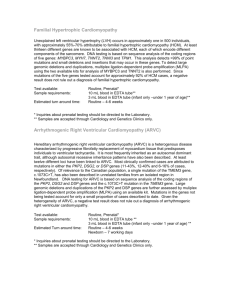
What am I? cardiomyopathy A subacute or chronic disorder of the heart muscle. Treatment is palliative not curative. The client will have many changes to lifestyle and lifespan. Physiology: Dilated cardiomyopathy: Fibrosis of the myocardium and endocardium, dilated chambers, mural wall thrombi prevalent. Non-obstructive cardiomyopathy: Hypertrophy of the walls, hypertrophied septum, small chamber size . Obstructive cardiomyopathy: Same as non obstructed except for obstruction in the left ventricular wall. Restrictive cardiomyopathy: Mimics pericarditis, fibrosed walls can expand or contract, emboli is common. Causes: ❖ ❖ ❖ ❖ ❖ ❖ Genetic conditions. Long-term high blood pressure. Heart tissue damage from a previous heart attack. Chronic rapid heart rate. Heart valve problems. Metabolic disorders, such as obesity, thyroid disease or diabetes. Dilated cardiomyopathy ❖ ❖ ❖ ❖ ❖ ❖ ❖ Cardiac glycoside Diuretic Angiotensin-converting enzyme inhibitor, such as Oxygen Antiarrhythmics Beta-adrenergic blockers, Aldosterone antagonist, Vasodilator Angiotensin II receptor blocker Inotropic agent Anticoagulant Interventions/Teaching: ❖ ❖ ❖ ❖ ❖ ❖ Low-sodium, low fat Fluid restriction Avoid alcohol Rest periods Moderate exercise to prevent deconditioning Cardiac rehabilitation ❖ CNS: Fatigue and weakness Heart: HF, dysrhythmias and heart block, systemic or pulmonary emboli, s3, s4 gallop, cardiomegaly Non obstructive cardiomyopathy RESP: Dyspnea Heart: Angina , mild cardiomegaly, s4 gallop, ventricular dysrhythmias, sudden death, HF Fatigue, syncope obstructive cardiomyopathy ❖ ❖ ❖ RESP: Dyspnea Heart: Angina , mild cardiomegaly, s4 gallop, ventricular dysrhythmias, sudden death, HF Fatigue, syncope, ❖ mitral regurgitation, A- FIB obstructive cardiomyopathy RESP: Dyspnea Heart: Mild cardiomegaly, s4 / s3 gallop, Fatigue, heart block, emboli ❖ ❖ ❖ ❖ Treatments ❖ Medications: ❖ ❖ ❖ Labs & Diagnostics Assessment: ❖ ❖ ❖ Dilated cardiomyopathy: Symptomatic treatment of ❖ HF, vasodilators, heart transplant , control ❖ dysrhythmias. Nonobstructed cardiomyopathy: Symptomatic treatment, beta blockers, cardioversion, ❖ ventricular myotomy, valve replacement, digoxin, nitrates, vasodilators. obstructive cardiomyopathy: Symptomatic treatment, beta ❖ blockers, cardioversion, ventricular myotomy, valve replacement, digoxin, nitrates, vasodilators. Restrictive cardiomyopathy: Supportive treatment for symptoms, treatment of hypertension,conversion, exercise restrictions emergency treatment of acute pulmonary edema. www.SimpleNursing.com Plasma brain natriuretic peptide Levels may reveal heart failure and its severity used as an ongoing tool to help to monitor the response to treatment. Serum troponin, creatine kinase (CK), and CK-MB levels may be acutely elevated if the patient has myocarditis or acute coronary syndrome. Liver function tests May be elevated. B-type natriuretic peptide Levels identify the presence and severity of fluid overload. Urine toxicology screening May detect drugs leading to cardiomyopathy. Elevated creatinine May be related to hypovolemia or ACE inhibitors as etiology. Angiography Results rule out ischemic heart disease. Chest radiography Demonstrates moderate to marked cardiomegaly and possible pulmonary edema. Echocardiography May reveal ventricular thrombi, global hypokinesis, and the degrees of left ventricular dilation and systolic dysfunction. Gallium scanning May identify patients with dilated cardiomyopathy and myocarditis. Cardiac catheterization Can show left ventricular dilation and dysfunction, elevated left ventricular, right ventricular filling pressures, and diminished cardiac output. Transvenous endomyocardial biopsy May be used in determining the underlying cause in some patients (cardiac transplant patients) including myocarditis, connective disorders and amyloidosis. Electrocardiography Identifies arrhythmias and intraventricular conduction defects, and may reveal nonspecific ST-T wave changes and Q waves. Want a video to follow along? Go to Simplenursing.com 3-13