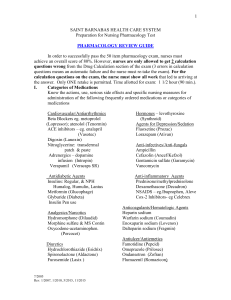
1 SAINT BARNABAS HEALTH CARE SYSTEM Preparation for Nursing Pharmacology Test PHARMACOLOGY REVIEW GUIDE In order to successfully pass the 50 item pharmacology exam, nurses must achieve an overall score of 80%. However, nurses are only allowed to get 2 calculation questions wrong from the Drug Calculation section of the exam (3 errors in calculation questions means an automatic failure and the nurse must re-take the exam). For the calculation questions on the exam, the nurse must show all work that led to arriving at the answer. Only ONE retake is permitted. Time allotted for exam: 1 1/2 hour (90 min.). I. Categories of Medications Know the actions, use, serious side effects and specific nursing measures for administration of the following frequently ordered medications or categories of medications Cardiovascular/Antiarrhythmics Beta Blockers eg. metoprolol (Lopressor); atenolol (Tenormin) ACE inhibitors – eg. enalapril (Vasotec) Digoxin (Lanoxin) Nitroglycerine: transdermal patch & paste Adrenergics – dopamine infusion (Intropin) Verapamil (Veracaps SR) Hormones – levothyroxine (Synthroid) Agents for Depression/Sedation Fluoxetine (Prozac) Lorazepam (Ativan) Antidiabetic Agents Insulins: Regular, & NPH Humalog, Humulin, Lantus Metformin (Glucophage) Glyburide (Diabeta) Insulin Pen use Anti-inflammatory Agents Prednisone/methylprednisolone Dexamethasone (Decadron) NSAIDS – eg.Ibuprophen, Aleve Cox-2 Inhibitors- eg Celebrex Analgesics/Narcotics Hydromorphone (Dilaudid) Morphine sulfate & MS Contin Oxycodone-acetaminophen. (Percocet) Diuretics Hydrochlorothiazide (Esidrix) Spironolactone (Aldactone) Furosemide (Lasix ) 7/2005 Rev. 1/2007, 1/2010, 5/2015, 11/2015 Anti-infectives/Anti-fungals Ampicillin Cefazolin (Ancef/Kefzol) Gentamicin sulfate (Garamycin) Vancomycin Anticoagulants/Hematologic Agents Heparin sodium Warfarin sodium (Coumadin) Enoxaparin sodium (Lovenox) Dalteparin sodium (Fragmin) Antiulcer/Antiemetics Famotidine (Pepcid) Omeprazole (Prilosec) Ondansetron (Zofran) Flumazenil (Romazicon) 2 Antiseizure Phenytoin sodium (Dilantin) High Alert Medications: Identified by TJC (The Joint Commission) -concentrated KCL, concentrated NaCl,, insulin, heparin Antidotes Protamine Sulfate Naloxone HCl (Narcan) Vitamin K (Aquamephyton) II. III. Herbal Interactions: anticoagulants and ginko biloba Important to Know: 1. Medication administration based on RN standards of practice. 2. How to administer intramuscular injections – variations by weight, size, age. 3. Nursing responsibilities for first-dose of any medication. 4. Nursing documentation for PRN medications. 5. How to draw up and administer insulin subcutaneously and how to use an insulin pen. 6. Heparin/Lovenox/Fragmin injection techniques and sites 7. Specific lab values to be monitored for patients on Lovenox/Fragmin, Heparin, Coumadin, Vancomycin 8. How to apply topical/ transdermal medication/patches 9. IV push medications 10. How to administer eye and ear drops – adults and pediatric 11. How to administer sustained release (SR, LX, LA etc.) tablets/capsules 12. Distinguish S/S of hypoglycemia & the interventions for treating it. 13. Measures for effective pain management – dosing schedule, documentation, use of appropriate pain scale eg. FLACC, BPS, CPOT, Wong-Baker, Numeric. 14. Safety measures for administration of TPN (total parenteral nutrition) 15. How to administer meds via NG tube 16. IV administration of diluted KCl only via central line or large vein 17. Monitoring for IV infiltration of vesicants (e.g. Dopamine) 18. Heparin Infusion weight-based dosages Conversions 1 kg = 1000 gm 1 gm = 1000 mg 1 mg = 1000 mcg 7/2005 Rev. 1/2007, 1/2010, 5/2015, 11/2015 1 liter = 1000 ml 1 kg = 2.2 lbs 1 tsp = 5 ml 1 oz = 30 ml 1 tbsp = 3 tsp 1 inch = 2.54 cm 3 IV. Policies - The following SBHCS policies apply to the administration of medication and must be followed at all times. TOPIC GOLDEN RULES ADDITIONAL INFORMATION PAIN Patients must receive adequate If the medications ordered are not pain control. controlling the patient’s pain, a new order should be obtained from the physician. Don’t let the patient suffer. Pain assessment, interventions, and outcomes must be documented completely Documentation includes: pain assessment, treatment, comfort level achieved (the pain goal for that patient), interventions when treatment is inadequate, and new outcomes from those interventions DOUBLE IDENTIFICATION To identify each patient receiving medication, the nurse must use 2 forms of identification. TELEPHONE ORDERS All telephone orders must be completely read back and verified to the physician as soon as they are recorded on the medical record and BEFORE they are executed. Forms of identification include the patient’s ID BAND (a must!); asking the patient his name, the MR number, date of birth, phone number, photo license, etc. The order read back and verification includes the patient’s name, date and time of the order, the name of the med, the dose, the route, the frequency of administration, any parameters or criteria for administration. VERBAL ORDERS Verbal orders can only be accepted in an emergency situation. An emergency situation is one in which the health of the patient would be compromised if there were a delay in administering the medication. For accuracy, all verbal orders must be read back and verified to the Physician completely as soon as they are written in the medical record. The order read-back and verification includes the patient’s name, date and time of the order, the name of the med, the dose, the route, the frequency of administration, any parameters or criteria for administration. a. Use a leading zero in front of the decimal dose of a medication. Correct: 0.35 mg Incorrect .35 mg ANNOTATION Correct & complete written FOR orders are required for each WRITTEN medication to be administered. ORDERS If any part of an order is missing, unclear, illegible, 7/2005 Rev. 1/2007, 1/2010, 5/2015, 11/2015 b. Do Not use a ‘trailing zero’ after a whole number dose of a medication 4 MISSED MEDICATION DOSES DANGEROUS ABBREVIATIONS includes unacceptable abbreviations, or does not conform to the patient’s condition, the nurse must contact the physician to correct the problem or clarify the order before administering the medication. Whenever a medication dose has been missed, the nurse should contact the physician to clarify what is best for the patient. Correct: 4mg Incorrect: 4.0 mg Certain previously-acceptable abbreviations CAN NO LONGER BE USED in the medical record. WRONG RIGHT U IU Units International Units ug Micrograms, mcg QD/OD Daily QOD Every other day The TJC and hospital policy now prohibits their use. c. Never use a range of doses or times. Correct: Percocet 1 tab. po q4h Incorrect: Percocet 1-2 tabs q 3-4 hours. When a medication dose is missed eg. the patient is off the unit, the nurse should not assume that the patient can wait until the next dose is due. The decision about the missed dose belongs to the physician. If these abbreviations appear in sc or sq a medication order, the order must be clarified with the QID physician and rewritten correctly. MS/MSO4 MgSO4 Subcutaneously Four times a day Morphine sulfate (morphine) Magnesium sulfate OS/OD/OU Left/right/both eyes AS/AD/AU Left/right/both ears V. Some Helpful Hints: Exam candidates may bring one nursing drug reference book and a calculator (extra batteries recommended) to use during the exam. Example: Mosby’s Nursing Drug Reference by Linda Skidmore-Roth; Cost: approx. $38.00. No cell phones may be brought into the exam area or used during the test. VI. Sample Conversions and Calculations: The problems below represent the types of calculations that will be presented on the nursing pharmacology exam. The answers are found at the end of this review guide. 7/2005 Rev. 1/2007, 1/2010, 5/2015, 11/2015 5 Conversions: a. b. c. d. e. 2 tsp = _____ mL 450 mcg = _____ mg .048 gm = _____ mg 475 mg = _____ gm 3 tablespoons = _____ mL f. g. h. i. j. 2 oz = _____ mL 150 lbs = _____ kg 65 kg = _____ lbs 4.1 mg = _____ mcg 2.5 inches = _____ cm Calculations: 1. A child is to receive amoxicillin 50 mg po. The medication in oral suspension is labeled 125 mg per 5 ml. How many mls should the child receive? 2. The liquid medication label reads 100 mg per 2 ml. The order is for the patient to receive 200 mg of the medication. How many mls will be administered? 3. The patient is to receive digoxin 0.25 mg IV. Digoxin is in prefilled syringes of 0.5 mg per 2 mls. How many mls will be administered by syringe? 4. The physician orders dynapen 125 mg po stat. The bottle is labeled 25 mg per ml. How many mls should be given? 5. Penicillin G sodium for injection contains 250,000 units per ml. How many units are there in 3.5 mls? 6. The doctor orders 1000 ml of D5W every 6 hours. How many mls per hour should the patient receive? 7. Calculate the drip rate for an IV of D5 ½ NS to run at 20 ml per hour using a microdrip set (60 gtts per ml). 8. The patient is to receive Keflex 1 gm P.O. On hand is Keflex 250 mg per tablet. How many tablets should be administered? 9. Garamycin comes in a concentration of 80 mg per 2ml. How many mls would be needed for a dose of 40 mg? 10. The physician orders 1 liter of NS every 8 hours. How many mls per hour should the patient receive? Using macrodrip tubing (15 gtts per ml) what is the flow rate in gtts per minute? 7/2005 Rev. 1/2007, 1/2010, 5/2015, 11/2015 6 11. The patient is to receive Ancef 1 gram every 6 hours in 100 ml of normal saline to run over 30 minutes. If microdrip tubing is used (60 gtts per ml), what is the rate of flow in drops per minute? If macrodrip tubing is used (15 gtts per ml), what is the rate of flow in drops per minute? 12. One unit of blood, (250 ml per unit) must be infused over 4 hours. It cannot remain hanging longer than 4 hours. How fast must you run the blood using blood tubing of 10 gtts per ml? 13. Your patient has a PICC (Peripherally Inserted Central Line) and needs to receive 1000ml over 12 hrs. The infusion pump should be set at what rate? (ml/hr) PHARMACOLOGY REVIEW GUIDE - ANSWER KEY Conversions: a. b. c. d. e. 10 ml 0.45 mg 48. mg 0.475 gm 45 ml f. g. h. i. j. 60 ml 68.18 kg 143 lbs 4100 mcg 6.35 cm Calculations: 1. 2. 3. 4. 5. 6. 2 ml 7. 4 ml 8. 1 ml 9. 5 ml 10. 875,000 units 11. 166.6 ml per hr (167 acceptable) 12. 13. 7/2005 Rev. 1/2007, 1/2010, 5/2015, 11/2015 20 gtts per min. 4 tablets 1 ml 125 ml/hour; 31 or 32 gtts per min. 199 gtts per min. (198 or 200 is acceptable) 50 gtts per min, macrodrip 10 gtts per min 83 ml/hr