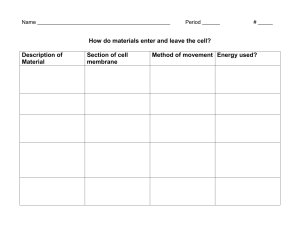
Chapter1: Orientation to Pharmacology A. Basic terms a. Drug i. any chemical that can affect living process Pharmacology i. the study of drugs and their interaction with living systems c. Clinical pharmacology i. the study of drugs in humans d. Therapeutics- AKA pharmacotherapeutics i. The use of drugs to diagnose, prevent, or treat disease or prevent pregnancy Properties of an Ideal Drug a. Effectiveness- the most important property. An effective drug is one that elicits the responses for which it is given. b. Safety- a safe drug is one that cannot produce harmful effect i. Adverse effect 1. Certain drugs can increase the risk of infection (eg. cyclophosphamide, methotrexate) 2. Opioid analgesics at high doses can cause respiratory depression (eg. Morphine) 3. Aspirin and other related drugs can cause severe gastric ulceration, perforation, and bleeding when taken for prolong periods of time. c. Selectivity- a drug that elicits only the response for which it is given Additional Properties of an Ideal Drug a. Reversible action i. effects must be reversible. Drug action must subside within an appropriate time b. Predictability i. tailor drug to individual to elicit the desired response c. Ease of administration i. should be simple to administer. Will enhance patient adherence and reduce risk d. Freedom from drug interaction i. interaction of drugs may be positive or negative e. Low cost i. an ideal drug is easy to afford f. Chemical stability i. an ideal drug would retain its activity indefinitely. Some drug loses their effectiveness over time g. Simple generic name i. an ideal drug should have a generic name that is easy to recall or pronounce The therapeutic Objective of Drug Therapy a. To provide the maximum benefit with minimum harm Factors the Determine the Intensity of Drug Response a. Administration i. Dosage size, route, timing ii. Med errors iii. Patient adherence b. Pharmacokinetics i. Determining how much of the administered dose gets to its sites of action ii. The impact of the body on drugs 1. Drug absorption 2. Drug distribution 3. Drug metabolism 4. Drug excretion c. Pharmacodynamic i. Impact of drugs on the body ii. Drug-receptor interaction 1. Binding of the drug to its receptors iii. Patient’s functional state 1. Influences pharmacodynamic processes iv. Placebo effects 1. Helps determine the Reponses a drug elicits d. Sources of individual variation i. Physiological variables 1. Age, gender, weight b. B. C. D. E. ii. iii. iv. Pathologic variables 1. Diminished function of kidneys and liver Genetic variables 1. Can alter the metabolism of drugs and predispose the patient to unique interactions Drug interactions Chapter 2: Applications of Pharmacology in Nursing Practice A. Evolution of Nursing Responsibility regarding drugs a. Right drug b. Right patient c. Right dose d. Right time e. Right assessment f. Right documentation g. Right evaluation h. Right of patient to education i. Right of patient to refuse care B. Evolution of Nursing Responsibilities Regarding Drugs a. Correct administration, without addition interventions, cannot ensure that treatment will result in the therapeutic objective b. Proper delivery is only the beginning of a nurse’s responsibility c. Nurses and healthcare providers must participate in a system of checks and balances designed to promote beneficial effects and to minimize hard to patients d. The nurse must know what meds are appropriate for the patient and what drugs are contraindicated for the patient e. The nurse must know the probable consequences of the interactions between the drug and the patient f. The nurse’s role as an advocate i. Last line of defense for the patient ii. Ethically and legally unacceptable to administer a drug that is harmful to the patient, even though the medication has been prescribed by a licensed prescriber and dispensed by a licensed pharmacist C. Application of Pharmacology in Patient Care a. Preadministration assessment i. Collecting baseline data 1. To evaluate the therapeutic response and adverse effects ii. Identifying high-risk patients 1. Predisposing factors such as liver and kidney impairment 2. Genetic factors 3. Drug allergies 4. Pregnancy 5. Older adults or pediatric age group iii. Tools: patient history, physical exam and lab results b. Dosage and administration i. Certain drugs have more than one indication ii. The dosage may differ for which the drug is being used iii. Many drugs can be administered by more than one route iv. The dosage may differ depending on the route selected v. Certain IV agents can cause severe local injury of extravasation occurs vi. Read medication order carefully vii. Verify the identity of the patient viii. Read the med label carefully ix. Verify dosage calculations x. Implement any special handling that the drug may require xi. Do not administer any drug if you do not understand the reason for its use c. Evaluating and promoting therapeutic effects i. Evaluating therapeutic responses 1. One of the most important aspects of drug therapy 2. The know the rationale for treatment and the nature and time course of the intended response 3. Cannot effectively evaluate a drug with multiple application if the intended use is not known ii. Promoting patient adherence 1. Also known as compliance or concordance 2. Extent to which a patient’s behavior coincides with medical advice iii. Implementing nondrug measures 1. Drugs therapy can often ne enhanced by nondrug measures 2. These include biofeedback, emotional support, smoking cessation, sodium restriction and so on d. Minimizing adverse interactions i. All drugs have the potential to produce undesired effects ii. Always know the following: 1. The major adverse effects that the drug can produce 2. The times when these reactions are likely to occur 3. Early signs that can adverse reaction is developing 4. Interventions that can minimize discomfort and harm iii. Take a thorough drug history iv. Advise the patient to avoid OTC drugs that can interact with the prescribed medication v. Monitor for adverse interactions that are known to occur vi. Be alert for as-yet-unknown interactions e. Making PRN decisions i. PRN: pro re nata; “as needed” ii. The nurse has discretion regarding how much drug to give and when to give it iii. Know the reason for the drug’s use iv. Be able to assess the patient’s medication needs f. Managing toxicity i. Early identification makes early intervention possible ii. Know the early signs of toxicity iii. Know the procedure for toxicity management D. Application of Pharmacology in Patient Education a. Drug name and therapeutic category b. Dosage size c. Dosing schedule d. Route and technique of administration e. Expected therapeutic response and when it should develop f. Nondrug measures to enhance therapeutic response g. Duration of treatment h. Method of drug storage i. Symptoms of major adverse effects and measures to minimize discomfort and harm j. Major adverse drug-drug and drug-food interactions k. Whom to contact in the event of therapeutic failure, severe adverse reactions, or severe adverse interactions l. Give the patient the following info: i. Name of drug ii. Dosage and schedule of administration iii. Technique of administration iv. Duration of drug use v. Storage of drugs m. Promoting therapeutic effects i. Nature and time course of expected beneficial effects ii. Recognizing treatment failure; allow for timely alternative therapy implementation n. Minimizing adverse effects i. Insulin OD ii. Anticancer and infection iii. Some side effects are benign but disturbing, esp. if they are unknow to the patient o. Minimizing Adverse Interactions i. Educate the patient about hazardous drug-drug and drug-food interactions 1. Ex: Phenelzine and it interactions with amphetamines (drugs) and figs (food) E. Application of the Nursing Process in Drug Therapy a. The nursing process is a conceptual framework that nurses employ to guide healthcare delivery. b. Assessment i. Collecting data to identify actual and potential health problems 1. Patient interview, medical and drug use history, physical examination, observation and lab test. c. Analysis: Nursing diagnoses i. Analyzing information collected to determine actual and potential health problems ii. A complete nursing diagnosis consist of the following 1. Statement of the patient actual or potential health problems 2. Statement of the problem’s probably cause or risk 3. Signs, symptoms or evidence of the problem d. Planning F. i. Outline specific interventions directed at solving or preventing the problems identified in analysis. ii. Plan is individualized iii. Nurse defines goals, set priorities, identify nursing interventions, and establish a criteria for evaluating success. iv. Ongoing process e. Implementation (Intervention) i. Carrying out the interventions identified during planning ii. Interventions are independent or collaborative f. Evaluation i. Determining the degree to which the treatment has succeeded ii. Identifying interventions that should be continued, discontinued or new interventions that may need to be implemented. Applying the Nursing Process in Drug Therapy a. Preadministration assessment i. Collection of baseline data to evaluate therapeutic effects ii. Collection of baseline data to evaluate adverse effects iii. Identification of high-risk patients 1. Factors that might increase risks of adverse reaction include age, body composition, pregnancy, diet, genetics and other drugs being used. 2. Distinguish between contraindication and precaution a. Contraindication is a condition that prohibits use of a particular drug under all but the most critical of circumstances b. A precaution is a condition that significantly increases the risk of an adverse reaction but is not life threatening 3. iv. Assessment of the patient’s capacity for self-care b. Analysis and nursing diagnosis i. Judge the appropriateness of the prescribes regimen ii. Identify potential health problems that the drug might cause iii. Determine the patient’s capacity for selfcare c. Planning i. Defining goals 1. Formulating ways to achieve goals ii. Setting priorities 1. Highest priority given to life-threatening conditions iii. Identifying specific interventions 1. Drug administration 2. Interventions to enhance therapeutic effects a. E.g. After administration of pain meds, turn the lights off so patient can relax 3. Interventions to minimize adverse effects 4. Patient education iv. Establishing objective criteria for evaluation d. Implementation i. Drug administration ii. Patient education iii. Interventions to promote therapeutic effects iv. Interventions to minimize adverse effects e. Evaluation i. Therapeutic responses ii. Adverse drug reactions and interactions iii. Adherence to prescribed regimen iv. Satisfaction with treatment Chapter 3: Drug Regulation, Development, Names, and Information A. Landmark drug legislation a. Federal pure Food and Drug Act, 1906 i. Set standards for drug quality, purity and strength ii. Product labeling b. Food, Drug, and Cosmetic Act, 1938 i. First to regulate drug safety c. Harris-Kefauver Amendments, 1962 i. First to demand that drugs actually be of some benefit d. Controlled Substances Act, 1970 i. Set rules for the manufacture and distribution of drugs considered to have potential for abuse e. Permission for accelerated drug approval 1992 i. Drugs can be approved for marketing before completion of Phase III trials f. Prescription Drug user Fee Act, 1992 i. Drug sponsors pay the FDA a fee to review drug in a timely fashion g. Food and Drug Administration Modernization Act, 1997 i. Widespread changes in the FDA regulation h. Best Pharmaceuticals for Children Act, 2002 i. Promote research on drug efficacy and safety in children i. Pediatric Research Equity Act, 2003 i. Promote research on drug efficacy and safety in children j. FDA Amendments Acts, 2007 i. Rigorous oversight of drug safety after it has been released for marketing k. Family Smoking Prevention and Tobacco Control Act, 2009 i. Allows the FDA to regulate cigarettes B. New drug development a. Randomized controlled trials i. Use of controls 1. Subjects in the RCT either given the new drug or either a standard treatment or a placebo (control) ii. Randomization 1. subjects are randomly assigned to a control group or the experimental group iii. Blinding – participants do not know if they are getting the real drug b. Preclinical testing c. Clinical testing i. Phase I 1. Small number of healthy volunteers. Some get placebo ii. Phase II and III 1. Tested in patients to determine therapeutic effects, dosage range, safety and effectiveness 2. 500-5000 patients receive the drug iii. Phase IV: Post marketing surveillance 1. New drug is released for general use 2. Observing effects in a large population d. Limited information about the majority of people i. women over 60 yrs. are not tested ii. small children are not tested e. Failure to detect adverse effects i. During clinical trials only a small number of patients are given the drug ii. These patients are carefully selected and do not represent the full spectrum of individuals who will eventually take the drug iii. Patients in the trials only take the drug for a short while f. Exercising discretion regarding new drug i. Be neither the first to adopt the new nor the last to abandon the old ii. Balance potential benefits against inherent risk iii. New drugs generally present greater risk than old ones C. Drug names a. Chemical Name i. Description of the drug using the nomenclature of chemistry b. Generic Name i. Name assigned by the United States Adopted Names Council ii. Each drug has only one generic name iii. The nonproprietary name 1. Less complex than chemical name iv. Stick to generic name! c. Brand name i. Name under which the drug is markets ii. The proprietary name or trade name iii. Must be approved by the FDA iv. Problem with trade name 1. Single drug can have multiple trade names 2. U.S. drugs and from outside of the US may have different active ingredients 3. Products with the same trade name may have different active ingredients a. Ex. Kaopectate D. Over-the-counter drugs a. Drugs that can be purchased without a Rx b. Americans spend about 20 billion annually on OTC drugs c. OTC drugs account for 60% of all doses administered d. 40% of Americans take at least one OTC drug every 2 days e. Four times as many illnesses are treated by a consumer using an OTC drug as by a consumer visiting a physician f. For most illnesses (60%-95%), initial therapy consists of self-care, including self-care medication with an OTC drug E. Sources of drug information a. Clinicians and pharmacists b. Poison control centers c. Pharmaceutical sales rep Chapter 4: Pharmacokinetics A. Pharmacokinetics a. Pharmacokinetics is derived from two Greek words: pharmakon (drug or poison) and kinetics (motion) b. Pharmacokinetics is the study of drug movement throughout the body c. Also includes drug metabolism and drug excretion B. Application of pharmacokinetics in therapeutics a. can help maximize beneficial effects and minimize harm C. The four basic pharmacokinetic processes Figure 1 The four basic Pharmacokinetic processes D. Passage of drugs across the cell membrane a. The cell of most membranes is so close to one another that drugs must pass through rather than pass between them b. The cytoplasmic membrane consists of a double layer of molecules known as phospholipids i. Phospholipids are simple lipids (fat) that contain an atom of phosphate ii. Each phospholipid molecule consists of a head (phosphate-containing component) and two tails (long chain hydrocarbon) iii. Large protein molecules may be embedded in the membrane c. There are three ways to cross the cell membrane i. Channels and Pores 1. Channels are extremely small and only small compounds such as potassium and sodium can pass through the channels ii. Transport system (P-glycoprotein) 1. P-glycoproteins are transmembrane protein that transport a wide variety pf drugs out of cells 2. In the liver PGP transport drugs into the bile for elimination 3. In the kidney PGP pumps drugs back into the urine for excretion 4. In the placenta it transports drugs back into the maternal blood 5. In the brain it pumps drugs into the blood, limiting the drug’s access to the brain iii. Direct penetration (most common) 1. For most drugs, movement throughout the body is dependent on the drugs ability to penetrate membranes directly 2. Most drugs are too large to pass through channels or pored 3. Most drugs lack transport systems to help Figure 2 The structure of the cell membrane them cross all of the membranes that separate them from their sites of action, metabolism and excretion 4. Like dissolve like a. Cell membranes are composed primarily of lipids; therefore, to directly penetrate the membrane, a drug must be lipid soluble (lipophilic) d. Passage of Non-Lipophilic Molecules Across the membranes i. Polar molecules 1. Uneven distribution of charge 2. No net charge ii. Ions 1. No net electric charge 2. Quaternary ammonium compounds a. Molecules that contain at least one atom of nitrogen and carry a positive charge at all times b. Carries a positive charge. Not lipid soluble and cannot cross the BBB 3. pH-dependent ionization a. acid is a proton donor -tends to ionize in basic (alkaline) media b. base is a proton acceptor- tends to ionize in acidic media c. not lipid soluble and therefore cannot cross the BBB 4. Ion trapping (pH partitioning) a. Acidic drugs accumulate on alkaline side b. Basic drugs accumulate on acidic side c. The process where a drug accumulates on the side of a membrane where the pH most favors it ionization E. Absorption a. The movement of a drug from its site of administration into the blood b. The rate of absorption determines how soon effects will begin. The amount of absorption helps determine how intense the effects will be c. Factors Affecting Drug Absorption i. Rate of dissolution 1. Rapid dissolution has a faster onset than drugs formulated for a slow dissolution ii. Surface area 1. The larger the surface area the faster the absorption a. Orally administered drug is usually absorbed in the small intestines rather than the stomach iii. Blood flow 1. Drugs are most rapidly absorbed from sites where blood flow is high. 2. The greater the concentration gradient the more rapidly absorption will be iv. Lipid solubility 1. Highly lipid-soluble drugs are absorbed more rapidly than drugs whose lipid solubility is low 2. Lipid soluble drugs can easily cross the cell membrane v. pH partitioning 1. absorption is enhanced when the difference between the pH of plasma and the pH at the site of administration is such that the molecules will have a greater tendency to be ionized in the plasma d. Characteristics of Commonly Used Routes of Administration i. Intravenous 1. Barriers to absorption a. No barriers to absorption 2. Absorption pattern a. Instantaneous Advantages a. Rapid onset, ideal for emergencies b. Precise control over the amount of drug c. Suitability for large volumes d. Suitability for irritant drugs 4. Disadvantages a. Expensive b. Irreversible c. Inconvenient d. Risk of fluid overload, infection and embolism ii. Intramuscular 1. Barriers to absorption a. The only barrier to absorption is the capillary wall b. Large gaps between the cells that comprise the capillary wall. c. Drugs and other molecules can freely move in and out of the blood through these gaps d. Lipid soluble drugs can also pass freely through the cell of the capillary wall Figure 3 Drug movement at capillary beds 2. Absorption pattern a. Rapid with water soluble drugs b. Slow with poorly soluble drugs 3. Advantages a. Permits use of poorly soluble drugs b. Permits use of depot preparations a. Drug is absorbed slowly over an extended time 4. Disadvantages a. Possible discomfort b. Inconvenience c. Potential for injury iii. Subcutaneous 1. Barriers to absorption a. The only barrier to absorption is the capillary wall 2. Absorption pattern a. Rapid with water soluble drugs b. Slow with poorly soluble drugs 3. Advantages a. Permits use of poorly soluble drugs b. Permits use of depot preparations a. Drug is absorbed slowly over an extended time 4. Disadvantages a. Possible discomfort b. Inconvenience c. Potential for injury iv. Oral 1. Barriers to absorption a. Must cross the epithelial lining of the GI tract and the capillary wall 2. Absorption pattern a. Slow and variable 3. 3. 4. F. Advantages a. Ease b. Convenient c. Inexpensive d. Safety Disadvantages a. High variability b. Inactivation by gastric acid and digestive enzymes c. Oral drug must pass through the liver before reaching general circulation a. Enteric-coated oral drugs are designed to release their contents into the small intestine not in the Figure 4 Movement of drug foll. GI absorption stomach b. Sustained-released formulation are designed to release their content slowing permitting longer intervals between doses Distribution a. The drug movement from the blood to the interstitial space of the tissues and from there into the cells b. Distribution is determined by three factors: i. Blood flow to tissues 1. Drugs are carried by the blood to tissues and organs of the body 2. Blood flow determines the rate of delivery 3. Abscesses and tumors a. Low regional blood flow affects therapy b. Pus-filled pockets rather than internal blood vessels c. Solid tumors have limited blood supply ii. Exiting the vascular system 1. After delivery to the organ or tissue via blood, it exists the vascular system 2. Drugs pass between capillary cells rather than through them 3. Blood-Brain Barrier a. Tight junctions between the cells that comprise the walls of most capillaries in the CNS b. Because of the BBB drugs must pass through the cells of the capillary wall c. Only drugs that are lipid soluble or that have a transport system can cross the BBB to a significant degree 4. Placental Drug Transfer a. Membranes of the placenta do NOT constitute an absolute barrier to the passage of drugs i. Movement is determined in the same way as it is for other membranes 5. Risks with drug Figure 5 drug movement across the BBB a. Birth defects: Mental retardation, gross malformations, low birth weigh b. Mother’s use of habitual opioids: Birth of drug-dependent baby 6. To enter the fetal circulation, drugs must cross membrane of the maternal and fetal vascular systems a. Lipid soluble drugs can readily cross these membranes and enter the fetal blood, whereas ions and polar molecules cannot reach the fetal blood 7. Protein Binding a. Drugs form reversible bonds with various proteins b. Plasma albumin is the most abundant and important protein i. Large molecule that always remains in the bloodstream Figure 6 Placental Drug Transfer ii. Affecting drug distribution iii. Entering cells 1. Some drugs must enter cells to reach the site of action 2. Most drugs must enter cells to undergo metabolism and excretion 3. Many drugs produce their affects by binding with receptors on the external surface of the cell membrane a. These do not need to cross the cell membrane to act G. Drug Metabolism a. Also known as biotransformation b. The enzymatic alteration of drug structure c. Takes place in the liver d. Hepatic drug-metabolizing enzymes i. Most drug metabolism that takes place in liver is Figure 7 Protein binding of drugs performs by the hepatic microsomal enzyme system, which is also known as the P450 system ii. Metabolism does not always result in a smaller molecule e. Therapeutic consequences of drug metabolism i. Accelerated renal drug excretion ii. Drug inactivation iii. Increased therapeutic action iv. Activation of prodrugs v. Increased or decreased toxicity f. Special consideration in drug metabolism i. Age ii. Induction of drug-metabolizing enzymes iii. First-pass effect iv. Competition among drugs g. Enterohepatic Recirculation i. Repeating cycle in which drug is transported 1. From the liver into the duodenum via the bile duct 2. Back to the liver via the portal blood ii. Limited to drugs that have undergone glucuronidation H. Excretion a. Defined as the removal of drugs from the body b. Drugs and their metabolites can exist the though urine, sweat, saliva, breast milk or expired air c. Steps in renal drug excretion i. Glomerular filtration ii. Passive tubular reabsorption iii. Active tubular secretion d. Factors that modify renal drug excretion i. pH-dependent ionization ii. competition for active tubular transport iii. age e. Nonrenal Routes of Drug excretion i. Breast milk ii. Bile – Enterohepatic recirculation iii. Lungs (anesthesia) iv. Sweat/saliva f. Time course of Drug Responses i. Plasma drug levels 1. There is a direct correlation between therapeutic and toxic responses and the amount of drug present in the plasma 2. Two plasma drug levels a. Minimum effective concentration MEC a. Plasma drug level below which Figure 8 Renal drug excretion therapeutic effects will not occur b. Toxic concentration a. When plasma drug climb too high 3. Therapeutic range a. The objective of drug dosing is to maintain plasma drug levels within the therapeutic range ii. Single-dose time course 1. The duration of effects is determined largely by the combination of metabolism and excretion 2. For drug levels above the minimum effective dose, the therapeutic response will be maintained iii. Drug half-life 1. The time required for the amount of drug in the body to decrease by 50% 2. Percentage and not the amount of drug lost in a half-life 3. Determines dosing interval iv. Drug levels produced with repeated doses 1. Process by which plateau drugs levels are achieved 2. When drugs are administered repeatedly, their levels will gradually rise to reach a steady plateau 3. Plateau will be reached in about four half-lives 4. The time required to reach plateau us independent of dosage size, although the height of the plateau will be higher with larger doses 5. Fluctuations can be reduced by a. Giving a smaller dose at shorter intervals b. Using continuous infusions c. Using depot preparation 6. For a drug with a long half-life, it may be necessary to use a loading dose (large initial dose) to achieve plateau quickly 7. Plateau is maintained by giving smaller doses (maintenance doses ) 8. When a drug administered is discontinued, 94% of the drug in the body will be eliminated over an interval of about four half lives.