitor bowel sounds to make sure the GI tract is not over doing it Uses o Used to increase urination o Only to be used for urinary retention (not caused by an obstruction) From injury, will only increase bladder contraction to get urine out More of a muscle issue Antidote o Atropine Indirect-Acting Cholinergic Agonists Work with the parasympathetic do not work directly, but rather work around it Functions o Breaks down AChE into choline and acetic acid o Allows Ach to activate muscarinic and nicotinic (cholinergic) receptors Effects o Stimulates skeletal muscle; increases tone o Greater GI motility, but can cause bradycardia, miosis o Bronchial constriction, promotes urination Contraindications/caution o Intestinal and urinary obstruction; asthma/COPD Classifications o Reversible (Neostigmine, Physostigmine, and Donepezil) Medications can be counteracted if there is too much Used to treat glaucoma and used to improve muscle strength in myasthenia gravis patients o Irreversible (Echothiophate) Very hard to reverse Used to treat glaucoma, but can be seen in nerve agents and insecticides SLUDGE Too much of a cholinergic agonist cholinergic crisis Parasympathetic system is working in overdrive S: salivation L: lacrimation (crying) U: urination D: diarrhea G: gastric or vomiting E: emesis (vomiting) Three killer B’s o Bradycardia o Bronchospasm o Bronchorrhea (respiratory depression) To reverse a cholinergic crisis ATROPINE Reversible vs. Irreversible Reversible o Pupil constriction in glaucoma, increases muscle strength in myasthenia gravis o Muscle cramps, twitching, bradycardia, GI cramps Irreversible (Echothiophate) o Produces pupillary constriction in glaucoma, potent due to long lasting effects Takes days to weeks for the medication to leave the system o Increased secretions, bradycardia, GI effects Anticholinergics Action o Inhibit the action of Ach by occupying Ach receptors o By blocking the parasympathetic nerves, the sympathetic system will dominate AKA o Cholinergic blocking agonists, cholinergic or muscarinic antagonists, antiparasympathetic agents, antimuscarinic agents, and antispasmodics, parasympatholytic Effects o Heart Large doses will increase heart rate o Lungs Bronchodilation o GI Slows motility o GU Increases sphincter constriction o Eye Dilates pupils, decreases accommodation o Glands Decreases secretions o CNS Decreases tremors and rigidity Why we use in Parkinson patients Too many anticholinergics: o Hot as Hare High temperatures, no sweating o Mad as a Hatter Confusion, delirium o Red as a Beet Flushed face, tachycardia o Dry as a Bone Decreased secretions, thirsty, dry mouth REMEMBER: anticholinergic toxicity can mimic a psychotic break or psychotic episode o Psychotic breaks DO NOT have dry mouth, hyperthermia, or dry skin Treatment for anticholinergic crisis: physostigmine Atropine Most common use: when patients are bradycardic for no reason & are not tolerating the decreased heart rate Action o Increases pulse, decreases motility and peristalsis, as well as salivary secretions Side effects/adverse effects o Dry mouth and skin, blurred vision, photophobia, tachycardia, congestion, flushing, and urinary retention o DO NOT WANT TO USE IN GLAUCOMA PUPIL CONSTRICTION o Used as a pre-op intervention to decrease salivary secretions want to prevent aspiration Nursing interventions o Monitor vital signs, urinary output, and bowel sounds Watch blood pressure and heart rate o Monitor safety Dizziness, tachycardia, low blood pressure o Provide mouth care and eyedrops Drying of secretions o Avoid hot environments When we dry up secretions, they do not have the ability to sweat o Avoid ETOH, cigarettes, caffeine, and ASA at bedtime Can counteract the normal side effects o Wear sunglasses in bright light photophobia o Teach to avoid motor vehicles or participating in activities which require alertness o Encourage intake of foods high in fiber Because atropine decreases GI motility, which leads to constipation o These medications can cause confusions bed alarm to improve safety Motion Sickness Treated using anticholinergics (classified as antihistamines) o Scopolamine o Dimenhydrinate (Dramamine) o Meclizine HCl (Antivert) Side Effects o Dries secretions, facial flushing, muscle weakness, drowsiness, hypotension, and tachycardia Chapter 37: Cardiac Glycosides, Antianginals, and Antidysrhythmics Heart Failure 101 Patho o In acute heart failure, the heart muscle weakens and enlarges (cardiomegaly) o It then loses its ability to pump blood adequately o Compensatory mechanisms then fail Decrease in cardiac output will enter into acute heart failure o Results in congestion of blood in the lungs (left sided) or periphery (right sided) Right sided o Blood backs up in the periphery o Right ventricle cannot pump sufficiently to pump blood into the lungs for oxygenation Left Sided o Blood backs up in the lungs o Left ventricle cannot work efficiently to pump blood into systemic circulation BNP o How we judge heart failure o Brain natriuretic peptide o Secreted from atrial cardiac cells and aids in the diagnosis of HF o Normal Range: < 100 pg/mL Can slightly elevate in patients that are obese or elderly Cardiac Glycosides Digitalis preparations (Digoxin) Actions o Positive inotropic: increases myocardial contractility o Negative chronotropic: decreases heart rate o Negative dromotropic: decreases conduction o Increase in stroke volume=increase in cardiac output Uses o Heart failure o Atrial fibrillation (A-fib) o Atrial flutter (A-flutter) Contraindications o Certain dysrhythmias Bradycardia o Hypothyroidism o Renal disease Will mess with the kidney issues lowers heart rate, therefore lowering kidney perfusion Drug interactions DOES NOT PLAY WELL WITH OTHERS o Diuretics: hypokalemia can send patients into a worsening dysrhythmia o Glucocorticoids: Na retention hypernatremia o Antacids: decreased absorptions patient is not receiving all of the effects they should o Use caution with herbal supplements because digoxin is derived from a plant Side Effects o Anorexia, HA, fatigue o Visual disturbances o Drowsiness o Bradycardia Interventions o Apical pulse FOR A FULL MINUTE Atrium could be contracting faster than the ventricles o Teach signs of toxicity o Hold if heart rate is <60 o Monitor Dig levels and K+ (whether they are in the hospital or at home) o Monitor for edema If we are holding on to sodium, we are also holding onto water Dig Toxicity o Severe bradycardia o Intense headaches that lead to visual disturbances: white/green/yellow halos Angina Acute cardiac pain caused by a temporary inadequate blood flow to the myocardium either due to plaque occlusions, or spasms of the coronary arteries o Should alert the person that their heart isn’t as well as it should be; Precursor to a heart attack Classic o Occurs with predictable stress or exertion; resolves with rest Ex: running on a treadmill Unstable o Occurs frequently with progressive severity unrelated to activity; not resolved with rest o Not influenced by stress/exertion; unpredictable in intensity “What were you doing when it started?” CLASSIC AND UNSTABLE ANGINA ARE BIG PRECURSORS OF A POTENTIAL MI Variant o Occurs during rest o Due to the coronary vasospasms o AKA Printzmetal or vasospastic Antianginal Drugs Nitrates o Reduction of venous tone o Decreases workload of heart o Vasodilation Beta Blockers o Decreases workload of the heart and oxygen demands CCB o Decreases workload of the heart and oxygen demands Nonpharmacological treatments: o Avoid heavy meals o Quit smoking o Avoid extreme weather changes (variant) o Avoid/decrease strenuous exercise o Emotional upset/stress Nitrates Nitroglycerin o Action Vascular and coronary vasodilation Decreases preload and afterload Heart will not stretch as much and will not have to work as much o Contraindications Hypotension, increased ICP, severe anemia, on erectile dysfunction (ED) medications Never give to a patient with a systolic BP of 100 o Side effects/adverse reactions Headache!!! can give OTC non-opioid medications (Tylenol) Decreased BP, vasodilation, reflexive tachycardia Fatigue and mental status changes o Transdermal patch Apply to hairless area Use new patch-new site- every day educate patient to rotate sites o Patch free hours (10-12 hour gap between each patch) o Wear gloves!!! o Do not apply in areas where defibrillation may be needed patches usually go on arms Oral extended-release capsule and tablet o Do not chew or crush o Given sublingually!!!! Aerosol spray (inhalation, translingual) o As the nurse, do not inhale wear a mask upon administration! Take one on the onset of angina; if no relief in 5 minutes, call 911. Can take one every 5 minutes for up to 3 doses total Assess vitals (BP and HR) and pain scale every 5 minutes (before each dose) if in the hospital Beta Blockers Decrease heart rate and blood pressure Decreased workload/O2 demand Atenolol and Metoprolol Calcium Channel Blockers Relax coronary artery spasms good for vasospastic angina patients (variant) Decreased peripheral resistance allows stuff to pass through without the spasms Amlodipine and diltiazem Anti-Dysrhythmic Drugs Arrhythmia vs. dysrhythmia o Arrhythmia: absence of rhythm (flatline) o Dysrhythmia: deviation of the normal rate or heart rhythm Types o Atrial Prevent proper filling of the ventricles and decrease cardiac output Can live with these and not even know o Ventricular Life-threatening; causes ineffective filling of the ventricles, leading to decreased or absent cardiac output cannot live with these rhythms Antidysrhythmic drugs o Goal: restore the cardiac rhythm to normal o Keeps the dysrhythmias from getting to severe o Can be prodysrhythmic o DO NOT WANT THE PATIENT TO GET TO RAPID A-FIB o Classes (TABLE 37.5) Fast (sodium) channel blockers, beta blockers, drug that prolong repolarization, and slow (Ca+) channel blockers Class 1 Sodium Channel Blockers (-amide) o Decreases Na influx into cardiac cells o Decreased conduction velocity in the cardiac tissues, suppresses automaticity, and increases recovery time o Slows down conduction pathway so the conduction has time to get through Sub classes o 1A: slows conduction, prolongs repolarization (procainamide, quinidine) o 1B: slows conduction, shortens repolarization (lidocaine) Key medication to treat ventricular dysrhythmias Deadly dysrhythmias=LIDOCAINE o 1C: prolonged conduction with little/no effect on repolarization (flecainide) Side effects o Hypotension, heart failure, new or worsening dysrhythmias, N/V/D Nursing Interventions o Obtain thorough health and drug history certain drugs can induce dysrhythmias o Labs (CBC, CMP, and CEs(cardiac enzymes)) troponin o Vital signs and continuous cardiac monitoring will be hooked up to a telemetry machine o Monitor for signs of edema o Monitor thyroid, respiratory, and neurological function o Teach patient to avoid caffeine, ETOH, and tobacco, low sodium diet Caffeine and tobacco are stimulants and ETOH has diuretic properties Chapter 38: Diuretics Diuretics Induce voiding produces fluid removal from the body Uses o Decrease hypertension o Decrease edema in HF and renal/liver disorders o Main action: diuresis Action o Produce diuresis by stopping sodium (Na) and water reabsorption in the kidney tubules Types o Thiazide and thiazide-like o Loop or high-ceiling o Osmotic o Carbonic anhydrase inhibitor o Potassium-sparing Patho background: o 50-55% of sodium reabsorption occurs in the proximal tubules o 35-40% of sodium reabsorption occurs in the Loop of Henle o 5-10% of sodium reabsorption occurs in the distal tubules o 2-3% in the collecting ducts o Diuretics that act of tubules closer to the glomeruli are going to have the greatest effect on diuresis Thiazide Diuretics Action o Acts on distal convolluted renal tubules o Promotes Na+, Cl-, and H2O excretion all follow each other Use o Hypertension and peripheral edema Medications o Hydrochlorothiazide (HCTZ), Metolazone Chemistry Abnormalities o Hypokalemia, hypomagnesemia o Hypercalcemia, hypochloremia o Hyperuricemia, hyperglycemia, and hyperlipidemia Side Effects o Dizziness, headache, GI distress, electrolyte imbalances Nursing Interventions o TEACH TO TAKE IN THE MORNING o VS, I&Os, daily weight (at home or in the hospital) o Monitor labs o Avoid salt and calcium rich foods o Sun precautions necessary o Monitor and educate regarding orthostatic hypotension rise slowly, change position slowly o Contraindicated in renal patients and patients taking lithium Loop Diuretics Action o Acts on the ascending Loop of Henle o Excretes Na, H2O, K, Ca, and Mg Uses o HTN, pulmonary edema, peripheral edema r/t heart failure, hypercalcemia, and renal disease Medications o Furosemide, bumetanide Caution o More potent diuretic; can cause more rapid diuresis with decreases in vascular fluid volume, cardiac output, and BP Lab changes sodium, water, potassium, calcium, magnesium Nursing Considerations o Same as thiazide diuretics o Because loop diuretics are more potent, there is an increased risk of hypotension teach how to take BP; need to take daily o Always taken with food to help with absorption Osmotic Diuretics Mannitol o Action Increases Na reabsorption in the proximal tubules and Loop of Henle Excretes, Na, Cl, K, and H2O o Uses Prevent kidney failure if creeping towards stage 1, we can use to prolong kidney life Decrease ICP and IOP o Side Effects Electrolyte imbalances, pulmonary edema, GI distress, tachycardia, and headache Contraindicated in heart and true renal failure o Need to remember: solution; cannot give if the medication has any crystals present K+ Sparing Diuretics Action o Blocks action of aldosterone o Promotes Na/H2O excretion and K+ retention o Mild diuretic; can be used in combo with others; would still need to keep an eye on Uses o Edema, HTN, increase urine output (because more mild diuretic), ascites, hypokalemia Medications o Spironolactone, amiloride, and triamterene Side Effects o Hyperkalemia, GI distress o Weakness o Photosensitivity Contraindications o Severe renal/hepatic disease and in hyperkalemia need to look at K+ levels before admin o Use caution with DM, other HTN meds, and ACE inhibitors (increased K+ levels) Nursing considerations o Avoid foods high in potassium