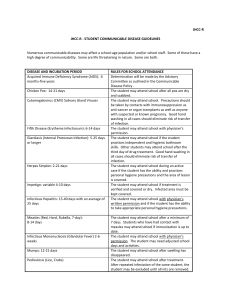
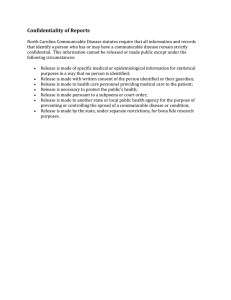
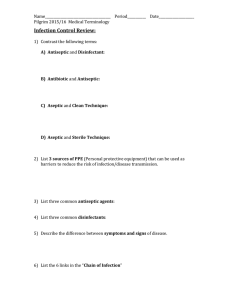
COMMUNICABLE DISEASE MODULE 1 DEFINITION OF COMMUNICABLE DISEASE At the end of the course the student will be able to understand: 1. The overview and purpose of the diagnostic procedure 2. The definition of communicable diseases, terminologies important in its process different 3. The types of communicable diseases, pattern of diseases, occurrence and immunity 4. Process of chain of infection, mode of transmissions 5. The different infection control measures 6. The isolation technique and the transmission based precautions 1 COMMUNICABLE DISEASE DEFINITION OF COMMUNICABLE DISEASE body by directly applying physical or chemical means. a. Concurrent disinfection b. Terminal disinfection COMMUNICABLE DISEASE NURSING AND ITS DIFFERENT TERMINOLOGIES ▪ Disease caused by an infectious agent from an infected individual and transmitted to a susceptible host either by direct/ indirect contact or through direct inoculation into a broken skin. ▪ HABITAT – is the place where an organism lives or where an organism is usually found. HOST – is a person, animal or plant on which a parasite depends for its survival. ISOLATION – is the separation from other persons of an individual suffering from a communicable disease. Is an illness caused by an infectious agent or its toxic product that are transmitted directly or indirectly to a well person through an agency, and a vector or an inanimate object. QUARANTINE – is the limitation of freedom of movement of persons or animals which have been exposed to CD/s for a period of that disease. COMMON TERMINOLOGIES INFECTION – is the implantation and successful replication of an organism in the tissue of the host resulting to signs and symptoms as well as immunologic response. RESERVOIR – is composed of one or more species of animal or plant in which an infectious agent lives and multiplies for survival and reproduces itself in such a manner that it can be transmitted to man. CARRIER – is an individual who harbors the organisms and is capable of transmitting it to a susceptible host without showing manifestations of the disease. SURVEILLANCE watching. – is the act of TYPES OF COMMUNICABLE DISEASE ▪ Infectious Disease – not easily transmitted by ordinary contact but require a direct inoculation through a break in the previously intact skin or mucous membrane. CONTACT – is any person or animal, or freshly soiled materials. DISINFECTION – is the destruction of pathogenic microorganism outside the 2 COMMUNICABLE DISEASE d. Some other factors ▪ Contagious Disease – easily spread and is directly transmitted from person to person SPORADIC - intermittent occurrence of a disease./ Occasionally and irregularly with no specific pattern. Why infections occur? Some bacteria develop resistance to antibiotics Some microbes such as influenza have so many different strains that a single vaccine cannot protect against all of them. Most viruses resist antiviral drugs New infectious agents occasionally arise such as HIV and Corona Viruses. ENDEMIC – continuous or constant occurrence of a disease in a certain area Some microbes localize in areas of the body that make treatment difficult EPIDEMIC –sudden increase in the number of cases of a disease in a short period of time/ occur in a greater number than what is expected in a specific area over a specific time. ASPECTS OF CARE OF PATIENTS WITH COMMUNICABLE DISEASE PATTERNS OF DISEASE/ INCIDENCE OF THE DISEASE A. PREVENTION 1. HEALTH EDUCATION Educate the family and the client with respect to: • Availability and importance of prophylactic immunization • Manner in which infectious illness is spread and methods of avoiding the spread • Importance of seeking medical advice for any sign of health problem • Importance of environmental cleanliness and personal hygiene • Means of preventing contamination of food and water supply 2. IMMUNIZATION – induction or introduction of specific protective antibodies in a susceptible person PANDEMIC -worldwide epidemic/ affects several countries or continents INFECTION AND THE ASPECTS OF CARE OF PATIENTS WITH COMMUNICABLE DISEASE What is infection? ❖ The production of microorganisms injures the patient by; 1. Competing with the host metabolism, 2. Cellular damage produced by the microbes, 3. Intracellular multiplication Severity of Infection ⚫ Varies with the; a. Disease producing ability b. Number of invading organism c. The strength of the host’s defense 3 COMMUNICABLE DISEASE • for the purpose of producing cellular immunity. • Expanded Program of Immunization (EPI) / Proclamation No. 6: Prevent the seven childhood diseases, TB, DPT, polio, measles, hepatitis B • U.N. goal: universal child immunization Proper supervision of food handlers B. CONTROL – LIMIT THE SPREAD OF INFECTION BY MEANS OF: 1. Isolation – separation of infected persons from other persons during the period of communicability in order to prevent the direct or indirect transmission of the infectious agent from infected persons to other person who are susceptible or who may spread the disease to others. Purpose of Isolation • Is to confine the infectious agent to a circumscribed area and to prevent the escape of infection from that area. IMMUNITY ▪ Immunity is the process of rendering an individual resistance or immunity to a specific disease. TYPES OF IMMUNITY 1. Natural Immunity: innate; inherent; inborn A. Natural * Natural Active: Through exposure or having disease itself *Natural Passive: Maternal antibodies received by the baby through placental transmission. 7 Categories Recommended In Isolation 1. Strict Isolation – to prevent highly contagious or virulent infections 2. Contact Isolation – to prevent the spread of infection primarily by close or direct contact. 3. Respiratory Isolation – to prevent transmission of infectious diseases over short distances through the air. 4. TB isolation – for TB patients with smear or with chest X-ray which strongly suggest active tuberculosis. 5. Enteric Isolation – is for infections with direct contact with feces 6. Drainage/Secretion Precaution – to prevent infections that are transmitted 2. Acquired Immunity B. Artificial * Artificial Active: Introduction of antigens that will stimulate the body to produce antibodies, e.g. live attenuated vaccine *Artificial Passive: Introduction of antibodies, e.g. Immunoglobulin 3. ENVIRONMENTAL SANITATION – P.D. 856 • Anti-littering: P.D. 825 4 COMMUNICABLE DISEASE by direct or indirect contact with purulent materials or drainage from an infected body site. Universal Precaution –is applied when handling blood and body fluids a. Applied to patients with HIV/HBC b. Intended to prevent parenteral, mucous membrane, and non-intact skin exposure of health care workers to bloodborne pathogens. c. The isolation is necessary to prevent infections that are transmitted by direct contact with infected blood or body fluids. d. This applied to blood, semen, vaginal secretions, and other body fluids,(CSF, synovial fluid, pleural fluid, peritoneal fluid, pericardial fluid, amniotic fluid), and tissues containing visible blood. 4. Disinfection – any physical or chemical process to destroy undesired animal forms present in the person, clothing or environment. • Concurrent – the application of disinfection as rapidly as possible after the discharge of infectious material from the body of an infected person or as after the soiling of articles with such infectious discharges. • Terminal – the process of rendering the personal clothing and immediate physical environment of the patient free from the possibility of conveying the infection to others at the time when the patient is no longer a source of infection. 5. Asepsis – the state or condition of being free from infection. A. CHAIN OF INFECTION 1. Describes the development of an infectious process 2. An interactive process involving an agent, host, and environment is required The six essential links (elements) in the chain of infection: 1. AGENT • An entity that is capable of causing disease. • Agents that cause disease may be as follows: 2. Quarantine – limitation of freedom of movement of persons or animals who have been exposed to a communicable disease for a period of time equal to the longest usual incubation period of the diseases so as to prevent effective contact with those who are not exposed. May either be complete or modified. 3. Fumigation – any process by which the killing of animal forms is accomplished with the use of gaseous agents. Biological Agents: Living organisms that invade the host, causing disease. a. Bacteria 5 COMMUNICABLE DISEASE • • May be harmful or beneficial d. Protozoa • Larger than bacteria • Absorb nutrients from the body of the host e. Rickettsia • Small, gram-negative bacterialike microbes that can induce life-threatening infections • Like viruses, they require a host cell for replication • Usually transmitted through a bite of arthropod carriers like lice, fleas, ticks as well as through waste products f. Spirochete • A bacterium with flexible, slender, undulating spiral rods that possess cell wall. • Three forms of spirochete that cause a disease: Treponema Leptospira Borilia g. Parasites • Live on or without other organisms • Live at the expenses of others • Don’t usually kill their host but take only the nutrients they need. Simple, one-celled microbes with double-celled membranes that protect them from harm • Produce rapidly and are considered the most common cause of fatal infectious disease • Classified according to: Shape (cocci, bacilli, spirillae) Need of oxygen (aerobic, anaerobic) Response of staining (grampositive or negative; acid fast or non-acid fast) Motility (motile, non-motile) Tendency to capsulate (encapsulated, capsulated) Capacity to form spores (spore-forming, non-sporeforming) b. Viruses • Smallest known microbes • Cannot replicate independently in the host’s cells; rather, they invade and stimulate the host’s cells to participate in the formation of additional viruses c. Fungi • Found almost everywhere on earth • Live in organic matter, soil, water, animals and plants • Can also live inside and outside the body 6 COMMUNICABLE DISEASE THE CHAIN OF INFECTION BIOLOGICAL AGENT Intact immune system Disinfection Exercise Cleaning Immunization Sterilization Proper nutrition SUSCEPTIBLE HOST RESERVOIR OR SOURCE Skin integrity Proper hygiene Sterile technique Change of dressing Proper disposal of needle or sharps Cleaning of equipment Sterilization PORTAL OF ENTRY TO HOST PORTAL OF EXIT FROM RESERVOIR Wearing of gloves masks gowns goggles (APPEs) Clean dressing over wounds Medical or surgical asepsis Covering mouth and nose when coughing or sneezing Proper disposal of contaminated object Hard hygiene MODE OF TRANSMISSION FIGURE 1.1 THE CHAIN OF INFECTION 7 COMMUNICABLE DISEASE Chemical agents. Substances that can interact with the body, causing disease, such as food additives, medications, pesticides, and industrial chemicals Contact Transmission This involves the transfer of an agent from an infected person through a fomite, or close contact with contaminated secretions. Sexually transmitted diseases are spread by direct contact. Common viral infections (cold, measles, and flu) are spread by close contact with contaminated secretions. ▪ Direct Contact – person to person ▪ Indirect Contact – inanimate objects or personal things ▪ Droplet Contact – contact with discharges from coughing, sneezing or talking with infected person Physical agents. Factors in the environment that are capable of causing disease, such as heat, light, noise, and radiation 2. RESERVOIR • A place or environment where the agent can survive and multiply • The most common reservoirs are: Humans Animals Physical environment Fomites 3. PORTAL OF EXIT • Route, path or way by which an infectious agent leaves the reservoir to be transferred to a susceptible host. • The agent leaves the reservoir through body secretions including: Sputum (from the respiratory tract) Semen, vaginal secretions, or urine (from the genitourinary tract) Saliva and feces (from the gastrointestinal tract) Blood Draining wounds Tears ▪ 4. MODES OF TRANSMISSION • The process of the infectious agent moving from the reservoir or source through the portal of exit to the portal of entry of the susceptible “new” host. Most infectious agents have a usual primary mode of transmission, but some microorganisms may be transmitted by more than one mode/depending on the agent. Almost anything in the environment can become a potential mode of transmission. HORIZONTAL TRANSMISSION Figure 1.2 Horizontal Transmission (Direct Contact) 8 COMMUNICABLE DISEASE DIRECT CONTACT Airborne Transmission ▪ Occurs when a susceptible host contacts droplet nuclei or dust particles that are suspended in the air. Contaminated droplets containing the measles virus are in the spray from sneezing. The droplet can find a portal of entry through the mucous membranes or conjunctiva. Droplets that do not remain airborne or settle out are excluded from this category. Figure 1.4 (Mosquitoes) Vectorborne Transmissions Vertical Transmission ▪ Refers to the mother-to-child transmission through the placental barrier or breastfeeding Figure 1.3 Airborne Transmission Vehicle Transmission ▪ Occurs when an agent is transferred to a susceptible host by contaminated inanimate objects such as water, food, milk, drugs, and blood. Cholera is transmitted through drinking water and salmonellosis is transmitted through contaminated meat. Figure 1.5 Verticaltransmissions through breastfeeding and placental barrier 5. Portal of Entry • The route by which an infectious agent enters the host Vectorborne Transmission ▪ Occurs when an agent is transferred to a susceptible host by animate means such as mosquitoes, fleas, ticks, lice, and other animals. Lyme disease, malaria, and West Nile virus are examples of diseases spread by vectors. 6. Host • A host is an organism that can be affected by an agent. • A human being is usually considered a host. • Susceptible host is a person who has no resistance to an agent and thus is 9 COMMUNICABLE DISEASE • vulnerable to disease. For example, an individual who has not received the measles vaccine is more likely to contract the infection because of the lack of immunity o the infectious agent. Compromised host is a person whose normal body defense is impaired and is therefore susceptible to infection. For example, a person with a common cold or superficial burns is at greater risk for infection because of the impaired state of the body system mechanisms. FIGURE 1.6 BREAKING THE CHAIN OF INFECTION 10 COMMUNICABLE DISEASE 1. Infection Defense Control: First Line of Hand hygiene is the first line of defense against infection and is the single most important practice in preventing the spread of infection. • Between Agent and Reservoir The first link in the chain of infection is between the agent and the reservoir. • Between Reservoir and Portal of Exit Promoting proper hygiene, changing dressings and linens, and ensuring that clean equipment is used in client care ways to break the chain of infection between the reservoir and the portal of exit The goal is to eliminate the reservoir for the microorganism before a pathogen can escape to a susceptible host. • Between Portal of Exit and Mode of Transmission The goal in breaking the chain of infection between the portal of exit and the mode of transmission is to prevent the exit of the infectious agents. Clean dressings must be maintained on all wounds. Clients should be encouraged to cover their mouths and noses when sneezing or coughing, and the nurse must do so as well. Gloves must be worn when caring for a client who may have infectious secretions, and care must be taken to properly 11 dispose of any contaminated article. • Between Mode of Transmission and Portal of Entry Asepsis must be ensured and barrier protection worn when the care of clients involves contact with the body secretions. Gloves, masks, gowns, and goggles are barrier protection that can be used. Proper hand hygiene and proper disposal of contaminated equipment and linens are ways to prevent transmission of microorganisms to other clients and health care workers. • Between Portal of Entry and Host Maintaining skin integrity and using sterile technique or client contacts are methods of breaking the chain of infection between portal of entry and host. Avoiding needle sticks by properly disposing of sharps also reduces the potential for infection by denying a portal of entry. The goal at this point in the chain is to prevent the transmission of infection to a client or health care worker who is not infected. • Between Host and Agent Breaking the chain of infection between host and agent means eliminating infection before it begins. There are many ways to reduce the risk of acquiring infection: COMMUNICABLE DISEASE Proper nutrition, exercise, and immunizations allow an individual to maintain an intact immune system, thus preventing infection. kind and contamination. • 2. Infection Control: Cleansing Cleansing is a potential hazard to the nurse from the splashing of contaminated material onto the body. Nurses should wear gloves, masks, and goggles during cleansing. • Disinfection is the elimination of pathogens, except spores, from inanimate objects. Disinfectants are chemical solutions used to clean inanimate objects. Common disinfectants are alcohol, sodium hypochlorite, quaternary ammonium, phenolic solutions, and glutaraldehyde. • A germicide is a chemical that can be applied to both animate (living) and inanimate objects to eliminate pathogens. Antiseptic preparations such as alcohol and silver sulfadiazine are germicides. • Sterilization is destroying all microorganisms including spores. Equipment that enters normally sterile tissue or blood vessels must be sterilized. Methods of achieving sterilization are moist heat (steam), dry heat, and ethylene oxide gas. The method of sterilization depends on the object to be sterilized and the 12 • amount of Autoclaving sterilization, which uses moist heat or steam, is the most common sterilization technique used in the hospital setting. Boiling water is not an effective sterilization measure, because some viruses and spores can survive boiling water. Objects that have been boiled in water for 15 to 20 minutes at 121ºC (249.8ºF) are considered clean but not sterile (Department of Labor, 1991) Promoting proper hygiene, changing dressings and linens, and ensuring that clean equipment is used in client care are ways to break the chain of infection between the reservoir and the portal of exit. The goal is to eliminate the reservoir for the microorganism before a pathogen can escape to a susceptible host. B. TYPES AND INFECTIONS STAGES OF 1. Types of Infections • Localized infections are limited to a defined area or single organ with symptoms that resemble inflammation (redness, tenderness, and swelling), such as a cold sore. • Systemic infections affect the entire body and involve multiple organs, such as AIDS. COMMUNICABLE DISEASE 2. Stages of Infection • Incubation Stage. The incubation period is the time between entry of infectious agent in the host and the onset of symptoms. During this time, the infectious agent invades the tissue and multiplies to produce an infection. The client is typically infectious to others during the latter part of this stage. For example, the incubation period for varicella (chicken pox) is 2 to 3 weeks. The infected person is contagious from 5 days before any skin eruptions to no more than 6 days after the skin eruptions appear. Safety • Always verify the incubation period of a suspected infection. Remember that a client may be able to transmit the infection to another person before the onset of symptoms. Prodromal Stage. The prodromal stage is the time from the onset of non-specific symptoms until specific symptoms begin to manifest. The infectious agent continues to invade and multiply in the host. A client may also be infectious to other persons during this time period. In the client with 13 chickenpox, a slight elevation in temperature will occur during this stage, followed within 24 hours by eruptions on the skin. • Illness Stage. The illness stage is the time when the client has specific signs and symptoms of an infectious process. The client with chickenpox will experience a further rise in temperature and continued outbreak of skin eruptions for at least 2 to 3 more days. • Convalescent Stage. From the beginning of the disappearance of acute symptoms until the client returns to the previous state of health. The client with chickenpox will see the skin eruptions and irritations begin to resolve during this stage. C. NOSOCOMIAL INFECTION A nosocomial infection is an infection acquired in a hospital or other health care facility that was not present or incubating at the time of the client’s admission. They also include those infections that become symptomatic after the client is discharged and infections passed among medical personnel. Nosocomial infections are COMMUNICABLE DISEASE also called hospital-acquired infections. These types of infections typically fall into four categories: urinary tract, surgical wounds, pneumonia, and septicemia. Most nosocomial infections are transmitted by health care personnel who fail to practice proper hand hygiene or who fail to change gloves between client contacts. The hospital environment provides exposure to a variety of organisms to which the client has not typically been exposed in the past. Therefore, the client has no resistance to these organisms, illness impairs the body defenses. STANDARD PRECAUTIONS FOR INFECTION CONTROL (Use for all clients) Wear Gloves Figure 1.8 Handwashing Wear gloves (clean, nonsterile adequate) whenever contact is expected with blood, body fluids, secretions, excretions, mucous membranes and non-intact skin and contaminated items. Wash hands before contact with each client, during care as needed (even if wearing gloves) to prevent cross contamination of body sites, and after touching blood, body fluids, secretions, excretions, and contaminated items (with or without gloves). Figure 1.7 Use a plan (non-antimicrobial) soap during routine handwashing: Use a antimicrobial agent or a waterless antiseptic agent as per agency policy. Always change gloves between clients and between tasks and procedures on the same client after contact with material that may contain a high concentration of microorganisms. Remove gloves promptly after use, before touching non-contaminated items and environment surfaces, and before going to another client, wash hands. 14 COMMUNICABLE DISEASE Face Protection (mask, goggles, face shield) Figure 1.9 Wear a face shield, or wear goggles and a mask thatcovers both the nose and the mouth during proceduresand client care activities that are likely to generate splashes or sprays of blood, body fluids, secretions or excretions to provide protection of the mucousmembranes of the eyes, nose and mouth. Wear Gown and other protective apparel Figure 1.10 Wear a gown to prevent contamination of clothing and skin from blood and body fluids exposures. Gowns especially treated to make them permeable to liquids and leg/shoe covers provide greater skin Patient-Care Equipment Figure 1.11 Handle used patient – care equipment soiled with blood, body fluids, secretions or excretions in a manner that prevents skin and mucous membrane exposures, contamination of clothing and transfer of microorganism, to other patients and environments. Ensure that reusable equipment is not used for the care of another patient until it has been appropriately cleaned and reprocessed and single use items are properly discarded. 15 protection when splashes or large quantities of ineffective material are present or anticipated. Remove soiled gown as soon as possible; wash hands to avoid transfer of microorganisms. COMMUNICABLE DISEASE Environmental Control Figure 1.12 Follow hospital procedures for routine care, cleaning, and disinfection of environment surfaces, beds, and bedrails, bedside equipment and other frequently touched surfaces. Linen Figure 1.13 Handle, transport, and process used linen soiled with blood, body fluids, secretions or excretions in a manner that prevents exposures and contamination of clothing and avoids transfer of microorganisms to other patients and environments designed for holding the 16 needle sheath. Never recap used needles using both hands and any other technique that involves directing the point of a needle toward any part of the body; rather, use either a one-handed “scoop” technique or a mechanical device assist in maintaining appropriate hygiene or environment control. Consult Infection Control if a private room is not available. Figure 1.14 Occupational Pathogens Health and Bloodborne Prevent injuries when using needles, scalpels and other sharp instruments or devices, when handling sharp instruments after procedures; when cleaning used instruments and when disposing of used needles. Handle, transport, and process used linen soiled with blood, body fluids, secretions or excretions in a manner that prevents exposures and contamination of clothing and avoids transfer of microorganisms to other patients and environments designed for holding the needle sheath. COMMUNICABLE DISEASE Figure 1.15 Figure 1.16 Use Resuscitation devices as in alternative to mouth-to-mouth resuscitation. Patient Placement 17 Use a private room for a patient who contaminates the environment or who does not (or cannot be expected to) COMMUNICABLE DISEASE Table 1.1 TRANSMISSION BASED PRECAUTIONS (use when indicated) Airborne Precautions Use when small (<5 um) pathogen-infected droplet nuclei may remain suspended in air over time and travel distances greater than 3 feet. Examples, varicella, measles, tuberculosis Droplets Precautions Observe standard precautions. Place client in private room or with another client having the same infection but not other infections (cohorting). If possible, use room equipped with negative pressure ventilation, outside venting, and 6-12 air exchanges per hour. Keep the door to the room closed. Wear a special approved particulate filter mask (N95) whenever entering room of all clients with tuberculosis or when staff or visitors not exposed to rubella or varicella must enter room. Limits visitors and caretakers to those already immune if chicken pox (varicella) or measles are involved. Keep client in room. Place surgical mask on client if transport is necessary. Follow additional agency guidelines. Observe standard precautions. Use with large (>5 um) pathogen-infected droplets that travel 3 feet or less via coughing, sneezing, etc. or during procedures (sunctioning) Place client in private room or with another client having the same infection, but no other infections (cohorting). Examples: hemophilis influenza, Neisseria meningitides, others Special ventilation is not necessary and the door may remain open. When private room or cohorting is unavailable, keep a distance of 3 feet or more between the infected client and other clients or visitors. Wear a mask when working within 3 feet of the client or entering the room according to agency policy. Limit the transport of the client from the room and then mask the client, if possible. Contact Precautions: Use with known or suspected microorganisms transmitted by direct hand-to-skin client contact or indirect contact with surfaces or care items in the environment. Examples: Clostridium difficile, diphtheria (cutaneous), herpes simplex (mucocutaneous or neonatal), impetigo, pediculosis, scabies, zoster (disseminated, immunocompromised host), (Ebola, Lassa, Marburg), others Additional recommendations for specific pathogens may also apply. Observe standard precautions. Place client in private room or use cohorting, consult agency infectious disease department as needed. Wear gloves when entering the room, change gloves after contact with infected material, remove gloves before leaving room and wash hands immediately with antimicrobial agent or waterless antiseptic agent, then ensure that hands do not touch potentially contaminated room surfaces or items. Wear a clean, non-sterile gown when entering room is clothing may have substantial contact with client, environmental surfaces or items, or if client is incontinent, or has diarrhea, ileostomy, colostomy or wound drainage not contained by a dressing. Remove gown before leaving the room, then ensure that clothing does not contact potentially contaminated environmental surfaces. Limit to essential purposes client transport from room. If transport is needed, maintain precautions to minimize the risk of pathogen transmission to other clients and environmental surfaces or equipment. When possible, dedicate the use of non-critical client-care equipment to a single client or cohort colonized with the same pathogen; if use of common equipment or items is unavoidable, adequately clean and disinfect them before use on another client. Additional recommendations for specific pathogens may also apply. 18 COMMUNICABLE DISEASE PRACTICE TO PASS: Answer the puzzle below: 19 COMMUNICABLE DISEASE MODULE 2 DISEASES AFFECTING GASTROINTESTINAL SYSTEM LEARNING OBJECTIVES At the end of the course the student will be able to understand: 1. The different communicable diseases occur, other names, and etiologic agents 2. The incubation period, period of communicability and transmission of different communicable diseases 3. The different diagnostic procedures, signs and symptoms and treatment 4. The process, prevention and control and management of every communicable diseases. 20 COMMUNICABLE DISEASE DISEASES AFFECTING GASTROINTESTINAL SYSTEM (Bacterial in Origin) TYPHOID FEVER A. AKA: Enteric Fever B. Causative agent – Salmonelia typhosa C. Incubation period between 7-14 days – usually Figure 2.1 Diagnostic Features of Typhoid Fever D. Period of communicability – for as long as the bacteria are in the stools G. Signs and symptoms 1. Prodromal stage – for 3-4 days 1.1. Dull headache; malaise 1.2. Chills; fever; body aches 1.3. Vomiting or diarrhea. 2. Fastigeal/pyrexial stage – during the second week 2.1. Exanthema rose spots – 4 to 5 peculiar rosecolored macules or meculopapules seen on the 7th to the 12th day on the abdomen and chest (in adult) or on the face (in infants) 2.2. Ladder-like fever 2.3. Enlarged spleen 2.4. Typhoid psychosis 2.4.1. Coma-vigil look – pupils dilate and patient appears to have blank stares or staring without seeing. 2.4.2. Difficulty putting out the tongue. E. Mode of transmission – by food and water contaminated by stools and urine of patients or carriers. The vehicles are the 5 Fs: 1. Feces 2. Food 3. Flies 4. Fomites 5. Fingers F. Diagnostic/laboratory exams 1. Blood culture – during the prodromal stage Widal Test to determine the antigen left by the microorganism • Antigen O – presently infected • Antigen H – has been exposed before or has received toxin • Typhidot 2. Urine culture 3. Stool culture 21 COMMUNICABLE DISEASE 2.4.3. Carphologia – involuntary and aimless picking of linen 2.4.4. Subsultus tendinum – involuntary twitching of the tendon of the wrists. 2.4.5. Constant tendency to slip down toward the foot of the bed. 1.2. Vivotif 1.2.1. Capsule form 1.2.2. Given 1 hour before meal every other day for 3 doses 1.2.3. 3 years immunity 2. Control 2.1. Proper handwashing; clean environment 2.2. Boil drinking water 2.3. Avoid street foods and improperly washed or improperly cooked food 3. Deferenscence stage – 3rd week Intestinal hemorrhage – microorganism produces ulcers in the intestine Intestinal perforation – spillage of fecal material in the peritoneum, causing peritonitis Cough and hypostatic congestion of the lungs; pneumonia Leukopenia 3. Treatment 3.1. Medical care – the drug of choice is Chloromycetin 3.2. Nursing care 3.2.1. Regulation of the diet 3.2.2. Regulation of dehydration 3.2.3. hygiene and control TETANUS • Important information ▪ Infectious but not contagious ▪ Brought about by direct inoculation of material containing the causative agent ▪ Always a serious disease 4. Lysis/convalescence stage – although signs and symptoms subsides, patient should still be observed for relapses which could be fatal. H. Management 1. Prevention 1.1. Immunization – CDT (Cholera, Dysentery, Typhoid) 1.1.1. Given IM at the deltoid 1.1.2. Children – 0.25 ml, Adults – 0.5 ml 1.1.3. 6 months immunity • • 22 AKA: lockjaw Causative agent: clostridium tetani ▪ A common inhabitant of the soil specially if fertilized with manure ▪ Long, slender, gram-positive bacillus COMMUNICABLE DISEASE ▪ ▪ ▪ ▪ • Forms spores which are extremely resistant to heat and ordinary antiseptics Extremely anaerobic (does not grow in the presence of free oxygen) Multiplies only at the site of the wound Produces its deadly effect by releasing a true soluble toxin (tetanospasmin) which reaches the brain and spinal cord and responsible for muscle spasm • Predisposing factors ▪ Newborns whose method of delivery and umbilical cord care are not aseptic ▪ Following surgeries, infected wounds ▪ Women are poorer risks than men, so are the very young and the very old. • Incubation Period ▪ Commonly 5-10 days but may vary from 2 days to several weeks or longer, depending on the extent, location and characteristics of the wound. ▪ A short incubation period gives a bad prognosis ▪ The longer the incubation the greater the probability of recovery • Mode of Transmission ▪ Normally mode of transmission is through punctured wound that is contaminated by dust, soil, or animal excreta containing C. tentani • Rugged traumatic wounds and burns • • • 23 Umbilical stump in newborn especially for babies delivered at home with faulty cord dressing; babies delivered to mothers without tetanus toxoid immunization Unrecognized wounds (cleaning of the ears with sharp materials) Dental extraction, circumcision, ear piercing Signs and Symptoms ▪ Stiffness in the neck, jaw muscles (trismus), abdomen or limbs which either rapidly or gradually increases until the jaws are locked (trismus) and cannot be opened. Masseter muscle is dominant. ▪ The lips protrude and the corners of the mouth are drawn out of shape, giving rise to rise to the sardonic grin (risus sardonicus). Heightened by simultaneous elevation of the eyebrows and wrinkling of the forehead, the eyes remain partially closed ▪ The head retract, other muscles of the body become spastic, the back become bowed and the stiffened patient rests on his head and heels (opisthotonos) ▪ Slightest stimulation of the patient causes frightful convulsions and causes unbearable pain. Voluntary movements are not possible. Convulsion last from a few to COMMUNICABLE DISEASE an almost continuous seizure during the 24-hour period Types of Stimuli 1. Exteroceptives – outside the patient, bright lights, loud noise 2. Interoceptives – from the patient himself’ flatus 3. Proprioceptives – touching the patient, jamming the bed, turning the patient • Low grade fever, profuse sweating • Difficulty in breathing and swallowing • Difficulty in breathing and swallowing • Cyanosis • Urinary retention and Constipation should be wrapped in paper and burned ASAP) c. Terminal disinfection (walls and furniture washed with soap and water , room thoroughly aired mattress and pillows autoclave or aired/sunned for 6-8 hours Treatment MEDICAL CARE 1. ATS, (ANST), 2. TAT 0.01 ml Neutralizes the toxin 3. and 0.09 ml NSS 4. Epinephrine or steroid to counteract anaphylaxis 5. Antibiotics – Penicillin , destroy the microorganism 6. Prevent and control spasm a. muscle relaxants – methocarbamol (Robaxin, Robaxisal) Baclofen b. Sedatives –Valium (diazepam) c. Tranguilizers – Thorazine 7. Tracheostomy, if needed MANAGEMENT 1. Prevention a. Active Immunization with tetanus toxoid – DPT 6 weeks after birth, 0.5ml for 3 doses –(46 weeks interval) b. Tetanus toxoid for non-pregnant women ▪ 1st dose given anytime – 0.5ml ▪ 2nd dose after one month ▪ 3rd dose after 6 months ▪ 4th dose after 1 year ▪ 5th dose after another year c. Antitoxin – is used for the treatment of clinical tetanus and for passive immunization or prophylaxis in recently wounded individuals never previously immunized with tetanus toxoid. NURSING CARE 1. Patient should be in a quiet, darkened, well ventilated and nonstimulating environment 2. Minimal gentle handling of patientproper scheduling of nursing care activities so as not to disturb patient very often, daily cleansing bath with warm water, change position, oral hygiene 3. Liquid diet of 3000-4000 calories via tube feedings if indicated 4. Prevent injury a. do not leave the patient alone b. siderails of the bed always raised c. padded tongue blades or metal spoon to guard against respiratory obstruction 5. Proper wound care – wash with flowing water, then rinse with antiseptic solution and cover with thin dressing. 2. Control a. Medical aseptic technique b. Concurrent (All materials contaminated with secretions 24 COMMUNICABLE DISEASE Figure 3.1 Manifestations of Tetanus Hookworm Disease Etiologic Agent • ⚫ Ancylostomiasis, Miner’s Disease, Egyptian Chlorosis ⚫ An intestinal parasite of humans that usually causes diarrhea or cramps. Occurs mostly in tropical and subtropical countries Cyclostome duodenale – prevalent in Europe and Asia • Necator americanus – Central and South America and West Africa o Both are pathogenic to man o Source of infection is the soil contaminated with feces o Female hookworm – 10,000 to 20,000 eggs 25 COMMUNICABLE DISEASE • • o Eggs in moist and oxygen-rich soil will develop into embryos within 24-72 hrs. o Larvae take about 6 weeks to develop into a mature larvae that can cause human infection. o It remains alive in the soil for several weeks under favorable condition. Diagnostics • Microscopic exam of feces for the eggs • Blood exam reveals eosinophilia • Treatment Modalities: o Pyrantel embonate (Quantrel) o Tetrachloroethylene o Carbon tetrachloride Incubation Period o Hookworm ova appear in the stool about 4-6 weeks after the larvae penetrate the skin o 40-100 days or 2-8 weeks • Period of Communicability o Person remains spreaders of infection as long as they remain infected Nursing Management • • Mode of Transmission • • Directly through the skin of the foot (ground itch) • Ingestion of contaminated drinking water and food • Incidence: o Most important helminth infection of man • All persons are susceptible • 15-25 years of age (common) • Tropical and subtropical countries (common) • • • • • • • Clinical Manifestations • • • • • • • • Perverted appetite Pedal edema and edema in other portions of the body maybe present • Small lesion of the intestinal mucosa Iron deficiency anemia Abdominal pain, diarrhea, allergic reactions like urticaria Mentally and physically underdeveloped (children) Protruding abdomens and lethargic (child) Malnourished and undernourished (child) Lazy, have no energy, lack ambition (child) Pupils are dilated Isolation not necessary Diet high in calories, vitamins, and minerals Personal hygiene should be maintained Prevention: Health education Prevent pollution of streams and lakes with human excreta In endemic areas, avoid walking barefoot Good hygiene is important Animals should not be allowed to defecate on the streets or beaches where most people likely linger Purified or boiled water must be used for drinking Vegetables should not be eaten raw Hydatid Disease • 26 Cystic echinocccosis (CE), also known as hydatid disease, is caused by infection with the larval stage of Echinococcus granulosus, a ~2-7 millimeter long tapeworm found in dogs (definitive host) and sheep, cattle, goats, and pigs (intermediate hosts). Although most infections in humans are asymptomatic, CE COMMUNICABLE DISEASE causes harmful, slowly enlarging cysts in the liver, lungs, and other organs that often grow unnoticed and neglected for years. Prevention • Mode of Transmission • • • • Humans can be exposed to these eggs by "hand-to-mouth" transfer or contamination. o By ingesting food, water or soil contaminated with stool from infected dogs. o By petting or handling dogs infected with the Echinococcus granulosus tapeworm. These dogs may shed the tapeworm eggs in their stool, and their fur may be contaminated. • • • Prevent dogs from feeding on the carcasses of infected sheep. Control stray dog populations. Restrict home slaughter of sheep and other livestock. Do not consume any food or water that may have been contaminated by fecal matter from dogs. Wash your hands with soap and warm water after handling dogs, and before handling food. Teach children the importance of washing hands to prevent infection. Leptospirosis is a bacterial disease that affects both humans and animals. Humans become infected through direct contact with the urine of infected animals or with a urine-contaminated environment. The bacteria enter the body through cuts or abrasions on the skin, or through the mucous membranes of the mouth, nose and eyes. Person-to-person transmission is rare. Risk factors for human infection include uncontrolled dogs living closely with people, uncontrolled slaughter of livestock, and unsanitary living conditions. Clinical Manifestations • Pain or discomfort in the upper abdominal region or chest, nausea, vomiting, or coughing may occur as a result of the growing cysts. Rupture of cyst fluid can lead to allergic reactions or even death. In the early stages of the disease, symptoms include high fever, severe headache, muscle pain, chills, redness of the eyes, abdominal pain, jaundice, hemorrhages’ in the skin and mucous membranes, vomiting, diarrhea, and rash. Diagnostics • • • o o X-rays or MRI scans Blood tests Treatment: Surgical removal of the cyst modified surgical procedure (aspiration) o Medication Synonyms o Weil’s Disease, Canicola Fever, Hemorrhagic Jaundice, Mud Fever, Swine Herd Disease 27 COMMUNICABLE DISEASE During pregnancy, leptospirosis can affect the fetus. Anyone who has the infection during pregnancy will need to spend time in the hospital for monitoring. Symptoms The signs and symptoms of leptospirosis usually appear suddenly, about 5 to 14 days after infection. However, the incubation period can range from 2 to 30 days, according to the CDC. Mild leptospirosis Signs and symptoms of mild leptospirosis include: o o o o o For mild cases, the doctor may prescribe antibiotics, such as doxycycline or penicillin. o o o o Patients with severe leptospirosis will need to spend time in the hospital. They will receive antibiotics intravenously. Depending on which organs leptospirosis affects, the individual may need a ventilator to help them breathe. a fever and chills coughing diarrhea, vomiting, or both headache muscle pain, particularly lower back and calves a rash red and irritated eyes jaundice Most people recover within a week without treatment, but around 10 percent go on to develop severe leptospirosis. Severe leptospirosis If it affects the kidneys, dialysis may be necessary. Signs and symptoms of severe leptospirosis will appear a few days after mild leptospirosis symptoms have disappeared. Intravenous fluids can provide hydration and essential nutrients. Symptoms depend on which vital organs are involved. It can lead to kidney or liver failure, respiratory distress, and meningitis. These can be fatal. Hospital stays may range from a few weeks to several months. This mostly depends on how the patient responds to antibiotic treatment, and how severely the infection damages their organs. The heart, liver, and kidneys 28 COMMUNICABLE DISEASE If leptospirosis affects the heart, liver, and kidneys, the person will experience: The lungs If it affects the lungs, the person cannot breathe. o o o o o o o o o o o fatigue irregular, often fast, heartbeat muscle pains nausea nosebleeds pain in the chest panting poor appetite swelling of the hands, feet, or ankles unexplained weight loss jaundice, seen in a yellowing of the whites of the eyes, tongue, and skin o Without treatment, this can lead to life-threatening kidney failure. Signs and symptoms include: o o o o high fever panting coughing up blood In severe cases, there may be so much blood that the person suffocates. Diagnosis Early-stage, mild leptospirosis is hard to diagnose, because the symptoms can resemble those of flu and other common infections. The brain If it affects the brain or spinal cord, meningitis, encephalitis, or both may develop. If a physician suspects severe leptospirosis, the patient may undergo specific diagnostic tests. Various tests are available. In some cases, tests may need repeating to confirm the result. Meningitis is an infection of the membrane covering the brain and spinal cord, while encephalitis refers to infection of brain tissue. Both conditions have similar signs and symptoms. The doctor will ask about any recent travel, especially to areas where leptospirosis is common. These may include: They may ask if the person: confusion or disorientation drowsiness fits or seizures high fever nausea photophobia, or sensitivity to light problems with physical movements stiff neck inability to speak vomiting aggressive or unusual behavior Untreated meningitis or encephalitis can result in serious brain damage, and it may be life-threatening. has been swimming in a lake, pond, canal, or river has had contact with any activities that occurred in a slaughterhouse, on a farm, or relating to animal care may have had contact with animal urine or blood A number of blood and urine tests can confirm or rule out leptospirosis. 29 COMMUNICABLE DISEASE In the United States, leptospirosis is a notifiable disease. The doctor must inform the relevant health authorities if a person’s diagnosis confirms an infection. Types There are leptospirosis. 2. Victims who survive the first 12 hours after ingestion have a greater chance of survival B. AKA: Red Tide two main types of Mild leptospirosis: This accounts for 90 percent of cases. Symptoms include muscle pain, chills, and possibly a headache. Severe leptospirosis: Between 5 and 15 percent of cases can progress to severe leptospirosis. Organ failure, internal haemorrhaging, and death can result if the bacterium infects the liver, kidneys, and other major organs. The Centers for Disease Control and Prevention (CDC) puts the fatality rate between 5 and 15 percent among those with severe illness. With effective and timely treatment, leptospirosis is less likely to become severe. Figure 2.3 Poisoning Paralytic Shellfish C. Causative agent – single celled dinoflagellates, specifically Pyromidium bahamenvar compressum 1. There are 2000 varieties, 30 of which become poisonous after heavy rainfall preceded by prolonged summer 2. Commonly called planktons 3. Toxins are not totally destroyed by cooking Those more likely to develop severe leptospirosis tend to be those who are already sick, for example, with pneumonia, those under the age of 5 years, and those in older age. PARALYTIC SHELLFISH POISONING A. Important Information 1. A syndrome of characteristics symptoms predominantly neurologic which occur within minutes or several hours after ingestion of poisonous shellfish D. Incubation period – 30 minutes to several hours after ingestion of 30 COMMUNICABLE DISEASE poisonous shellfish talaba, halaan, etc.) (tahong, 3. More common and more severe in children than in adults E. Mode of transmission – Ingestion of raw or inadequately cooked seafood: specially bivalve shellfish or mollusk during red tide season B. AKA 1. Bacillary – Shigellosis, Bloody Flux 2. Cholera – El Tor 3. Amoebic – Amoebiasis F. Signs and Symptoms 1. Numbness of the face specially around the mouth 2. Dizziness, floating sensation, weakness 3. Headache; rapid pulse; vomiting 4. Difficulty of speech (ataxia) and difficulty of swallowing (dysphagia) 5. Tingling sensation, paresthesia and eventual paralysis of the hands and feet C. Causative agent – gramnegative, nonsporulating, nonmotile bacteria 1. Bacillary – shigella Dysenteriae; Flexnar; Boyclii; Sonne 2. Cholera – Vibrio comma; Ogawa; Inaba; El Tor 3. Amebic – Entamoeba histolytica D. Incubation period – 4-7 days E. Period of communicability – during acute infection and until the infectious agent is no longer present in the stools, usually within 4 weeks after illness G. Management 1. Induce vomiting 2. To weaken the effect of toxic effect of Red tide, give coconut milk and sodium bicarbonate solution during the early stage. If given the last stage the condition will get worst. F. Mode of transmission – by direct or indirect fecal-oral transmission from a patient or carrier DYSENTERY/ CHOLERA G. Diagnostic/laboratory exams 1. Stool exam – fresh stool within 30 minutes to one hour should be examined for the presence of trophozoites 2. Rectal swab A. Important Information 1. Protozoa in origin 2. Name used in connection with various-intestinal disturbances with such common symptoms as severe abdominal pain (griping), tenesmus and frequent mucoid or bloody stools. H. Signs and symptoms 1. Bacillary 1.1 Ushered by chills followed by fever 31 COMMUNICABLE DISEASE 1.2 Nausea, vomiting, tenesmus (constant bearing down sensation in the rectum as though the bowels must move; yet when thay do, no relief is left) 1.3 Severe diarrhea at first mucoid and later bloody, alternating with constipation 1.4 Bowek movements may be 30-40 times or more in 24 hours 1.5 Extreme thirst and rapid dehydration 2. Cholera 2.1. Starts with acute colicky pains in the abdomen, accompanied by mild diarrhea in which stools are at first yellowish becoming grayish-white (“ricewatery”). Use of water bed is necessary because bowel movements are very frequent 2.2. Marked mental depression, headache, vomiting, fever may or may not be present 2.3 Extreme thirst, thickly furred tongue, severe or violent cramps in the legs and feet 2.4. Face appears shriveled, eyes sunken and the skin an ash-gray color 2.5. Washerwoman’s hands – because of rapid dehydration Figure 2.4 Cholera Control 3. Amoebic 3.1 Primary or intestinal 3.1.1. Vomiting, tenesmus, severe abdominal cramps 3.1.2. Diarrhea alternating with constipation; stools are mucopurulent, foulsmelling and with bloody streaks 3.2 Secondary – incident to the migration of amoeba to other organs, usually the liver (hepatitis) and the brain 32 COMMUNICABLE DISEASE I. Medical Management – basically IV therapy 1. Bacillary and Cholera – antibiotics 2. Amoebic – antiprotozoan agent, e.g. Araien 2.2. Causative agent – DNAcontaining virus 2.3. Mode of transmission – blood and other body fluids; percutaneous/inoculation 2.3.1 Use of contaminated needles 2.3.2 Blood transfusion 2.3.3 Oral-oral transmission 2.3.4 Sexual transmission 2.3.5 Vertical / transplacental transmission 2.4 Predisposing factors 2.4.1 Health workers 2.4.2 Blood recipients 2.4.3 Drug addicts 2.4.4 Promiscuous individual/multiple sex partners 2.5 Incubation period – 6 weeks to 6 months HEPATITIS A. Causative agents 1. Microorganisms – bacteria, viruses, protozoa, spirochetes 2. Too much alcohol 3. Drug intoxication 4. Chemical intoxication B. Types 1. Hepatitis A 1.1 Synonyms: Infectious hepatitis; Catarrhal hepatitis; Epidemic Hepatitis 1.2 Causative agent – RNAcontaining virus 1.3 Mode of transmission – food and water contaminated with feces and saliva of patient with Hepatitis A 1.3.1 Fecal-oral 1.3.2 Oral-oral 1.4 Predisposing factor 1.4.1 Food handlers 1.4.2 Unsanitary living conditions 1.4.3 Oral-anal sex 3. Hepatitis C 3.1 AKA: Past-transfusion hepatitis 3.2 Causative agent – Hepatitis C virus 3.3 Mode of transmission – percutaneous, particularly blood transfusion 3.4 Predisposing factors 3.4.1 Paramedical team 3.4.2 Blood recipients 3.5 Incubation Period – 2 weeks to 6 months 1.5 Incubation period 2 – 7 weeks 2. Hepatitis B – most fatal 2.1. AKA: Serum hepatitis; Homologous hepatitis; Viral hepatitis 4. Hepatitis D 4.1. Dormant type of hepatitis 4.2. Can be acquired only if with Hepatitis B 33 COMMUNICABLE DISEASE 4.3. Same mode of transmission, predisposing factors and incubation period as Hepatitis B Post-icteric stage ▪ Signs and symptoms subside ▪ Takes 3-4 months for the liver to regenerate 5. Hepatitis E Important information – if hepatitis recons at age 2030, it can lead to cancer of the liver AKA: Enteric hepatitis Causative agent – Hepatitis E virus Mode of transmission – fecal-oral Predisposing factors and incubation – same as Hepatitis Manifestation/Signs Symptoms C. Diagnostic/laboratory exams 1. Liver Functions Test. Liver Enzyme Test – to determine the extent of liver damage 1.1 Alanine Amino Transferase (ALT) – 1st to increase when there is liver damage 1.2 Aspartate Amino Tranferase (AST) – SGOT 1.3 Alkaline Phosphatase (ALP) and 2. Serum Antigen Antibody Test – for hepatitis 2.1 HasAg-surface AntiHAV 2.1.1 IgG 2.1.2 IgM 2.2 HbsAg-surface AntiHBs 2.3 HbeAg-Protein Independent AntiHBe 2.4 HbcAg-Care Independent AntiHBc 2.5 HcsAg-Surface Independent AntiHCs Pre-icteric stage ▪ Fever, body malaise (due to irritability of the liver to convert glucose to glycogen) ▪ Weight loss ▪ Anorexia and vomiting (due to inability of the liver to deaminase protein) ▪ Right upper quadrant pain (due to infiltration and liver inflammation) ▪ Anemia (due to decreased life span of RBCs – normal life span of RBCs is 120 days) 3. Ultrasound 4. Liver biopsy 5. Urinalysis Icteric stage ▪ Jaundice – due to excessive bilirubin in the blood ▪ Pruritus (itchiness) – due to bile salts in the sweat ▪ Tea-colored urine – due to excess bilirubin in the kidneys ▪ Acholic (gray-colored) stools ▪ Hepatomegaly D. Management 1. Prevention ▪ Immunization for Hepatitis A and B ▪ Monogamy 34 COMMUNICABLE DISEASE 2. Control ▪ avoid mode of transmission ▪ handwashing ▪ standard precaution PINWORM-INFESTATION 3. Nursing care 3.1 Complete bed rest – to facilitate liver regeneration 3.2 Diet – to promote tissue repair 3.2.1 decrease fat, carbohydrates increases (CHO), protein (CHON) – if with simple hepatitis 3.2.2 decrease fat, increase CHO, decrease CHON – if with severe hepatitis Figure 2.6 Viral Hepatitis Overview 35 ▪ Important Information An intestinal roundworm which infects only man. If found in one family member, there are most probably infected also ▪ AKA : Nocturnal Ani; Enterobiasis, Oxyurasis, seatworm or threadworm ▪ Causative agent – Enterobius vermicularis, (a nematode) 1. Lives and breads in the small intestine. 2. When eggs are swallowed, they hatch in the stomach and small intestine. 3. Gravid worms migrate during the night down the rectum and even the perianal area to lay their eggs, causing severe itching. 4. May enter the vagina and into the peritoneal cavity. 5. Eggs are infective within a few hours after leaving the GIT. 6. Eggs are easily blown around by mild breezes and are very infectious. 7. Eggs are not destroyed by ordinary laundering. ▪ Incubation period – the life cycle of the worm requires 2-6 weeks to be completed. ▪ Period of communicability – as long as gravid females are discharging eggs on the perineal skin. COMMUNICABLE DISEASE ▪ Mode of transmission – direct transfer of infective eggs by hand from anus to mouth of the same or another person, or indirectly through contaminated clothing, linen, food, etc. Dustborne infection is also possible. ASCARIASIS ▪ Important information A chronic condition often producing no symptoms. More prevalent in tropical countries like the Philippines ▪ Causative agent – Ascaris lumbricoides A large roundworm Eggs hatch in the intestinal canal and release larva → intestinal wall → lymphatic and circulatory systems → lungs → bronchioles → bronchi → pharynx → back to the small intestines where they mature. Female produces around 20,000 eggs/day. Figure 2.8 Pinworm Cycle ▪ Diagnostic exam – Test tape ➢ Best done upon waking up in the morning before bathing or bowel movement. ➢ Scotch tape placed against the anus and then examined microscopically for eggs. ▪ Management ▪ Handwashing ▪ Wear well-fitting underwear ▪ all members of the household should be treated with Piperazine hexahydrate (500 mg/tsp) for 1 week ➢ ½ tsp OO for children ➢ tsps BID for adults ▪ 36 Figure 2.9 Ascariasis Incubation period – reach maturity about 2 months after ingestion COMMUNICABLE DISEASE ▪ Period of communicability – as long as mature gravid worms are in the intestines. ▪ Signs and symptoms – seen only when with heavy infestation - Abdominal pain; marked disturbances of digestion - Insomnia; restlessness Sequela – destruction of the bowel when there is a bolus of worms ▪ ▪ 2. Small filterable virus introduced through the oropharynx and which leaves the body via discharges from the throat and the gastrointestinal tract (virus found in +stools 2 weeks before appearance of symptoms 3. May exist in contaminated water supplies and sewage or infected milk 4. Can survive in body secretions at ordinary temperature outside the body for long periods. 5. Multiplies in the tonsils an Peyer’s Management – anthelminthics e.g., Antiox POLIOMYELITIS ▪ Disease of the lower motor neuron involving the anterior horn cells, characterized by changes in the CNS ▪ An acute paralytic condition which is very contagious and infectious. ▪ Characterize by changes in the central nervous system ▪ Disease of the lower motor neuron involving the anterior horn cells ▪ No patient dies except if respiration is affected by involvement of the spinal cord. No matter how severely paralyzed, if respiration is not involved the prognosis is good. patches before it enters the blood stream Figure 2.10 Poliomyelitis Predisposing Factors 1. children below 10 years old 2. male more often affected 3. poor environmental and hygienic conditions – flies may act as mechanical vectors Synonym: Infantile paralysis, Heine medin disease Causative Agents: Legio debilitants Characteristics: 1. Three stains: Brunhilde (provides permanent immunity) Lansing and Leon (give temporary immunity) Incubation Period: usually 12 days, may vary from 7-21 days 37 COMMUNICABLE DISEASE Signs and Symptoms 1. Abortive stage – headache sore throat, slight or moderate, occasional vomiting 2. Preparalytic stage – signs of infection a. tightness/spasm of the back muscle and hamstrings b. stiff neck c. paresthesias d. Hoynes signs – in supine lift patient shoulder, if head drops abnornal e. Pofer sign – opisthotonos with head refraction Mode of Transmission 1. droplet infection – in early infection 2. body secretions – nasopharyngeal 3. fecal-oral –during late stage Diagnostic /Laboratory Exams 1. Lumbar tap –(+) Pandy test (increased protein in CSF) 2. Muscle wasting 3. Stool exam – 10 days after being infested (late stage) 3. Paralytic Stage –classified according to the site involved and the resulting clinical picture a. actual paralysis is commonly the first presenting sign b. persistent headache c. biphasic pattern 1. first phase is similar to signs of the abortive type, then a few days of remission of symptoms wherein patient appears to have recovered 2. Second phase starts when patient develops weakness or paralysis, which appears more often on the 2nd day and then reaches its maximum by the 6th day. a. Constipation; vomiting b. Irritability, lethargy c. Pinched, poison affording maximum comfort to painful muscle is diagnostic d. Profuse sweating usually over areas in which the muscles are involved e. Changing deep tendon reflexes, hyperactive at the start and then diminution or loss. Pathophysiology Legio debilitants Children below 10 years of age Droplets Nasopharyngeal secretions Abortive Stage Multiplies in tonsils and Payer’s patches Sore throat Fever, headache, body malaise Anorexia, abdominal pain, nausea and vomiting Low lumbar pains Diarrhea/constipation Lymphatic system Prepalytic Stage Blood stream Muscle tightness/spasm Stiffneck Paresthesia Hoyne sign Pover sign CNS Paralytic stage (Flabby, flaccid and soft muscle) 1. bulbar 2. spinal 3. bulbospinal Figure 2.11 Pathophysiology of Poliomyelitis 38 COMMUNICABLE DISEASE Management Prevention ▪ Passive Immunization – gamma globulin IM may protect a person who has had intimate contact with a fresh case of active poliomyelitis for 2-3 weeks ▪ Active immunization – oral polio vaccine (Sabin), 2-3 drops p. o. 4-6 weeks after birth for 3 doses (infant should not be fed for at least 30 minutes after to promote absorption of the vaccine) Control ▪ Aseptic techniques and avoiding infected discharges Treatment: generally symptomatic and supportive ▪ Medical care ➢ Iron lung machine – if with respiratory paralysis ➢ Tracheostomy if necessary ➢ Physiotherapy Nursing Care ▪ Comfort and hygiene measures ➢ Do not touch or massage painful areas ➢ Apply warm packs to relieve muscle shortening, pain and tenderness ▪ Diet – bland, high protein ▪ Tracheostomy care Types of paralysis a. bulbar – cranial nerve are affected b. spinal – anterior horn cells are affected, causing paralysis of the affected extremities c. bulbospinal – combination of both Figure 2.12 Muscles Commonly weakened by Polio 39 COMMUNICABLE DISEASE PRACTICE TO PASS: Answer the puzzle below, refer to the next page for the questions/items: 40 COMMUNICABLE DISEASE PRACTICE TO PASS: Questions/Items for puzzle on page 57 41 COMMUNICABLE DISEASE PRACTICE QUESTIONS: Situation: Malaria is said to be endemic in Tropical countries 1. A client is concerned about contracting malaria while visiting relatives in Palawan. The nurse explains that the best way to prevent malaria is to avoid; A. Mosquito bites B. Untreated water C. Undercooked food D. Over-populated areas B. inhaling cocaine C. sharing food utensils with an HIV positive person without proper cleansing of the utensils D. having sexual intercourse with a HIV positive person without using a condom 5. A client with HIV is taking Zidovodine (AZT). AZT is the drug that acts to; A. destroys the virus B. enhance the body’s antibody production C. slow replication of the virus D. neutralizes the toxins produces by the virus 2. When teaching a client about drug therapy against plasmodium falcifarum, the nurse should indicate the fact that; A. The infection are controlled B. Immunity will prevent immunization C. The infection can generally be eliminated D. Transmission by the anophelies mosquito can occur 6. The nurse is instructing a group about food preparation. They are told to avoid using products in damaged cans because they might contain the anaerobic spore-forming rod; A. Escheria coli B. Clostridium tetani C. Salmonella typhosa D. Clostridium botulism 7. When caring for a client with Hepatitis A the nurse should take special precautions to; A. prevent droplet spread of infection B. use caution when bringing food to the client C. use gloves when removing the client’s bedpan D. wear mask and gown before entering the client’s room 3. When caring for a client who is HIV positive, the primary responsibility of the nurse is to explain how the client can prevent; A. AIDS B. Social isolation C. Other infections D. Kaposi’s sarcoma 4. A home health care nurse begins caring for a 25 year old female client who has just been diagnosed with the human immunodeficiency virus infection. The client asks the nurse, “How could this have happened”? The nurse responds to the question based on the most frequent mode of HIV transmission which is; A. hugging with HIV positive sexual partner without using barrier protection 8. The nurse is planning a community education program on how to prevent the transmission of viral hepatitis. Which of the following types of hepatitis is considered to be primarily a sexually transmitted disease? A. Hepatitis A 42 COMMUNICABLE DISEASE B. Hepatitis B C. Hepatitis C D. Hepatitis D A. B. C. D. 9. When caring for a client with scabies, the nurse should be aware that scabies is; A. highly contagious B. a chronic problem C. caused by a fungus D. associated with other allergies impotence scrotal swelling and dysuria urinary retention Dribbling of urine 14. The nurse understand that organism that causes a trichonomal infection is a; A. yeast B. fungus C. protozoa D. spirochete 10. The term Condylomata acuminate refers to; A. scabies B. herpes zoster C. venereal warts D. cancer of the epididymis 15. The oral drug that is likely to be prescribed for treatment of trichonomas vaginalis is A. penicillin B. Gentian violet C. Nystatin (mycostatin) D. Metronidazole (flagyl) 11. Client’s who develop general paresis as a complication of syphilis are usually treated with; A. Penicillin B. Major tranquilizers C. Behavioural modification D. Electroconvulsive therapy 16. When teaching parents at the school about communicable diseases, the nurse reminds them that these diseases are serious and that encephalitis can be a complication of; A. pertussis B. chicken pox C. poliomyelitis D. scarlet fever 12. When educating a female client about gonorrhea, the nurse should emphasize that for women gonorrhea; A. is often marked by dysuria and vaginal discharge B. does not lead to serious complications C. can be treated but not cured D. may not cause symptoms until serious complications occur 17. A mother ask the nurse how to tell the difference between measles and a German measles . The nurse tells the mother that with measles the child has; A. a high fever and koplik’s spots B. a rash on the trunk with pruritus C. nausea, vomiting and abdominal cramps D. symptoms similar to a cold, followed by a rash 13. A female client with gonorrhea informs the nurse that she has had sexual intercourse with her boyfriend and asks the nurse, “Would he have other symptoms?” The nurse responds that in men the symptoms of gonorrhea includes; 43 COMMUNICABLE DISEASE D. “Respiratory precautions are indicated for 18 days after the onset of parotid swelling” 18. Chicken pox can sometimes be fatal to children who are receiving; A. insulin B. steroids C. antibiotics D. anti-convulsants Situation: Isadora, age 9 was bitten by a dog on his way home from school. When his father knew about this, he wanted the dog killed once. 19. The nurse obtains a sputum specimen from a client with suspected tuberculosis for laboratory study. Which of the following laboratory techniques is most commonly used to identify tubercle bacilli sputum? A. acid fast staining B. sensitivity testing C. agglutination testing D. dark field illumination 22. When Isadora was brought to the health center you interviewed Isadora and his father. You told Isadora’s father not to kill the dog…. A. observe the dog for 24 hours B. must be confined in a cage C. should be experimented for negri bodies D. has to be observed for 10 days 20. The nurse should include which of the following instruction when developing a teaching plan for clients who are receiving INH and Rifampicin for treatment of tuberculosis A. take the medication with antacid B. double the dose if a drug dose is forgotten C. increase intake of dairy products D. limit alcohol intake 23. Sight and sound of water as well as drip of the faucet disturb a patient with rabies, which one should you do first? A. place patient near window B. cover the IV bottle with brown paper C. sponge only with warm face cloth D. keep patient clean and quiet 24. Immunization with tetanus toxoid is an example of; A. naturally acquired immunity B. naturally acquired passive immunity C. artificially induced active immunity D. artificially acquire passive immunity 25. An example of active naturally acquired immunity is; A. Gamma globulins injection B. Measles vaccination C. Chicken pox D. Placental transfer of maternal antibodies 21. A nurse provides instructions to a mother of a child with mumps regarding respiratory precautions. The mother asked the nurse about the length of time required for the respiratory precautions. The nurse most appropriately responds that; A. “respiratory precautions are necessary for the entire time of illness” B. “respiratory precautions are necessary until swelling is gone” C. “Respiratory precautions are indicated during the period of communicability” 44 COMMUNICABLE DISEASE D. 2-3 weeks after 1st eruption 1st appeared 26. Measles (Rubeola) is a viral disease, which is large contributor to pneumonia deaths in young children. Which of these are characteristics signs of measles? A. Vomiting, headache, fine petecheal rashes and epistaxis B. Sudden onset of slight fever, skin eruptions which are abundant of the face and extremities C. Rash which spreads from face to trunk and limbs, conjunctivitis, high fever and tiny white spots in the mucosa inside the check. D. Sudden onset of slight fever and skin eruptions which are more abundant on covered than on exposed parts of the body 29. Characteristics eruption in chicken pox A. macular B. popular C. pustular D. vesicular 30. Which of the following communicable diseases cannot be transferred through droplet infection? A. Malaria B. Mumps C. Tuberculosis D. Measles 27. What statement made by a pregnant mother whose niece has German measles best indicates an understanding of the implications of viral infections like rubeola and more importantly rubella? A. “I’ll remember to give my niece aspirin for the fever” B. “I’ll ring my niece to wish her well and explain why I cannot go and visit” C. “if I catch the infection, I need not worry for the virus won’t harm my unborn child” D. “If I catch the infection, I will need to be vaccinated against measles immediately”. 31. Which of the following are respiratory diseases? A. pertussis, pneumonia, malaria B. diphtheria, leprosy, shingles C. PTB, coryza, pertussis D. Elephantiasis, parotitis, impetigo contagiosa 32. Etiologic agent of diphtheria A. staphylococcus aureus B. klebs loefflers bacillus C. bordet-Gengao bacillus D. alpha-hemolytic streptococcus 33. Characteristic sign of diphtheria; A. bullneck appearance B. Aerosangenous discharge C. Pseudomembrane D. Inflamed tonsils 28. School children with chicken pox should be kept out of control for at least; A. 1 week before appearance of rashes B. 1 week after eruption appears or until vesicles becomes dry C. 1 week before recovery Situation: Roger 8 years old was referred to the hospital because of low grade fever, general malaise and loss of appetite. On PE there is a whitest-gray 45 COMMUNICABLE DISEASE membrane patch on his tonsils, soft palate and ovula. Diagnosis: Diphtheria D. Treponema Pertenue 38. The primary lesion of Syphilis is: A. Chancre B. Gummas C. Condylamata Lata D. Maculopapular rashes 34. Diphtheria is characterized by; A. acute nasopharyngitis B. persistent cough for 2 weeks C. acute pharyngitis and laryngitis with pseudomembrane D. catarrhal symptoms with paroxysmal cough 39. Prevention and control of syphilis will be one of the agenda in your conference with the midwives. Which of these is not relevant? A. Immunization of contacts B. Need to immediate report cases found and their contacts to health authority C. Need for early diagnosis and treatment D. Symptoms of syphilis and its mode of transmission 35. Bacterial conjunctivitis is common usually during summer months. Conjunctivitis is transmitted through; except; A. contact with discharges from the conjunctivitis of infected persons B. mechanical transmission by vectors such as flies C. contact with discharges from the upper respiratory tract of infected persons through contaminate finger articles D. all these mode of transmission Situation: One of the responsibilities of a nurse is to protect self and patient from acquiring infections. 40. A nurse is assigned in the emergency room, admitted a patient with hemoptysis and fever, cough for a month but with stable vital signs. Which kind of precautions should you employ? A. Contact precautions B. Enteric precautions C. Droplet precautions D. Airborne Precautions Situation: Leprosy is chronic skin and peripheral nerves disease caused by Mycobacterium leprae. 36. A nurse role in the prevention of spread of leprosy is through; A. health education B. proper nutrition C. Personal hygiene D. BCG vaccination 41. The receiving nurse in the Medical surgical ward will expect which isolation technique upon the arrival of the patient? A. respiratory isolation B. strict isolation C. TB isolation D. Enteric Isolation Situation: Mrs. Escudero lives in an urbanized community. She is positive to syphilis so she goes to the health center for proper management. 29. The causative agent of Syphilis is: A. Treponema Pallidum B. HIV C. Neisseria group Situation: Knowledge of the basic concepts and principles related to care 46 COMMUNICABLE DISEASE of patients with communicable disease is vital in the performance of the nurse role as health educator. B. personal hygiene C. complete immunization D. physical stamma 42. Air, water and food can serve as: A. Vehicle of transmission of infectious agents B. Reservoirs of microorganism C. Entry routes for infectious agents D. Vehicles for exit of infectious sperm 46. When “breaking the chain of infection” which of the following is TRUE? A. a virulent agent can resist disinfectant B. an appropriate portal of entry will not cause infection C. mode of entry of harmful organisms is direct entry D. every link in the chain of infection can be interrupted 43. As you made your home visits, you see mothers preparing food at home. Conscious of the principles underlying hand washing, you remind them to wash their hands before handling foods for the simple reasons that: A. Hands can be sterile by thoroughly scrubbing with soap and water. B. Soap used in hand washing acts as a disinfectant. C. transient bacteria can be reduced by mechanical cleansing D. through hand washing, heat coagulates protein Situation: Pneumonia remains to be one of the leading causes of deaths. Hence, this was discussed in the one conferences at the Rural Health Unit. 47. This disease is characterized by: A. sudden onset with chills, fever, pleural pain and cough productive of “rusty” sputum B. fever, headache, malaise, anorexia, and non productive cough C. fever, fatigue, cough chest pain and loss of weight D. fever, cough, hoarseness and hemoptysis 44. The incidence of ascariasis can be reduced by preventing other children from acquiring the disease. This can be done through: A. Teaching the children to cut fingernails and was hands before putting anything into the mouth B. Avoiding overcrowded places C. Teaching children to use slippers while playing on the soil. D. Avoiding direct contact with children suffering from parasitism 48. Pneumonia is transmitted through which of these modes: A. through articles freshly soiled with respiratory discharges B. by direct oral contact C. by droplet spread D. any of these mode of transmission 45. The first line of defense of the body against disease is: A. an intact skin Situation: Rainy season is evident again and dengue hemorrhagic fever is 47 COMMUNICABLE DISEASE one of the locally endemic diseases in the community. 49. Capillary fragility test was done to a patient suspected of DHF. It can be achieved by doing: A. schick's test B. rumple needle test C. tine test D. dick's test 50. Hematology report on platelet count revealed 250, 000 mm3. From the nurses knowledge of the lab she would: A. call the physician's attention to this value and anticipate transfusion of the whole blood B. have vitamin K available for IV infusion C. call the physician's attention and call laboratory to order the platelet transfusion D. realize that this is a normal value References: David L. Heymann, Control of Communicable Disease Manual 19th Edition Dionesia Mondejar – Navales, Handbook of Common Communicable and Infectious Diseases. Copyright 20008 48