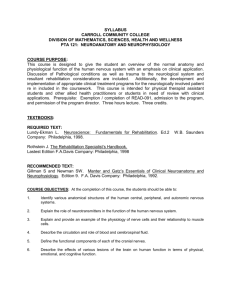
File Name: NG Gen FT POlO J£ Mlbme:an1tldl1ll5drtilfse 9iiatt HealIh Smt:t ~ TITLE: HSEWest Page I of 11 Mid Western Regional Hospital Dooradoyle, Limerick, Ireland Nursing Service Neurological Observations - Adult (Over Age 16Yrs) EDITION NO: 3 DATE OF ISSUE: REVIEW INTERVAL: COPY: 45 (Full Text) Every2Yean AUTHORIZED BY: Iv.. ' TITLE: r, w.nL.'\,.( JI;.~ Gerardine Kennedy ADONlNlD'Se Practice Development Unit ).A.o. '4A. ~ 0. 0"",,-. AlDirector ofNlD'Sing Vo Maura Fitzgerald AUTHOR(S) TITLE: Ann Reidy Caroline Bridgeman Sheila Sheehy Clinical Placement Coordinator Staff Nurse Staff Nurse LOCATION OF COPIES: RELATED DOCUMENTS: IB; IC; ID;AIE;2B; 2C; 2D; 3A; 3B; 3C; 3D; 4B; Trauma, ICU; HDU; CCU; HODU; AMAU;)(RAY; 1. Neurological Observation Chart. MWRH, Endoscopy Haemodialysis; SOW; SlUlshine; Dooradoyle, (June 2008). Rainbow; Caterpillar; OPD & Dermatology; Pulmonary FlUlction; Diabetic Unit; CAAU; Main 2. Report Writing Policy & Guideline, Theatres; Day Theatres; Eye Theatres; NPDU; ADON MWRHs, (2005). Office; DON Office; Allocations Office :. Oncology CNS, Haematology CNS, Palliative Care 3. Nursing Care Plan Guideline, MWRH, (2008). CNS, Breast Care CNS, Stoma Care CNS, Clinical Trials, Haemovigilance, Phlebotomy Room, Smoking Cessation DOCUMENT REVIEW HISTORY Review Date June 2010 Reviewed/Edited By Signature File Name: NG Gon FT P 010 tE Feidhmeannaclll na Seirlhlse SWnte Health Service Execulhc TITLE: 1.0 HSEWest Page2 0fll Mid Western Regional Hospital Dooradoyle, Limerick, Ireland Date Written: 9TH May Nursing Service Neurological Observations - Adult (Over Age 16Yrs) 2008 (Full Text) PURPOSE 1.1 This guideline is intended to give guidance to nursing staff on the assessment and monitoring of patients who are potentially at risk of neurological deterioration. The guideline aims to provide information on the correct use of the Neurological Observation chart and how to interpret the findings. 2.0 SCOPE 2. 1 The guideline applies to all Nursing Staff and Student Nurses Under supervision in order that appropriate assessment and monitoring of patients who are potentially at risk of neurological deterioration is performed 2.2 It is the Nursing staff's responsibility to assess, monitor and record neurological observations , and to liaise with medical team/s as appropriate 3.0 DEFINITION 3.1 The assessment and classification of patients who have sustained a head injury should be guided by the adult version of the Glasgow Coma Scale (Please see appendix 1) 3.2 The Glasgow Coma Scale is a numerical grading system used to establish a patient's level of consciousness following a head injury. This provides an essential baseline for comparison scores .Its graphic, visual format ensures uniformity and gives a quick, concise, visual interpretation of the patient's level of consciousness and neurological status over a period of time. 4.0 PRE PROCEDURE CONSIDERATIONS 4.1 For patients admitted with a head injury the minimum acceptable documented neurological observations must include :The Glasgow Coma Scale: (GCS); pupil size and reactivity; limb movements, respiratory rate, heart rate; blood pressure, temperature and blood oxygen saturation. 4.2 The GCS evaluates three key categories of behaviour that most closely refiect activity in the higher centres of the brain. File Name: NG Gen FT POlO HSE West tE Page 3 ofll Feidhmeannadu na Seirtitist SWnte Ifcalth ServIce ExccutM! TITLE : Mid Western Regional Hospital Dooradoyle, Limerick, Ireland Date Written: gTH May 2008 Nursing Service Neurological Observations - Adult (Over Age 16Yrs) a. Eye opening b. Verbal response (Full Text) c. Motor response. The patient is assessed and scored in each area and the scores are added together to give the patients Glasgow Coma Score- the maximum score is 15; indicating an awake, alert and fully responsive patient and the lowest score is 3; indicating total unresponsiveness. A GCS score of 8 or less defines coma in 90% of cases. (Robertson 2003). 4.3 Head injured patients who warrant admission should have neurological observations carried out and recorded on a half hourly basis until GCS equal to 15 has been achieved or until discontinued by the medical team. 4.4 The minimum frequency of neurological observations for patients with a GCS score equal to 15 is as fol lows a. Half hourly for 2 hours b. I-hourly for 4 hours c. 2-hourly thereafter (NICE 2007). Should a patient with GCS equal to 15 deteriorate at any time after the initial 2-hour period, observations should revert to half hourly and follow the original frequency schedule 4.5 Important Factors for monitoring neurological observations a. Use all parts of the neurological observation chart. b. Record only what you see c. Listen to family members and friends d. Report any changes in the patients e. Do not be influenced by previous observations f. Do not use nail pressure or sterna I rub cond~ion 5.0 Procedure Explain procedure to the patient and gain their consent where possible. File Name: NG Gen FT POlO HSE West J£ Page40fll Mid Western Regional Hospital Dooradoyle, limerick, Ireland Feidhmeannacht na SeirItUse Si:iinle Ik:!aIth Service Ea'CutiYe TITLE: Date Written: 9TH May 2008 Nursing Service Neurological Observations - Adult (Over Age 16Yrs) (Full Text) 5.1 Table 1 How to use the Glasgow Coma Scale Eye Opening If the patient is unable to open his or her eye/s as a result of trauma or surgery, the letter (C) indicating closed-should be recorded in the first box. Otherwise this section should be completed as follows Score Method Eyes open spontaneously as you approach. If the patient is asleep wake the patient, 4 = Spontaneously ensuring he/she is fully roused and then complete the assessment he patient will respond to your voice. The best way to do this is to say his/her name. If there 3 = To Speech is no initial response, a raised voice should be used. The patient opens his/her eyes to painful stimuli. The best way to do this is to apply 2 = , To Pain = peripheral painful stimuli, see Table 2. Avoid central painful stimu li. No Response The patients eyes remain closed despite painful stimuli Best verbal response The patient may have difficulty in speaking (dysphasia).lf so the letter (0 ) should be recorded in the 'none' column. If the patient is intubated then the letter (T) should be recorded in the 'none' column This indicates the patient's orientation to Time, Place and person 5 = 4 Orientated - Confused he patient must be able to state his/her name where he /she is and the month of the year The patient is able to hold a conversation but is unable to answer the above questions correctly he/she should be considered confused.( Correct any wrongly answered questions) Change the order of questions to avoid the patient just repeating them 3 = Inappropriate The Patient uses random words rather than sentences, which make little sense in the context of the questions asked sometimes these words are words communicated as obscenities. - 2 he patient will only respond with moaning and groaning . Painful stimuli may be required to Incomprehensible sounds , = No Response gain a response There is no verbal response despite painful stimuli File Name: NG Gen FT POlO HSEWest tE Page 5 of 11 Fei.1Iune:annadJ1 !la SeirtWse SWore IleaIth SCrvicc £xccuU\>e TITLE: Mid Western Regional Hospital Dooradoyle, Limerick, Ireland Date Written: 9TH May 2008 Nursing Service Neurological Observations - Adult (Over Age 16Yrs) (Full Text) Best motor response- This indicates brain function A Deterioration of 1 point in the motor response or an overall deterioration of 2 pOints in the GCS is clinically significant and must be repotted immediately to medical staff (NICE, 2007) 6 - Obeys commands Ask the patient to perform a couple of different movements such as sticking out his/her tongue or lift up his/her arm 5 = Localises to pain ""pplya central painful stimulus using one of the recommended methods outlined in Table2 The patient should purposefully move his/her arm towards the site of pain to remove the cause of pain. 4 = 3 - Withdraws from pain Flexion to pain The patient will flex hisfher arm to pain but will not move towards the source of pain . The patient will flex his/her arms in response to pain but the wrist will also rotate. Often th thumb will also flex and move across or through the fingers 2 = Extension to pain Arms will straighten and the shoulder will rotate inwards when a painful stimulus is applie The legs may also straighten with the toes pointed downwards. 1 = No Response There is no physical response despite painful stimuli. (SHAH, 1999, Crawford and Guerrero, 2004, Waterhouse, 2005 Cited by Dawes E et al , 2007) Table 2 METHODS OF APPLYING PAINFUL STIMULI Central painful stimuli Method Action Evidence the thumb and forefinger take hold of Shah 1999, Wood row 2000, Mooney and Trapezius pinch or Using squeeze approximately 5cm of the trapezius muscle and twist Comerford 2003, Crawford and Geurrero 2004, Waterhouse 2005 Jaw Pressure Apply pressure with the thumb to the j aw, just in front Woodward 1997a, Waterhouse 2005 of the earlobe. This method should not be used if the patient has sustained any head or facial trauma Supra - orbital Feel along the medial aspect of the edge of the bone Shah 1999, Wooddrow 2000. Mooney and pressure above the eye for a groove or notch; apply pressure Comerford 2003, Crawford and Guerroro here with the thumb. This method should not be used 2004, Waterhouse 2005 if the patient has sustained any head or facial trauma Peripheral painful stimuli Method Action Evidence Lateral finger or toe Using a pen apply pressure to the lateral aspect of a Waterhouse 2005 pressure finger or toe. Rotate the pen around the finger in opposite direction to the nail. This should be performed for no longer than ten seconds File Name: NG Gen FT POl O J£ Feidhmeannac.ht IU SeirtDise S1:iime HSEWest Page 6 of 11 Mid Western Regional Hospital Dooradoyle, Limerick, Ire land I b1th SCrvicc Exi.'CutM! TITLE : Date Written: 9TH May 2008 Nursing Service Neurological Observations - Adult (Over Age 16Yrs) (Full Text) POINTS OF NOTE 5.2 A good sensitive indicator of neurological change is the patient's level of consciousness Is the patient becoming more difficult to rouse? Patients will often become more restless, or a previously restless patient will become atypica lly quiet. 5.3 Painful stimuli should only be carried out by experienced professionals and should not be applied to the lower limbs when assessing consciousness as any response elicited may be the result of a spinal reflex and could be confused with an appropriate response 5.4 Painful stimuli should only be used if the patient does not respond to firm and clear commands. 5.5 Only use the least amount of pressure to elicit a response to avoid bruising. 6.0 Vital Signs It is recommended that vital signs should be assessed in the following order: • Respirations • Temperature • Blood pressure • Pulse • P02 6. 1 Note that Respiratory patterns give the clearest indication of how the brain is functioning because the process of respiration is controlled by more than one area in the brain. (Oougherty and Lister (eds), 2004). File Name: NG Gen FT P 010 HSE West J£ Page70f ll Feidhmeannacht III SdrbhIse ~nlt licalth SCoice EJccutM! TITLE: Mid Western Regional Hospital Dooradoyle, limerick, Ireland Date Written: 9TH May 2008 Nursing Service Neurological Observations - Adult (Over Age 16Yrs) (Full Text) 7.0 Observation of pupil response a. Inform the patient and explain what you are going to do, b. Reduce the light from overhead lights Table 3 Observation of pupil response Observation Method General Observation Look at the shape of the pupils and their position. (Consider any underlying disease or medication) Is the eye too swollen to open? Attempts should be made to open a mildly swollen eye but if it too painful or the swelling is prolific the letter 'C' for closed should be recorded in the observation chart Pupil Size The size of the eye is measured in millimetres- a guide is given on the side of the neurological observation chart (Appendix 1). Use this guide so that the results are objective Record the size of the pupil at rest before any light is shone into the eye Pupil response To check the pupil response, move a bright pen torch from the outer aspect of the eye directly over the pupil. The pupil should constrict quickly. The pupil should dilate again when the bright light is moved away Repeat the test in the other eye Both eyes should constrict when a light is shone into one eye .This is called consensual reaction. These reactions are recorded as (+) for reaction (SI) for a sluggish reaction and (-) for no reaction Any changes in pupil reaction, shape or size are a late sign of raised intracranial pressure. Sluggish or suddenly dilated unequal pupils are an ind ication that oedema or haematoma is worsening and the oculomotor cranial nelVe is being compressed . Urgent intervention is required at this stage. File Name: NG Gen FT POlO HSE West tE Page 8 of 11 Fekihme:annachl. Ra Sei.rt:Wse SWnre lie2lth Service ExccullYe Mid Western Regional Hospital Dooradoyle, Limerick, Ireland Date Written: 9TH May 2008 Nursing Service Neurological Observations - Adult (Over Age 16Yrs) TITLE: (Full Text) 8.0 Limb Response a. Assess and record each limb separately (Waterhouse 2005). b. The observation chart should be marked with (L) for left limbs and (R) for right limbs c. Assessment of limb responses are best performed when the patient is lying down d. Carry out limb response as detailed below Table 4 Observation of limb movement Observation Result Method Normal power The patient will be able to push against resistance To determine whether the patient has with no difficulty normal power, mild or severe weakness. The patient will be able to push against restraints but Each limb is assessed and recorded will be easily overcome separately. Mild weakness Severe weakness Spastic flexion The patient will be able to move his/her limbs independently but will be unable to move against Arms -wh ile holding the wrist ask the resistance patient to pull you towards him/her towards The patient's limbs will flex in response to pain you and then push you away. painful stimuli. Arms wrists and possibly the thumb Extension will bend inwards. Legs will pull upwards Legs - holding the top of the ankle ask the The patient's limbs will extend in response to painful patient to lift his Iher leg off the bed then stimuli. Elbows ,wrists and fingers will straighten holding the back of the ankle ask the stiffly down the side of the body. Legs will stiffen and patient to pull the leg towards him/her feet will point downwards No response There is no motor response despite central and To determine a response of spastic f1exion peripheral painful stimuli. or extension apply central painful stimuli. If no response is elicited use peripheral painful stimuli. File Name: NG Gen FT P 010 tE FeidJureannachllll Selrbhfse SWnIe Health Smicc Exccume TITLE: 8.0 HSEWest Page 9 of 11 Mid Western Regional Hospital Dooradoyle, Limerick, Ireland Date Written : gTH May 2008 Nursing Service Neurological Observations - Adult (Over Age 16Yrs) (Full Text) POST PROCEDURE 8.1 The results of all assessments and any action taken should be recorded as per current Hospital Policy on documentation 8.2 Dots (.) not ticks or numbers must be used to fill out the Glasgow Coma Scale. The dots may be joined to fonn a graph ( Appendix 1 ) 8.3 Monitoring and exchange of infonnatlon about individual patients should be based on the three separate responses on the GCS. For example. a patient scoring 13 based on scores of 4 on eye opening. 4 on verbal response and 5 on motor response should be communicated as (E4. V4. and MS) 8.4 If a total score is recorded or communicated it should be based on a sum of 15. and to avoid confusion the denominator should be specified (for example 13/15). 8.5 The individual components of the GCS should be described in all communications and should always accompany the total score (for example E4. V4. MS. 13/15). 9.0Any of the following examples of neurological deterioration should prompt urgent reappraisal by the supervising doctor a Development of agitation or abnonnal behaviour b Any drop of three or more points in the eye-opening or verbal response scores of the Glasgow Coma Scale, or two or more points in the motor response score c Development of severe or increasing headaches or persisting vomiting d New or evolving neurological symptoms or signs. such as pupil inequality or asymmetry of limb or facial movement. 10.0 It is important to identify report and document any changes however subtle. (NICE 2007). 11 .0 Nurses should initiate the Neurological Observations Chart wherever they deem necessary for the appropriate care of patient 12.0 Consultation Trail This Guideline has been reviewed by the following: Consultant Anaesthetist Or. O'Dea Pauline Chapman AlCPC File Name: NG Gen FT POlO J£ Feidhrneannachl n Sei.1ti!ise SI:1in1e Heallh SCrvX:e Exccutlw: TITLE: HSEWest Page 10 of IJ Mid Western Regional Hospital Dooradoyle, Limerick, Ireland Date Written: 9TH May 2008 Nursing Service Neurological Observations - Adu lt (Over Age 16Yrs) (Full Text) REFERENCES Crimlisk Janet T. Grande Margaret M. (2004). Neurological Assessment Skills for the Acute Medical Surgical Nurse Orthopaedic Nursing Dawes E. et al (2007). Monitoring and record ing patients neurological observations Nursing Standard Vol22 No 10 40-45 Dougherty, I, & Lister, S., (eds.), The Royal Marsden Hospital Manual of Clinical Procedures, 61h edition, The Royal Marsden NHS Foundation Trust. Edwards L (200 1). USing the Glasgow Coma Scale analysis and limitations British Journal of Nursing 2001. Vol19 No 2 92-101 National Institute for Health and Clinical Excellence (2007) .Head Injury NICE clinical guideline 56 developed by the National Collaborating Centre for Acute Care Mooney G.P. (2005) Neurological Observations Nursing Times Vol.99 No 1725 Waterhouse C. (2005). The Glasgow Coma Scale and other neurological observations Nursing Standard. Vol 19 No 23 56-62 File Name: NG Gen FT P 010 HSEWest tE Page 11 of 11 Mid Western Regional Hospital Dooradoyle, Limerick, Ireland feidhmeannadl1 ll2 Sdrbh!se SWrue Date Written: 9lH May 2008 Health ServIce ExecuU\le TITLE : Nursing Service Neurological Observations· Adult (Over Age 16Yrs) (Full Text) 12,0 APPENDIX 1 NEUROL.OGICAi. OBSERvAnoN CHART :: 1 :: ........ u._" ......- .. • ...... . , . ~ -_. - - . , , o -, • • , • • • • I'- ' •PlI!!f! .,,' " " ,'~ , • ,,.. , 1 F~.=. ; r. ! •r --'~ [ ,,, s...._fIU 6_ ',,- ___ ~ _ dI I - ~.i' , ~ ...,....... .. 0 1 -=-f.... ...'- ~ - • . - • ..... •• -... --..... .. ........ ---_ ... I.-~ ,5.. . , -~ . ~- ,, , "- • , •• r- ~ ,~ ---,." ~,_()f '1" · • • ... .......... . :r.L!o ,;. • • " _ K' ~ . ' • • .... M ,.,.., " "" D . v '" -'-" - "'"M' .... , . ~ ~ , ,- , .- ~ l I .. '", - ,,.. , - t: ( (,. ....M --" ...... -~ '"' ,." =-t Qmil,5::lfe · II ' -"""' _ _G'aIgcw _ -"- " ." ,. ... , .,,- " ~ = . .-. -_........'" 15 Pdnt