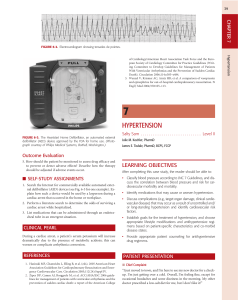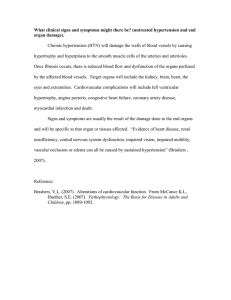
39 CHAPTER 7 FIGURE 6-2. Electrocardiogram showing torsades de pointes. 7 HYPERTENSION FIGURE 6-3. The Heartstart Home Defibrillator, an automated external defibrillator (AED) device approved by the FDA for home use. (Photograph courtesy of Philips Medical Systems, Bothell, Washington.) Salty Sam . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Level II Julie M. Koehler, PharmD James E. Tisdale, PharmD, BCPS, FCCP Outcome Evaluation 5. How should the patient be monitored to assess drug efficacy and to prevent or detect adverse effects? Describe how the therapy should be adjusted if adverse events occur. LEARNING OBJECTIVES After completing this case study, the reader should be able to: ■ SELF-STUDY ASSIGNMENTS • 1. Search the Internet for commercially available automated external defibrillator (AED) devices (see Fig. 6-3 for one example). Explain how such a device would be used by a layperson during a cardiac arrest that occurred in the home or workplace. Classify blood pressure according to JNC 7 Guidelines, and discuss the correlation between blood pressure and risk for cardiovascular morbidity and mortality. • Identify medications that may cause or worsen hypertension. • Discuss complications (e.g., target organ damage, clinical cardiovascular disease) that may occur as a result of uncontrolled and/ or long-standing hypertension and identify cardiovascular risk factors. 2. Perform a literature search to determine the odds of surviving a cardiac arrest while hospitalized. 3. List medications that can be administered through an endotracheal tube in an emergent situation. CLINICAL PEARL During a cardiac arrest, a patient’s serum potassium will increase dramatically due to the presence of metabolic acidosis; this can worsen or complicate arrhythmia conversion. REFERENCES 1. Hazinski MF, Chameides L, Elling B, et al. (eds). 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2005;112(24):Suppl IV. 2. Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College • Establish goals for the treatment of hypertension, and choose appropriate lifestyle modifications and antihypertensive regimens based on patient-specific characteristics and co-morbid disease states. • Provide appropriate patient counseling for antihypertensive drug regimens. PATIENT PRESENTATION 쐽 Chief Complaint “I just moved to town, and I’m here to see my new doctor for a checkup. I’m just getting over a cold. Overall, I’m feeling fine, except for occasional headaches and some dizziness in the morning. My other doctor prescribed a low-salt diet for me, but I don’t like it!” Hypertension of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). Circulation 2006;114:e385–e484. 3. Wenzel V, Krismer AC, Arntz HR, et al. A comparison of vasopressin and epinephrine for out-of-hospital cardiopulmonary resuscitation. N Engl J Med 2004;350:105–113. 40 SECTION 2 쐽 HPI HEENT Sam Street is a 62-year-old African-American male who presents to his new family medicine physician for evaluation and follow-up of his medical problems. He generally has no complaints, except for occasional mild headaches and some dizziness after he takes his morning medications. He states that he is dissatisfied with being placed on a low sodium diet by his former primary care physician. He reports a “usual” chronic cough and shortness of breath, particularly when walking moderate distances (states, “I’m just out of shape”). TMs clear; mild sinus drainage; AV nicking noted; no hemorrhages, exudates, or papilledema Cardiovascular Disorders 쐽 PMH Hypertension × 15 years Type 1 diabetes mellitus Chronic obstructive pulmonary disease, Stage 2 (Moderate) Benign prostatic hyperplasia Chronic kidney disease 쐽 FH Father died of acute MI at age 71. Mother died of lung cancer at age 64. Mother had both HTN and DM. 쐽 SH Former smoker (quit 3 years ago; smoked 1 ppd × 28 years); reports moderate amount of alcohol intake. He admits he has been nonadherent to his low sodium diet (states, “I eat whatever I want.”) He does not exercise regularly and is limited somewhat functionally by his COPD. He is retired and lives alone. 쐽 Meds Triamterene/hydrochlorothiazide 37.5 mg/25 mg po Q AM Insulin 70/30, 24 units Q AM, 12 units Q PM Doxazosin 2 mg po Q AM Albuterol INH 2 puffs Q 4–6 h PRN shortness of breath Tiotropium DPI 18 mcg 1 capsule INH daily Salmeterol DPI 1 INH BID Entex PSE 1 capsule Q 12 h PRN cough and cold symptoms Acetaminophen 325 mg po Q 6 h PRN headache 쐽 All PCN—Rash 쐽 ROS Patient states that overall he is doing well and just getting over a cold. He has noticed no major weight changes over the past few years. He complains of occasional headaches, which are usually relieved by acetaminophen, and he denies blurred vision and chest pain. He states that his shortness of breath is “usual” for him, and that his albuterol helps. He denies experiencing any hemoptysis or epistaxis; he also denies nausea, vomiting, abdominal pain, cramping, diarrhea, constipation, or blood in stool. He denies urinary frequency, but states that he used to have difficulty urinating until his physician started him on doxazosin a few months ago. Neck Supple without masses or bruits, no thyroid enlargement or lymphadenopathy Lungs Lung fields CTA bilaterally. Few basilar crackles, mild expiratory wheezing Heart RRR; normal S1 and S2. No S3 or S4 Abd Soft, NTND; no masses, bruits, or organomegaly. Normal BS. Genit/Rect Enlarged prostate; benign Ext No CCE Neuro No gross motor-sensory deficits present. CN II–XII intact. A & O × 3. 쐽 Labs Na 142 mEq/L K 4.8 mEq/L Cl 101 mEq/L CO2 27 mEq/L BUN 22 mg/dL SCr 1.6 mg/dL Glucose 136 mg/dL Ca 9.7 mg/dL Mg 2.3 mEq/L HbA1C 6.2% Alb 3.5 g/dL Hgb 13 g/dL Hct 40% WBC 9.0 × 103/mm3 Plts 189 × 103/mm3 Fasting Lipid Panel Total Chol 169 mg/dL LDL 99 mg/dL HDL 40 mg/dL TG 151 mg/dL Spirometry (6 months ago) FVC 2.38 L (54% pred) FEV1 1.21 L (38% pred) FEV1/FVC 51% 쐽 UA Yellow, clear, SG 1.007, pH 5.5, (+) protein, (–) glucose, (–) ketones, (–) bilirubin, (–) blood, (–) nitrite, RBC 0/hpf, WBC 1–2/ hpf, neg bacteria, 1–5 epithelial cells 쐽 ECG Normal sinus rhythm 쐽 ECHO (6 months ago) Mild LVH, estimated EF 45% 쐽 Assessment 1. Hypertension, uncontrolled 2. Type 1 diabetes mellitus, controlled on current insulin regimen 3. Moderate COPD, stable on current regimen 4. BPH, symptoms improved on doxazosin 쐽 Physical Examination Gen WDWN, African-American male; moderately overweight; in no acute distress VS BP 168/92 mm Hg (sitting; repeat 170/90), HR 76 bpm (regular), RR 16 per min, T 37°C; Wt 95 kg, Ht 6'2'' QUESTIONS Problem Identification 1.a. Create a list of this patient’s drug-related problems, including any medications which may be contributing to the patient’s uncontrolled hypertension. 41 CHAPTER 7 1.b. How would you classify this patient’s HTN (e.g., Prehypertension, Stage 1, or Stage 2), according to JNC 7 Guidelines? 1.c. What are the patient’s known cardiovascular risk factors, and what is the patient’s Framingham risk score? 1.d. What evidence of target organ damage or clinical cardiovascular disease does this patient have? Desired Outcome Hypertension 2. List the goals of treatment for this patient (including the patient’s goal blood pressure, according to JNC 7 Guidelines). Therapeutic Alternatives 3.a. What lifestyle modifications should be encouraged for this patient to achieve and maintain adequate blood pressure reduction? 3.b. What reasonable pharmacotherapeutic options are available for controlling this patient’s blood pressure, and what comorbidities and individual patient considerations should be taken into account when selecting pharmacologic therapy for his HTN? How might Mr. Street’s HTN medications potentially affect his other medical problems? Optimal Plan FIGURE 7-1. The LifeSource UA-767 Plus—One-Step Plus Memory digital home blood pressure monitor. (Photo courtesy of A&D Medical, Milpitas, California.) • Renovascular disease (bilateral or unilateral renal artery stenosis) • Heart failure due to left ventricular systolic dysfunction 3. Describe how you would explain to a patient how to use a digital home blood pressure monitor such as the one shown in Fig. 7-1. 4.a. Outline specific lifestyle modifications for this patient. 4.b. Outline a specific and appropriate pharmacotherapeutic regimen for this patient’s uncontrolled hypertension, including drug(s), dose(s), dosage form(s), and schedule(s). Outcome Evaluation 5. Based on your recommendations, what parameters should be monitored after initiating this regimen and throughout the treatment course? At what time intervals should these parameters be monitored? Patient Education 6. Based on your recommendations, provide appropriate education to this patient. ■ SELF-STUDY ASSIGNMENTS 1. Review the American Heart Association Scientific Statement on the treatment of hypertension in the prevention of and management of ischemic heart disease, and highlight the key differences in recommendations for managing a hypertensive patient with known CHD. 2. Outline the changes, if any, that you would make to the pharmacotherapeutic regimen for this patient if he had a history of each of the following co-morbidities or characteristics: • Severe-persistent asthma • Major depression • Gout • Cerebrovascular disease • Peripheral arterial disease • Isolated systolic hypertension • Migraine headache disorder • Liver disease CLINICAL PEARL The risk of hemorrhagic stroke may be increased by the use of aspirin therapy in patients with uncontrolled hypertension. REFERENCES 1. Salerno SM, Jackson JL, Berbano EP. Effect of oral pseudoephedrine on blood pressure and heart rate: a meta-analysis. Arch Intern Med 2005;165:1686–1694. 2. Chobanian AV, Bakris GL, Black HR, et al. and the National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–1252. 3. Rosendorff C, Black HR, Cannon CP, et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation 2007;115:2761–2788. 4. Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001;344:3–10. 5. Douglas JG, Bakris GL, Epstein M, et al. Management of high blood pressure in African Americans: Consensus Statement of the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. Arch Intern Med 2003;163:525–541. 6. ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002;288:2981–2997. 7. UKPDS 39. Efficacy of atenolol and captopril in reducing risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 39. UK Prospective Diabetes Study Group. BMJ 1998;317:713– 720.