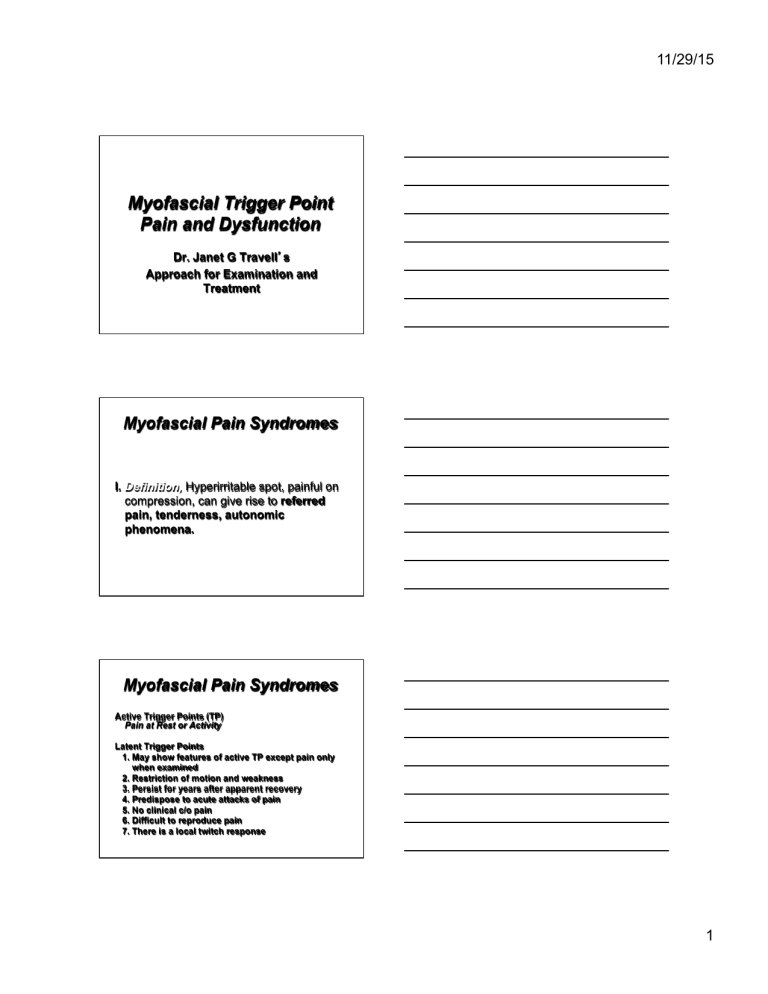
11/29/15 Myofascial Trigger Point Pain and Dysfunction Dr. Janet G Travell’s Approach for Examination and Treatment Myofascial Pain Syndromes I. Definition, Hyperirritable spot, painful on compression, can give rise to referred pain, tenderness, autonomic phenomena. Myofascial Pain Syndromes Active Trigger Points (TP) Pain at Rest or Activity Latent Trigger Points 1. May show features of active TP except pain only when examined 2. Restriction of motion and weakness 3. Persist for years after apparent recovery 4. Predispose to acute attacks of pain 5. No clinical c/o pain 6. Difficult to reproduce pain 7. There is a local twitch response 1 11/29/15 Myofascial Pain Syndromes II. Incidence 1. Latent TPs afflict nearly half the population. 2. Patients with chronic pain, MPS cause of pain in half of the patients. 3. Likelihood of developing active TPs increases with age. 4. Laborers who exercise their muscles every day less likely to develop active TPs than sedentary workers who become weekend warriors. Myofascial Pain Syndromes III. Symptoms 1. PAIN ONSET: Abrupt or Gradual (Chronic Overload) CHARACTER: Steady, Deep & Aching, Rarely Burning Referral: In Specific Patterns NOT Simple Segmental Patterns Pain Picture: A Precise Pictorial Representation of Pain is Needed for an Accurate Diagnosis. Myofascial Pain Syndromes III. Symptoms (continued) 2. LIMITED ROM AND STIFFNESS WORSE ON ARISING IN THE MORNING AND RECURS AFTER PERIODS OF OVERACTIVITY OR IMMOBILITY 3. WEAKNESS 4. OTHER NON-PAIN SYMPTOMS AUTONOMIC, PROPRIOCEPTIVE, REDUCED STIMULATION THRESHOLD AND DISTURBANCE OF MOTOR COORDINATION 5. DEPRESSION 6. SLEEP DISTURBANCE 2 11/29/15 Myofascial Pain Syndromes III. Symptoms (continued) 7. ACTIVATION Direct Activation: a) ACUTE OVERLOAD b) OVERWORK FATIGUE c) DIRECT TRAUMA d) CHILLING Myofascial Pain Syndromes III. Symptoms (continued) 7. Activation Indirect Activation: a) Other TP’s b) Visceral Disease c) Arthritic Joints d) Emotional Distress Myofascial Pain Syndromes Satellite TP’s - occur in muscles within the reference zone Secondary TP’s - occur in adjacent or synergistic muscles weakened or shortened by primary TP 3 11/29/15 Myofascial Pain Syndromes IV. PHYSICAL EXAMINATION 1. MOBILITY AND POSTURE 2. NEUROMUSCULAR EXAM 3. CUTANEOUS SIGNS (Dermatographia, Panniculosis) 4. COMPRESSION TEST 5. DISTURBANCE OF NON-SENSORY FUNCTION (ie autonomic, motor unit activity) 6. TRIGGER POINT EXAM a) TAUT BAND b) LOCAL TWITCH RESPONSE c) JUMP SIGN d) PRODUCE REFERRED PAIN Myofascial Pain Syndromes V. LAB FINDINGS 1. Routine Lab: No Abnormalities 2. EMG of involved muscle at rest NO Abnormalities 3. Thermograms over active TP may show increased skin temperature Myofascial Pain Syndromes VI. TREATMENT SPRAY AND STRETCH 1. PATIENT POSITIONED COMFORTABLY 2. STABILIZATION: ANCHOR ONE END OF MS 3. SPRAY SKIN OVER THE MS A) PARALLEL SWEEPS IN ONE DIRECTION B) 18 INCHES ABOVE THE SKIN C) 4 INCHES PER SECOND D) SPRAY ALONG REFERENCE ZONE E) HOLD BOTTLE AT A 30 DEGREE ANGLE 4. STRETCH MUSCLE PASSIVELY “STRETCH IS THE ACTION, SPRAY IS THE DISTRACTION” 4 11/29/15 Myofascial Pain Syndromes SPRAY AND STRETCH CONTINUED 5. REPEAT WITH PARALLEL AFTER REWARMING 6. MOVE MS THRU 3 CYCLES OF FULL ROM 7. RECOMMEND HOT BATH TO PATIENT AND HOME STRETCHING PROGRAM REASONS FOR FAILURE 1. PERPETUATING FACTORS 2. INADEQUATE SPRAYING OF ALL TP AREAS 3. PATIENT NOT FULLY RELAXED 4. INCORRECT SPRAYING TECHNIQUE 5. INADEQUATE STRETCHING TECHNIQUE 6. INCOMPLETE STRETCH 7. INCREASED MS SORENESS IF MUSCLE NOT REWARMED 8. RECURRENCE IF PATIENT FAILS TO ACTIVELY MOVE THRU FULL ROM 9. INCOMPLETE SPRAY AND STRETCH 10. NON COMPLIANCE WITH HOME EXERCISE PROGRAM Myofascial Pain Syndromes VII. ETHYL CHLORIDE VS FLUORI METHANE ETHYL CHLORIDE FLAMMABLE TOXIC GEN. ANESTHETIC EXPLOSIVE LOCAL CHILLING FLUORI METHANE NON-FLAMMABLE NON-TOXIC NON-ANESTHETIC NON-EXPLOSIVE NON-CHILLING 5 11/29/15 Myofascial Pain Syndromes VIII. PERPETUATING FACTORS A) MECHANICAL 1. ANATOMIC VARIATIONS; SHORT LEG, SHORT HEMIPELVIS, SHORT UPPER ARMS AND LONG SECOND METATARSAL (MORTON’S FOOT) 2. POSTURAL STRESS 3. CONSTRICTION OF MUSCLES (ie HEAVY PURSE, NARROW BRA STRAPS, TIGHT COLLAR,TIGHT TIE, TIGHT BELT, EDGE OF SEAT) Myofascial Pain Syndromes VIII. PERPETUATING FACTORS B) SYSTEMIC PERPETUATING FACTORS 1. NUTRITIONAL INADEQUACIES / ENZYME DYSFUNCTION a) THIAMINE B1 b) PYRIDOXINE B6 c) FOLATE AND COBALAMINS B9 AND B12 d) ASCORBIC ACID, VITAMIN C e) DIETARY MINERALS AND TRACE ELEMENTS Ca, K, Fe, Mg Myofascial Pain Syndromes VIII. PERPETUATING FACTORS B) SYSTEMIC PERPETUATING FACTORS 2. METABOLIC AND ENDOCRINE DYSFUNCTION a) HYPOMETABOLISM (ie LOW THYROID) b) HYPOGLYCEMIA c) HYPERURICEMIA AND GOUT 6 11/29/15 Myofascial Pain Syndromes VIII. PERPETUATING FACTORS B) SYSTEMIC PERPETUATING FACTORS 3. CHRONIC INFECTION a) VIRAL DISEASE b) BACTERIAL INFECTIONS c) INFESTATIONS d) ALLERGIC RHINITIS 4. PSYCHOLOGICAL FACTORS Myofascial Pain Syndromes IX MYOFASCIAL PAIN vs FIBROMYALGIA 1. FM may initially be isolated to a few well-defined locations prior to spreading. Therefore, FM may represent a generalized form of MPS. 2 MPS which have become chronic may resemble FM involving multiple sites and causing systemic symptoms. Myofascial Pain Syndromes IX MYOFASCIAL PAIN vs FIBROMYALGIA 3. Simons feels its necessary to distinguish these 2 conditions. Etiology of FM is usually systemic whereas MPS is related to focal dysfunction of the muscle. 4. Mayo Clinic uses term Tension Myalgia for Fibrositis, FM and MPS. They use 3 broad categories a) Generalized Tension Myalgia- Corresponds to FM b) Localized Tension Myalgia- Corresponds to MPS c) Regional Tension Myalgia pts with symptoms between the other two categories 7 11/29/15 TRIGGER POINTS INCREASED BY 1. Strenuous use especially in shortened position. 2. Passive quick stretch of a muscle 3. Direct pressure 4. Involved ms in short position for prolonged period 5. Sustained or repeated contraction 6. Cold damp weather, viral infection, tension 7. Exposure to cold draft (ie: air conditioner) 8. Cold packs applied to TP area continuously TRIGGER POINTS DECREASED BY 1. Short period of rest 2. Slow steady passive stretch ( hot shower or bath) 3. Moist heat applications 4. Short periods of light activity 5. Specific Myofascial Therapy Alternative Treatment Techniques for Myofascial Trigger Points 8 11/29/15 ISCHEMIC COMPRESSION * Noninvasive, Effective but Painful * Pressure applied to most tender spot * Pain eases, pressure increased * TP no longer painful release pressure, and perform AROM * Procedure causes ischemia, followed by reactive hyperemia * Advise patient pain will increase during Tx. Post –Isometric Relaxation * Stretch muscle to onset of resistance * Patient contracts against fixed resistance - 25% of maximal effort 6-10 seconds * Maintain the position passively the patient “ Let’s go” * Cycle is repeated 3-5 times Deep Muscle Massage 1. Deep Friction- Purpose to move superficial tissue over underlying structures. 2. Cyriax Deep Friction – Across the muscle long axis. 3. Stripping- Digital Pressure starts at distal end, fingers slide across muscle length, gradually increase pressure, continue motion over and beyond the TP 4. Strumming- Painful deep release technique, performed with fingers in rigid extension, scrubbing motion parallel to muscle fibers, follow with interferential, TENS, VMS and ice 9 11/29/15 Modalities Ice Massage Two Techniques 1. Intermittent use instead of spray 2. Non-specific application of cold, principle similar to TENS Cold plus stretch gives more sustained relief than cold alone Excessive cold decreases muscle resting length Modalities Ultrasound - May be used by itself or in combination with electrical stimulation (Medco-sonlator) Can be helpful Diagnostically and therapeutically Modalities Heat - Moist heat relaxes muscles and diminishes tension on the TP’s Patient’s home exercises are more effective if done immediately after heating 10 11/29/15 Modalities Biofeedback- Not a direct myofascial technique, addresses the fact that patient’s express anxiety through increased muscle tension TENS- Non specific pain relief may help regain mobility Modalities Dry Needling Ø This is a general term for a therapeutic procedure that involves multiple advances of a filament needle into a muscle in the area of the body which produces pain and typically a trigger point. There is no injectable solution and typically the needle that is used is very thin. Modalities States that do not support PT’s using Dry Needling are as follows: via KinetaCore PT education services California, Connecticut??, Delaware ??, Florida, Hawaii, Idaho, Utah, Indiana ??, Kansas, Maine ??, Michigan??,MN?, MO?? NY,PA, SD, TN,WA? 11 11/29/15 Contraindications to Stretching 1. 2. 3. 4. When bony block limits joint movement After recent fracture Presence of acute inflammation or infection Sharp or acute pain with joint movement or muscle elongation 5. Hematoma or other tissue trauma 6. When contractures / shortened soft tissue is providing increased joint stability 7. When contractures / shortened soft tissue is a basis for increased functional abilities (ie SCI or CVA patient’s –Tenodesis) Rehabilitation Exercises Manual Stretching Home Exercise and Self Stretching Aerobic Exercise Strengthening Exercise Eccentric lengthening reactions to increase function and restore muscle to its normal resting length JOINT PLAY “Voluntary movements cannot be achieved unless certain well defined movements of joint play are present. Movements of joint play are independent of the action of the voluntary muscles….Their integrity, not their range, is the basis of their importance. It is the summation of the movements of joint play and the movements of the voluntary range that make up the movements of the living anatomy” Mennell 12 11/29/15 THANK YOU! 13 11/29/15 14 11/29/15 15 11/29/15 16 11/29/15 17 11/29/15 18 11/29/15 19 11/29/15 20 11/29/15 21 11/29/15 22 11/29/15 23 11/29/15 24 11/29/15 25 11/29/15 26 11/29/15 27 11/29/15 28 11/29/15 29 11/29/15 30 11/29/15 31 11/29/15 32 11/29/15 33 11/29/15 34 11/29/15 35 11/29/15 36 11/29/15 37 11/29/15 38 11/29/15 39 11/29/15 40 11/29/15 41 11/29/15 42 11/29/15 THANK YOU! 43