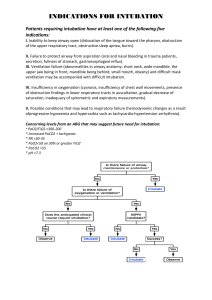
Management of Acute Airway Obstruction Consideration for Bronchoscopy and Topicalization of Airway ASA Difficult Airway Algorithm Dr. Suman Shrestha Dep of Anaesthesiology 1st year resident,PAHS OBJECTIVES • To know about causes and pathophysiology of acute airway obstruction. • To know about the approach for management of acute airway obstruction. • To know about bronchoscopy and its consideration. • To know about ASA difficult airway Algorithm. What is an Airway? • The path air follows to get into and out of the lungs. • The mouth and nose are the normal entry and exit ports. • Entering air then passes through nose, the paranasal sinuses, the back of the throat (pharynx),continues through the voice box (larynx), down the trachea, and finally out the branching tubes known as bronchi. Respiratory Anatomy What is Airway Obstruction? • Any obstacle from Mouth to Lungs • May be Partial or Complete • Limitation of air entry into Lungs • Causing Lack of O2 Inflow or CO2 Outflow • Relieving obstruction is very important for LIFE! Introduction Obstruction of the airway at its most extreme is an anaesthetic emergency requiring immediate intervention. In advanced life support algorithms, it usually refers to loss ofairway patency in the unconscious patient or blockage by a foreign body in the event of choking. Airway obstruction may present acutely or chronically depending on the site, degree of narrowing and cause. The anatomical level can broadly be categorised as supraglottic, glottic (laryngeal) or subglottic. Introduction The obstruction may be due to luminal pathology such as inflammation, tumour or haematoma or it may result from external compression and distortion. Central airway compromise due to anterior mediastinal masses can pose difficulties by nature of the obstruction being sited distal to surgical airway rescue. Management of the obstructed airway is particularly challenging and accounted for 40% of all cases reported to the 4th UK National audit. Mechanism of Airway Obstruction LEVEL OF OBSTRUCTION PATHOLOGY SIGN AND SYMPTOMS Supraglottic Oropharyngeal lesions base of tongue, tumours, epiglottitis, retropharyngeal abscess, invasive high oesophageal tumours Dysphagia,drooling,stridor,Sno ring,gurgling sounds,snorting sound,muffled voice,visible swelling Glottic Vocal cord paralysis, glottic tumours, polyps Stridor,paroxysmal nocturnal dyspnea,voice changes(hoarse cry,voices) Subglottic Tracheal stenosis, laryngomalacia, subglottic tumours Expiratory stridor Distal tracheal Lymphoma, thyroid mass, mediastinal masses Presentation of airway obstruction Presentation of airway obstruction Shortness of breath, Increased work of breathing Respiratory fatigue and distress Signs of use of accessory muscles Tracheal tug Chest wall recession Hypoxia Difficulty in swallowing Agitated Weakening of cough Why is it Important to Maintain Airway? • Sensitive organs like brain and heart can die within a few minutes without O2. • Patient becomes unconscious (hypoxia and hypercarbia) and further risk of Aspiration. • Trauma patient management of Airway comes FIRST. • Crucial few minutes Decision making in airway obstruction How time critical is airway management? Will holding measures be useful? For any lesion Where is the lesion? Is it mobile/fixed? Is it Annular/large/pedunculated/ball valve type? How does it influence airway intervention? Predictors for difficult face mask Ventilation Obesity Age 55 and above H/O snoring Lack of teeth Presence of Beard Mallampatti class III or IV Abnormal mandibular protrusion test Decreased inter dental distance Decreased thyromental distance Decreased neck movement Tumor or mass over neck HOLDING MEASURES High flow nasal oxygen: Oxygen delivery via high-flow nasal cannulae (HFNC) is revolutionising airway management. Steroid therapy: If there is inflammation or oedema associated with the obstruction, steroids may be helpful, particularly in more elective procedures where there is sufficient time for the drug to act. Nebulized epinephrine: Epinephrine is a vasoconstrictor and is frequently utilized. It appears to be effective in reducing stridor in a variety of case reports with varying obstructive aetiology. Heliox: (79% Helium plus 21% oxygen )Helium is a less dense gas than oxygen, and this improves airflow, reducing the increased work of breathing secondary to the obstruction by encouraging laminar flow within the narrowed upper airway. Continuous positive airway pressure ATLS (Advanced Trauma Life Support) Performed in an injured / trauma patient Starts as BTLS on site of injury Consists of the following components: Airway Breathing Circulation We will only discuss the AIRWAY part of the trauma protocol. AIRWAY RESCUE METHODS MANUAL MANOEUVRES: Mostly done at site, also in ambulance Head tilt finger chin lift jaw thrust Clearing mouth with hooked INSTRUMENTATION: If above unsuccessful, mostly ambulance/hospital facility Various artificial airways like Ambu Bag, Oropharyngeal and Nasopharyngeal Airway, Endotracheal Tube, Laryngeal Mask Airway SURGICAL AIRWAY: If 2nd Option unsuccessful, almost always in hospital Surgical Creation/Bypass of Airway Includes Cricothyroidotomy and Tracheostomy. MANUAL MANOEUVRES See for Any Response / Call Name Call for Help / Ambulance MANUAL MANOEUVRES (cont….) Head Tilt and Chin Lift (Opens the Oral Airway if Tongue Obstruction) MANUAL MANOEUVRES (cont….) Hear for Breathing, see chest movements If NO then start Mouth to Mouth Breaths, but Nose must be pinched to Avoid Leakage of Air MANUAL MANOEUVRES (cont….) LATERAL LYING POSITION FOR A BREATHING UNCONSCIOUS PATIENT Artificial Airways AMBU Bag and Procedure (Remember to do Head Tilt and Chin Lift to Open the Airway otherwise Bagging will be Ineffective) Oropharyngeal Airway (Guedel Airway) Artificial Airways (cont…) Artificial Airways (cont…) Nasopharyngeal Airway Artificial Airways (cont…) Laryngeal Mask Airway Artificial Airways (cont…) Laryngoscope with Various Sizes of Blades (Left Picture) Used to Intubate Endotracheal Tube with Cuff (Right Picture) Artificial Airways (cont…) Laryngoscopic View of Epiglottis and Glottis (Laryngeal Opening) and Endotracheal Tube In Place Investigations for the obstructed airway Nasendoscopy :A nasendoscopy is non invasive,quick to perform ,less airway irritation and providing a great deal of information about the appearance of the airway without laryngospasm and loss of airway. Computed tomography : Computed tomography (CT) scans provide a rapid and accurate assessment of the structures of the airway. It is readily available, quick and usually well tolerated. Magnetic resonance imaging : Magnetic resonance imaging is extremely good for delineating soft tissue structures and the physical structure of the airway. Basic management choices Airway devices and techniques used to secure the airway.These are: Awake or asleep intubation. Spontaneous Ventillation or ablation of Spontaneous Ventillation (e.g. applying positive pressure ventilation to paralysed patients). Non-invasive or invasive airway devices. Direct or indirect laryngoscopy to facilitate tracheal intubation. Awake or asleep intubation Most patients with a normal appearance can be intubated after induction of anaesthesia (asleep intubation). Anaesthesia causes airway obstruction and decrease in respiratory reserve .The ‘margin of safety’ is narrowed, full pre-oxygenation with the ‘three-minute tidal volume’ or ‘eight deep breath’ technique and transnasal oxygen insufflation is beneficial, as it prolongs safe apnoea time. Awake or asleep intubation cntd. If face mask ventilation or intubation is predicted to be difficult, and attempts are at high risk of morbidity, the airway should be secured before induction of anaesthesia (awake intubation). This maximises the ‘margin of safety’, as airway muscle tone and reflexes are maintained, and respiratory function is unaffected by anaesthetic agents. It also avoids the risk of a post-induction ‘cannot intubate, cannot ventilate’ (CICV) scenario, which has an incidence of 0.01%– 0.17%. Preserved or ablated spontaneous ventilation SV is preserved in the awake state or during anaesthesia after careful titration of intravenous or volatile agents Under acceptable intubating conditions, induction takes approximately six minutes using 7% sevoflurane in normal patients(56) but much longer in patients with AAO, as the obstruction prevents delivery of the volatile agent. induction and intubation with 8% sevoflurane without the use of muscle relaxants is associated with a higher failed intubation rate(57) and up to 10%–25% of upper airway complications, such as breath-holding and coughing. In patients with AAO, laryngospasm is more common.Several cases of failed gas induction leading to serious morbidity, including airway obstruction, laryngospasm, failed intubation necessitating surgical airway procedure, and cardiac arrest are reported. Preserved or ablated spontaneous ventilation A new strategy is to use a rapid-sequence dose of the intermediateacting rocuronium (1.2 mg/kg) and follow this with its reversal agent, sugammadex (16 mg/kg), if bailout is required. This combination gives a similar onset but faster offset time compared with suxamethonium. the use of muscle relaxants in CICV cases as they may resolve failure to ventilate caused by laryngospasm and aid mask ventilation is recommended. In symptomatic patients with large mediastinal masses or tracheobronchial lesions, maintaining SV and avoiding the use of muscle relaxants is considered the safest option. The resulting negative intrathoracic pressure helps to keep the intrathoracic airways open.( Noninvasive or invasive airway devices ACUTE EPIGLOTTITIS • Epiglottitis describes inflammation of the epiglottis and adjacent supraglottic structures. • Sudden onset of sore throat and fever followed within a matter of hours as toxic, swallowing difficulty, and labored breathing. • Drooling of saliva and hyperextended neck, assume the tripod position, sitting upright and leaning forward with the chin up and mouth open while bracing on the arms. ACUTE EPIGLOTTITIS Radiographic features of epiglottitis include: • An enlarged epiglottis protruding from the anterior wall of the hypopharynx (the "thumb sign“) • • • • Loss of the vallecular air space Thickened aryepiglottic folds Distended hypopharynx (nonspecific). Straightening or reversal of the normal cervical lordosis ACUTE EPIGLOTTITIS CONTD.. Patient able to maintain airway • supplemental humidified oxygen • In young children, avoid increasing anxiety by permitting them to sit in a position of comfort upon the parent’s lap. Children younger than 6 years of age: epiglottitis undergo endotracheal intubation Older children and adults: severe respiratory distress (eg, stridor, drooling, sitting erect, cyanosis) or >50 % obstruction of the laryngeal lumen endotracheal intubation ACUTE EPIGLOTTITIS CONTD.. • Patient not able to maintain airway • Bag-valve-mask ventilation • Oxygenation not maintained • Immediately attempt to place an oral endotracheal • Emergency surgical airway varies by age • < 12 years of age, perform needle cricothyroidotomy • In older patients, perform surgical cricothyroidotomy Antimicrobial therapy Racemic epinephrine Bronchodilators and parenteral glucocorticoids CROUP • A respiratory illness characterized by inspiratory stridor, barking cough, and hoarseness. • Result from inflammation in the larynx and subglottic airway • Viral croup (classic croup) refers to the typical croup syndrome that occurs commonly in children 6 months to 3 years of age. • The anatomic hallmark of croup is narrowing of the subglottic airway. CROUP CONTD.. • The cricoid cartilage of the subglottis is a complete cartilaginous ring. • The cricoid cannot expand, causing significant airway narrowing whenever the subglottic mucosa becomes inflamed. • Dynamic obstruction of the extrathoracic trachea below the cartilaginous ring may occur when the child struggles, cries, or becomes agitated. CROUP CONTD.. Imaging • Radiographic confirmation is not required • Indication: • If the diagnosis is in question, • Atypical course • An inhaled or swallowed foreign body is suspected • Croup is recurrent, • There is a failure to respond as expected to therapeutic interventions. CROUP CONTD.. • Findings • In children with croup, a posterior-anterior chest radiograph demonstrates subglottic narrowing, commonly called the "steeple sign“. • The lateral view may demonstrate over distention of the hypopharynx during inspiration and subglottic haziness. CROUP CONTD.. Initial treatment of moderate to severe croup includes administration of dexamethasone and nebulized epinephrine. Also receive supportive care including humidified air or oxygen, antipyretics, and encouragement of fluid intake Dexamethasone (0.6 mg/kg, maximum of 16 mg) Some Other Causes Bacterial Tracheitis Retropharyngeal Abscess Peritonsillar Abscess Laryngeal Papillomatosis Chocking • • • • Airways obstruction by a foreign body. Recognition of chocking is important. Look for signs of chocking. Assess severity. Chocking cntd.. Small children often choke on food or small objects and usually clear the obstruction spontaneously with coughing and choking. Only about 2% of FB aspiration cases need an intervention. Complete airway obstruction (ie, is unable to speak or cough), dislodgement using back blows and chest compressions in infants, and the Heimlich maneuver in older children, should be attempted. Recognition of FBAO Heimlich Maneuver- place your fist on the patient’s midline between the waist and rib cage. Grasp the fist and rapidly deliver four upwards thrusts. For a complete airway obstruction In an infant, alternate back blows & chest thrusts Chest thrust TRAUMA • Blunt or penetrating injury to various anatomic structures may result in upper airway obstruction. • Traumatic injury to the face may cause soft tissue swelling or hemorrhage, leading to airway compromise. BURN INJURIES • Facial burns or burnt facial hairs should alert the possibility of thermal injuries to the upper airway. • Despite no initial airway compromise, edema can rapidly progress. ANAPHYLAXIS • May be severe and life-threatening when edema involves the retropharynx and/or larynx. • Usually sudden onset of symptoms and there may be associated signs such as urticaria and facial swelling. • Emergent treatment can be life-saving. ANGIOEDEMA • Laryngeal edema occurs in approximately ½ of all patients with inherited angioedema at their lifetime. • Tooth extraction and oral surgery are common triggers for laryngeal attacks. LARYNGOSPASM • An acute manifestation of vocal cord dysfunction that is usually precipitated by irritation of the vocal cords. • The symptoms of vocal cord dysfunction (VCD) are usually chronic. • The acute onset or worsening of stridor from VCD can be alarming and this is particularly true when the VCD is due to a lesion in the brainstem. • Hypocalcemic tetany is a rare cause of laryngospasm. DECREASED OROPHARYNGEAL MUSCLE TONE • The tongue can fall back into the pharynx and obstruct the airway in children with decreased oropharyngeal muscle tone as can occur with depressed levels of consciousness or neuromuscular disease (eg, cerebral palsy, congenital myopathies, or cranial neuropathy). • Simply repositioning the airway may relieve the obstruction. • Persistent obstruction may be treated with a nasopharyngeal airway in the conscious or semiconscious patient. AIRWAY SECRETIONS OR BLEEDING • Oropharyngeal or nasopharyngeal bleeding and secretions can cause significant upper airway obstruction in children. • Superficial suctioning of the naso- and oropharynx and, as needed, control of bleeding resolves the obstruction. Congenital causes of upper airway obstruction • • • • • • • Laryngomalacia Subglottic stenosis Choanal atresia Laryngeal web Laryngeal cyst Vocal cord paralysis Vascular ring developmental anomaly of aorta Bronchoscopy A technique of visualizing the inside of the airways for diagnostic and therapeutic purposes by using a bronchoscope. 2 types of bronchoscopy : Rigid Flexible fibre optic Rigid bronchoscope Rigid bronchoscopy Indications: A) Diagnostic To find the cause of wheezing, haemoptysis, or unexplained cough for more than 4 weeks. When X-ray chest shows: -Atelectasis of a segment, lobe or entire lung -Localised opacity of a segment or lobe of lung -Obstructive emphysema –to exclude foreign body. -Hilar or mediastinal shadows. Vocal cord palsy Collection of bronchial secretions -for culture and sensitivity tests, acid fast bacilli, fungus, malignant cells. 2)Therapeutic 1. Removal of foreign bodies. 2.Removal of retained secretions or mucus plug. -in cases of head injuries, chest trauma, thoracic or abdominal surgery or comatosed patients. Contraindications: • Absolute – inability to adequately oxygenate the patient during procedure • Coagulopathy or bleeding diathesis that cannot be corrected. • Rigid bronchoscopy - Aneurysm, marked kyphosis. • Recent MI or unstable angina. • Respiratory failure requiring mechanical ventilation. Technique 1.Anaesthesia General anaesthesia with no endotracheal tube or with only a small bore catheter. 2.Position (Barking-dog position) Patient lies supine Head is elevated by 10-15 cm by placing a pillow under the occiput. Neck is flexed on thorax and head is extended on atlanto-occipital joint. Methods to introduce bronchoscope: • Direct method –directly through the glottis • Through laryngoscope -glottis exposed with a spatular type laryngoscope -the bronchoscope is introduced through the laryngoscope -laryngoscope withdrawn. -Infants, young children, adults-short neck & thick tongue. Procedure • A piece of gauze is placed on the upper teeth to avoid injury. • Proper-sized bronchoscope is lubricated with a swab of autoclaved liquid paraffin or jelly. Held by the shaft in the right hand in a pen-like fashion. Retract the upper lid and guide the bronchoscope with left hand. • Look through the scope, identify the tip of epiglottis and pass the scope behind it. The epiglottis lifted forward to expose the glottis. Rotate the scope 90˚ clockwise so that the tip is in the axis of glottis. Once the trachea is entered, scope is rotated back to the original position. • Gradually advanced the scope and the tracheobronchial tree examined. Axis of bronchoscope should correspond with axes of trachea and bronchi. • Direct vision, right angled and retrograde telescope can be used for magnification and detailed examination. • Biopsy of the lesion of suspicious area can be taken. • Secretions can be collected for exfoliative cytology, or bacteriologic examination. Post-operative care Keep patient in humid atmosphere Watch for respiratory distress -due to laryngeal spasm or subglottic oedema if the procedure had been unduly prolonged or repeated introduction of bronchoscope. -inspiratory stridor and suprasternal retraction will indicate need for tracheostomy. Complications Injury to the teeth Hemorrhage from the biopsy site Hypoxia and cardiac arrest Laryngeal oedema Precautions during bronchoscopy Select proper size Do not force through closed glottis Repeated removal and introduction should be avoided Should not be prolonged >20 min. in infants and children Flexible fibre optic bronchoscopy Provides magnification and better illumination. Smaller size –permits examination of subsegmental bronchi. Easy to use in patients with neck or jaw abnormalities. Can be performed under topical anaesthesia & useful for bedside examination of critically ill patients suctions/biopsy channel provided helps to remove secretions, inspissated mucus plug and small foreign bodies. Can be easily passed through endotracheal tube or in tracheostomy opening. Flexible fibre optic bronchoscopy Limited utility in children –problem of ventilations ASA DIFFICULT AIRWAY ALGORITHM Basics Evaluation of the Airway Informing the patient/Bystander Availability of a Trained Assistant Availability of equipment Optimise the position / Preoxygenation Assess the basic management problems • Difficult supraglottic airway placement •Difficulty with patient cooperation or consent • Difficult mask ventilation •Difficult intubation • Difficult laryngoscopy •Difficult surgical airway access Consider the basic management choices • Awake Intubtn vs. Intubtn after induction of GA • Non-Inv. vs. Inv. Techniques initial approach • Video Assisted Laryngoscope as an initial approach to intubation • Preservation vs. ablation of spont. ventilation Throughout the process of difficult airway Actively deliver supplemental OXYGEN Develop primary and alternative strategies AWAKE INTUBATION INTUBATION AFTER INDUCTION OF GA AWAKE INTUBATION Airway approached by NON Invasive Airway Access Succeed Invasive Airway Access Fail Cancel case Invasive airway access Consider feasibility of other options INTUBATION AFTER INDUCTION OF GA INITIAL INTUBATION UNSUCCESSFUL FROM THIS POINT ONWARDS CONSIDER INITIAL INTUBATION ATTEMPTS SUCCESSFUL . 1.CALL FOR HELP 2.Return to spont ventilation 3.Awaken the patient INITIAL INTUBATION ATTEMPTS UNSUCCESSFUL FACE MASK VENTILATION ADEQUATE FACE MASK VENTILATION NOT ADEQUATE FACE MASK VENTILATION ADEQUATE NONEMERGENCY PATHWAY Ventilation adequate, intubation unsuccessful Alternative approaches to intubation SUCCESSFUL INTUBATION INVASIVE AIRWAY ACCESS FAIL AFTER MULTIPLE ATTEMPTS CONSIDER FEASIBILTY OF OTHER OPTIONS AWAKEN THE PATIENT FACE MASK VENTILATION NOT ADEQUATE CONSIDER/ATTEMPT SGA SGA NOT ADEQUATE OR NOT FEASIBLE SGA ADEQUATE EMERGENCY PATHWAY Ventilation not adequate, intubation unsuccessful Call for help Emergency NON invasive airway ventilation Successful ventilation Invasive airway access Consider feasibility of other options FAIL Emergency invasive airway access Awaken the patient From: Practice Guidelines for Management of the Difficult Airway:An Updated Report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway Anesthesiology. 2013;118(2):251-270. doi:10.1097/ALN.0b013e31827773b2 Follow-up Care Extuabation strategy Postextubation care and counselling Documentation of a difficult airway Registration with notification service Take Home Message Patients with airway obstruction are high risk; they should be managed by senior anaesthetic and surgical staffs that have good technical and nontechnical skills. There is no universal ‘best approach’ with experts often providing differing opinions on optimal management. The best outcomes are achieved by the right personnel using equipment with which they are familiar and skilled, at the right time, and in the right location. Holding measures are often useful, allowing time to assemble team members, gain further information, and plan airway intervention. Oxygen delivery utilising high-flow nasal cannula is revolutionising airway management and should be available. Flexible bronchoscopy is a standard of care for specific indication . However ,alternative techniques need to be considered. References Wong P, Wong J, Mok MUS. Anaesthetic management of acute airway obstruction. Singapore Med J. 2016;57(3):110. Lynch J, Crawley SM. Management of airway obstruction. BJA Educ. 2018;18(2):46. Bryant H, Batuwitage B. Management of the Obstructed Airway. 2016 Diseases of Ear,Nose and Throat And Head and Neck surgery , PL Dhingra, Shruti Dhingra. 6th Edition. MODERATOR DR. BISHAL GURUNG LECTURER DEP. OF ANAESTHESIOLOGY , PAHS Thank you !