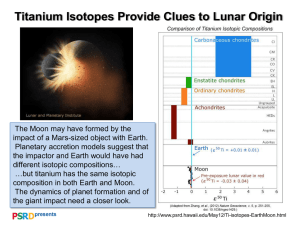
Titanium for medical and dental applications—An introduction 1.1 F.H. (Sam) Froes Consultant to the Titanium Industry, Tacoma, WA, United States 1.1.1 Background Titanium was first used in orthopedic applications in the 1950s. Orthopedics is that branch of surgery which is concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat mus culoskeletal trauma, spine diseases, sports injuries, and much more. Currently, titanium alloys are the main preference (Fig. 1.1.1) for orthopedic devices such as hip joints, bone screws, knee joints, spinal fusion cages, shoulder and elbow joints, and bone plates and scaffolds (Fig. 1.1.2) [1–3]. Titanium is the metal of choice for orthopedic practitioners because of its general corrosion resistance (Fig. 1.1.3) unlike iron (Fig. 1.1.4). It is inert in the human body and is resistant to attack by body fluids. Additionally, it has proven to be compatible with bone density, it is strong, and has a low modulus; hence, it is an excellent material for the orthopedic arena. Titanium is also used in cardiovascular applications (i.e., pertaining to the heart and blood vessels throughout the body). Blood vessels carry nutrients and oxygen to the tissues of the body and remove carbon dioxide and other wastes. They are subject to a number of diseases including arteriosclerosis, coronary artery disease, heart valve dis ease, and many more. The human body readily accepts titanium; it has proven to be more biocompatible than stainless steel or cobalt chrome. In addition, titanium has a higher fatigue strength than many other metals. It is also compatible with MRI (magnetic resonance imaging) and CT (computed technology), which also contributes to making it the material of choice in orthopedic applications. More than 1000 tonnes (2.2 million pounds) of titanium are implanted in patients worldwide every year, and this is set to increase as people live longer, or are seriously injured in road traffic or other accidents. Titanium is light, strong, and totally biocompatible, making it one of the few materials currently known that naturally matches the requirements for implantation in the human body. Because titanium resists corrosion, is biocompatible, and has an innate ability to join with human bone, it has become a staple of the medical field. From surgical titanium instruments to orthopedic titanium Titanium in Medical and Dental Applications. https://doi.org/10.1016/B978-0-12-812456-7.00001-9 © 2018 Elsevier Inc. All rights reserved. 4 Fig. 1.1.1 Characteristics of titanium which make it attractive for medical and dental applications. Titanium in Medical and Dental Applications High corrosive resistance Low specific gravity Biocompatible material Nonmagnatic property TITANIUM High specific strength Fig. 1.1.2 Ti-6Al-4V scaffold for medical implant applications fabricated using Selective Laser Melting Additive Manufacturing technology. rods, pins, and plates, titanium has become the fundamental material used in medicine. Titanium is also much-used outside medicine. This makes it incredibly useful for many different industries, including the automotive, aerospace, and architectural worlds. Titanium for medical and dental applications—An introduction 5 Fig. 1.1.3 General corrosion behavior of commercial purity titanium and Ti-Pd alloys compared to other metals and alloys in oxidizing and reducing acids; with and without chloride ions. In general, each metal or alloy can be used for those environments below its respective solid lines. Fig. 1.1.4 Titanium is very corrosion resistant, unlike iron [4]. 1.1.2 Body implants The implant must be permanent in critical applications where it cannot readily be maintained or replaced. There is no more challenging situation in this respect than implants in the human body. Here, the effectiveness and reliability of both 6 Titanium in Medical and Dental Applications implants and medical and surgical instruments are essential factors in saving lives and in the long-term relief of suffering and pain. Implantation represents a potential assault on the chemical, physiological, and mechanical structure of the human body. There is nothing comparable to a metallic implant in living tissue. Most metals in body fluids and tissue are found in stable organic complexes. Corrosion of implanted metal by body fluids results in the release of unwanted metallic ions, with likely interference in the processes of life. Corrosion resistance is not itself sufficient to suppress the body’s reaction to cell-toxic metals or allergenic elements such as nickel, and even in very small concentrations from a minimum level of corrosion, these may initiate rejection reactions. Titanium is judged to be completely inert and immune to corrosion by all body fluids and tissue, and is, thus, wholly biocompatible. The reasons for selecting titanium for implantation are a combination of the most favorable characteristics, including immunity to corrosion, biocompatibility, strength, low modulus and density, and the capacity for joining with bone and other tissue (osseointegration). The mechanical and physical properties of titanium alloys combine to provide implants which are highly damage tolerant. The human anatomy naturally limits the shape and allowable volume of implants. The lower modulus of titanium alloys compared to steel is a positive factor in reducing bone resorption. Two further parameters define the usefulness of the implantable alloy, the notch sensitivity (i.e., the ratio of tensile strength in the notched to the unnotched condition) and the resistance to crack propagation, or fracture toughness. Titanium scores well in both cases. Typical NS/TS ratios for titanium and its alloys are 1.4–1.7 (1.1 is a minimum for an acceptable implant material). The fracture toughness of all high-strength implantable alloys is above 50 MPa.m-½, with critical crack lengths well above the minimum for detection by standard methods of nondestructive testing. Examples of titanium use in body implants are shown in Figs. 1.1.5–1.1.7, and its dental use is illustrated later in this chapter. For dental applications, a major change in restorative dental practice worldwide has been made possible using titanium implants. A titanium “root” is introduced into the jaw bone with time subsequently allowed for osseointegration. The superstructure of the tooth is then built onto the implant to give an effective replacement. Titanium is also used in surgery to repair facial damage. Use of the patient’s own tissue cannot always obtain the desired results. Artificial parts may be required to replace facial features lost through damage or disease and so restore the ability to speak or eat, as well as improve cosmetic appearance. Osseointegrated titanium implants meeting all the requirements of biocompatibility and strength have enabled unprecedented advances in surgery, for the successful treatment of patients with large defects and hitherto highly problematic conditions. A comprehensive article on “Understanding Implants in Knee and Hip Replacement” appeared in the journal of the International Titanium Association 2nd Quarter, 2016 Medical Edition [5]. It showed that titanium knee replacements can be tailored to the patient’s size, weight, and gender (a woman has a narrower bone structure, especially on the femur). A companion article [5, p. 20] discusses the Titanium for medical and dental applications—An introduction 7 Fig. 1.1.5 Knee joint implant replacement x-ray showing in medical orthpodedic traumatology scan. Courtesy of Shutterstock. Fig. 1.1.6 Titanium bone implants. influence of processing (in particular, etched versus unetched conditions) on the performance of titanium middle ear prostheses, with the etched condition exhibiting superior performance. A further article [5, p. 76] presents details on a 3D-printed titanium hip implant with a fully porous cup (Fig. 1.1.8) allowing in-growth of bone and tissue, resulting in superior performance. An additive manufactured rib cage and sternum implant is shown in Fig. 1.1.9A and B [5, p. 82]. Fig. 1.1.10 illustrates a fecal continence restoration system consisting of a series of titanium beads with magnetic cores connected by titanium wires to form a ring [5, p. 83]. 8 Titanium in Medical and Dental Applications Fig. 1.1.7 A traditional total hip replacement implant. From http://www.geripal.org/2013/01/metal-on-metalhip-replacements-tragic.html. Fig. 1.1.8 Smith and Nephew revised acetabular fully porous cup with Conceloc technology. (Courtesy Professor H. P. Tang, State Key Laboratory of Porous Metal Materials, Northwest Institute for Nonferrous Metal Research). An additive manufactured jaw bone is shown in Fig. 1.1.11 [4]. Other interesting work involved a study of Ti-Au alloys [6]. An alloy consisting of 3:1 Ti::Au (Fig. 1.1.12) was found to be four times harder than pure titanium and was more biocompatible and exhibited superior wear resistance, making it appear to be an attractive choice for implant applications. Fig. 1.1.9 (A) A 3D additive manufactured rib cage and sternum implant. (B) How the component shown in A is inserted into the human body. Fig. 1.1.10 Titanium fecal continence restoration system. 10 Titanium in Medical and Dental Applications Fig. 1.1.11 An additive manufactured jaw bone. Fig. 1.1.12 Crystal structure of beta titanium-3 gold (Courtesy E. Morosan, Rice University). 1.1.3 Dental implants The use of titanium in dental applications has also increased dramatically over the past 20 years. The replacement of missing teeth with implant-supported prostheses, illustrated in Figs. 1.1.13–1.1.14 [4] has become widely accepted in dentistry for the rehabilitation of fully and partially edentulous patients. This breakthrough in oral rehabilitation is based on the concept of osseointegration. This biological phenomenon is described as direct bone deposition upon a titanium implant surface. Currently, commercially pure (CP) titanium has become the material of choice in implant dentistry, since it has excellent biological and biomechanical properties. Titanium for medical and dental applications—An introduction 11 Fig. 1.1.13 Titanium dental implants (top) and their insertion into the mouth (bottom). Titanium implant description Typical ‘two-piece’ titanium implant connection that is ready to have the crown or bridge connected with a little screw. Titanium implants are placed deep under the gum in order to hide the metal color. This is difficult to brush and for this reason, the connections tend to produce halitosis. This is the area where the corrosion of metal implants is greater. This connections have been proven to accumulate bacteria in all kinds of situations with poor or very good oral hygiene and in any kind or brand of titanium two-piece implants. This is the location where the crown or bridge is connected to the titanium implants Fig. 1.1.14 How the dental implant procedure works. 1.1.4 Titanium surgical instruments A wide range of surgical instruments are made from titanium (see Figs. 1.1.15–1.1.17 [4]). One of its advantages in this respect is its lightness, which helps to reduce the surgeon’s fatigue. Instruments are frequently anodized to provide a nonreflecting 12 Titanium in Medical and Dental Applications Fig. 1.1.15 Titanium surgical instruments, scissors, forceps, and needle holders. Fig. 1.1.16 Titanium instruments, surgical screws, and various implants. surface, essential in microsurgical operations such as eye surgery. Titanium instruments can be sterilized repeatedly without compromising edge or surface quality, corrosion resistance, or strength. Titanium is nonmagnetic, and there is, therefore, no threat of damage to small, sensitive, implanted electronic devices. Titanium for medical and dental applications—An introduction 13 Fig. 1.1.17 Additional titanium instruments. 1.1.5 Titanium in wheel chairs, etc. The same characteristics that make titanium a preferred choice for implants and instruments make it a good choice, particularly in tubular form (Fig. 1.1.18A and B [4]) for wheel chairs (Fig. 1.1.19 [4]) and walkers (Fig. 1.1.20 [4]). The tubular products are generally fabricated as either seamless or welded components from commercially pure titanium or the Ti-3Al-2.5 V alloy. 1.1.6 Specifications for titanium in medical and dental applications Forms and material specifications are detailed in a number of international and domestic specifications, including ASTM and BS7252/ISO 5832, as shown in Table 1.1.1 [2]. Alloys such as Ti-6Al-7Nb eliminate the use of V, an element which can cause cytotoxic outcomes (negatively influencing human cells in a similar manner to the effect of puff adder venom). Mechanical properties of titanium alloys suitable for use in medical and dental applications are shown in Table 1.1.2 [7]. 1.1.7 Other titanium-based materials Nickel titanium, also known as nitinol (part of a shape memory alloy), is a metal alloy of nickel and titanium, in which the two elements are present in roughly equal atomic percentages, for example, nitinol 55, nitinol 60. Nitinol alloys exhibit two closely related and unique properties: shape memory effect (SME) and superelasticity (SE; also called pseudoelasticity, PE). Shape memory is the ability of nitinol to undergo deformation at one temperature, then recover its original, undeformed shape upon heating above its “transformation temperature.” Superelasticity occurs at a narrow 14 Titanium in Medical and Dental Applications Fig. 1.1.18 (A) Titanium tubing. (B) Titanium tubing ready for use in wheel chair or walker applications. Titanium for medical and dental applications—An introduction Fig. 1.1.19 (A,B) Titanium is a popular choice for wheel chairs. Fig. 1.1.20 A titanium walker. 15 16 Titanium in Medical and Dental Applications Table 1.1.1 Specifications for titanium in medical and dental applications ASTM BS/ISO Alloy(S) designation F67 F136 F1472 Part 2 Part 3 Part 3 F1295 – F1580 F1713 F1813 Part 11 Part 10 – – – Unalloyed Titanium—CP grades 1–4 (ASTM F1341 specifies wire) Ti6Al4V ELI wrought (ASTM F620 specifies ELI forgings) Ti6Al4V standard grade (SG) wrought (F1108 specifies SG castings) Ti6Al7Nb wrought Ti5Al2.5Fe wrought CP and Ti6Al4V SG powders for coating implants Ti13Nb13Zr wrought Ti12Mo6Zr2Fe wrought Table 1.1.2 Titanium alloys suitable for medical applications ASTM grade Property 1 2 3 4 5 Yield strength (MPa) Ultimate tensile strength (MPa) Elongation (%) Elastic modulus (GPa) 170 240 275 345 380 450 483 550 795 860 24 103–107 20 103–107 18 103–107 15 103–107 10 114–120 Adapted from ASTM F67 (Grade 1 to 4) and F136 (Grade 5). temperature range just above its transformation temperature; in this case, no heating is necessary to cause the undeformed shape to recover, and the material exhibits enormous elasticity, some 10–30 times that of ordinary metal. Nitinol is highly biocompatible and has other properties that make it suitable for use in orthopedic implants. Its unique properties have caused high demand in less invasive medical devices. Nitinol tubing is commonly used in catheters, stents, and superelastic needles. In colorectal surgery, the material is used in devices for reconnecting the intestine after removing the pathology. Nitinol is used for devices developed by Franz Freudenthal to treat patent ductus arteriosus, blocking a blood vessel that bypasses the lungs and has failed to close after birth in an infant. In dentistry, this alloy is used in orthodontics for brackets and wires connecting the teeth. Once the SME wire is placed in the mouth, its temperature rises to ambient body temperature. This causes the nitinol to contract back to its original shape, applying a constant force to move the teeth. These SME wires do not need to be retightened as often as other wires because they can contract as the teeth move, unlike conventional, stainless-steel wires. Additionally, nitinol can be used in endodontics, where nitinol files are used to clean and shape the root canals during the root canal procedure. Titanium for medical and dental applications—An introduction 17 Nitinol’s unusual properties are derived from a reversible solid-state phase transformation known as a martensitic transformation. At high temperatures, nitinol assumes an interpenetrating, simple, cubic structure referred to as austenite. At low temperatures, nitinol spontaneously transforms to a more complicated, body-centered, tetragonal crystal structure known as martensite. The temperature at which austenite transforms to martensite is generally referred to as the transformation temperature. The mechanism of the shape memory effect involving the transformation from the low-temperature martensite to the higher-temperature austenite causes the original shape to be recovered (see Figs. 1.1.21 and 1.1.22 [4]). 15 nm 0 0.3 46 22 20 nm 0.3015 nm 0. 96.8 41 ᑻ 0. Austenite nm Martensite Fig. 1.1.21 Mechanism of the shape memory effect. The transformation from the lowtemperature martensite to the higher-temperature austenite causes the original shape to be recovered. Fig. 1.1.22 Demonstration of the shape memory effect. 18 Titanium in Medical and Dental Applications Fig. 1.1.23 A nitinol stent. Fig. 1.1.24 How a nitinol stent works. A nitinol stent and how it works is shown in Figs. 1.1.23 and 1.1.24 [4]. A nitinol fixation device is shown in Fig. 1.1.25 [4]. Dental use of nitinol is shown in Fig. 1.1.26, [4] a dental brace. Recently, alloys have been developed beyond the first-generation terminal alloys. These include Ti-6Al-4V, Ti-6Al-7Nb, and the commercially pure grades. These alloys are low modulus near beta and beta alloys, which match the low modulus of human bone much better [8]. Alloys such as Ti-29Nb-13Ta-4.6Zr, Ti-13Nb-13Zr, and Ti-10Nb-10Zr have been fabricated by metal-injection molding methods and have good strengths and excellent biocompatibility with the human body. Titanium for medical and dental applications—An introduction 19 Fig. 1.1.25 Nitinol fixation devices. Fig. 1.1.26 Nitinol dental braces. (A) Schematic of braces in place on teeth and (B) dental braces on teeth. 1.1.8 Post script A comprehensive summary of the use of AM in dentistry is shown in Fig. 1.1.27. 1.1.9 This book This book focuses on titanium in medical and dental applications, including implants, instruments, and devices such as wheel chairs and walkers. The book contains information on various fabrication techniques including conventional ingots and 20 Titanium in Medical and Dental Applications 3D Printing—Manufacturing Methods—Dental Industry Laminated Object Manufacturing (LOM) 3.2% n itio ) os ep FDM dD ( se ling Fu ode 0.8% 1 M Sele Me ctive L ltin ase g 11. (SLM r ) 3% 3D in kjet P 7.1% rinting rs he Ot .4% 8 Se tive Laser lec Sintering (SL S) 14.3% La Dire se ct rS M 2. int eta 3 % er l in g A) (SL phy gra o h lit reo 27.5% Ste ) ht ig LP l L (D ta ing i ig D ess .5% oc 1 Pr c Beam Electroni BM) (E Melting 2% 3. Others Include Laser Powder Sintering | Solid Freeform Fabrication | Robocasting Fig. 1.1.27 A comprehensive summary of the use of AM in dentistry. Courtesy of Sagacious Research. subsequent processing (forging, rolling, extrusion, etc.), and approaches such as powder metallurgy, additive manufacturing, and metal injection molding. It also contains information on a number of alloys starting with commercially pure titanium and Ti-6Al-4V and extends to compositions such as nitinol (with compositions close to equiatomic Ti-Ni). References [1] [2] [3] [4] Titanium Industries, Inc., US office of Technical Assessment Web Page (accessed 7-07-16). AZO Materials Web Page (accessed 7-07-1) Wikipedia, (accessed 7-17-16). Internet Explorer, Titanium Implants Illustrations, vol. 8 (accessed 11-25-16). Titanium for medical and dental applications—An introduction 21 [5] Padgett, D.E., Windsor, R.E., 2016. International Titanium Association. Titan. Today (2nd Quarter), 11. [6] Anon, 2016. Gold boosts titanium knee strength. Adv. Mater. Process. 174 (8) 8,9. [7] Elias, C.N., et al., 2008. Biomedical applications of titanium and its alloys. JOM (March), 46. [8] B. Williams, Powder injection molding international, “World PM2016: PIM Technical Sessions Review Advances in Novel Titanium Alloys for Biomedical Applications.