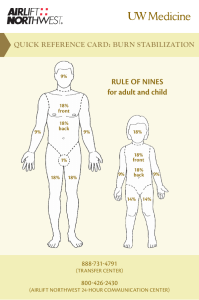
Burn injury burn : transfer energy from a heat source to the body. Burn wound occur when there is contact between tissue and an energy source and destruction of the integumentary system. The major cause of fires in the home and burn injury in the USA is carelessness with cigarettes & hot water from water heater, and in Pakistan the most cause of burn injury from misuse of gasoline heater, cooking accident & suicidal attack. Types of burn injury 1. Thermal burns : ( most common type ), can be caused by flam, flash, or contact with hot objects. 2. Chemical burns : alkali burns and acid burns. 3. Electrical burns. 4. Inhalation ( smoke ) injury 5. Radiation burns. 6. Cold thermal injury ( frostbite ) . Thermal Burns • Most common (2/3 burns) • Examples: flame, hot surface, sunburn, hot water, hot metal, hot grease, frost bite Chemical Burns • Common in industry • Caused by strong acids or alkali • Severity of the burn depends on amount of time chemical was in contact with the skin Electrical Burns • Difficult to determine extent of damage since most of the burn involves deeper layers • Passage of electrical current may cause cardiac arrest &/or cardiac dysrhythmias Inhalation Burns • Definition: burn of the respiratory tract • Caused by inhalation of toxic products or smoke in an enclosed space Ionizing Radiation Burn • Often occurs when a patient receives an overdose of radiation Cold thermal injury ( frostbite ) . Classification of burn injury The treatment of burns is related to the severity of the injury . Severity is determined by : 1- Depth of burn. 2- Extent of burn calculated in percent of total body surface area ( TBSA). 3- Location of burn. 4- Patient risk factors. Depth of burn According to American Burn Association there are new categorizing to the burn : • Superficial burn (first degree burn ) • Superficial partial-thickness burn ( second degree ) : moist, blister, some blanching. Deep partial-thickness burn ( second degree ) :dry, pale, waxy, no blanching. • Full thickness ( third degree ) : white, cherry red, black. Very painful, dry, red burns which blanch with pressure. They usually take 3 to 7 days to heal without scarring. Also known as first-degree burns. The most common type of first-degree burn is sunburn. Firstdegree burns are limited to the epidermis, or upper layers of skin. Very painful burns sensitive to temperature change and air exposure. More commonly referred to as second-degree burns. Typically, they blister and are moist, red, weeping burns which blanch with pressure. Scarring is usually confined to changes in skin pigment. Second – degree burns Blistering or easily unroofed burns which are wet or waxy dry, and are painful to pressure. Their color may range from patchy, cheesy white to red, and they do not blanch with pressure. It is sometimes difficult to differentiate these burns from full-thickness burns. Third – degree burns Burns which cause the skin to be waxy white to a charred black and tend to be painless. Healing is very slow, if at all, and may require skin grafting. Severe scarring usually occurs. Characteristics of burns of various depth: Extent of body surface area injured • Various methods are used to estimate the TBSA affected by burns among them are the rule of nines, the Lund and Browder method and the palm method Rule of nine • An estimation of TBSA involved in a burn is simplified by using rule of nine • It is a quick way to calculate the extent of burn • The sytem assigns percentages in multiples of nine to major body surfaces Lund and browder method • Recognizes the percantages of TBSA of various anatomic parts especially the head and legs and changes with growth • By dividing the body into very small areas and providing and estimate of the proportion of TBSA accounted for by such parts , one can obtain a reliable estimate of the TBSA burned Palm method • In patient with scattered burns, a method to estimate the percantage of burn is the palm method • The size of the patient´s palm is approximately 1% of TBSA Local and systemic resposes to burns • Burns that do not exceed 25% TBSA produce a primarily local response • More than 25% produce both a local and a systemic response and considered major burn injury • System response is due to the release of cytokines and other mediators into the systemic circulation • The release of local mediators and chanes in blood flow , tissue edema and infection can cause progression of the burn injury Medical care • Laboratory: • CBC show eleveted hematocrit due to hemoconcentration and later decreased hematocrit may mean vascular damage to endothelium, white blood cell count may increase due to inflammatory response to the trauma and wound infection • WBC count may increase due to inflammatory response to the trauma and wound infec tion Medical care • WBC can be as high as 30,000 mm initially, but resolves within 2 days • Leukopnia may occur as a side efect from silver sulfadiazine • Thrombocytopenia may result within the first 72 hours because of hemodilution and potential microthrombi, protein and albumin are decreased • Because of protein loss from increased vascular permeability, coagulation studies usually will show increased prothrombin and partial thromboplastin time during the first 72 hours after injury as a result of leakage of clotting factors from the intravascular space Medical care • Electrolytes may show initially hyperkalemia resulting from injury, later changing to hypokalemia when duiretic phase begins, sodium initially decreased with fluid loss and later changes to hypernatremia when renal system attempt to conserve water, alkaline phosphatase elevated, glucose elevated from stress reaction, albumin decreased, creatinine elevated because of renal dysfunction • Carboxyhemoglobin may be done to identify carbon monoxide poisining with inhalation injury Medical care • Radiography: chest x-ray used to identify complications that may occur as a result of inhalation injury or with fluid shifting from rapid replacement • Arterial blood gases: used to identify hypoxia or acid base imbalances, acidosis may be noted because of decreased renal perfusion, hypercapnia and hypoxia may occur with carbon monoxide poisining Medical care • Lung scan:to identify magnitude of lung damage from inhalation injury • Electrocdiogram: used to identify myocardial ischemia or dysrhythmias that may occur with burns or electrolyte imbalances • Analgesics: required to reduce pain associated with tissue damage and nerve injury • Tetanus toxiod: required to provide immunity against infective organisms • Antimicrobials:required to treat infection Medical Care • surgery: required for skin grafting, fasciotomy, debridement, or repair of other injuries • IV fluid: massive amount of IV fluids may be required for fluid resuscitation immediately post burn and will be required for maintenance of fluid balance as shifting occurs BURN MANAGEMENT Wound Management • • • • Pain control through IV Cleanse and debride Apply topical antimicrobial agent Instruct patient/family on home care and expected outcomes • Teach signs/symptoms of infection Topical Antimicrobial Agent • • • • Silver sulfadiazine (Silvadene Cream 1%) Mafenide Acetate (Sulfamylon) Nanocrystalline silver (Acticoat) Silver nitrate solution (0.5%) Infection Control • Bathe or clean the whole body (MONITOR TEMPERATURE) • Debride burned areas • Shave hair in burned areas • Wash and cut hair if scalp is burned Dressings • Apply topical agent and cover with dressing • Elevate burned extremity • Fit and apply appropriate splints Grafts • Autograft (same individual) – Split thickness – Full thickness – Muscle flaps • Allograft (same species) • Xenograft (different species) Photo from www.medlineplus.gov Escharotomy • Procedure used to reduce pressure in burned area by splitting eschar open with surgical scalpel • Used when there is decline/absence of pulse or changes in breathing pattern Photo from www.burnsurgery.org Escharotomy for upper extremity and chest. Escharotomy for lower extremity Escharotomy for upper extremity post electrical burn. SCAR MANAGMENT • Use silicone gel sheets under pressure garment • Wear pressure garments 23 hours/day for 1 year • • • • • CRITERIA FOR TRANSFER TO BURN CENTER >10% TBSA in patients • Significant chemical <10 years and >50 years of age >20% TBSA between 11-49 years of age Face, eyes, ears, hands, feet, genitalia, perineum, or joints Full-thickness >5% Electrical burns burns • Inhalation injury • Preexisting illness that could complicate • Require special social, emotional, or long-term rehabilitative support Physical Therapist’s Role • Wound management (extent depends on facility) • Prevent contractures – – – – • • • • Splinting Massage Positioning Pressure garments Maintain or increase ROM Maintain or increase muscular strength Maintain or increase cardiovascular endurance Return to function Physiotherapy items in the after care of a burn patient 1. Exercising, training and ambulation 2. Mobilisations and oedema control 3. Positioning and splinting 4. Scar management Physiotherapy items in the after care of a burn patient 1. Exercising, training (and ambulation) -Mobility and ADL -Muscle strength and cardiovascular condition! (24 - 48h after trauma) Physiotherapy items in the after care of a burn patient 2. Mobilisations and oedema control -Prevention & treatment contractures (type?) Considered Best Practice Physiotherapy items in the after care of a burn patient 3. Positioning and splinting -Prevention & treatment contractures -Static versus dynamic Physiotherapy items in the after care of a burn patient 4. Scar management - Pressure Therapy -Prevention & treatment of hypertrophic scars -fastening healing, flattening and itch reduction Physiotherapy items in the after care of a burn patient 4. Scar management - Silicone -Prevention & treatment of hypertrophic scars Hydration Considered Evidence Based (gel sheeting) Thank you Together, we can make a difference!