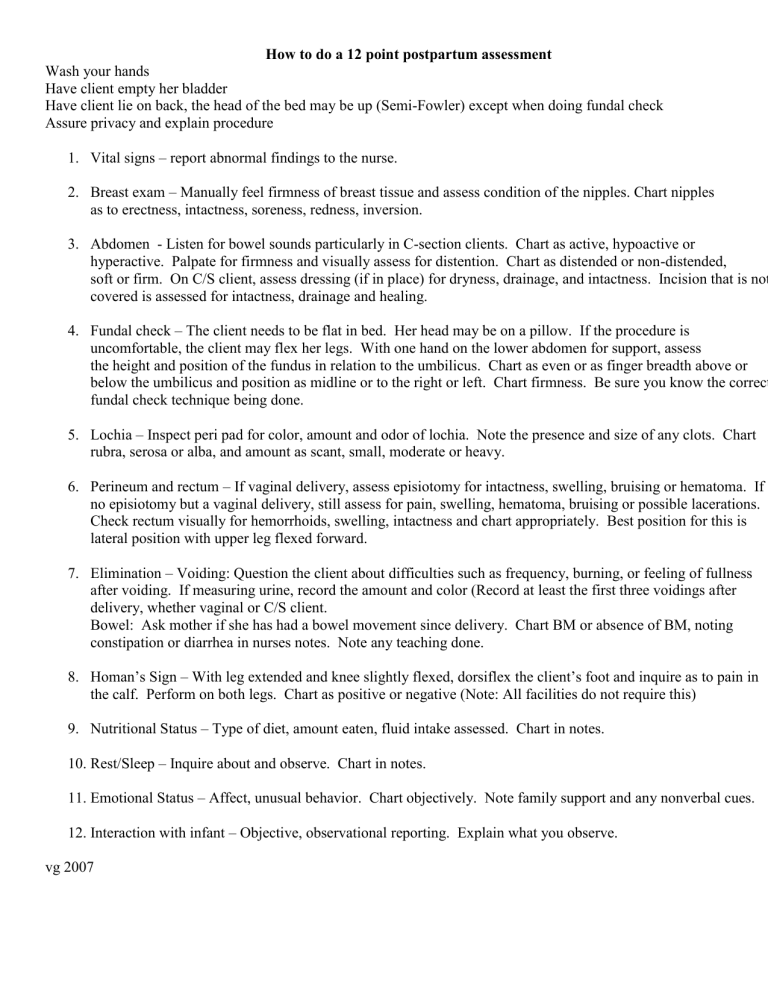
How to do a 12 point postpartum assessment Wash your hands Have client empty her bladder Have client lie on back, the head of the bed may be up (Semi-Fowler) except when doing fundal check Assure privacy and explain procedure 1. Vital signs – report abnormal findings to the nurse. 2. Breast exam – Manually feel firmness of breast tissue and assess condition of the nipples. Chart nipples as to erectness, intactness, soreness, redness, inversion. 3. Abdomen - Listen for bowel sounds particularly in C-section clients. Chart as active, hypoactive or hyperactive. Palpate for firmness and visually assess for distention. Chart as distended or non-distended, soft or firm. On C/S client, assess dressing (if in place) for dryness, drainage, and intactness. Incision that is not covered is assessed for intactness, drainage and healing. 4. Fundal check – The client needs to be flat in bed. Her head may be on a pillow. If the procedure is uncomfortable, the client may flex her legs. With one hand on the lower abdomen for support, assess the height and position of the fundus in relation to the umbilicus. Chart as even or as finger breadth above or below the umbilicus and position as midline or to the right or left. Chart firmness. Be sure you know the correct fundal check technique being done. 5. Lochia – Inspect peri pad for color, amount and odor of lochia. Note the presence and size of any clots. Chart rubra, serosa or alba, and amount as scant, small, moderate or heavy. 6. Perineum and rectum – If vaginal delivery, assess episiotomy for intactness, swelling, bruising or hematoma. If no episiotomy but a vaginal delivery, still assess for pain, swelling, hematoma, bruising or possible lacerations. Check rectum visually for hemorrhoids, swelling, intactness and chart appropriately. Best position for this is lateral position with upper leg flexed forward. 7. Elimination – Voiding: Question the client about difficulties such as frequency, burning, or feeling of fullness after voiding. If measuring urine, record the amount and color (Record at least the first three voidings after delivery, whether vaginal or C/S client. Bowel: Ask mother if she has had a bowel movement since delivery. Chart BM or absence of BM, noting constipation or diarrhea in nurses notes. Note any teaching done. 8. Homan’s Sign – With leg extended and knee slightly flexed, dorsiflex the client’s foot and inquire as to pain in the calf. Perform on both legs. Chart as positive or negative (Note: All facilities do not require this) 9. Nutritional Status – Type of diet, amount eaten, fluid intake assessed. Chart in notes. 10. Rest/Sleep – Inquire about and observe. Chart in notes. 11. Emotional Status – Affect, unusual behavior. Chart objectively. Note family support and any nonverbal cues. 12. Interaction with infant – Objective, observational reporting. Explain what you observe. vg 2007