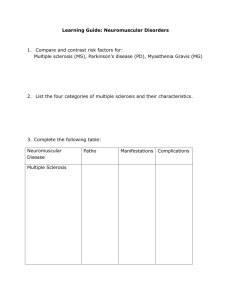
NURS 4410 NEURO- CHAPT 69 & 70 LECTURE VERSION Spring 2019 Alfred State Marilyn J. Oggeri MSN, RN MANAGEMENT OF PATIENTS WITH NEUROLOGICAL INFECTIONS, AUTOIMMUNE DISORDERS, & NEUROPATHIES / ONCOLOGICAL OR DEGENERATIVE 1 NEUROLOGICAL DISORDERS LEARNING OBJECTIVES 16. Differentiate among the primary causes, collaborative care, and nursing management of meningitis, brain abscesses, encephalitis, Creutzfieldt-Jacob disease, MS, Myasthenia Gravis, Guillian-Barre, Cranial Nerve Disorders, Brain / Spinal tumors, Parkinson’s, Huntington’s, MD 2 INFECTIOUS NEUROLOGIC DISORDERS 1. Meningitis 2. Brain abscesses 3. Encephalitis 4. Creutzfeldt-Jakob disease and variant Creutzfeldt-Jakob disease QUESTION Is the following statement true or false? Meningitis is an inflammation of the pia mater, the arachnoid, and the cerebrospinal fluid– filled subarachnoid space. ANSWER True Meningitis is an inflammation of the pia mater, the arachnoid, and the cerebrospinal fluid– filled subarachnoid space. QUESTION What is a positive Kernig’s sign? A. Extreme sensitivity to light B. Any attempts at flexion of the head are difficult because of spasms in the muscles of the neck. C. When the patient is lying with the thigh flexed on the abdomen, the leg cannot be completely extended. D. When the patient’s neck is flexed, flexion of the knees and hips is produced; when the lower extremity of one side is passively flexed, a similar movement is seen in the opposite extremity. ANSWER C. When the patient is lying with the thigh flexed on the abdomen, the leg cannot be completely extended. Photophobia is common with meningitis and is extreme sensitivity to light. Nuchal rigidity is any attempts at flexion of the head are difficult because of spasms in the muscles of the neck. Kernig’s sign is when the patient is lying with the thigh flexed on the abdomen, the leg cannot be completely extended. Brudzinski’s sign is when the patient’s neck is flexed, flexion of the knees and hips is produced; when the lower extremity of one side is passively flexed, a similar movement is seen in the opposite extremity. KERNIG’S SIGN BRUDZINSKI’S SIGN MENINGITIS 1. Inflammation of the membranes and the fluid space surrounding the brain and spinal cord 2. Types 1. Septic caused by bacteria (Streptococcus pneumoniae, Neisseria meningitidis) 2. Aseptic caused by viral infection, lymphoma, leukemia, or brain abscess 3. N. meningitidis is transmitted by secretions or aerosol contamination, and infection is most likely in dense community groups such as college campuses 4. Manifestations include headache, fever, changes in LOC, behavioral changes, nuchal rigidity (stiff neck), positive Kernig's sign, positive Brudzinski’s sign, and photophobia MEDICAL MANAGEMENT 1. Prevention by vaccination against Haemophilus influenzae and S. pneumoniae for all children and all at-risk adults 2. Prevention by meningococcal vaccination for adolescents and highrisk groups 3. Early administration of high doses of appropriate IV antibiotics for bacterial meningitis 4. Dexamethasone (steroid) 5. Treatment dehydration, shock, and seizures NURSING MANAGEMENT 1. Frequent or continual assessment, including VS and LOC 2. Protect patient form injury related to seizure activity or altered LOC 3. Monitor daily weight (look at fluid shifts), serum electrolytes, urine volume, specific gravity, and osmolality 4. Prevent complications associated with immobility 5. Infection control precautions 6. Supportive care 7. Measures to facilitate coping of patient and family BRAIN ABSCESS 1. Collection of infectious material within brain tissue 2. Risk is increased in immunocompromised patients 3. Prevent by treating otitis media, mastoiditis, sinusitis, dental infections, and systemic infections promptly 4. Manifestations may include headache that is usually worse in the morning, fever, vomiting, neurologic deficits, signs and symptoms of increased ICP 5. Diagnosis by MRI or CT 6. CT-guided aspiration is used to identify the causative organisms BRAIN ABSCESS (CONT’D) 8. Medical management 1. Control ICP 2. Drain abscess 3. Administer appropriate antibiotic therapy; corticosteroids may be used to treat cerebral edema 9. Nursing management 1. Frequent and ongoing neurologic assessment and of responses to treatment 2. Assure patient safety and protect from injury 3. Provide supportive care ENCEPHALITIS 1. Acute, inflammatory process of the brain tissue 2. Causes include viral infections (herpes simplex [HSV]), vector-borne viral infections (West Nile, St. Louis), and fungal infections 3. Manifestations may include headache fever, confusion, changes in LOC; vector borne—rash, flaccid paralysis, Parkinson-like movements 4. Medical management 1. Acyclovir for HSV infection, amphotericin or other antifungal agents for fungal infection 5. Nursing management 1. Frequent and ongoing assessment 2. Supportive care CREUTZFELDT-JAKOB DISEASE AND VARIANT CREUTZFELDT-JAKOB DISEASE 1. Rare, degenerative infectious, transmissible spongiform encephalopathies (TSEs) 2. TSEs are caused by prions: small proteinaceous particles that are smaller than viruses and resistant to sterilization 3. The disease is not spread by casual contact; vCJD may be contracted through ingestion of infected beef. 4. Manifestations include affective, sensory, motor, and cognitive impairments. 5. No effective treatment; progressive and fatal 6. Nursing management 1. Prevention of disease transmission; blood and body fluid precautions 2. Supportive care AUTOIMMUNE NEUROLOGIC DISORDERS 1. Multiple sclerosis (MS) 2. Myasthenia gravis 3. Guillain-Barré syndrome QUESTION Is the following statement true or false? Multiple sclerosis is an immune-mediated, progressive demyelinating disease of the peripheral nervous system. ANSWER False Multiple sclerosis is an immune-mediated, progressive demyelinating disease of the central nervous system, not the peripheral nervous system. MULTIPLE SCLEROSIS 1. A progressive immune-related demyelination disease of the CNS 2. Clinical manifestations vary and have different patterns 3. Frequently, the disease is relapsing and remitting; has exacerbations and recurrences of symptoms, including fatigue, weakness, numbness, difficulty in coordination, loss of balance, pain, and visual disturbances 4. Medical management 1. Disease-modifying therapies; interferon -1a and interferon -1b, glatiramer acetate (Copaxone), and IV methylprednisolone 2. Symptom management of muscle spasms, fatigue, ataxia, bowel and bladder control PROCESS OF DEMYELINATION TYPES AND COURSES OF MULTIPLE SCLEROSIS QUESTION Is the following statement true or false? Myasthenia gravis is an autoimmune attack on the peripheral nerve myelin. ANSWER False Guillain–Barré syndrome is an autoimmune attack on the peripheral nerve myelin. Myasthenia gravis is an autoimmune disorder affecting the myoneural junction and is characterized by varying degrees of weakness of the voluntary muscles. NURSING PROCESS: THE CARE OF THE PATIENT WITH MULTIPLE SCLEROSIS—ASSESSMENT 1.Neurologic deficits 2. Secondary complications 3. Impact of disease on physical, social, and emotional function and on lifestyle 4. Patient and family coping NURSING PROCESS: THE CARE OF THE PATIENT WITH MULTIPLE SCLEROSIS—DIAGNOSES 1. Impaired physical mobility 2. Risk for injury 3. Impaired bowel and bladder function 4. Impaired verbal communication 5. Disturbed thought processes 6. Ineffective coping 7. Impaired home maintenance 8. Potential sexual dysfunction NURSING PROCESS: THE CARE OF THE PATIENT WITH MULTIPLE SCLEROSIS—PLANNING 1.Major goals may include 1. Promotion of physical mobility 2. Avoidance of injury 3. Achievement of bowel and bladder continence 4. Promotion of speech and swallowing mechanisms 5. Improvement in cognitive function 6. Development of coping strengths 7. Improved home maintenance 8. Adaptation to sexual function INTERVENTIONS 1, Use a collaborative approach 2. Coordinate and refer as needed to health care services: social services, speech therapy, physical therapy, counseling services, home care services, and so on 3. Activity and rest 1. Program of activity and daily exercise 2. Relaxation, coordination exercises, walking, muscle-stretching exercises 3. Avoid very strenuous activity and extreme fatigue INTERVENTIONS (CONT’D) 1. Bowel and bladder control 1. Instruction or administration of prescribed medications 2. Voiding schedule 3. Bowel training program 4. Adequate fluid and fiber to prevent constipation 2. Reinforce and encourage swallowing instructions 3. Strategies to reduce risk of aspiration 4. Memory aides, structured environment, and daily routine to enhance cognitive function INTERVENTIONS (CONT’D) 1. Interventions to minimize stress 2. Maintenance of temperate environment—air conditioning to avoid excessive heat and avoidance of exposure to extreme cold 3. Use assistive devices and modifications for home care management and independence in ADLs 4. Support of coping MYASTHENIA GRAVIS 1. Autoimmune disorder affecting the myoneural junction 2. Antibodies directed at acetylcholine at the myoneural junction impair transmission of impulses 3. Manifestations 1. a motor disorder 2. Initially symptoms involve ocular muscles: diplopia (double vision) and ptosis (eyelid drooping) 3. Weakness of facial muscles, swallowing and voice impairment (dysphonia), generalized weakness MYASTHENIA GRAVIS (CONT’D) Normal ACh receptor site ACh receptor site in myasthenia gravis MEDICAL MANAGEMENT 1. Pharmacologic therapy 1. Cholinesterase inhibitor: pyrostigmine bromide (Mestinon) 2. Immunomodulating therapy 2. Plasmapheresis 3. Thymectomy MYASTHENIC CRISIS VS CHOLINERGIC CRISIS 1. Result of disease exacerbation or precipitating event, most commonly a respiratory infection 2. Severe generalized muscle weakness with respiratory and bulbar weakness 3. Patient may develop respiratory compromise/failure 4. Caused by overmedication with cholinesterase inhibitors 5. Severe muscle weakness with respiratory and bulbar weakness (motor neuron impairment of Cranial nerves 9-12) 6. Patent may develop respiratory compromise and failure MANAGEMENT OF MYASTHENIC CRISIS 1. Patient education in signs and symptoms of myasthenic crisis and cholinergic crisis 2. Ensuring adequate ventilation; intubation and mechanical ventilation may be needed. 3. Assessment and supportive measures 1. Measures to ensure airway and respiratory support 2. ABGS, serum electrolytes, I&O, and daily weight 3. If patient cannot swallow, nasogastric feeding may be required 4. Avoid sedatives and tranquilizers NURSING PROCESS: THE CARE OF THE PATIENT WITH MYASTHENIA GRAVIS 1. Focus on patient and family education 2. Medication education and management 3. Energy conservation 4. Strategies to help with ocular manifestations 5. Prevention and management of complications and avoidance of crisis 6. Measures to reduce risk of aspiration 7. Avoidance of stress, infections, vigorous physical activity some medications, and high environmental temperatures GUILLAIN-BARRÉ SYNDROME 1. Autoimmune disorder with acute attack of peripheral nerve myelin 2. Rapid demyelination may produce respiratory failure and autonomic nervous system dysfunction with CV instability 3. Most often follows a viral infection 4. Manifestations are variable and may include weakness, paralysis, paresthesias, pain, and diminished or absent reflexes, starting with the lower extremities and progressing upward; bulbar weakness; cranial nerve symptoms; tachycardia; bradycardia; hypertension; or hypotension GUILLAIN-BARRÉ SYNDROME (CONT’D) 5. Medical management 1. Requires intensive care management with continuous monitoring and respiratory support 2. Plasmapheresis and IVIG are used to reduce circulating antibodies **Recovery rates vary, but most patients recover completely NURSING PROCESS: THE CARE OF THE PATIENT WITH GUILLAIN–BARRÉ SYNDROME— ASSESSMENT 1. Ongoing assessment for with emphasis on early detection of life-threatening complications of respiratory failure, cardiac dysrhythmias, and deep vein thrombosis (DVT) 2. Monitor for changes in vital capacity and negative inspiratory force 3. Assess VS frequently or continuously, including continuous monitoring of ECG 4. Patient and family coping NURSING PROCESS: THE CARE OF THE PATIENT WITH GUILLAIN-BARRÉ SYNDROME—DIAGNOSES 1. Ineffective breathing pattern 2. Impaired gas exchange 3. Impaired physical mobility 4. Imbalanced nutrition 5. Impaired verbal communication 6. Fear 7. Anxiety COLLABORATIVE PROBLEMS AND POTENTIAL COMPLICATIONS OF GUILLAINBARRE SYNDROME 1. Respiratory failure 2. Autonomic dysfunction 3. DVT 4. Pulmonary embolism 5. Urinary retention NURSING PROCESS: THE CARE OF THE PATIENT WITH GUILLAIN-BARRÉ SYNDROME—PLANNING Major goals include 1. Improved respiratory function 2. Increased mobility 3. Improved nutritional status 4. Effective communication 5. Decreased fear and anxiety 6. Effective patient and family coping 7. Absence of complications INTERVENTIONS 1. Enhancing physical mobility and prevention of DVT 1. Support limbs in functional position 2. Passive ROM at least twice daily 3. Frequent position changes at least every 2 hours 4. Elastic compression hose or sequential compression boots 5. Adequate hydration 2. Administer IV and parenteral nutrition as prescribed 3. Carefully assess swallowing and gag reflex and take measures to prevent aspiration INTERVENTIONS (CONT’D) 1. Develop a plan for communication individualized to patient needs 2. Decreasing fear and anxiety 1. Provide information and support 2. Referral to support group 3. Relaxation measures 4. Maintain positive attitude and atmosphere to promote a sense of well-being 5. Diversional activities CRANIAL NERVE DISORDERS 1. Refer to Table 69-2 2. Trigeminal neuralgia (tic douloureux) 3. Bells’ palsy TRIGEMINAL NEURALGIA (TIC DOULOUREUX) 1. Condition of the fifth cranial nerve characterized by paroxysms of pain 2. Most commonly occurs in the second and third branches of this nerve. Vascular compression and pressure is the probable cause. 3. Occurs more often in the fifth and sixth decades and in women and persons with MS 4. Pain can occur with any stimulation such as washing face, brushing teeth, eating, or a draft of air. 5. Patients may avoid eating, neglect hygiene, and even isolate themselves to prevent attacks. DISTRIBUTION OF THE TRIGEMINAL NERVE BRANCHES MEDICAL MANAGEMENT 1. Antiseizure medications such as carbamazepine (Tegretol), gabapentin (Neurontin), phenytoin, or antispasmodic medication baclofen (Lioresal) 2. Surgical treatment 1. Microvascular decompression of the trigeminal nerve 2. Radiofrequency thermal coagulation 3. Percutaneous balloon microcompression NURSING INTERVENTIONS 1. Patient education related to pain prevention and treatment regimen 2. Measures to reduce and prevent pain; avoidance of triggers 3. Care of the patient experiencing chronic pain 4. Measures to maintain hygiene: washing face, oral care 5. Strategies to ensure nutrition; soft food, chew on unaffected side, avoid hot and cold food 6. Recognize and provide interventions to address anxiety, depression, and insomnia BELL’S PALSY 1. Facial paralysis caused by unilateral inflammation of the seventh cranial nerve 2. Manifestations: unilateral facial muscle weakness or paralysis with facial distortion, increased lacrimation (tears), and painful sensations in the face; may have difficulty with speech and eating 3. Most patients recover completely in 3 to 5 weeks, and the disorder rarely recurs. DISTRIBUTION OF THE FACIAL NERVE (#7) MANAGEMENT 1. Medical 1. Corticosteroid therapy may be used to reduce inflammation and diminish severity of the disorder. 2. Nursing 1. Provide and reinforce information and reassurance that stroke has not occurred. 2. Protection of the eye from injury; cover eye with shield at night, instruct patient to close eyelid, use of eye ointment and sunglasses. 3. Facial exercises and massage to maintain muscle tone BRAIN & SPINAL CORD TUMORS 1.Brain Tumors 1. Classified by location and histology characteristics (what kind of cells the tumor is made up of) 2. Symptoms depend on the location and size of the lesion and its compression on the nearby structures 3. Dx with CTs, MRIs, PET scans, EEGs, Bx, Spinal Tap 4. Rx depends on type location and accessibility of the tumor 1. Surgery – goal is to remove tumor WITHOUT ↑ neuro s&s OR ↓ s&s by decompression. 2. Radiation Rx 3. Chemotherapy 4. Pharmacological Rx for s&s control 2. Spinal Cord Tumors 1. Classified by their anatomic relation to the spinal cord 2. Manifestations include pain, weakness, loss of motor or sensory or reflexes 2. Rx depends on type of tumor and location PARKINSON’S DISEASE 1.Slow, progressive neurologic movement disorder associated with decreased levels of dopamine 2.Manifestations: 1.Cardinal: tremor, rigidity, bradykinesia/akinesia, postural instability 2.Autonomic: sweating, drooling, flushing, orthostatic hypotension, gastric and urinary retention 3.Dysphagia 4.Psychiatric changes: depression, anxiety, dementia, delirium, hallucinations 3.Treatment directed toward controlling symptoms and maintaining functional independence. 1.Pharmacologic treatment (Levodopa, Table 70-1) 2.Surgical procedures 1.Stereotactic Procedures; thalamotomy, pallidotomy 3.Neural transplantation 4.Ongoing research HUNTINGTON’S DISEASE 1. A chronic progressive hereditary disease that results in choreiform( rapid, jerky, involuntary, purposeless) movements and dementia 2.Transmitted as an autosomal dominant trait 3. Pathology involves premature death of cells in the striatum of the basal ganglia (control of movement) and the cortex (thinking, memory, perception, judgment) 4.Refer to Chart 70-5 5.Treatment is aimed at s&s relief. AMYOTROPHIC LATERAL SCLEROSIS (ALS) 1. “Lou Gehrig disease” 2. Loss of motor neurons in the anterior horn of the spinal cord and loss of motor nuclei of the lower brainstem 3. Manifestations 1. Progressive weakness and atrophy of muscles, cramps, twitching, and lack of coordination 2. Spasticity, deep tendon reflex brisk and overactive 3. Difficulty speaking, swallowing, breathing MUSCULAR DYSTROPHIES 1. Incurable disorders characterized by progressive weakening and wasting of skeletal and voluntary muscles 2. Most are inherited disorders 3. Duchenne muscular dystrophy is the most common and inherited as a sex-linked trait (influences males. Women carry it but their sons get it) 4. Common characteristics: 1. Varying degrees of muscle wasting and weakness 2. Abnormal elevation in serum levels of muscle enzymes REFERENCES Hinkle, J., Cheever, K., Brunner & Suddarth’s Textbook of Medical-Surgical Nursing, 14th Edition, LWW, 2018 Oggeri, M.J. Neuro 4410 2018 Lectures/PPT, Alfred State College Oggeri, M.J. , Shepard, T., Neuro 4410 2017 Focus on Head InjuryIICP Lecture /PPT, Alfred State College Oggeri, M.J. , Shepard, T., Neuro 4410 2017 Head Injury and Spinal Injury Lecture/PPT, Alfred State College Oggeri, M.J., Neuro 3310 2017 Neuro Assessment Lecture/PPT, Alfred State College Shepard, T., 4410, 2017 Back Pain & Spinal Injury Lecture/PPT, Alfred State College 58