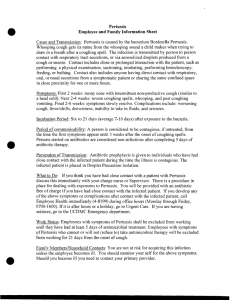
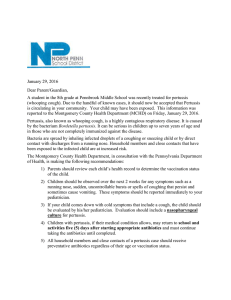
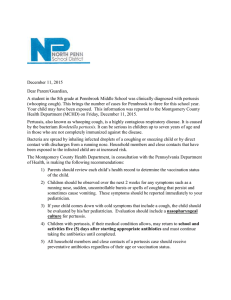
Bordetella Introduction The Genus Bordetella is named after Jules Bordet, who along with Gengou, identified the small ovoid bacillus causing whooping cough in the sputum of children suffering from the disease (1900) and succeeded in cultivating it in a complex medium ( 1906). The bacillus is now known as Bordetella pertussis (pertussis meaning intense cough). A related bacillus, Bord parapertussis was isolated from cases of whooping cough (1937). Bord bronchiseptica isolated from dogs with bronchopneumonia (1911) occasionally infect human beings, producing a condition resembling pertussis. The fourth member of the genus is Bord avium which causes respiratory disease in turkeys. Bordetella pertussis Morphology It is Gram negative. It is a small, ovoid coccobacillus ( 0.5 μm). It is nonmotile and nonsporing. It is capsulated. Freshly isolated strains of Bord pertussis have fimbriae. Cultural characteristics Aerobic Grows optimally at 35 to 37˚C Complex media are necessary for primary isolation Preferred medium – Bordet Gengou glycerin potato blood agar ◦ Blood for neutralizing inhibitory substances formed during bacterial growth. ◦ Charcoal also serves the same purpose. Charcoal blood agar is a useful medium. Colonies on bordet gengou medium Growth is slow(48-72 hours). Colonies are small, dome shaped, smooth, opaque, viscid, greyish white, refractile and glistening, resembling 'bisected pearls‘ or 'mercury drops'. Surrounded by a hazy zone of hemolysis. Confluent growth presents an 'aluminium paint‘ appearance. Biochemical reactions Do not ferment sugars Indole test + Nitrates + Citrates + Urease + Catalase + Oxidase + Resistance It is a delicate organism, being killed readily by heat (55°C for 30 minutes), drying and disinfectants. Outside the body, Bord pertussis in dried droplets is said to survive for five days on glass, three days on cloth and a few hours on paper. Antigenic properties virulence factors Toxins Trachealcytotoxin: lt is a part of cell wall peptidoglycan, which causes damage to the cilia of respiratory epithelial cells by producing interleukin-1 and nitric oxide intracellularly. Pertussis Toxin (PT) It is the most important virulence factor, and is expressed only by B. pertussis, B. parapertussis and B. bronchiseptica possess the genes coding for PT, but due to mutation in the promoter region of the genes,. they do not express PT. Adenylatecyclase toxin: It activates cyclic AMP, which impairs the host immune function. Dermonecrotic toxin: it may contribute to the respiratory mucosal damage. Endotoxin: It has properties similar to those of other gram-negative bacterial LPS. Adhesins: they play a role in bacterial attachment. Examples include: Filamentous hemagglutinin (FHA) Pertactin, an outer-membrane protein Fimbriae or pili or agglutinogens BrkA (Bordetella resistance to killing) protein: It mediates the serum resistance and adhesion. Pertusis toxin Mechanism: PT is similar to cholera toxin in its structure and is composed of A and B subunits. B subunit: It is pentameric, responsible for binding to target cells and inserting A-subunit into the cytoplasm. A subunit: It is the active subunit, which causes ADP ribosylation of G protein, which activates adenylyl cyclase, leading to concentrations of cAMP; which is responsible for producing a variety of biologic effects, such as: ◦ T cell mitogeniclty ◦ Hemagglutination ◦ Adhesion to respiratory ciliated cells ◦ Inhibition of neutrophil oxidative burst monocyte migration, histamine release from mast cells ◦ Induction of leukocytosis ◦ Enhancement of insulin secretion leading to hypoglycemia Characteristics of bordetella species Clinical features Incubation period : 7- 10 days 3 stages:Catarrhal phase: lasts for 1-2 weeks, ◦ Characterized by common cold like non specifc symptoms, such as coryza, lacrimation, mild cough, low-grade fever and malaise. ◦ It is highly infectious stage. ◦ Both smear and cultures are likely to be positive. Convalescent stage: ◦ The frequency and severity of coughing gradually decreases. ◦ Antibodies may appear in serum. Paroxysmal phase: ◦ Patients are less infectious; smear and culture may become negative. ◦ It is characterized by specific symptoms, such as whooping cough and posttussive vomiting. Whooping Cough Each paroxysm consists of 5-10 repetitive violent spasmodic coughs, which ends with an audible sound or whoop. Paroxysms may be precipitated by noise, eating or physical contact. In between the paroxysms patient may appear to be normal. The frequency of paroxysms varies widely, from several per hour to 5- 10 per day. Episodes are often worse at night. During a spasm there may be visible neck vein distension, bulging of eyes, tongue protrusion and cyanosis. Complications More common among infants than among older children or adults. Pressure effects during the violent spasms of coughing results in subconjunctival hemorrhage, hernias, pneumothorax, rib fracture and petechiae on the face and body. Pneumonia may develop especially in old age, due to secondary infection due to encapsulated bacteria. It occurs in infants, it is usually due to B. pertussis. Neurological complications, such as convulsions, encephalopathy and coma may also occur. Epidemiology Human disease, there is no animal reservoir. Source: Early cases (catarrhal stage) are the main source of infection. There is no carrier state. Age: Predominantly a disease of pre-school children below 5 years. As the maternal antibodies are not protective, infants remain the most vulnerable group, accounting for highest morbidity and mortality. Shift of median age: Pertussis has shifted from infants to older children and adolescence in countries with high vaccination coverage. This indicates that pertussis immunizations or natural infection do not provide Lifelong immunity. Mode of transmission: via inhalation of droplets (by coughing or sneezing or even talking) or rarely through direct contact Lab diagnosis Specimen collection Nasopharyngeal secretions obtained by- Nasopharyngeal aspiration (best method) Pernasal swab (by using a sterile swab on a flexible wire). Type of swabs used: For culture, alginate swabs are the best followed by dacron swabs. However, for PCR, only dacron or rayon swabs are recommended. Transport: Specimens should be processed immediately. If delay is expected, then suitable charcoal-based medium (Amies) can be used. Direct detection: B. pertussis may be directly detected from nasopharyngeal secretions by direct immunofluorescence test using fluorescein labelled polyclonal or monoclonal antibodies. Because of poor sensitivity and specificity, it is not widely used. Culture: ◦ B. pertussis is a strict aerobe, grows best at 35-37°C. ◦ lt is fastidious, requires special complex media for primary isolation, such as◦ Charcoal agar supplemented with 10% horseblood and cephalexin (Regan and Lowe medium). Currently the medium of choice. ◦ Bordet-Gengou glycerine-potato-blood agar was a traditional medium used before. ◦ Colonies are greyish white, convex with a shiny surface appear after 3-5 days, described as mercury drops or bisected pearls appearance. ◦ Culture remains positive only during first 3 weeks of infection ◦ Culture becomes negative within 5 days of start of antibiotics. Culture smear: Gram-staining of culture reveals small, ovoid coccobacilli (0.5 μm), tend to arrange in loose clumps, with clear spaces in between giving a thumb print appearance (Fig. 34.l C). ◦ Capsules may be demonstrated in fresh cultures, but are often lost on subculturing. ◦ Bipolar metachromatic granules may be demonstrated on staining with toluidine blue. Detection of serum antibodies: Enzyme immunoassays (EIA) using purified antigens of B. pertussis, such as PT, FHA and pertactin are the methods of choice. ◦ Demonstration of a rise of IgG antibodies in paired sera or detection IgA or IgM antibodies provides definite diagnosis. ◦ However, antibodies are also elevated in immunized people. Molecular methods: PCR is being increasingly used in many laboratories replacing culture, because of increased sensitivity, specificity and quicker results. The most common targeted genes are 1S481 and the PT promoter region genes. Prevention Vaccine Whole-cell Pertussis Vaccines Prepared by heating followed by chemical inactivation and purification of whole B. pertussis bacilli. OPT vaccine: In India and many other countries, whole cell (WC) pertussis vaccine is given under national immunization programme, along with diphtheria toxoid and tetanus toxoid. Three doses of DPT are given at 6, 10 and 14 weeks, followed by two boosters at 1 ½ years and 5 years. Pertussis component acts as an adjuvant and increases immunogenicity of OT and TI. Adverse effects ◦ Common: Fever, injection-site pain, erythema, swelling, and irritability. ◦ Uncommon: Borderella pertussis encephalitogenic. It is associated with neurological complications (encephalitis, prolonged convulsion) and hypotonic hyporesponsive syndrome. ◦ The estimated risk is 1:1,70,000 doses administered. Contraindications: ◦ Children more than 5-6 years age. ◦ Any associated progressive neurological conditions. ◦ Children with strong family history of epilepsy. ◦ Hypersensitivity to previous dose. Acellular Pertussis Vaccine It is composed of pertussis toxoid and 2 or more other bacterial components such as FHA, pertactin or fimbriae. Though the efficacy is same as WC vaccine, it is associated with fewer side effects as compared with the latter and can be safely given after 5-6 years. Treatment As pertussis is mainly toxin mediated, antibiotics are less useful once the infection is established. However, they play a vital role to eliminate the bacteria from nasopharynx. ◦ Macrolides are the drugs of choice (erythromycin for 7- 14 days) . ◦ Cotrimoxazole is the alternative in macrolide resistance. Isolation in a quiet environment may inhibit the stimulation of paroxysms. Cough suppressants are not much effective. Thank you………