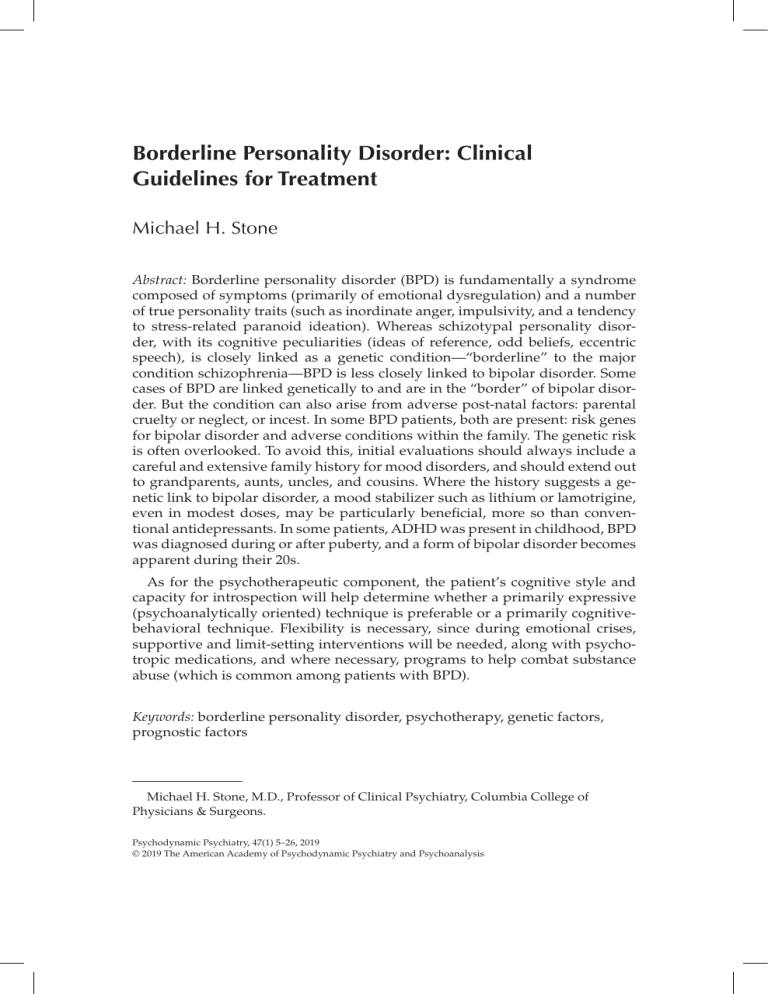
STONE CLINCIAL TREATMENT GUIDES FOR BPD Borderline Personality Disorder: Clinical Guidelines for Treatment Michael H. Stone Abstract: Borderline personality disorder (BPD) is fundamentally a syndrome composed of symptoms (primarily of emotional dysregulation) and a number of true personality traits (such as inordinate anger, impulsivity, and a tendency to stress-related paranoid ideation). Whereas schizotypal personality disorder, with its cognitive peculiarities (ideas of reference, odd beliefs, eccentric speech), is closely linked as a genetic condition—“borderline” to the major condition schizophrenia—BPD is less closely linked to bipolar disorder. Some cases of BPD are linked genetically to and are in the “border” of bipolar disorder. But the condition can also arise from adverse post-natal factors: parental cruelty or neglect, or incest. In some BPD patients, both are present: risk genes for bipolar disorder and adverse conditions within the family. The genetic risk is often overlooked. To avoid this, initial evaluations should always include a careful and extensive family history for mood disorders, and should extend out to grandparents, aunts, uncles, and cousins. Where the history suggests a genetic link to bipolar disorder, a mood stabilizer such as lithium or lamotrigine, even in modest doses, may be particularly beneficial, more so than conventional antidepressants. In some patients, ADHD was present in childhood, BPD was diagnosed during or after puberty, and a form of bipolar disorder becomes apparent during their 20s. As for the psychotherapeutic component, the patient’s cognitive style and capacity for introspection will help determine whether a primarily expressive (psychoanalytically oriented) technique is preferable or a primarily cognitivebehavioral technique. Flexibility is necessary, since during emotional crises, supportive and limit-setting interventions will be needed, along with psychotropic medications, and where necessary, programs to help combat substance abuse (which is common among patients with BPD). Keywords: borderline personality disorder, psychotherapy, genetic factors, prognostic factors Michael H. Stone, M.D., Professor of Clinical Psychiatry, Columbia College of Physicians & Surgeons. Psychodynamic Psychiatry, 47(1) 5–26, 2019 © 2019 The American Academy of Psychodynamic Psychiatry and Psychoanalysis 6 STONE Establishing guidelines for the treatment of borderline personality disorder (BPD) is a particularly daunting task. This is so for a number of reasons. To begin with, BPD is albeit a psychiatric disorder, not a true personality disorder in the same sense as, for example, compulsive, dependent, or avoidant disorders. The true personality disorders need not be accompanied by symptom-disorders (such as social anxiety, anorexia, substance abuse, depression), whereas BPD is always accompanied by identifiable symptom-disorders. The latter of course have a bearing on what would be the appropriate treatment measures. Further, because it is not necessary to manifest all the diagnostic descriptors (items) for BPD, many combinations of the diagnostic items will suffice—as long as patients have the minimum number to establish the BPD diagnosis—but, as a result, will describe patients who differ considerably from one another. A patient with identity disturbance, mood lability, and chronic feelings of emptiness, for example, will differ considerably from a BPD patient with marked impulsivity, tendencies to self-harm and suicidal gestures, and inordinate anger. The treatment approach will likewise differ considerably. A patient of the latter type will require much more in the way of limit-setting and medication than would be necessary for the less action-prone patient. The cognitive style of the patient also figures importantly into the equation. BPD patients who are highly reflective and introspective may respond well with a psychodynamic therapy, such as expressive (Gunderson, 2001), transference-focused psychotherapy (TFP) (Kernberg et al., 1989; Kernberg, Yeomans, Clarkin, & Levy, 2008), or mentalization-based treatment (Bateman & Fonagy, 2004). Other BPD patients of a different cognitive style may make better progress with a different modality, such as dialectic behavior therapy (DBT; Linehan, 1993) or schema-based therapy (SBT; Young, Klosko, & Weishaar, 2003). Another important and often neglected consideration pertinent to the treatment of patients is the genetic factor. Whereas patients with schizotypal personality may routinely be understood as within the penumbra of schizophrenia, and often have schizophrenic relatives, borderline patients—in a smaller, but still significant percentage of cases—have relatives in the manic-depressive spectrum, including those with recurrent depressive disorders or others within the bipolar spectrum. Many BPD patients themselves can eventually be diagnosed with either a bipolar I or a bipolar II disorder. The latter is characterized as consisting of hypomanic episodes alternating with severe periods of depression. The importance of the genetic factor underpinning psychological attributes in general was emphasized recently by Robert Plomin (2018). He cautions, for example, that, “There is no point at which genetic risk tips over into pathology. We all have thousands of DNA differences that CLINCIAL TREATMENT GUIDES FOR BPD 7 predispose us to schizophrenia; genetic risk depends on how many of these differences we have. It’s all quantitative…a matter of more or less. Genetically speaking, there are no disorders, just dimensions” (p. 1). In this regard, many BPD patients may be understood dimensionally as within the bipolar spectrum. In order to better to ascertain the degree of genetic susceptibility, it is important to take a family history in one’s initial interviews with borderline patients, including if possible two or three generations of relatives—extending out to grandparents, aunts, uncles, and cousins. This exercise will be all the more relevant when assessing those BPD patients who have not been highly traumatized or sexually molested: In these patients, absent the post-natal (environmental) factors that conduce to the development of BPD, genetic predisposition is apt to weigh more heavily in the balance of contributing factors. Among the 71 BPD patients I have worked with over the years, 68 were female—13 of whom (19%) had been incest victims. Thirteen were themselves bipolar and came from families with a history of bipolar relatives. There was an overlap group of six patients who had been both incest victims and diagnostically bipolar. In my long-term (10- to 25-year) follow-up study of hospitalized borderline patients, 28 of the 145 female patients had been incest victims—the same percentage as noted in my private-patient series (19.3%). Three of the hospitalized patients (in what I called the PI-500 study) had later committed suicide (Stone, 1990), but it was encouraging to note that about half of these 28 patients were doing fairly well at follow-up (with a Global Assessment Score of 61 to 70 in six cases) or quite well (GAS score 71 or higher). The incest factor may help account for the lopsided sex distribution among BPD patients (which is usually at least 3:1 in most series), since females are much more likely to be victims of incest than men, and the psychologically damaging effects of incest (as well as of other forms of sexual molestation) often include long-lasting distrust of men (or in some cases to promiscuity) and thus to the “stormy relationships” that constitute one of the BPD diagnostic items, as well as to depression. Women are already more vulnerable to depression than men, while men are more prone than women to develop what Annett Schirmer called “disorders of antisocial emotions” (Schirmer, 2013, p. 605). “Mood lability” (often with episodic depression) is yet another BPD item. The BPD item “inordinate anger” may be linked either to bipolar spectrum psychopathology or to having been abused sexually or physically during one’s early years. Some patients have of course experienced both: the genetically predisposed mood disorder and the environment-related molestation. In line with Plomin’s emphasis on a “dimensional” approach to diagnosis, I had earlier offered various examples related to the interaction of the genetic predisposition (depending on its strength) to bipolar spec- 8 STONE trum disorders and the level of adverse environment (Stone, 2013). Different scenarios were discussed. If, for example, one had a high genetic risk for bipolar disorder but had grown up in a tranquil, non-abusive environment, the eventual illness might consist of bipolar disorder combined with BPD (more likely in female patients). In a similarly tranquil home, someone with just moderate genetic risk for bipolar disorder might emerge with a bipolar spectrum condition—but without the BPD. Moderate genetic risk but coupled with an adverse environment (that might also include incest) would then predispose to the combined condition: bipolar disorder plus BPD. Absent any significant genetic risk, however, a highly adverse environment would predispose just to BPD alone. The section that follows provides examples of BPD patients from families with varying degrees of genetic risk. GRADATIONS OF GENETIC RISK FOR SERIOUS MENTAL ILLNESS: ILLUSTRATIVE EXAMPLES AND TREATMENT IMPLICATIONS Patient A was diagnosed with BPD at 22 when she was hospitalized shortly after the birth of her son. Her husband of two years had abandoned her in the middle months of her pregnancy. She reacted to this with severe depression and suicidal gestures (self-cutting). Three years earlier, both her parents had committed suicide in a suicide pact prompted by her father’s business failure. Her father had been diagnosed with bipolar I disorder, and her mother had been hospitalized numerous times with what was called paranoid schizophrenia. She had been alternatingly rejecting and physically abusive toward her daughter during her first 12 years, but had then switched to becoming increasingly dependent on her throughout her adolescence. The mother’s father had been treated for a paranoid disorder, and both of her father’s sisters had been hospitalized on a few occasions for severe depression. After leaving the hospital, patient A was able to complete college and work in the financial industry. In the years that followed, she remained in psychotherapy and had a series of turbulent romantic relationships, though she never remarried. Her most prominent borderline features were mood-lability, inordinate anger, tempestuous interpersonal relationships, stress-related paranoid ideation, and efforts to avoid abandonment. Another prominent abnormality consisted of an inability to understand and relate properly to social cues, always “saying the wrong thing,” after the manner of people with Asperger syndrome (i.e., high functioning within the autistic spectrum disorders). She has continued CLINCIAL TREATMENT GUIDES FOR BPD 9 in twice-weekly psychotherapy (initially of a psychodynamic nature; more recently, primarily supportive). Medications have consisted of antidepressants and anti-anxiety agents, occasionally supplemented with small doses of an antipsychotic drug (aripiprazole/Abilify) and moodstabilizers (lithium and lamotrigine in small doses). A willingness for sex allowed her to retain close relationships with men for extended periods, but now in her mid-70s this has no longer been possible. She has never had close friendships with women, and now is burdened with loneliness and a diminished capacity for enjoyment. Psychotherapy at this point is purely supportive, with an emphasis on teaching her, when meeting someone new, to ask what the other person thinks about some important topic of the day, rather than blurting out her own view— which is usually extreme and off-putting, tending only to alienate the other person and preventing a friendship from developing. Patient B has been in psychotherapy almost continually since her mid-teens. Her mother and brother suffered from recurrent depression; both were also narcissistic and rejecting in their attitude toward her. The maternal grandfather had carried on an incestuous relationship with her for the five years between ages eight and thirteen. A paternal aunt was bipolar. In the aftermath of the incest (which included intercourse), the patient became morbidly obese as she entered her 20s— with the conscious idea that by making herself unattractive to men in that way, she could avoid being taken advantage of. She did eventually marry, however, and had three children (all boys). The eldest son had attention-deficit disorder with hyperactivity in adolescence, culminating in a distinct bipolar I disorder as he entered his 20s. The middle son was diagnosed with BPD in late adolescence, largely because of his impulsivity, angry outbursts, and mood lability. He also abused hallucinogens. I began working with the patient when she was in her mid-30s, shortly after she was released from the hospital because of a suicide attempt in the midst of violent arguments with her husband. Treatment consisted initially of twice-weekly psychotherapy, combining expressive and supportive elements. A highly intelligent and artistically gifted woman, she earned a fair amount of money by painting and selling portraits. Unusually vulnerable to feelings of abandonment, she reacted with intense anger when I was going to miss a few sessions in order to give lectures outside the city. This issue was eventually resolved, and the therapy became more supportive, focusing on conflicts relating to her children. The two older boys were contemptuous of her because of her obesity. They knew nothing about her incest history, and remained judgmental and unsympathetic. At my urging, she underwent bariatric surgery and lost over 100 pounds. She was then less depressed, but still limited in her functioning due to the obesity-related arthritic problems 10 STONE in her legs. Several medications had proven helpful: antidepressants (chiefly fluoxetine), mood-stabilizers (oxcarbazepine/Trileptal and lithium), and—during spells of anxiety—clonazepam. Her relationship with her husband had improved markedly. And during her sessions, she now dwelled less on issues relating to herself and more on the continuing problems with her children. Patient C came from a family where the genetic predisposition to bipolar disorder was notable but where the negative environmental factors were of only moderate proportions. Both parents were professionals, and both were given to episodic depressions of marked severity. The maternal grandfather was a short-tempered and at times violent man. He was considered bipolar but whose manic episodes were marked by extreme irritability rather than by exaggerated cheerfulness. Her older sister had been hospitalized in mid-adolescence for depression and suicidality, and was diagnosed with BPD. Patient C was more sociable and more readily likeable than the other members of her family. While still in graduate school, she married a man who proved to be dour and uncommunicative. After three years, divorce seemed unavoidable; she made a suicide attempt with a drug overdose and had to be briefly hospitalized. I began treating her just after her release from the hospital. The pertinent BPD criteria were her impulsivity, suicidal behaviors, mood lability, stormy relationships with men, and fear of abandonment. In her first dream, she saw herself in a hospital bed, mortally ill; a doctor enters her room. He is quite drunk but reassures her by saying: “Donchu worry, yer gonna be aw-right.” The transference implications were clear: I was no more reliable than her father (who abused alcohol). As she came to trust me more in the months that followed, she now felt she had an ally—someone who would be there for her as she went ahead with the divorce. She did however make one suicide gesture via reckless driving when she separated completely from her husband. The focus in therapy was then on her insecurity and low self-regard that led her to engage in brief affairs with a number of different men. Her attractiveness made it easy for her to find them, but she tended to choose men who treated her shabbily. The men were often much older, and she came to understand that they were father-substitutes who were not more caring or reliable, as it turned out, than her own father. She experienced periods of depression as each of these relationships foundered. Antidepressants offered some relief during this time. After two years, her level of self-confidence improved; she then met a man, a promising young professional whose affection for her was genuine. They married, and she has enjoyed a satisfying life with him for over 20 years, working productively and raising their two children. She would no longer be considered borderline. CLINCIAL TREATMENT GUIDES FOR BPD 11 Patient D came from a family with a modest degree of genetic predisposition to bipolar disorder, but differed from the previous three patients, in that she had not experienced any significantly adverse postnatal factors. She was one of two children raised in an upper middle class family by affectionate parents, both professionals who were never neglectful, abusive, rejecting, or otherwise disagreeable. Her father developed a severe and chronic depression when she was in her early teens and has worked only sporadically since. Her menarche was at 15. The following year, she became severely depressed and suicidal, and was hospitalized for what turned out to be the first of a dozen subsequent admissions for depression and suicide attempts. Although she had always been a straight-A student, she was unable to finish high school until she was 20. Along the way, she developed other conditions, most notably anorexia nervosa (with profound weight loss) and obsessive-compulsive disorder—with a fear of inadvertently harming others. These fears resembled those described by LeGrand du Saulle (1883): she left her books on the floor, for example, lest one of them fall and injure her cat. Occasionally, her depression would be interrupted by a brief hypomanic episode marked by rapid speech and unaccustomed gregariousness. She was diagnosed with both BPD (especially because of the self-damaging acts) and bipolar II. Some felt her borderline disorder was somehow an expression of the underlying bipolar condition, given that she had none of the adverse environmental factors that often precede the development of BPD. After release from a hospitalization in her early 20s, a new psychiatrist focused on what he saw as narcissistic features, placing less emphasis on medication. Not long after, she engaged in another episode of self-cutting and was once again hospitalized. This time, her after-care was conducted by a psychopharmacologist who focused on the bipolar aspects of her condition and prescribed a combination of lithium and clozapine. The latter was in response to her failure in the past to benefit from the conventional antipsychotic medications. With this regimen, she was able to make substantial improvement. She was able to attend college, achieving straight A’s as she had done earlier in high school. She was more selfconfident and began dating, though she continued to be self-conscious about her weight, objectively low as it was, and ate very sparingly. Her mood was brighter, and for the first time she began to look forward to what she now saw as a rewarding future. Patient E was born in Argentina and came to the United States after the death of her father when she was seven. Apart from a sister with mild but recurrent depressions and an aunt with bipolar disorder, the other members of her immediate family did not suffer from mood or other psychiatric disorders. The family was wealthy, including her 12 STONE mother’s second husband whom she married when the patient was 10. The patient idolized her father, who had been a kindly and indulgent man; his death was the major trauma in her life. Her mother was inordinately strict and at times punitive. During her childhood years, if her mother felt she had been “naughty,” she would be strapped to a chair and spanked severely. Her worst punishment came when her mother caught her and a boy (they were both seven) showing each other their sexual parts. This set the stage for one of the major symptoms that emerged during her adolescence, namely, pronounced germ-phobia and related obsessive-compulsive phenomena. She suffered a breakdown during college, made a suicide attempt with pills, and was hospitalized for a lengthy period. Her psychiatrist used a primarily psychoanalytic approach, focusing on the connection between her equating sex with sinfulness. Her symptoms persisted after her release to a point where she could no longer handle money, because it had been touched by so many people. Clothes and bedding were sent daily to the cleaners. Cognitive aberrations developed along similar lines, and this led from her original diagnoses of BPD and bipolar disorder to BPD and schizoaffective disorder. Walking in the street past a fat or pregnant woman made her feel she would somehow become pregnant and fat. In reaction, she became anorectic and quite slender. She was 30 when I began treating her. My initial approach was also psychoanalytically oriented. She was very receptive, worked diligently with dream material, and showed good understanding of the connection between her childhood sexual “sinfulness” and her morbid fear of all things “dirty” and sexual. But the symptoms did not lose their strength. I began to adopt a more behavior-oriented (and to me, less familiar) approach. I asked her once, for example, to hold out her hands. I dropped several dollar bills onto them, and urged her to accept that “you will live to the morrow.” Meaning: nothing bad will happen to you. She gradually became more at ease with handling money and with sleeping several nights in a row without changing the sheets. She began to date a man she had met at a social gathering. She gradually overcame her compunctions about sex. He proposed to her and intimated that he was a man of means. But this turned out to be untrue: he proved to be more in love with her family’s money than with her. She broke the engagement, but became suicidal; her fragility was heightened by her having stopped her antipsychotic medication for several weeks while she was away with him. Upon her return, I restored her medication and went with her to the emergency room, where after a few hours her suicidal feelings abated. This was a turning point. During the next several months, she became less depressed and less symptomatic. She met a much more suitable (and honorable) man—whom she later married. I have maintained con- CLINCIAL TREATMENT GUIDES FOR BPD 13 tact with her over the ensuing 30 years, during which time she raised a son who is now in college and, after completing training, has been working effectively in a mental-health profession. She would no longer be considered either borderline or schizoaffective. Contributing to her emergence from the severe symptomatology of her earlier years were the important (and mitigating) factors of her positive personality traits, such as those emphasized in the five-factor model of Costa and Widiger (2002) and enumerated by Trull and McCrae (2002)—in particular: agreeableness and conscientiousness (Stone, 1993, pp. 112-130). GRADATIONS OF SEXUAL MOLESTATION BY FAMILY MEMBERS AS A RISK FACTOR IN THE DEVELOPMENT OF BPD I recently provided clinical vignettes of patients with BPD who had during their childhood (i.e., prepubescent) and adolescent years been the victims of transgenerational incest (Stone, 2017a). The most common form encountered was father-daughter. Uncles or grandparents were the perpetrators in a few of the other cases. Other forms of incest involving a parent are much less common: father-son, mother-son, and mother-daughter. In over 50 years of practice (and hospital work), I have encountered only one instance of mother-daughter incest. This was a French woman whose mother had abused her when she was a girl of seven or eight. I encountered her as a woman in her 20s with suicidal and self-injury tendencies as well as other borderline features. The inappropriate sexuality of her earlier years seemed to carve out a path of sexual deviance, and she became involved in the pornography industry, but she always lived at the mercy of the men who hired her to take part in porn films. One of the few patients I worked with who had been the victim of father-son incest in adolescence had been raped anally by his father. Enormously angry and resentful, the patient identified as gay, but hated his homosexuality and hated people in general. He contracted AIDS in one of his rare homosexual contacts and died in the early 1980s when the epidemic was at its peak. Mother-son incest was also rare: there were only two cases among the 550 patients in my PI-500 follow-up study (Stone, 1990). Both later committed suicide. I have worked with a third such patient (on an ambulatory basis): this man was eventually able to make an excellent adjustment. Among the larger group of incest victims were women who had been abused by an older male relative or, in rarer instances, by several brothers; the psychological damage tended to be worse when the perpetrator was a father rather than any other male relative. Among the examples 14 STONE mentioned in my 2017a article, jealousy was a serious problem, since by its nature, father-daughter incest implies that the father has been unfaithful to the mother. The question arose in these women: Could a man, including a husband, ever be trusted? One woman, for example, had grown up in an impoverished family where the parents divorced, and she and her father had slept (and had sex) in his car. A quite beautiful woman, she later married a man who went from having a modest job as a plumber to becoming a highly successful contractor and multimillionaire. He proved, however, no more faithful to her than her father had been to her mother. They divorced. She then began an affair with a much more wholesome and loyal man—about whom she was nevertheless pathologically jealous. I worked with her in psychotherapy for two years, after which her jealous tendency appreciably lessened, and she was able to make a much more stable (and trusting) marriage. This was one of the very few cases I have ever worked with where a jealous person was eventually able to make a satisfactory marital relationship. She showed six of the nine BPD characteristics initially, but later would no longer meet BPD criteria. The interplay of adverse factors such as incest—and genetic factors aside from those that appear to heighten the risk for BPD—needs to be taken into account. But we know little about the favorable genetic factors that render certain persons relatively invulnerable to early traumata such as incest. Some favorable genetic factors apparently allowed the jealous woman just mentioned to rise above prolonged father-daughter incest, marital infidelity, and jealousy to eventually form a stable marriage. In contrast, several of the young women in the PI500 series committed suicide in their 20s and 30s. One had grown up as one of eight children in an extremely wealthy family. Her narcissistic father had committed incest with her and two of her sisters, one of whom had already committed suicide by the time our “P-I” patient was admitted to our service. She had run away from home, been hospitalized at our unit, eloped after a few months, and briefly became one of Andy Warhol’s actresses. She made a serious suicide attempt from which she was rescued, met a man she later married, but soon after—feeling despondent about not being able to function well as a wife given her chaotic past—committed suicide. In contrast, another young woman who had been involved in a father-daughter incest situation had run away from home in her late teens, become a fashion model, and then the mistress of a wealthy older man. She later married briefly and had a child whom, after divorce, she raised herself. When I saw her in psychotherapy she was in her mid-20s. She showed five of the BPD criteria and was markedly histrionic and “flighty”—in the sense that she often skipped sessions, going away with her sister and using CLINCIAL TREATMENT GUIDES FOR BPD 15 marijuana and cocaine. She is currently in her mid-50s and is leading a more tranquil life, living with former high-school friends. Her life has had some of the characteristics of Marie DuPlessis, the beautiful young woman from Normandy, who became first the mistress of the novelist Alexander Dumas, then briefly of Liszt, and finally the wife of a French count—and the inspiration of Verdi’s La Traviata—before dying of tuberculosis at 23 (Weis, 2015). Although sibling incest is more common than transgenerational incest, there were no known cases among the patients in the PI-500. Brother-sister incest is much more common than sister-sister. The latter is often characterized by mutuality and the absence of force, and for these reasons, apparently less pathogenic (let alone conducing to the development of BPD) (Russell, 1986, pp. 49-50). The one instance of brother-sister incest in my practice occurred 50 years ago and involved siblings who had been consistently neglected by their parents. In their teens, they began sleeping together and having sex, each serving as a kind of surrogate parent as well as close companion for the other. My patient (the sister) later married and was doing well when I contacted her after many years in a follow-up effort. But in another case, where I served as a consultant, a woman had, in effect, been gang-raped by her four brothers. When she married and later had a daughter and son of her own, she became convinced, to the point of delusion, that her husband would commit incest with their daughter. She divorced. The two teenage children preferred to remain with their (non-abusive) father and were both doing well when I followed up on their situation years later. Clearly, the hostility and violence of her brothers were the pathogenic elements in her personality aberration. One needn’t have invoked a genetic abnormality. From an etiological standpoint, genetic predisposition to bipolar disorder and the post-natal factor of incest are sometimes commingled as fostering BPD. A former borderline patient of mine, for example, had been sexually molested by both parents; her father had been hospitalized earlier for manic-depression (bipolar I disorder). Her chief BPD characteristic, besides suicidal gestures and threats, was her inordinate anger. In her case, the father was the more loving parent, while the mother was consistently hostile. Though both parents had obviously taken advantage of her, it was the mother’s dislike and hostility that seemed the primary cause of my patient’s anger and contempt. She never spoke ill of her father even though he had also misused her egregiously via the incest. The genetic “loading” was great since two paternal uncles had also been diagnosed as bipolar. When transgenerational incest (especially by a father) is accompanied by sadism, this seems sufficient in and of itself to bring about BPD 16 STONE in the victim as she (or rarely he) enters adolescence. I had occasion, when making diagnostic evaluations at a drug-abuse clinic, to interview a woman in her 30s with BPD and multiple drug abuse (alcohol, marijuana, and cocaine). Her history of incest was the most sordid I had encountered before or since. When she was seven, her father would immobilize her with handcuffs and then proceed to rape her as well as beat her with a stick. Her wounds came to the attention of the school authorities, and the father was arrested. Instead of receiving the life sentence he deserved, his mother bailed him out of jail where he had been held for several weeks. By the time I saw my patient years later, her life consisted of a series of brief and stormy relationships with men, drug abuse, suicide gestures, and all-too-understandable anger and misanthropy. There was no indication that there had been bipolar relatives in her background—not even her father, who was a sadistic psychopath, but not a manic-depressive. INADEQUATE MOTHERING Thus far we have focused on the presence of hostile or hurtful parenting, especially in the form of sexual molestation, as a forerunner of BPD psychopathology. There are other BPD patients for whom inadequate mothering appears to have played a prominent, at times even decisive role in the development of their personality disorder. The poor mothering might come in the form of neglect, active cruelty or hostility, or some combination. One borderline patient I worked with 20 years ago was the survivor of a car-crash in which both her Korean parents were killed. At age four, she was then raised by an uncle and aunt. The aunt would feed her own children, but would starve her niece or else do cruel things to her, like shove chopsticks into the back of her throat. The aunt let her own children use the bathroom, but made her niece go outdoors and leave her waste in the yard. Her uncle and male cousin then committed incest with her when she got a little older. Finally, when in her mid-teens, she came to the United States to live with families that take in students. Though she was an A-student at a prestigious university, she struggled with agoraphobia, bouts of self-cutting, and suicide gestures that at one point necessitated hospitalization. She was quite an appealing young woman, but her fear of abandonment and clinginess proved burdensome to her boyfriends, who eventually left her. I treated several women with BPD who had grown up in prominent families of great wealth, where the fathers were indifferent to their children while the mothers were basically decent and caring women whose CLINCIAL TREATMENT GUIDES FOR BPD 17 husbands commandeered their time to such an extent that they had very little time for their children. These patients, in effect, had a loving mother who just wasn’t there. These patients found being alone intolerable and tended to develop eating disorders (anorexia or bulimarexia). Several of these effectively “motherless” young women had sexual relationships with other female students at college, so that the (now sexualized) closeness served to compensate to a degree for what had been missing in their original mother-daughter relationship. I have treated several patients with BPD whose mothers were scarcely available—whose longing for closeness with a mother expressed itself in their dreams as having sex with another woman. As one enters puberty, the emerging sexuality often adds an element of sexual coloration to an underlying wish for closeness. These women were frightened that they were becoming lesbians and the exploration of this material was so fraught that further psychoanalytic work on this issue proved too uncomfortable. The “cure” was instead to find the right man, marry, and envelop themselves in the blanket of conventional and, for them, reassuring, heterosexuality. These patients did succeed in finding suitable mates—allowing their mother-longing and homosexual fears to be given a decent “closed casket” burial. Some of the patients had mothers who were openly hostile toward them. One such mother, who was divorced from the father when their daughter was four, forbade the girl any contact, even by phone, with the father. I treated this patient when she was hospitalized for a suicide attempt just after starting college. For a time, she was sexually promiscuous, but hostile to the men she would consort with; she was intensely lonely, felt alienated, and was consumed with envy for people who had ordinary lives. She did not become reunited with her father until her late 30s, and she then married an older man with whom she was finally able to carve out a pleasant and productive life (Stone, 1990). As with many women with BPD, she chose not to have children, perhaps sensing inchoately that, lacking the usual template for mothering that girls absorb from having a good mother, becoming a mother herself would not be a comfortable or rewarding task. DISCUSSION Regarding a possible hereditary factor predisposing to BPD, the very term borderline was used in the early 20th century to designate a condition that in milder form resembled—that is, was “borderline” to—one of the two major psychoses, whether schizophrenia or manic-depression (now bipolar disorder). As mentioned above, there was a tighter 18 STONE connection, both conceptually and epidemiologically, between schizotypal personality and (full-blown) schizophrenia. The connection between BPD and bipolar disorder seemed weaker. In an earlier article, for example, McGlashan (1983) noted that the evidence then available suggested schizotypal personality as a variant of schizophrenia, whereas any connection between BPD and primary affective disorder (viz. bipolar disorder) was suggested but not conclusive. Twin studies by Torgersen in Norway (1984) found that genetic factors appeared to influence the development of schizotypal personality, but not borderline personality. A decade later, he was even more skeptical about genetic transmission in BPD (Torgersen, 1994). Contemporary thought, as outlined by Kavoussi and Siever (1992), acknowledges that there is, nevertheless, a measure of overlap between the two personality types, but this is more likely a manifestation of dimensional psychology—as emphasized in Plomin’s work (2018). Much of the confusion concerning the legitimacy of genetic factors in BPD stems, however, from a failure to appreciate that the characteristics of schizotypal personality emphasize cognitive peculiarities (eccentric speech, ideas of reference, etc.), which are hardly likely to arise in relation to incest, bad parenting, maternal neglect, or the other disadvantages that show up repeatedly in the histories of BPD patients. So schizotypal characteristics emerge as formes frustes (a crude or unfinished form) of the major psychosis; namely, the predominantly cognitive psychosis of schizophrenia. But the emotional dysregulation that is the sum and substance of BPD can indeed arise out of either hereditary predisposition to a mood-oriented psychosis (manic-depression/bipolar disorder) or the disruptive or violent or neglectful parental rearing that, as noted earlier, is present in the great bulk of BPD patients. The exceptions are those few borderline patients who—as in some of the clinical vignettes above—had warm and loving parents, and who were not abused, molested, neglected, or even affected by the death of a parent in their formative years. In these admittedly uncommon borderline patients, there is nothing left to account for their psychopathology except genetic influences. So from this perspective, BPD may be best understood as a mixed condition etiologically: a disorder of emotional regulation that may arise primarily from (a) disadvantageous early environment, (b) genetic loading for bipolar disorder, or (c) a mixture of the two. It should be recalled that a certain proportion of persons diagnosed in adolescence or their early 20s with BPD go on to show clear-cut signs of bipolar disorder as they enter adult life. Among the latter, there is a tendency to remain symptomatic and burdened as they grow older, in contrast to the larger group of primarily environmentally disadvantaged BPD patients, many of whom, especially with good treatment, become healthier as they get past 30— CLINCIAL TREATMENT GUIDES FOR BPD 19 and live essentially well, achieving remission and even recovery (Stone, 1990; Zanarini et al., 2012). As for the impact of incest and other forms of abusive or otherwise disadvantageous parenting (such as neglect or punitiveness), there is a variety of pathological consequences. Becoming borderline is one of them—one manifestation of which is a heightened “free-floating anxiety” (Dulz & Schreyer, 1997). Incest may also lead to the development of insecure attachment, as well as to the characteristics of post-traumatic stress disorder (PTSD)—with its startle responses, nightmares, intrusive recollections of original traumatic events, and so forth (Alexander et al., 1998). In another study, the timing at which incest experiences occurred played a role in the later severity of symptomatology. McLean and Gallop (2003), for example, found that the development of BPD and complex PTSD was more common in women who had experienced early-onset versus late-onset (viz. post-pubertal) paternal incest. Erdinç and colleagues (2004) point to the multiple effects associated with incest: besides BPD and PTSD, one also encounters dissociative amnesia—the latter characterized by an obliteration from memory of the traumatic sexual experiences (until eventually restored through psychotherapy). Another unfortunate consequence of the incest experience, observed in a number of gynecologic patients, was chronic pelvic pain, in addition to BPD. Early family dysfunction, including incest, was noted in a significant proportion of these women (Gross, Doerr, Caldirola, Guzinski, & Ripley, 1980/1981). One of the defining attributes of BPD is “inappropriate, intense anger or difficulty controlling anger” (American Psychiatric Association, 2013). Kernberg (1994) has examined the issue from the perspective of the relationship between inborn (i.e., genetic) predisposition to aggressive behavior versus the (post-natal) effects of severe trauma and psychosocial pathology stemming from adverse early experiences. From a therapeutic standpoint, he drew attention to management of intense hatred, linked to aggression, in the transference, when a psychoanalytically oriented form of therapy is the primary treatment modality. It is clear from both the clinical vignettes and the references on incest cited here that inordinate anger may arise from both pre- and postnatal influences. Many persons born with a genetic predisposition to bipolar disorder may show the predominantly manic symptomatology, a common manifestation of which, along with manic grandiosity, is the temperamental factor of (extreme) irritability. The latter may surface as a personality marked by a heightened predisposition to anger. And as we have noted, a good number of patients with BPD have developed as borderline via this form of inheritance, even if raised in a non-abusive (and incest-free) environment. But as also noted, many patients with 20 STONE BPD, even with no known risk for bipolar disorder, come by their inordinate anger in reaction to incest or to other adverse factors, such as parental brutality or devastating criticism and humiliation. We have also drawn attention to the many combined cases of BPD, where the patient has been burdened by both genetic and environmental disadvantages. Though most of the related literature stems from studies in the United States and Europe, a similar situation is described in an article from the Indian subcontinent (Menon, Chaudhari, Saldanha, Devabhaktuni, & Bhattacharya, 2016). In their study of 36 BPD patients, almost half (16 or 44%) reported a history of childhood sexual abuse, usually occurring between the ages of seven and twelve. The abnormalities ascribed to the abuse were chiefly identity disturbance, recurrent suicidal or selfharm behaviors, and paranoid/dissociative symptoms. It is worth recalling that the intense jealousy noted in certain sexually abused BPD patients, especially incest victims, is itself a paranoid reaction in which all subsequent sexual partners are suspect—of infidelity. In the typical case of father-daughter incest, the daughter comes to realize that her father was obviously unfaithful to her mother—so, in effect, how can any man be trusted? Though incest in BPD patients has gotten considerable attention, others have drawn attention to the high frequency of adverse parental factors. Judith Herman and colleagues (1989) mentioned, for example, how in their studies four out of five (81%) patients with BPD had suffered some form of abuse, including physical abuse (71%), sexual abuse (68%), and witnessing serious domestic violence (62%). One colleague in the Herman, Perry, and van der Kolk article explains further that prolonged and severe trauma early in life often leads to the emotional dysregulation that is a key feature of BPD—predisposing to self-soothing behaviors: clinginess and overdependency in relationships, eating disorders, substance abuse, or the paradoxical self-mutilation—paradoxical because self-cutting, for example, would be painful for an ordinary person, but is acceptable to some borderline patients, since the controlled and bearable physical pain becomes an antidote to the unbearable and global psychological pain (van der Kolk, Hostetler, Herron, & Fisler, 1994). Some consider traumatic childhood to be the main etiological factor in the development of BPD (Kuritárné, 2005), although I believe this impression is to an extent sample-dependent. Cultural and socioeconomic factors enter into the equation, since (as shown by Russell, 1986) incest and family brutality are more common in certain cultural backgrounds and socioeconomic conditions and less so in others, such that the balance between genetic and environmental factors is not the same in all samples of BPD patients. More detailed impressions and connections arose out of the large-scale study of 290 BPD CLINCIAL TREATMENT GUIDES FOR BPD 21 patients by Zanarini and her colleagues (2002). Sexual abuse, for example, tended to occur both in childhood and adolescence on a weekly basis, usually for a year or more. Sexual penetration and/or use of force were widespread, occurring in over half the cases. Severity of the abuse was noted to correlate with symptom severity in all the major aspects of borderline psychopathology; namely, affect, cognition, impulsivity, and disturbed interpersonal relationships. Others have been at pains to remind us that several personality disorders besides BPD are also often set in motion by sexual and physical abuse, especially paranoid and antisocial disorders. The marked jealousy in certain women who had been incest victims is itself a variety of paranoid disorder. Sexual, physical, and emotional abuse was common in the backgrounds of paranoid patients of whatever sort (Bierer et al., 2003). Indeed, cases of pure BPD—with no accompanying personality disorders—are all but unknown. Almost invariably, BPD will be accompanied by one or more comorbid personality disorders, especially among the so-called dramatic cluster in DSM: histrionic, narcissistic, and antisocial. But other disorders are also common: paranoid and dependent (Oldham, Skodol, Hyler, Rosnick, & Davies, 1992). In this regard, the only patient I treated in the past 50 years who was the victim of father-son incest (he had been anally raped repeatedly during his adolescence) met criteria for BPD (he showed five items: identity disturbance, suicidal behaviors, affective instability, inappropriate anger, and stress-related paranoid ideation), but also, and more prominently, for paranoid personality disorder. Adding to his distrust and paranoid development was his older brother who, out of wanton cruelty, used to push his hands onto a hot radiator. Though he was a linguistics scholar, his self-regard was severely impaired, and he felt that I looked down on him as though I would “rather treat a Rockefeller for nothing” than treat him for a modest fee. In the beginning, he made violent threats toward me, but softened when he realized that we had some things in common; we both spoke German and Japanese and were both aficionados of opera. But he never overcame his distrust of his co-workers and often felt the police were checking up on him. My work with him was primarily supportive, in hopes of enhancing his self-esteem. On one occasion when he was about to throw away his opera ticket because he didn’t deserve it, I wrote on a prescription pad: “Go to the damn opera!” And he did. This was in line with the recommendations of Gunderson and Chu (1993) who advised, when dealing with borderline patients who had been traumatized via early child abuse, that clinicians endeavor to facilitate a stronger therapeutic alliance through acknowledgement of the patient’s victimization: this, by enhancing the patient’s often enfeebled sense of self-worth. The authors also under- 22 STONE lined the value of reframing the patient’s experience in the here and now as a consequence of the childhood trauma. In the case of my sexually and physically brutalized patient, my task was to help him understand—through sympathy and decency, more than through correct interpretations—that the human race was not as universally malign as his past had taught him to expect. In line with the growing emphasis on early childhood trauma as the primary factor setting in motion the development of BPD, Saunders and Arnold, writing in the same year as the Gunderson and Chu article (1993), criticized the inconsistent findings of the earlier etiological speculations that emphasized separation-individuation issues, empathic failures in early childhood, early losses and separations, and so forth. Instead they remarked how a half to three-quarters of BPD patients had childhood abuse and trauma in their histories—which Saunders and Arnold saw as of greater etiological importance. These impressions are more in harmony with my own views, where many of the personality traits seen again and again in BPD patients can be ascribed in fair measure to incest victimization— particularly, mistrustfulness, jealousy, seductiveness, hostility, impulsivity, defiance, and emotional volatility (Stone, 1989). The critique of Saunders and Arnold (1993) notwithstanding, we should not overlook the impact in certain borderline patients of problems relating to adverse mother-child, rather than father-child, interactions. In a study from Heidelberg and Palermo of 44 adolescent female hospitalized borderline patients and 47 controls, the three main independent predictors of the BPD–related psychopathology were (in that order) sexual abuse, generally dysfunctional family, and low maternal care (Infurna et al., 2016). Under the heading of “low maternal care,” there were several varieties. Some mothers, for example, offered what was called “affectionless control”—characterized by low care and high overprotection. This was often associated with subsequent depressive syndromes. Some mothers, in contrast, showed “neglectful parenting,” where there was low care and little protection. The authors speculated that inadequate mothering might magnify the ill effects of other forms of parental maltreatment (including sexual or physical abuse). In my own studies, 28% of the female BPD patients had had to deal with maternal inadequacies. In the largest group (12 patients), the problem was chiefly maternal hostility. Three of the patients had also been incest victims. There had been one suicide. The hostility often took the form of withering criticism and contempt; one of the mothers had also been physically abusive. Six of the mothers had been neglectful; sometimes this took the form of grossly preferring the patient’s brother. Three of the mothers had been warm and consistently caring—but had been rendered largely unavailable emotionally because their husbands CLINCIAL TREATMENT GUIDES FOR BPD 23 resented their attention to the children and commandeered their wives’ attention all to themselves. The fathers insisted on long vacations without the children, and interfered in other ways with any efforts on their wives’ part to spend more time with the children. All but one of the patients suffered from depression; half of the 12 with hostile mothers eventually showed signs of bipolar disorder, including the one woman who committed suicide. In this entire group, inadequate or disturbed mother-daughter relationships together constituted an important factor predisposing to BPD, and occurred as often as the more dramatic (and probably still more pathogenic) incest factor. But half of the entire patient group was bipolar, meaning that there was a confluence of genetic and environmental factors in them that underlay their borderline disorder. The proportion of these factors will presumably vary from one sample of BPD patients to another, but it is highly unlikely that in any large sample the patients would all be of the genetic type or else exclusively all of the adverse parenting type. In general, the importance of paying attention to both genetic and environmental factors when evaluating a new patient who appears to meet criteria for BPD is precisely because BPD is a syndrome—in effect, a mixture of symptoms (such as anxiety, mood disturbances, etc.) and personality traits (inordinate anger, paranoid tendencies, impulsivity), rather than a personality disorder in the strict sense of the term, composed merely of actual traits (as is the case, for example, with dependent and schizoid disorders). Each patient with BPD needs to be seen as situated along a spectrum—with the primarily genetic-engendered at one end and the primarily environment-based at the other, and with all the other combinations in between. This places an emphasis on taking a detailed family history (including grandparents, aunts, uncles, and cousins, etc.) to ascertain whether there are relatives with mood disorders or psychotic conditions. With female patients, inquiry about alterations in mood and irritability around the time of the menses is also important—since such disturbances, especially if severe, may point to possible bipolar vulnerability. If the latter is present, the medication regime may well require the addition of a mood stabilizer, such as lithium or lamotrigine, since psychotherapy of any sort would not suffice (as was the case with the suicidal young woman mentioned above who required lithium and clozapine to restore emotional equilibrium). Another important consideration at the outset of treatment with borderline patients is the assessment of their cognitive style. Those with a good reflective capacity and of an introspective turn of mind are apt to work well with a psychoanalytically based approach (expressive psychotherapy, transference-focused psychotherapy, or other similar method). In patients where those capacities are not very prominent, 24 STONE a cognitive-behavioral approach (dialectic behavioral therapy, schema therapy, etc.) may prove more effective (Stone, 2017b). Treatment with borderline patients is generally a lengthy process. As such, what may have been a suitable treatment approach at the outset may be less suitable at a later stage, when a shift to a different modality may prove more effective. As emphasized by Judd and McGlashan (2003) and Livesley (2008, 2012), flexibility in treatment methods will be a key element in the therapist’s overall approach. REFERENCES Alexander, P. C., Anderson, C. L., Brand, B., Schaeffer, C. M., Grelling, B. Z., & Kretz, L. (1998). Adult attachment and long-term effects in survivors of incest. Child Abuse & Neglect, 1, 45-61. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Association. Bateman, A., & Fonagy, P. (2004). Psychotherapy for borderline personality disorder: Mentalization-based treatment. Oxford, UK: Oxford University Press. Bierer, L. M., Yehuda, R., Schmeidler, J., Mitripoulou, V., New, A. S., Silverman, J. M., & Siever, L. J. (2003). Abuse and neglect in childhood: Relationship to personality disorder diagnosis. CNS Spectrum, 10, 737-754. Costa, P. T. Jr., & Widiger, T. A. (Eds.). (2002). The five-factor model of personality. Washington, DC: American Psychological Association. Dulz, B., & Schreyer, D. (1997). The problems in dealing with the incest experiences of borderline patients. Psychiatrische Praxis, 24, 265-269. Erdinç, I. B., Sengὕl, C. B., Dilbaz, N., & Bozkurt, S. (2004). A case of incest with dissociative amnesia and post-traumatic stress disorder. Turk Psikiyatri Dergisi, 15, 161-165. Gross, R. J., Doerr, H., Caldirola, D., Guzinski, G. M., & Ripley, H. S. (1980/1981). Borderline syndrome and incest in chronic pelvic pain patients. International Journal of Psychiatry in Medicine, 10, 79-96. Gunderson, J. G. (2001). Borderline personality disorder: A clinical guide. Washington, DC: American Psychiatric Press. Gunderson, J. G., & Chu, J. A. (1993). Treatment implications of past trauma in borderline personality disorder. Harvard Review of Psychiatry, 1, 75-81. Herman, J., Perry, J. C., & van der Kolk, B. A. (1989). Childhood trauma in borderline personality disorder. American Journal of Psychiatry, 146, 490-495. Infurna, M. R., Brunner, R., Holz, B., Parzer, P., Giannone, F., Reichl, C., … Kaess, M. (2016). The specific role of childhood abuse, parental bonding, and family functioning in female adolescents with borderline personality disorder. Journal of Personality Disorders, 30, 177-192. Judd, P. H., & McGlashan, T. H. (2003). A developmental model of borderline personality disorder: Understanding variations in course and outcome. Washington, DC: American Psychiatric Press. Kavoussi, R. J., & Siever, L. J. (1992). Overlap between borderline and schizotypal disorders. Comprehensive Psychiatry, 33, 7-12. CLINCIAL TREATMENT GUIDES FOR BPD 25 Kernberg, O. F. (1994). Aggression, trauma, and hatred in the treatment of borderline patients. Psychiatric Clinics of North America, 17, 701-714. Kernberg, O. F., Selzer, M., & Koenigsberg, H. (1989). Psychodynamic psychotherapy of borderline patients. New York: Basic Books. Kernberg, O. F., Yeomans, F. E., Clarkin, J. F., & Levy, K. N. (2008). Transferencefocused psychotherapy: Overview and update. International Journal of Psychoanalysis, 89, 601- 620. Kuritárné, I. S. (2005). Childhood trauma in the etiology of borderline personality disorder. Psychiatria Hungarica, 20, 256-270. LeGrand du Saulle, H. (1883). Les hystériques: État physique et l’etat physique mental. Paris: Baillière. Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford. Livesley, W. J. (2008). Integrated therapy for complex cases of personality disorder. Journal of Clinical Psychology, 64, 207-221. Livesley, W. J. (2012). Moving beyond specialized therapies for borderline personality disorder: The importance of integrated domain-focused treatment. Psychodynamic Psychiatry, 40, 47-74. McGlashan, T. H. (1983). The borderline syndrome. II. Is it a variant of schizophrenia or affective disorder? Archives of General Psychiatry, 40, 1319-1323. McLean, L. M., & Gallop, R. (2003). Implications of childhood sexual abuse for adult borderline personality disorder and complex post-traumatic stress disorder. American Journal of Psychiatry, 160, 369-371. Menon, P., Chaudhari, B., Saldanha, D., Devabhaktuni, S., & Bhattacharya, L. (2016). Childhood sexual abuse in adult patients with borderline personality disorder. Industrial Psychiatry Journal, 25, 101-106. https://www.ncbi.nlm.nih.gov/ pubmed/28163415 Oldham, J. M., Skodol, A. E., Hyler, S. E., Rosnick, L., & Davies, M. (1992). Diagnosis of DSM-III-R personality disorder by two structured interviews: Patterns of comorbidity. American Journal of Psychiatry, 149, 213-220. Plomin, R. (2018, November 17). Our fortunetelling genes. Wall Street Journal Review, pp. 1-2. Russell, D. E. H. (1986). The secret trauma: Incest in the lives of girls and women. New York: Basic Books. Saunders, E. A., & Arnold, F. (1993). A critique of conceptual and treatment approaches to borderline psychopathology in light of findings about childhood abuse. Psychiatry, 56, 188-203. Schirmer, A. (2013). Sex differences in emotion. In J. Armony & P. Vuilleumier (Eds.), The Cambridge handbook of human affective neuroscience (pp. 591-610). New York: Cambridge University Press. Stone, M. H. (1989). Individual psychotherapy with victims of incest. Psychiatric Clinics of North America, 12, 237-255. Stone, M. H. (1990). The fate of borderline patients. New York: Guilford. Stone, M. H. (1993). Abnormalities of personality. New York: Norton. Stone, M. H. (2013). A new look at borderline personality disorder and related disorders: Hyper-reactivity in the limbic system and lower centers. Psychodynamic Psychiatry, 41, 437-466. Stone, M. H. (2017a). Borderline patients 25 to 50 years later. Psychodynamic Psychiatry, 45, 259-296. 26 STONE Stone, M. H. (2017b). Borderline personality disorder: Treatment from the contextual perspective. Psychodynamic Psychiatry, 45, 1021. Torgersen, S. (1984). Genetic and nosologic aspects of schizotypal and borderline personality disorders. A twin study. Archives of General Psychiatry, 41, 546-554. Torgersen, S. (1994). Genetics in borderline conditions. Acta Psychiatrica Scandinavica, 379(Suppl.), 19-25. Trull, T. J., & McCrae, R. C. (2002). A five-factor perspective on personality disorder research. In P. T. Costa & T. A. Widiger (Eds.), The five-factor model of personality (pp. 45-57). Washington, DC: American Psychological Association. Van der Kolk, B. A., Hostetler, A., Herron, N., & Fisler, R. E. (1994). Trauma and the development of borderline personality disorder. Psychiatric Clinics of North America, 17, 715-730. Weis, R. (2015). The real Traviata. New York: Oxford University Press. Young, J. E., Klosko, J. S., & Weishaar, M. E. (2003). Schema therapy: A practitioner’s guide. New York: Guilford. Zanarini, M. C., Frankenburg, F. R., Reich, D. B., & Fitzmaurice, G. (2012). Attainment and stability of sustained symptomatic remission and recovery among patients with borderline personality disorder and Axis II comparison subjects: A 16-year prospective follow-up study. American Journal of Psychiatry, 169, 476-483. Zanarini, M. C., Yong, L., Frankenburg, F. R., Hennen, J., Reich, D. B., Marino, M. F., & Vujanovic, A. A. (2002). Severity of reported childhood sexual abuse and its relationship to severity of borderline psychopathology and psychosocial impairment among borderline patients. Journal of Nervous and Mental Disease, 190, 381-387. 225 Central Park West, Suite 114 New York, NY 10024 Michaelhstonemd@gmail.com