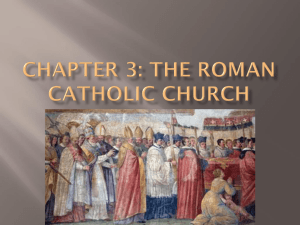
Prepared by Kurt Schaberg Kidney Tumors Eosinophilic Oncocytoma CK7 CD117 CA-IX Vimentin AMACR Racemase SDH FH - + - - - + + (rare) Chromophobe RCC + + - - - + + Papillary RCC (Type 2) +/- - +/- + + + + HLRCC-associated RCC - - - - - + -! SDH-deficient RCC - - - - +/- -! + Acquired Cystic Disease-associated RCC - + + + Clear Cell RCC (sometimes pinkish) - - + + - ++ + Oncocytoma Benign Abundant eosinophilic, mitochondria-rich cytoplasm Round, regular nuclei throughout Tight nests and alveoli surrounded by myxoid or hyalinized hypocellular stroma. Some solid areas acceptable. Grossly: Circumscribed, mahogany brown NOT allowed: Necrosis, Sheet-like or papillary growth, clear or sarcomatoid cells Stains: Only rare CK7 + cells (Most CK7 Negative!) Chromophobe Renal Cell Carcinoma Clear to Eosinophilic cytoplasm Prominent “Plant-like” cell membranes Perinuclear clearing Round to Koilocytic nuclei (hyperchromatic, crinkled, and/or binucleated) Stains: CK7+, Hale’s colloidal iron + Better prognosis than clear cell RCC. No need to grade. Chromophobe/oncocytoma hybrid tumors may be seen in Birt-Hogg-Dubé syndrome Papillary RCC (Type 2) Predominantly papillary architecture Type 2 is lined by large cells with abundant eosinophilic cytoplasm Higher nuclear grade→ Prominent Nucleoli (consider HLRCC though!) Macrophages, edema, psammoma bodies Hereditary Leiomyomatosis and Renal Cell Carcinoma-associated RCC Abbreviated: HLRCC-associated RCC Prominent, eosinophilic, inclusion-like nucleoli with perinucleolar clearing Usu. Papillary to tubular architecture Loss of Fumarate Hydratatse (FH) expression (Germline FH mutations) Usually younger patients. Cutaneous and uterine leiomyomas. Aggressive tumors! Succinate Dehydrogenase Deficient RCC Eosinophilic cytoplasm with “flocculent” cytoplasm/inclusions (see arrows) Neuroendocrine-like nuclei (round, evenly dispersed chromatin Solid to nested architecture Defined by loss of Succinate Dehydrogenase B (SDH-B)→ Majority of patients have germline mutations. Young age, good prognosis SDH-deficient tumor syndrome: SDH-deficient RCC, paraganglioma/pheochromocytoma, SDHdeficient GISTs Acquired Cystic Disease-associated RCC Occurs only in patients with ESRD with cystic disease Abundant granular eosinophilic cytoplasm Microcribriform appearance due to frequent intracytoplasmic and intercellular microlumens Large nuclei with prominent nucleoli Frequent oxalate crystals and calcifications Clear Cell RCC Although it is called “Clear Cell” RCC, some cases can have relatively eosinophilic cytoplasm. More common with higher grades Can have “Rhabdoid” areas Look for classic clear cell areas as a clue Clear Clear Cell RCC CK7 CD10 CA-IX Keratins/ EMA Melanocytic Markers TFEB/ TPF3 - + + + - - + (basal + - - (diffuse) Clear Cell Papillary RCC + Multilocular cystic renal cell neoplasm of LMP - + + + - - MiTF translocationassociated RCC - + - - (weak to neg) +/- + - cup-like) Clear Cell RCC Predominantly clear cells (contains lipid and glycogen) with sharp cell borders Sheets and nests of cells surrounded by extensive capillary network Frequent alveolar lumens Grossly: Yellow, with frequent hemorrhage and necrosis Associated with von Hippel Lindau Syndrome (VHL gene)—Along with: Hemangioblastomas, pheochromocytoma, pancreatic serous cystadenomas, and endolymphatic sac tumor WHO/ISUP grading system for clear cell and papillary renal cell carcinomas Grade Findings 1 Nucleoli are absent or inconspicuous and basophilic at 400x magnification 2 Nucleoli are conspicuous and eosinophilic at 400x and visible but not prominent at 100x 3 Nucleoli are conspicuous and eosinophilic at 100x 4 Extreme nuclear pleomorphism, multinucleate giant cells, and/or rhabdoid and/or sarcomatoid differentiation Multilocular Renal Cell Neoplasm of Low Malignant Potential Cysts lined by single layer of low-grade clear cells (grade 1-2 only) Groups of low-grade clear cells are permitted within the septa, but must not be expansile nodules or show infiltrative growth Features not allowed: Necrosis, Vascular invasion, Sarcomatous differentiation NOTE: No longer called a carcinoma as act so indolently Clear Cell Papillary RCC Mixture of tubular, cystic, acinar and papillary patterns Lined by a single layer of cuboidal to low columnar cells Scant eosinophilic to clear cytoplasm Nuclei apical to mid-cytoplasmic orientation (“pseudoendometrial” appearance) Low-grade and Low-stage Unique immunophenotype (CK7 +, CA-IX basolateral cuplike) Very indolent (no reported metastases!) MiT Family Translocation RCC Gene fusions in MiT family transcription factors TFE3 or TFEB (Demonstrate with cytogenetics, FISH, or IHC) Composed of cells with abundant to voluminous cytoplasm Clear to granular eosinophilic cytoplasm Sharp cell borders Frequent papillary, pseudopapillary, alveolar and nested patterns Vesicular nuclei with prominent nucleoli Most often recognized in younger patients Variable outcomes Basaloid Papillary RCC (Type 1) CK7 CD10 CA-IX AMACR Racemase WT-1 CD57 + + -/+ + - - - - + + - - + - (luminal) Metanephric Adenoma - Wilms Tumor -/+ (in + epithelium) (diffuse) Mucinous Tubular and Spindle Cell RCC + -/+ - + - - Tubulocystic RCC +/- + -/+ + - - Papillary RCC (Type 1) Predominantly papillary architecture Often some tubular or solid growth also Type 1 is lined by small cells with scant amphophilic cytoplasm Lower nuclear grade than type 2 Macrophages, edema, psammoma bodies Papillary Adenoma Same thing, but < 1.5 cm Nuclear grade 1 or 2 Benign Metanephric Adenoma Benign Composed of small, primitive tubules. Cells have minimal cytoplasm with uniform, small nuclei Minimal mitoses. Grossly: well-circumscribed, unencapsulated, tan nodule. Very cellular with minimal stroma. May appear papillary or glomeruloid Often incidental, but associated with polycythemia Tubulocystic RCC Closely packed variably sized tubules and cysts No solid component→ Grossly looks like a sponge Lined by cuboidal to flattened and hobnail cells High grade nuclear features with prominent round nucleoli Good Prognosis Grossly looks like a sponge Wilms Tumor (Nephroblastoma) 1 Vast majority in Children Triphasic (recapitulating nephrogenesis): 1) Blastema (small, undifferentiated, overlapping cells) 2) Epithelium (Tubules, rosette-like to well-formed) 3) Stroma (Nondescript spindled cells, occasional heterologous elements) 2 3 Special reporting (amount of Anaplasia, etc…) Anaplasia = increased nuclear size (>3x size), hyperchromasia, and mitotic figures → Chemo resistant Malignant, but often good survival Mucinous Tubular and Spindle Cell Carcinoma Like the name says: 1) Elongate tubules that blend into 2) Bland spindle cells, set in 3) Mucinous stroma 2 Cytologically bland with small oval nuclei Very indolent/benign course 1 3 Spindled (Adult) Angiomyolipoma Benign Member of “PEComa” family (Perivascular Epithelioid Cell) Generally 3 components (like the name): 1) Blood vessels (“Angio”) 2) Smooth muscle (“Myo”)—often blending with vessels 3) Fat (“Lipoma”)—often seen radiographically Stains with Melanocytic Markers: HMB45 +, MelanA +/-, Desmin + (in muscle) Associated with Tuberous sclerosis Renomedullary Interstitial Cell Tumor Benign Usually incidental, small, well-circumscribed Located in renal medulla Composed of bland stellate cells set in loose to dense fibrocollagenous stroma with entrapped tubules at the periphery Sarcomatoid RCC Renal cell carcinoma of any type exhibiting at least focal sarcomatoid/spindle cell differentiation Represents a form of high-grade transformation, not a distinct subtype of renal cell carcinoma Requires evidence of epithelial differentiation (either conventional component or CK expression) Automatically WHO/ISUP grade 4 Poor prognosis Other Spindled Tumors Mixed-Epithelial Stromal Tumor—Benign tumor. Cystic and solid. Ovarian-type stroma and smooth muscle with bland epithelial cysts (conceptually sort of like a mucinous cystic neoplasm of the pancreas, but epithelium is hobnailed and bland). Stroma stains with desmin and ER. Juxtaglomeurlar Cell Tumor—Benign tumor that originates from smooth muscle cells in the walls of the glomerular afferent arteriole (juxtaglomerular apparatus)→ secretes renin→ Hypertension, Hyperaldosteronism, hypokalemia! Monotonous eosinophilic spindled to epithelioid cells with oval nuclei. Mucinous tubular and spindle cell carcinoma Sarcomatoid clear cell RCC Renomedullary interstitial cell tumor (And any other sarcoma pretty much) High-Grade Collecting Duct Carcinoma High-grade renal carcinoma arising in medulla of the kidney, with a predominantly invasive tubular growth pattern. Diagnosis of exclusion. Requires: 1) No other RCC, Urothelial carcinoma, or Metastasis 2) Predominantly tubular growth 3) Firm mass centered in Medulla 4) Prominent stromal desmoplasia 5) Infiltrative growth 6) High nuclear grade Poor Prognosis Urothelial carcinoma Always consider as a possibility if doesn’t fit well into one of the RCC diagnoses. Sample and examine the renal pelvis for urothelial CIS Stains: GATA-3 +, p63+, HMWCK+, CK7+, CK20+, Pitfalls: PAX8+, CA-IX + Other Renal Medullary Carcinoma—Like collecting duct carcinoma, but associated with sickle cell disease, INI-1 loss Sarcomatoid clear cell RCC, RCC NOS, Metastases, Sarcomas Papillary Papillary adenoma Papillary RCC Clear cell papillary RCC MiTF translocation-associated RCC Urothelial carcinoma HLRCC-associated RCC Spindled (Kids) Clear Cell Sarcoma Aggressive→ Old name “bone metastasizing renal tumor of childhood” Nests or cords of uniform cells with clear cytoplasm and fine chromatin and a delicate vascular network Some areas may be sarcomatous/anaplastic No good stains Rhabdoid Tumor Aggressive Sheets and trabeculae of cells with: Eccentric nuclei with vesicular chromatin and prominent nucleoli Eosinophilic cytoplasm with pink hyaline inclusions (looks “rhabdoid”) Stains: CK+, INI-1 loss, Myogenin/MyoD1 - Congenital Mesoblastic Nephroma Classic Variant Fibromatosis-like: intersecting bundles of bland spindled cells, infrequent mitoses Infiltrates adjacent kidney and structures Cellular Variant Recurrent ETV6-NTRK3 fusions (Same as infantile fibrosarcoma, secretory carcinoma) Pushing border, dense cellularity, numerous mitoses Biopsy/FNA Algorithm