••
rn
_,
(f)
.
CLINICAL
ASSESSMENT
RECOMMENDATIONS
-
- ··
- · ~----------
CLINICAL
ASSESSMENT
RECOMMENDATIONS
AMERICAN SOCIETY
of
HAND THERAPISTS
Copyright
pists
©
1981 by the American Society of Hand
A11 rights reserved.
Printed in the United States of America
Thera-
Ueveloped and written by:
Elaine Ewing Fess, MS, OTR
Christine A. Moran, MS, RPT
Edited by the following 1980-81 ASHT officers and
ittee Chairmen:
A. Gloria Hershman, OTR
Evel yn J. Mackin, LPT
Georgiann F. Laseter, OTR
Valerie A. Holdeman, RPT
Karen H. Prendergast, RPT
Gloria DeVore, OTR
Cynthia A. Philips, OTR
Shirley Ollos Pearson, MS, OTR
Lynnlee Fullenwider, OTR
Carolina deLeeuw, OTR
Margaret S. Carter, OTR
Susan D. Morales, OTR
Judith A. Bell, OTR
Judy C. Colditz, OTR
Comm-
Robert J. Duran, M.D., 1980- 81 Chairma n of the Clinical
Committee of the American Society for Surge ry of the Hand,
and Jerome E. Adamson, M.D. are gratefull y acknowledged
for their assistance in developing and editing this mono graph.
Elaine Ewing Fess
Christine A. Moran
TABLE OF CONTENTS
Introduction
Assessment Recommendations
Joint Motion
3
Grip and Pinch
6
Volume
8
Dexterity and Coordination
Bibliography
..
10
13
I
often say that when you can measure what you are speak-
ing
about
about
it;
knowledge
and express it in numbers,
you know something
but when you cannot measure it in numbers your
is
of a meag re and unsatisfactory kind; it may
be the
beginning of knowledge but have scarcely in your
thought
advanced
to the
stage
of science whatever the
matter may be.
Lord Kelvin
INTRODUCTION
The fundamental goal of hand rehabilitation is to return
each patient to an optimal level of competency in meeting
the daily challenges of his environment.
Accomplishment
of this goal is dependent upon the expertise of those who
are responsible for directing the individual rehabilitation programs, and their effectiveness is contingent upon
their abilities to identify and perceive the specific
hand dysfunction problems presented. Because the understanding of these problems, through analysis of assessment data, is directly influenced by the quality of information gathered, it is imperative that data collection
and review be implemented utilizing stringent criteria for
the selection of evaluation instruments and methods.
A thorough, exacting and unbiased assessment procedure
provides the medical specialist with information that
delineates pathology and establishes a framework for predicting the rehabilitation potential of a hand which has
been debilitated by disease or injury.
The analysis of
initial evaluation data assists in identifying treatment
objectives, facilitates ordering of priorities, and provides a baseline for a nonprejudicial determination of
patient progress. In addition to stimulating patient and
staff motivation, the use of objective measurements recorded at regular intervals throughout a systematic
course of treatment allows for an impartial appraisal of
the effectiveness of treatment methods.
Assessment data
obtained through formal study and investigation also
serves as the foundation of a common language for professional communication and promotes unbiased comparison of
hand rehabilitation methods and techniques.
While the value of experience cannot be underestimated, in
an era of increasing consumer awareness and demand for
accountability, one must question the sole reliance on
therapeutic techniques which have not been substantiated
or given credence through quantitative measurement.
The
use of instruments which have been proven to measure precisely and accurately and which produce consistently dependable information allows the clinician to move from a
· subjective to objective level of observation and understanding.
The greater the accuracy of the instrument in
its ability to measure a given entity, the better the opportunity the examiner has of deducing reasonable conclusions. When dealing with numrically expressed facts,
identifying and eliminating extraneous variables reduces
~---
the chance of error or subconscious bias in subsequent
judgments and decisions.
Although numerous instruments have been designed to aid in
defining pathology of the hand, no single device exists
which has universal application. Instead, various tools
have been developed to measure specific capacities of the
hand i.e., strength, motion, volume and coordination. The
astute clinician, relying on many tools to assess the
total spectrum of hand performance, chooses testing instruments which will provide the most accurate and precise
information possible.
The importance of critically appra1s1ng hand assessment
instruments cannot be overemphasized. Many of the currently available and commonly utilized tools are surprisingly inadequate when viewed in terms of consistency,
dependability, and accuracy. Even when instruments meet
selection criteria, recalibration adjustments are necessary. Hand assessment instrumentation is in a developmental phase and the challenges of refinement are just
becoming apparent!
PURPOSE
To encourage more uniform procedures, the purpose of this
monograph is to recommend basic guidelines for four
techniques frequently utilized in the appraisal of hand
dysfunction: (l) range of motion, (2) grip and pinch
strength, (3) volume, and (4) coordination and dexterity.
These recommendations are introduced not with the intent
of mandating protocol but in hopes of initiating steps
toward a more coherent and concise language among mediMethods and
cal specialists dealing with the hand.
nomenclature which have been selected with exacting
criteria significantly enhance the possibility for precise assessment and directly influence the quality of
treatment and communication.
2
ASSESSMENT RECOMMENDATIONS
JOINT MOTION
Based on a review of The Hand, published by the American
Society for Surgery of the Hand, Joint Motion - Method of
Measurin and Recordin , by the American Academy
of
Orthopedic Surgeons, AAOS), and other pertinent studies,
it is recommended that joint measurement be taken with an
appropriate size goniometer utilizing oo as neutral position.
Unless specified, goniometric measurements may be
taken on either the dorsal or lateral aspect of the joint
{Figure 1), and in the presence of moderate to severe
joint swelling, lateral measurements are preferred.
The
consistency of instrument placement is of prime importance. Any deviation from the normally utilized routine
should be recorded. Both tendon excursion (active motion)
and joint motion or capsular tightness (passive motion)
should be noted, and because proximal joint posture influences distal joint motion, the position of the elbow,
forearm or wrist should be standardized according to the
specific joint being measured.
For example, forearm
motion (pronation, supination) should be measured with the
elbow in 90° of flexion to eliminate the extraneous variable of humeral rotation. Normal motion comparison values
may be obtained by measuring the uninvolved extremity or
in instances of bilateral involvement, through comparison
with normal ratings established by the AAOS.
Wrist Motion
Saggital and coronal wrist motion measurements are significantly influenced by both forearm position and placement of the goniometer. To enhance the consistency of
range of motion assessment, it is recommended that wrist
volar flexion and radial and ulnar deviation measurements, be taken with the forearm in pronation and with the
goniometer placed dorsally on the wrist.
Wrist dorsiflexion should also be measured with the forearm pronated,
but the goniometer should be placed volarly. Alignment of
the goniometer on either the dorsal or volar suface of
the wrist, should correspond to the long axis of the forearm and the third metacarpal, eliminating the variable of
the more mobile fourth and fifth carpometacarpal joints.
3
Fig. l ~Consistency of placement of the goniometer on
either the dorsal or lateral aspect of the joints being
measured is of prime importance.
4
Uigital Motion
When measuring digital motion, the wrist should be placed
in neutral position to minimize the tenodesis effect of
extrinsic musculotendinous units. In addition to recording individual joint motion measurements, total passive
motion (TPM) and total active motion (TAM) values of the
digits are recommended.
Total motion of a digit is
described by a single number which represents the summation of the joint flexion measurements minus the summation of joint extension deficits.
TPM
(Total Passive Motion)
(MP+PIP+DIP passive flexion)
(MP +P IP+D IP
passive extension deficit) or total passive
flexion of the digit minus the total passive
extension deficit of the same digit.
TAM
(Total Active Motion)
(MP+PIP+DIP
active flexion)
(MP+PIP +DIP
active extension deficit) or total
active
flexion of the digit minus the total active
extension deficit of the same digit.
Total motion measurements are taken with the digits in a
"fisted" position, omitting any type of external "blocking" technique.
Hyperexte nsion is considered to be a
negative value in the actual mathematical computation of
TAM or TPM.
The use of total motion values facilitates
comparison of data by providing a composite statement of
the integrated motion of a digit.
In addition to specific goniometric measurements, the
distances of the individual pulps of the digits from the
distal palmar crease may be recorded in centimeters. Because of the greater margin of error and the lack of joint
specificity, it is recommended that this method not be
relied upon as the sole measureme nt of digital joint
motion, but may be employed as a useful and often more
graphic adjunctive technique. Prior to the introduction
of the TPM/TAM technique this method was used to obtain
composite digital motion values.
5
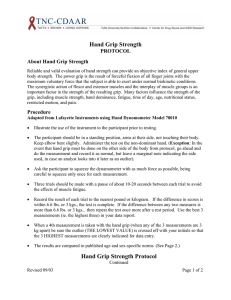
GRIP AND PINCH STRENGTH
In the assessment of grip strength, the use of a standard
adjustable handle dynamometer is recommended. Studies on
normal subjects utilizing this type of dynamometer have
shown that strength measurements vary according to the
subject•s sex, age, hand size, hand dominance, occupation,
motivation, and the time of day which the subject was
tested. Maximum readings occur most frequently in either
the second or third handle position, and on the first or
second attempt of a series of successive trials. To provide consistency in reporting of clinical and research
data, and in accordance with the guidelines established
by the Clinical Assessment Committee of the American
Society for Surgery of the Hand, it is recommended that
the second handle position of the dynamometer be used
when evaluating grip strength, and that three successive
grip determinations should be recorded in either kilograms or pounds.
Because the position of the extremity directly influences
grip measurements, the patient should be seated with his
shoulder adducted and neutrally rotated, elbow flexed at
90°, and the forearm and wrist in neutral position
(Figure 2). To prevent damage if the dynamometer is inadvertantly dropped, the examiner lightly supports the
base of the instrument as the patient is instructed to
maximally grip the handles.
Pinch strength, as measured by a commercially available
pinchometer, should be evaluated for both key (thumb pulp
to lateral aspect of middle phalanx of the index finger)
and tip pinch (thumb tip to index finger tip).
As with
grip strength, the readings of three successive trials
are recorded in either kilograms or pounds.
For consistency, the patient should be positioned as described
above.
It is important to document the variables of patient age,
sex, upper extremity dominance, and hand size. Any deviation from the normally utilized routine of measuring
should be recorded and the serial number of the instrument
employed noted so that the same instrument may be used for
successive evaluations. Subsequent measurements should be
taken at approximately the same time of day that the
initial evaluation was done. Both grip and pinch assessment instruments should be periodically recalibrated to
maintain accuracy.
6
Fig. 2 -- Positioning of the patient and placement of
dynamometer handle influence grip strength values.
7
the
Comparison index ratings may be expressed as a percentage
of pre-treatment mean to trial mean; as a percentage of
the contralateral extremity mean to the trial mean; or as
a percentage of an established 11 normal 11 (for the age, sex,
dominance, occupation, etc. of the patient) to trial
mean. When computing the mean or average of the readings
of the successive trials it is statistically important
that the number of trials determining the mean remain
constant.
For example, the comparison of a five-trial
mean to a three-trial mean would not be as statistically
significant as would the comparison of two three-trial
means. It is also important to note that studies differ
in reporting 11 normal 11 values for grip and pinch strength
depending on the specific measurement techniques utilized.
VOLUME
A commercially available water displacement volumeter is
recommended for assessment of composite mass of the hand
and forearm (Figure 3), providing immersion of the extremity in water is not contraindicated.
When specific
procedural guidelines are followed, the volumeter has been
shown to be accurate to within 10 ml. In order to assure
a high degree of instrument accuracy, it is recommended
that prior to testing, the volumeter be placed on a level
table and filled with water to the point of overflow. The
patient, with dressings and jewelry removed from the extremity, should then be seated comfortably next to the
volumeter and instructed to slowly immerse the hand and
forearm until a firm pressure from the stop rod is perceived in the third web space. Once full immersion has
occurred, it is important that the extremity be held
motionless until water spillage from the spout completely
stops.
Variables which have been shown to decrease the accuracy
of volumeter readings include (a) the use of a faucet or
hose which agitates or introduces excess air into the
water when filling the tank, {b) forearm or wrist movement
within the tank, (c) application of an inconsistent pressure on the stop rod, and (d) inconsistent placement of
the volumeter when making successive volumetric measurements.
8
Fig.
3 -- volumeter accuracy has been shown to be within
10 I'll.
9
DEXTERITY AND COORDINATION
It is recommended that hand coordination or manual dexterity be evaluated through the use of standardized hand
function tests . The term "standardized" indicates that a
test has been statis tically proved (A) to assess that
which it purports to evaluate, and (B) to measure consistently in separate testing situations and between different examiners. A standardized test includes:
(1) a
statement of purpose or intent, (2) correlation statistics
or other appropriate measure of validity,* (3) correlation statistics or other appropriate measure of reliability,* (4) instrument/equipment descriptions, (5) norms
which may be divided into subcategories appropriate to
the population i.e., age, sex, dominance, and in some
cases, occupation, (6) specific instructions for administration, scoring and interpretation, and (7) preferably a
bibliography of related literature.
When administering a standardized hand function test, it
is essential that the specified instructions be followed
and that the presentation sequence and the integrity of
the test be maintained. Portions or sequence of the test
may not be altered unless the consequences of such a
change have been evaluated and are delineated in the
test instructions.
These guidelines (l-7) have been presented to establish a
standard by which any hand function test may be appraised
as to its value as a reliable and valid testing instrument. Examples of standardized hand function tests include, but are not limited to, the Purdue Pegboard, the
Minnesota Rate of Manipulation , the Crawford Small Parts
Dexterity Test, and the Jebson Hand Dexterity Test
(Figure 4).
*NOTE:
"Average" or mean values alone do not denote validity corre 1at ions or re 1i abi 1ity coefficients.
10
A
8
Fig. 4 (A) - The Jebson Hand dexterity Test, consisting
of seven timed subtests, may be used to assess gross coordination skills. (B) The Purdue Pegboard is an example
of a standardized test which measures fine hand coordinat ion .
11
BIBLIOGRAPHY
Alder, H.L., Roessler, E.B.: Introduction to probability
and statistics, ed. 5, San Francisco, 1972, W.H. Freeman and Co.
American Academy of Orthopedic Surgeons: Joint motion
method of measuring and recording, Chicago, 1965, AAOS.
American Society for Surgery of the Hand: The hand -examination and diagnosis, Aurora, Colorado, 197B, ASHT.
Anastasi, Anne: Psychological testing, 4th ed., New York,
1976, Macmillan Pub. Co., Inc.
Bechtol, C.O.: Grip Test; Use of a Dynometer with Adjust820 -824;
able Handle Spacing, J Bone Joint Surg. 36-A:
B32, 1954.
Bolton, B. (ed): Measurements and evaluation in rehabilitation, Baltimore, 1976, University Park Press.
Bookwalter, K.W., et al.: Grip Strength Norms for Males,
Res Quart Amer. Ass. Health Phys. Educ., 21: 249-276,
19t>U.
Bowers, L.E.: Investigation of the relationshi p of the
hand size and lower arm girths to hand grip strength as
measured by selected hand dynamometers, Research Quarterly, 32: 30B-314, 1961.
Brand, P. and Wood, H.: Hand Volumeter Instruction Sheet,
U.S. Public Health Service Hospital, Carville, Los Angeles.
Burke, W.E., et al.: Relation of Grip Strength and GripStrength Endurance to Age, J Appl. Physiol, 5: 628-630,
1953.
Chaffin, U.: Ergonomics guide for the assessment of human
static strength, Am. Ind. Hyg. J., 36:
505-11, 1975.
Clarke, O.H.: Strength recovery from static and dynamic
muscular fatigue, Research Quarterly, 33:
349-355,
1962.
13
Clarke, H.H., Elkins, E.C., Martin, G.M. and Wakim, K.G.:
Relationship between body position and the application
of muscle power to movements of the joints, Arch. Phys.
Med. Rehabilitation, 31: 81-90, 1950.
Investigation of the T-5
Cotten, D.J. & Bonnell, L.:
cable tensiometer grip attachment for measuring strength
of college women, Research Quarterly, 40: 848-49, 1969.
Creelnan, G.:
Report on Hand Volumeter- Accuracy and
Sensitivity of Measurements, Engraving Experts/Medical
Supply Division, Idyllwild, California, 1979.
Currier, D.P.: Elements of research in physical therapy,
Baltimore, 1979, Waverly Press.
Davis, Frederick, B.: Educational measurements and their
interpretation, Belmont, California, 1964, Wadsworth
Pub. Co.
DeVore, G. and Hamilton, G.: Volume Measuring of the
verely Injured Hand, AJOT, 22: 16-18, 1968.
Eccles, M.:
5-8, 1959.
Se-
Hand Volumetrics, Br. J. of Phys. Med., 19:
Edwards, A.L.: Statistical analysis, ed.
1974, Holt, Rinehart and Wilson, Inc.
4,
New
York,
Everett, P.W., and Sills, F.D.:
Relationship of Grip
Strength to Stature, Somatotype Components and Anthropometric Measurements of Hand, Res Quart Amer. Ass. Health
Phys. Educ. 23: 161-166, 1952.
Fess, E., Harmon, K., Strickland, J. and Steichen, J.:
Evaluation of the Hand by Objective Measurement, ed.
Hunter J., Schneider L., Mackin, E. & Bell, Rehabilitation of the Hand, pg. 70-81, St. Louis, 1978, CV Mosby.
Flatt, A.E.:
Kinesiology of the
Course Lect. 18: 266-281, 1961.
hand, Instructional
Hazelton, F.T., Smidt, G.L., Flatt, A.E. and Stephens,
R.I.: The influence of wrist position on the force produced by the finger flexors, J. Biomechanics 8:
301306, 1975.
14
Hewitt, D.: The range of active motion at the wrist
women, J. Bone & Joint Surgery, 10: 775, 1928.
of
Heyward, V. McKeown, B. &Lesseman, R.: Comparison of
Stoelting hand grip dynamometer and linear voltage differential transformer for measuring grip strength, Research Quarterly, 46: 262-266, 1975 •.
.
Hines, M., and O'Connor, J.: A measure of finger dexterity, Personnel Journal, 4: 379-382, 1926.
Hislop, H.J.:
Quantitative changes in human muscular
strength during isometric exercise, J. Am. Phys. Ther.
Assoc., 43: 21-38, 1963.
Horwitz, T.: An anatomic and roentgenologic study of the
wrist joint, Surgery 7: 773, 1940.
Hultman, E. Bergstiom, Jr., & Mclennan Anderson, N.:
Breakdown and resynthesis of phosphorylcreatine and
adenosine triphosphate in connection with muscular work
in man, Scand J of Clinical and Lab. Investigation, 19:
56-66, 1967.
Hunter, J. and Mackin E.: Edema and Bandaging, ed. Hunter, J., Schneider, L., Mackin, E., & Bell, J., Rehabil itation of the Hand, pg. 113-121, St. Louis, 1978, cv
Mosby.
Jebson, R.H., Taylor, N., Triegchmann, R.B., Trotter, M.
J., and Howard, L.A.:
An objective and standardized
test of hand function, Archives of Physical Medicine and
Rehabilitation, 50: 311, 1969.
Kellor, M. et al.:
77-83, 1971.
Hand strength and dexterity, AJOT, 25:
Kellar, M. et al. (contributors): Technical manual: hand
strength and dexterity tests, Minneapolis, Minn., 1977,
Sister Kenny Institute.
Kettle, J., Rundle, F. &Oddie T.: Measurement of Upper
Limb Volume: A Clinical Method, Aust-New Zealand J. of
Surg., 27: 263-270, 1958.
Kirkpatrick, J.E.: Evaluation of Grip Loss; A Factor of
Permanent Partial Disability in California, Industr.
Med. Surg., 26: 285-289, 1957.
15
Kirkpatrick, J.E.:
Evaluation of Grip Loss: Factor of
Permanent Disability in California: Summation and Conclusions of Sub-committee for Study of Grasping Power
Committee on Industrial Health and Rehabilitation of
California Medical Association, Calif. Med., 85: 314320, 1956.
Kraft, G. and Detels, P.: Position of function of the
wrist, Arch. Phys. Med. Rehabilitation, - 53:
272-275,
1972.
Landsmeer, J.M.: Power grip and precision handling, Ann.
Rheum. Dis., 22: 164-170, 1962.
Montoye, H.J. and Faulkner, J.A.:
Determination of the
optimum setting of an adjustable grip dynamometer, Research Quarterly, 35: 29-36, 1964.
Mountcastle, V.B., Medical Physiology,
55, St. Louis, 1968, CV Mosby.
Vol.
II,
Chapter
Mundale, M.S.: The relationship of intermittent isometric
exercise to fatigue of hand grip, Archives of PMR, 51:
532-539, 1970.
Nemethi, C.E.:
Evaluation of Hand Grip in Industry, Industr. Med. Surg., 21: 65-66, 1952.
Patterson, H.M.: Grip Measurements as a Part of the PrePlacement Evaluation, Industr. Med. Surg., 34: 555-557,
1965.
Pryce, J.C.: The wrist position between neutral and ulnar
deviation that facilitates the maximum power grip
strength, Journal of Biomechanics, 13:
505-11, 1980.
Quantitative strength
Schenk, J.M. and Forward, E.M.:
changes with test repetitions, Phys. Ther., 45: 567569, 1965.
Schmidt, R.T., and Toews, J.V.: Grip Strength as Measured
by the Jamar Dynamometer, Arch of PM&R, June: 321-327,
1970.
Steindler, A.: The mechanics of muscular contractures
wrist and fingers, J. Bone & Joint Surgery, 14:
1932.
16
in
1,
Steindler, A.: Mechanics of Normal and Pathologic Locomotion in Man, Springfield, Illinois, 1935,
Thomas.
Stevens, J.C.:
Growth of Sensation on Seven Continua as
Measured by Force of Handgrip , J. Exp. Psych., 59 : 6067, 1960.
Swanson, A. B., Goran-Hagert, C., and Swanson, G.G.:
Evaluation of Impairment of Hand Function, Evaluation
of the Hand by Objective Measurement, ed. Hunter J.,
Schneider L., Mackin, E., and Bell, Rehabilitation of
the Hand, pg. 31-69, St. Louis, 1978, CV Mosby.
Tiffin, J. and Asher, E. J.: The Purdue pegboard;
norms
and studies of reliability and validity, J. Applied
Psychology, 32: 234-47, 1948.
Toews, J.V.: A Grip-Strength Study Among
Arch. Phys. Med., 45: 413-417, 1964.
Steelworkers,
Tuttle, W.W. Janney, C.D. & Thompson, C.W.: Relation of
maximum grip strength of grip strength endurance, J of
Applied Physio, 2: 663-670, 1950.
Wayl ett, J. and Sei bly, 0.:
A study to determine the
average deviation accuracy of a commercially available
volumeter, presented at Fourth Annual American Society
of Hand Therapists, Las Vegas, 1980.
Weiss, M.W. & Flatt, A.E.: A pilot study of 198 normal
children pinch strength and hand size in the growing
hand, AJOT, 25: 10-12, 1971.
17