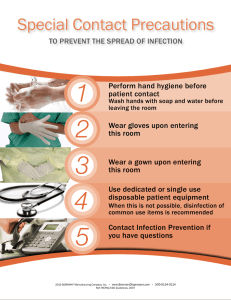
PRINCIPLES OF MEDICAL LABORATORY SCIENCE LAB 2 PHLEBOTOMY: DEFINITION PHLEBOTOMY or venesection came from two Greek words, phlebos which means vein; and temnein which means to cut. It is the act of opening a vein by using incision or puncture methods to draw blood for analysis or as part of therapeutic or diagnostic measures under the physician’s request PHLEBOTOMY: EVOLUTION (A BRIEF HISTORY) The practice of Phlebotomy can be tracked back to the time of the Stone Age when men used crude tools to cut vessels and drain blood from the body. The ancient Egyptians also practiced this as a form of “Bloodletting” as early as 1400 B.C. However, Phlebotomy became widely accepted during the time of Hippocrates (460-377 B.C.) when health was believed to be dependent on the balance of humors: Earth – Blood & Brain Air – Phlegm & Lungs Fire – Black Bile & Spleen Water – Yellow Bile & Gall Bladder To keep balance, excess humor is removed by bloodletting PHLEBOTOMY: INTRODUCTION Laboratory testing of blood specimen is vital to the correct diagnosis, treatment, and monitoring of a patient’s condition. Laboratory results constitute 70% of the objective information used by health-care providers to manage patient care and resolve patient health problems. The quality of a test result is only as good as the quality of the specimen analyzed. Therefore, reports from a suboptimal specimen can result in treatment that can be potentially harmful to the patient by overmedicating or under-medicating the patient with death being the worse patient outcome Although the primary concern or personnel collecting blood specimens is understandably to obtain the specimen, failure to adhere to the collection procedure can compromise the integrity of a successful collected specimen. Approximately 56% of laboratory error occurs during the pre-analytical phase (process that occurs before testing of the sample) of laboratory testing Influencing factors are the responsibilities of the blood collector and include: Monitoring of specimen ordering Correct patient identification Patient communication and safety Patient preparation Timing of collections Phlebotomy equipment Collection techniques Specimen labeling Specimen transportation to the laboratory Specimen processing PHLEBOTOMIST: ROLE IN HEALTHCARE The Phlebotomist’s primary role is to collect blood for accurate and reliable test results as quickly as possible and with the least discomfort to the patient. The job description can vary greatly from one health care environment to another A Phlebotomist is usually cross-trained in venipuncture, capillary collection, patient care, laboratory receptionist duties, sample processing, and computer work Phlebotomists have become key players on the health care team. They represent the laboratory and the health care center, they are in direct contact with the patient, and they perform tasks that are critical to the patient’s diagnosis and care PHLEBOTOMIST: PROFESSIONAL ATTITUDE Central to the job of drawing blood is the patient, who is often apprehensive about the procedure we perform. It is important not only to obtain a good sample, but to do so with minimal trauma to the patient. Bear in mind that the patient must be treated like anyone would like to be treated. Everyone must follow a professional code of conduct in the treatment of patients. The Phlebotomist’s own professional attitude toward the job and duties determines how the patient is treated. If the Phlebotomist attempts to draw a patient and does not feel confident about obtaining the sample, a “miss” of the patient will most likely result. Even when you try to hide it, a negative attitude will resurrect its ugly head and destroy rapport with patients, coworkers, and supervisors. It is not the events of the day that shape the Phlebotomist, it is how the Phlebotomist deals with those events. PHLEBOTOMIST: PROFESSIONAL GROOMING Just as the professional attitude of the Phlebotomist can determine how well a Phlebotomist is perceived by the patient, so can the grooming of the Phlebotomist affect this perception. The average patient a Phlebotomist will be working with is an older individual for whom often only conservative grooming and dress is acceptable. Most health care organizations restrict what the Phlebotomist is permitted to wear The following are the common dress code for most hospital-employed Phlebotomists: No visible tattoos No body piercing other than a minimum of two in the ears (one for each ear) No fingernails longer than one-fourth inch No blue jeans or casual attire No open-toed shoes No t-shirt or sweatshirts Often the Phlebotomist will be most comfortable and acceptable wearing scrub outfit. In some health care organizations, the scrub outfit is furnished WHAT IS PHLEBOTOMY? Does not generally talk about venesection only Includes arteries and capillaries VENESECTION – Ancient Times PHLEBOTOMY – Now Comes from the Greek words Phlebos which means “veins” and Temnein which means “to cut” The act of opening the vein by using incision or puncture for therapeutic or diagnostic measures WHY IS IT IMPORTANT? Correct and accurate diagnosis and treatment Monitoring of condition Follow proper procedure in blood collection and other medications Every step has a reason Good test result = Good quality specimen Failure to adhere to the collection procedure = Compromise integrity of a successfully collected specimen Approximately 56% of the laboratory errors occur in the preanalytical phase or process that occur before testing the sample of laboratory testing Most critical phase in the laboratory Includes phlebotomy or blood collection RESPONSIBILITIES OF A PHLEBOTOMIST Monitoring of specimen Correct patient identification Very critical; Has patient interaction Patient communication and Safety Communications is a skill Patient preparation Give the patient proper instructions before blood collection Timing of collections Phlebotomy equipment Collection techniques Specimen labeling As important as correct patient identification Specimen transportation Specimen processing THE PHLEBOTOMIST ROLE IN HEALTHCARE PRIMARY ROLE: To collect blood sample Represents the laboratory In direct contact with the patient Perform tasks critical to patient’s diagnosis and care PROFESSIONAL ATTITUDE Self-Confidence – Ability to trust your own personal judgement Know what you are doing Integrity – Quality of being honest and having strong moral principles Compassion – Being sensitive to the needs of a person and offering reassurance in a caring and humane way Show TLC (Tender Loving Care) Self-Motivation – Direct reflection of a person’s attitude towards life There is the initiative to do your work Dependability – If you are confident = Dependable Ethical Behavior – Making the right personal choices to help maintain high respect for self and for profession Code of Ethics PROFESSIONAL GROOMING DONT’S Visible tattoos Only tattoos that can be hidden Body piercing Only in the ears Fingernails longer than one-fourth inch For safety from hazardous waste; Use gloves always Jeans or casual attire Open-toed shoes T-shirts or sweatshirts – Casual attire is okay as long as it is proper Never forget your lab gowns & scrub suits Always wash your lab gowns regularly Never re-use gloves and PPE (masks, hairnets, etc.) PATIENT-CLIENT INTERACTION Important because we are in direct contact with the patient Recognize Diversity Every patient has different beliefs and opinions and we should respect that Professionalism Communication Patient’s Right Patient has the right to refuse and to request Confidentiality ANATOMY OF A PHLEBOTOMIST Sharp mind Learn how to troubleshoot Be cheerful Have a calm tone of voice Be compassionate and kind Have high level of patience Communication skills Steady hands Strong feet LABORATORY BIOSAFETY Regard all samples as potentially infectious (all types of fluids) BIOSAFETY AND BIOSECURITY BIOSAFETY Measures employed when handling biohazardous materials to avoid infecting oneself, others, or the environment “Protecting people from bad bugs” The containment principles, technologies, and practices that are implemented to prevent unintentional exposure to pathogens and toxins or their accidental release (WHO, 2006) Contain the pathogens so as not to infect others BIOSECURITY Measures employed to protect biohazardous materials, or critical relevant information, against theft or diversion by those who tend to pursue intentional misuse “Protecting bad bugs from bad people” The protection, control, and accountability for valuable biological materials within laboratories in order to prevent unauthorized access, loss, theft, misuse, diversion, or intentional release (WHO, 2006) Protect samples from the wrong people (may be used as a murder weapon) DIFFERENT ORGANIZATIONS IN THE FIELD OF BIOSAFETY Common goal: SAFETY 1. American Biological Safety Association (ABSA) Promotes biosafety as a scientific discipline Research and theories 2. Asia-Pacific Biosafety Association (A-PBA) Members are required to contribute to the development of the best biosafety practices Similar to PAMET (has contributions) Funds will be used for everyone Benchmark – recording 3. European Biological Safety Association (EBSA) Provide a forum for discussions and debates on issues of concern Convention Other people get to address their concerns and create a solution for it 4. Philippine Biosafety and Biosecurity Association (PhBBA) Assists the Department of Agriculture (DA) and Department of Health (DOH) to create a national policy and implement plan for biosafety and biosecurity No concrete policy for biosafety and biosecurity 5. Biological Risk Association Philippines (BRAP) Serve the emergent concerns of biological risk management in various professional fields CLASSIFICATION OF MICROORGANISMS ACCORDING TO RISK GROUPS Based on principal characteristics and relative hazards posed by infectious toxins or agents CLASSIFICATION OF LABORATORY BIOSAFETY ACCORDING TO LEVELS Based on composite of the design features, construction, containment facilities, equipment, practices, and operational procedures required for working with agents from various risk groups PRINCIPAL CHARACTERISTICS – Biochemical Results FUME HOOD Enclosure/ventilation which is connected to the exhaust fan So that the aerosol (fumes) like strong acids will be sucked and released into the environment BIOSAFETY CABINET Operator – Has filter (HEPA filter or High Efficiency Particulate Air Filter) Filters air so the smallest pathogens or particles will be trapped and filtered Sample is protected in a way that it is not contaminated HEPA FILTERS To prevent discharge of aerosol (source of infection) At least 2 filters – Supply & Exhaust AEROSOL Created by any activity that imparts energy into a liquid or semiliquid material E.g. When shaking, pouring, centrifugation, pipetting, streaking (in centrifugation – should be closed as well as the tube) Classification Biosafety Level Application Low to moderate risk Class-I 1,2,3 biologic agents Low to moderate risk Class-II 1,2,3 biologic agents Class-III 4 High risk biologic agents Biosafety Cabinets Ebola – Biosafety Level 4 Class 3 – Also known as glove boxes Risk Group Biosafety Level Laboratory Type 1 1 Microorganism: Unlikely Suitable for work involving Basic teaching, Research to cause disease viable microorganisms Risk: Low 2 2 Microorganism: Unlikely Deal with indigenous Primary health services; to be a significant risk moderate-risk, Diagnostic services, to; treatment and appropriate for samples Research preventive measure when there is uncertain are available Risk: Moderate presence of infectious agent 3 Microorganism: Known 3 to cause serious Works with indigenous or disease; Treatment and Special diagnostic exotic agents with preventive measure services, Research potential for respiratory are available transmission Risk: High (individuals), Moderate (Community) 4 Microorganism: Known 4 to produce lifeWork with dangerous and threatening, readily exotic agents. Generally a transmissible. Dangerous pathogen unit separate building or Treatment and completely isolated zone preventive measures with specialized ventilation are not usually available Risk: High 1: Unlikely to cause disease = Non-pathogenic 2: E.g. E.Coli; Staphylococcus aureus Control microbes/microorganisms Run it like a sample (to check presence) 4: E.g. Tuberculosis; St. Louis Encephalitis Virus (through respiratory transmission); Coxiella Ante-room – Room created before entering the actual site of infection Change clothes (No outside clothes allowed) SPECIMEN PROCESSING AND HANDLING All specimens should be transported to the laboratory in sealed containers/plastic bags Some has a biohazard symbol Place in transport container/vessel Contamination-leakage or improper collection technique Container must be screw-capped (slowly open it) Be careful when removing lids or caps – cover with gauze or disposable tissue to prevent splatters or spray HOW TO CLEAN SPILLED BLOOD 1. Get something that is absorbent (gauze, paper towel) 2. Let it absorb 3. Clean remnants using antiseptic (Best antiseptic: Bleach – 10% sodium hypochlorate solution or NaClO) HOW TO PREPARE 10% SODIUM HYPOCHLORATE 9 parts water and 1 part bleach Expired, spilt, and contaminated pharmaceutical products, drugs, and vaccines RADIOACTIVE WASTE Wastes that haven’t been in contact with communicable or infectious agents Hazardous chemicals or radioactive substances Recyclable/Biodegradable/Non-recyclable/Non-biodegradable PRACTICES OBSERVED IN A COLOR-CODING SYSTEM FOR HEALTH CARE WASTES Highly infectious waste must be disinfected at source Anatomical waste should be disposed through safe burial or cremation Pathological waste must be refrigerated if not collected or treated within 24 hours Chemical and pharmaceutical waste shall be segregated and collected separately Radioactive waste has to be decayed to background radiation levels All waste bins must be properly covered to prevent cross contamination Aerosol containers can be collected with the general waste Centrifugation-capped or covered trunnions to prevent aerosols. Tops should be close when in operation and never stopped by hand CENTRIFUGAL FIELDS – 10-12 kilograms Has a calculated speed Paraffin – Wax paper used to cover the mouth of the test tube NEVER PIPETTE BY MOUTH Check correct details of label and request name, age, sext, test, requesting physician, patient number, official receipt number Should be complete name WHAT’S IN THE TUBE Name Age Sex Date and time of collection Initials of physician/phlebotomist HEALTH CARE WASTE MANAGEMENT HEALTH CARE WASTE Solid or liquid wastes generated by any of the following: Diagnosis, treatment, and immunization of humans Research Production and testing of biological products TYPES OF HEALTH CARE WASTE INFECTIOUS WASTE Wastes suspected to contain pathogens or toxins in sufficient concentration that may cause disease to a susceptible host PATHOLOGICAL & ANATOMICAL WASTE Tissue section or organs from biopsy, autopsy, or surgery SHARPS Items that can cause cuts, pricks, or puncture wounds MOST DANGEROUS HEALTH CARE WASTE CHEMICAL WASTE Discarded chemicals during disintegration and sterilization May contain high content of heavy metals and derivatives PHARMACEUTICAL WASTE BENEFITS OF PROPER AND STRICT COMPLIANCE ON HEALTH CARE WASTE MANAGEMENT 1. Protection of patients, health workers, and the general population from adverse effects on health care waste 2. Contribution to the collaborative efforts of the world to protect the environment 3. Increased compliance of health care institutions to laws, regulations, and guidelines on health care waste 4. Prevention of long-term liabilities and loss of reputation INTERNATIONAL AGREEMENTS ON HEALTH CARE WASTE MANAGEMENT Montreal Protocol on Substances that Deplete the Ozone Layer (1987) Basel Convention on the Control of the Transboundary Movements of Hazardous Wastes and their Disposal (1989) UN Framework Convention on Climate Change (1992) ASEAN Framework Agreement on the Facilitation of Goods in Transmit (1998) Stockholm Convention on Persistent Organic Pollutants (2001) NATIONAL LAWS AND POLICIES ON HEALTH CARE WASTE MANAGEMENT DOH “Manual on Health Care Waste Management” in 2011 DOH AO No. 2008-0021 “Gradual Phaseout of Mercury in all Philippines Health Care Facilities and Institutions” R.A. 9275 “The Philippines Clean Water Act of 2004” R.A. 8749 “The Philippine Clean Air Act of 1999” TREATMENT OF HEALTH CARE WASTE PYROLYSIS – Thermal decomposition AUTOCLAVE MICROWAVE CHEMICAL DISINFECTION BIOLOGICAL PROCESS – Used an enzyme to decontaminate ENCAPSULATION – Filling of containers then sealing INERTIZATION – Involves the mixing of waste with cement and other substances; for pharmaceutical waste LANDFILL – Engineered site designed to keep waste isolated from the environment; must secure permit from DENR HAND HYGIENE One of the methods of breaking the chain of infection is proper hand hygiene The hand hygiene measures include hand washing and use of alcoholbased antiseptic hand cleaners Hand washing could be routine which uses plain soap and water. Meanwhile hand antiseptics uses antimicrobial soap to remove transient microorganisms, which is also the kind of soap used when washing the hands with the 2-minute surgical hand scrub prior to performing surgical procedures HAND WASHING WE NEED TO FOLLOW PROPER PROCEDURES – If not = Deemed useless and hands are still contaminated PRINCIPLE The proper handwashing technique cleans the hands and wrists. This procedure will also reduce the number of organisms present in the said areas of the body. It will decrease the chances of transferring organisms from a source to a susceptible host MATERIALS Sink with running water, preferably with the following: Foot operated controls or Hand sensor automatic dispenser In the absence of foot-operated controls or automatic sensors, the area should have a clean paper towel Disposal towels Soap from a foot-operated container or a pump container (bar soap is discouraged) Disposable paper towel Nail stick and./or brush HAND WASHING PROCEDURE Each step has a rationale Handwashing should be 40-60 seconds (whole procedure) while 20 seconds of it is for scrubbing-effective handwashing 1. Remove all rings, watches, and other jewelries or accessories 2. Stand a few inches from the sink Sink may be contaminated Body must not touch the sink 3. Turn on faucet with the foot pedal or with a disposable towel if not foot-controlled 4. Wet hands under the running water. Be careful to not touch the sides of the sink Warm water should be used The water should not be too hot or too cold and hand should be wet before applying soap to minimize drying, chopping, or cracking of hands from frequent hand washing Not necessary to use tissue to open faucet before handwashing 5. Apply soap, and lather well. The lather and scrubbing action will remove dirty and dead skin Common mistake – There is not enough soap to make good lather 6. Scrub for at least 15 seconds between fingers, knuckles, and around fingernails. Use a nail stick and a brush during the first hand washing of each day or when your hands become excessively soiled Necessary to dislodge microorganisms especially between the fingers and around the knuckles Has proper step for scrubbing procedure – To cover all surfaces of the hand Common Mistake – There is no force while scrubbing 7. Apply a little friction and rub hands together for at least 15 seconds Friction helps loosen dead skin, dirt, debris, and microorganisms 8. Rinse hands with water flowing downward from wrist to fingertips Complete the washing process again if this is the first hand washing of the day DOWNWARD MOTION Allows contaminants to be flushed from hands and wrist and down to the sink rather than to go back up to the hands, wrist, and to arms COMMON MISTAKE – Not all soap is rinsed off (usually around the wrist parts and in between fingers) 9. Dry hands and wrists with the disposable clean paper towels 10. Turn off the water with the disposable towels if the sink is not footcontrolled Tissue used for drying hands (if not fully soaked) – Can be used to turn off the faucet Clean hands should not touch the contaminated faucet handle (consider the whole sink as contaminated) WHEN IS HANDWASHING REQUIRED? 1. Before and after patient contact Each room of the patient has hand sanitizer 2. Between unrelated procedure from patient such as drawing of blood 3. Before putting on your gloves and after taking them off 4. Before leaving the laboratory 5. Before going to lunch or break 6. Before and after going to the restroom 7. Whenever the hands become knowingly and visibly contaminated ’ PERSONAL PROTECTIVE EQUIPMENT Includes the gloves, masks, shoes, and laboratory gowns. It may also include goggles and face shields. These PPE’s are used to protect the laboratory scientist/medical technologist from infectious material MASKS Prevent the transmission of infectious agents through the air. This should always be worn by the medical technologists especially when entering the respiratory isolation room. It should cover both the nose and mouth, and worn only once then discarded in an appropriate container. Masks are no longer effective once they become moist from breathing GLOVES Worn due to following reasons: 1. It prevents the medical technologists from transmitting their own microdata to the patient 2. It prevents transmission of microorganisms from one patient to another; and 3. It prevents the laboratory scientists or medical technologists from being infected by organisms from the patient Should be equivalent – Wearing should be as good as removing There is a proper order of putting on and removing PPE (form the most contaminated o the least contaminated) LABORATORY GOWNS Worn when soiling of clothes is possible while working in the laboratory or extracting blood from patients. It should be fluid resistant to prevent any blood or body fluids from soaking through and getting on the medical technologist. Wearing of laboratory gowns prevents transmission of microorganisms from the patient’s and environment to the medical technologist. Ideally, it should be used only once then disposed of in appropriate receptacle. PROPER DONNING OF PPE’S 1. LAB SHOES 2. HEAD CAP 3. LAB GOWN 4. MASK OR RESPIRATOR 5. GOGGLES 6. GLOVES Should be over the sleeve of the lab gown PRINCIPLE Proper donning and removing of PPE’s to prevent the transfer of organisms from a source to a susceptible host MATERIALS Biohazard waste container Disposable cap Disposable gloves (sterile or unsterile) Disposable mask Laboratory gown (preferably disposable) Laboratory shoes PROCEDURE 1. Remove all accessories and put away all gadgets. Store them inside the bag or locker 2. Remove street shoes and wear laboratory shoes 3. Wear the mask by placing the top of the mask over the bridge of the nose and pinch the metal strip to fit the nose. If you are using a mask with strings, tie the top strings of the mask so the strings are positioned above the ears then the lower strings behind the neck 4. If necessary, apply the cap to cover hair and ears. Pull long hair up under the cap 5. Place the gown in front of your body and place your arms through the sleeves of the gown. If you are wearing a gown with strings, tie top stings on the gown behind the neck then tie the lower strings of the gown behind the back 6. Make sure to button the gown properly 7. Put on gloves PROPER REMOVAL OF PPE’S 1. 2. 3. 4. 5. PRINCIPLE Opposite of donning Gloves (most contaminated) Goggles Lab Gown Mask Head Cap Before and after wearing PPE’s – Should do proper handwashing Proper removal of PPE’s prevents the transfer of organisms from a source to a susceptible host MATERIALS Same as donning PROCEDURE 1. Remove contaminated gloves properly and discard it into the biohazard container 2. Wash hands properly 3. Remove the mask. If you are using a mask with strings, untie the top tie first and then the bottom tie. Hold the mask by the ties and drop it into biohazard waster container 4. Remove the laboratory gown. Slip the fingers of one hand inside the cuff of the gown and pull the gown over the hand 5. Using the hand covered by the gown, pull the gown down over the other hand 6. Pull the gown off your arms. Hold the gown away from you and roll it into a ball with the contaminated side on the inside of the ball 7. Dispose the gown into the biohazard container or its appropriate receptacle 8. Remove the cap 9. Remove the laboratory shoes HOW TO REMOVE LAB GOWN Aim: To remove inside out PROPER REMOVAL OF CONTAMINATED GLOVES PRINCIPLE Gloves after usage should be removed properly to avoid contamination of the laboratory scientist or medical technologist. This will also decrease the transfer of organisms from a source to susceptible host. MATERIALS Biohazard waste container Gloves PROCEDURES 1. Place hands with gloves in front and away from the body 2. Grasp the palm of the loves on the left hand, and pull it down to turn it inside out. Do not touch the bare skin with the contaminated gloves 3. The right hand still having the gloves on should then hold the inverted and removed glove 4. Contain the inverted glove completely in the gloved hand 5. Insert two fingers of the ungloved hand under the cuff of the glove on the other hand 6. Pull down the glove to turn it inside out 7. Contain the other glove inside the inverted glove 8. Dispose the gloves into a biohazard container 9. Wash hands with running water