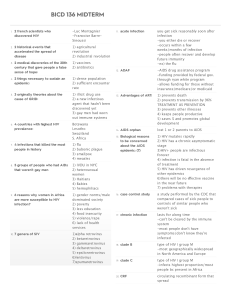
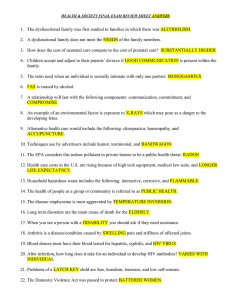
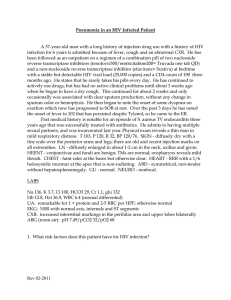
lOMoARcPSD|3134418 Answer KEY-HIV-AIDS- Unfolding Reasoning Nursing Process IV: Medical-Surgical Nursing (Borough of Manhattan Community College) StuDocu is not sponsored or endorsed by any college or university Downloaded by Danica Mijovic (danicamijovic@gmail.com) lOMoARcPSD|3134418 Human Immunodeficiency Virus UNFOLDING Reasoning Michelle Johnson, 36-years old Primary Concept Immunity Interrelated Concepts (In order of emphasis) • Gas Exchange • Infection • Stress • Coping • Clinical Judgment • Patient Education • Communication • Collaboration NCLEX Client Need Categories Percentage of Items from Each Category/Subcategory Safe and Effective Care Environment 17-23% • Management of Care 9-15% • Safety and Infection Control Health Promotion and Maintenance 6-12% Psychosocial Integrity 6-12% Physiological Integrity 6-12% • Basic Care and Comfort 12-18% • Pharmacological and Parenteral Therapies 9-15% • Reduction of Risk Potential 11-17% • Physiological Adaptation © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) Covered in Case Study ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✓ lOMoARcPSD|3134418 UNFOLDING Clinical Reasoning Case Study: History of Present Problem: Michelle Johnson is a 36-year-old African American female with no prior medical history who presents to the emergency department complaining of extreme fatigue for the past several months and experiencing occasional night sweats. During the past week, she has developed a sore throat, dry, nonproductive cough, fever at night with increasing shortness of breath. Michelle embarrassingly admits that she has had a vaginal yeast infection that she has tried to treat with over the counter medications with no success. Michelle states to the triage nurse, “I came in today because I am worried something is wrong with me, I hope it’s nothing serious!” Personal/Social History: Michelle has been divorced for five years and has two daughters (ages 14 and 16) who works full time as a legal secretary. She has recently been working longer hours, skipping meals, and stressed over the possibility of not being able to provide for her two daughters. She has been involved in only one relationship since her divorce. She is engaged to Ken, who has hemophilia and plan to get married next year. What data from the histories are RELEVANT and must be interpreted as clinically significant by the nurse? RELEVANT Data from Present Problem: Clinical Significance: Extreme fatigue for the past several months All of these problems can be caused by exposure to almost any virus and experiencing occasional night sweats. (e.g., influenza)—not just to HIV, BUT, these may be the first indications of the acute HIV infection several months ago. About 50% to 90% of people who are first infected with HIV develop an acute infection within four weeks. Manifestations of this acute HIV infection can be fever, night sweats, chills, headache, and muscle aches. During the past week, she has developed a sore throat, dry, nonproductive cough, fever at night with increasing shortness of breath. Potential respiratory infection with a dry cough and exertional dyspnea in the weeks before the development of other symptoms, fever plus a headache, malaise, night sweats, general fatigue, weight loss, and chest pain are among the clinical manifestations typically seen with HIV. Vaginal yeast infection that she has tried to treat with over the counter medications with no success. Vaginal infection that has not been able to be corrected by treatment is a clinical RED FLAG for HIV. Women often have gynecological conditions as a result of HIV infection. These can include persistent, reoccurring and difficult-to-treat vaginal yeast infections. Immunizations are also difficult as these patients can develop the condition you are trying to prevent: AKA chicken pox. Clinical Significance: Sole provider for her daughters, difficult financial burden. Is experiencing significant situational stress working long hours and intimate relationship with an individual with a significant chronic illness. RELEVANT Data from Social History: Working longer hours, skipping meals, and stressed over the possibility of not being able to provide for her two daughters. Patient Care Begins: Current VS: T: 99.6 F/37.6 C (oral) P: 108 (regular) R: 24 (regular) BP: 110/75 O2 sat: 91% RA P-Q-R-S-T Pain Assessment: Provoking/Palliative: Denies Quality: Region/Radiation: Severity: Timing: © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) lOMoARcPSD|3134418 What VS data are RELEVANT and must be interpreted as clinically significant by the nurse? RELEVANT VS Data: Clinical Significance: T: 99.6 Low-grade temperature may be due to infectious process such as pneumonia, but needs to be trended and closely monitored P: 108 Tachycardia likely indicates increased metabolism due to elevated temperature and infection, but could also be compensatory response due to dehydration or sepsis. More clinical data needs to be collected. R: 24 Too high and is a clinical RED FLAG. Tachypnea needs to be investigated d/t potential respiratory infection and respiratory distress. Sepsis should also be considered as tachypnea may be compensatory mechanism due to sepsis. BP: 110/75 Trend BP closely to determine patient ambiguity or softening of BP related to sepsis. TREND closely to determine if sepsis is developing! O2 sat: 91% RA Clinical RED FLAG. This is too low for a healthy woman and needs to correlate with HR of 108 or so to ensure accuracy. Current Assessment: GENERAL APPEARANCE: ORAL & NECK: RESP: CARDIAC: NEURO: GI: GU: SKIN: Average built female with a worried expression on her face. Appears pale and tired. Calm, body relaxed, no grimacing, appears to be resting comfortably Oral mucous moist and intact. Cervical lymph nodes enlarged bilaterally Slight SOB with exertion and crackles heard bilaterally in lower lobes posteriorly Tachycardia, pink, warm & dry, no edema, heart sounds regular with no abnormal beats, pulses strong, equal to palpation at radial/pedal/post-tibial landmarks, brisk cap refill Alert & oriented to person, place, time, and situation (x4) Abdomen flat, soft/nontender, bowel sounds audible per auscultation in all four quadrants Voiding without difficulty, urine clear/yellow Skin integrity intact, skin turgor elastic, no tenting present What assessment data is RELEVANT and must be interpreted as clinically significant by the nurse? RELEVANT Assessment Data: Clinical Significance: Appears pale and tired. Pale color could be due to lack of RBC/anemia, immune system suppressed, infection. General finding. Cervical lymph nodes enlarged bilaterally Indicates an infectious process that is present in her body that may be systemic Slight SOB with exertion and crackles heard bilaterally in lower lobes posteriorly Respiratory problem is likely consistent with pneumonia. Crackles are present as a result of fluid in the alveoli due to pneumonia or atelectasis. Also, respiratory sat that is low supports this concern. Cardiac Telemetry Strip: © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) lOMoARcPSD|3134418 Interpretation: Sinus tachycardia-rate 110 Clinical Significance: Tachycardia likely indicates increased metabolism due to elevated temperature and infection, but could also be compensatory response due to dehydration or sepsis. More clinical data needs to be collected. Sinus tachycardia is not normal and must be investigated – It is a symptom of a more significant problem. The care provider orders the following based on the clinical data that the nurse has collected: Collaborative Care: Medical Management Care Provider Orders: Complete blood count (CBC) Rationale: Has signs of obvious infection. Need to determine WBC and neutrophil, lymphocyte differential is relevant in this scenario. Basic metabolic panel (BMP) Determine chemistries of sodium and potassium as well as renal function/fluid balance once creatinine is known. Rapid HIV Determine if HIV is the primary source of infection in this scenario Chest x-ray Determine if pneumonia or another resp. Infection/problem is present that is causing her symptoms. Radiology Reports: Chest x-ray What diagnostic results are RELEVANT and must be interpreted as clinically significant by the nurse? RELEVANT Results: Clinical Significance: Diffuse ground-glass Represents the accumulation of intra-alveolar fibrin, debris, and organisms as a opacity present result consistent with pneumocystis pneumonia (PCP) bilaterally Lab Results: Complete Blood Count (CBC:) WBC (4.5–11.0 mm 3) Neutrophil % (42–72) Lymphocyte % (2-10) Hgb (12–16 g/dL) Platelets (150-450 x103/µl) Current: 3.0 88 6 9.8 208 High/Low/WNL? LOW HIGH WNL LOW WNL Most Recent: 8.5 70 4 10.5 225 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: These labs are ALWAYS RELEVANT, therefore they must be intentionally noted by the nurse! WBC: 3.0 • ALWAYS RELEVANT based on its correlation to the presence of inflammation or infection • Viral infections, overwhelming bacterial infections, and bone marrow disorders can all cause leukopenia. Patients with severe leukopenia should be protected from anything that interrupts skin integrity, placing them at © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) Worsening TREND-is a clinical RED FLAG lOMoARcPSD|3134418 risk for an infection that they do not have enough white blood cells to fight. Neutrophil %: 88 • ALWAYS RELEVANT for same reason as WBCs • Most common leukocyte • FIRST RESPONDER to any bacterial infection within several hours or when the inflammatory response is activated Worsening TREND-is a clinical RED FLAG. Elevated in response to bacterial infection • Normal finding. Elevated with viral infection, but not always elevated in the presence of HIV Stable Lymphocyte %: 6 Hgb: 9.8 • ALWAYS RELEVANT to determine anemia or acute/chronic blood loss. • Level supports chronic anemia Stable. Though LOW, it is not a recent trend • If platelets are low, it will obviously be significant and must be noted • Any patient on heparin products must also have this noted because of the clinical possibility of heparininduced thrombocytopenia (HIT) • Develops when immune system forms antibodies against heparin that cause small clots and lower platelet levels Stable Platelets: 208 Basic Metabolic Panel (BMP:) Sodium (135–145 mEq/L) Potassium (3.5–5.0 mEq/L) Glucose (70–110 mg/dL) Creatinine (0.6–1.2 mg/dL) Current: 148 3.5 90 0.8 High/Low/WNL? HIGH WNL WNL WNL Most Recent: 142 3.8 101 0.9 What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: TREND: Improve/Worsening/Stable: These labs are ALWAYS RELEVANT, therefore they must be intentionally noted by the nurse! Sodium: 148 • Is hypernatremic most likely because of dehydration • I consider Na+ the “Crystal-Light” electrolyte. Though this is simplistic, it does help to understand in principle how basic Na+ is to fluid balance • When you add one small packet of Crystal Light to your 16-ounce bottle of water, the concentration is just right. This is where a normal Na+ will be (135-145) • Where free water goes, sodium will follow to a degree. Therefore if there is a fluid volume deficit due to dehydration, Na+ will typically be elevated because it’s concentrated (less water) • If there is fluid volume excess, Na+ will be diluted and will likely be low. It is the “foundational” fluid balance electrolyte! © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) Worsening lOMoARcPSD|3134418 Potassium: 3.5 • Essential to normal cardiac electrical conduction, as is Mg+ • f too high or low can predispose to rhythm changes that can be life-threatening! • K+ tends to deplete more quickly with loop diuretic usage than Mg+ Stable Glucose: 90 • Required fuel for metabolism for every cell in the human body, especially the brain • Relevant with history of diabetes or stress hyperglycemia due to illness • Elevated levels post-op can increase risk of infection/sepsis. Stable Creatinine: 0.8 • GOLD STANDARD for kidney function and adequacy of renal perfusion • The functioning of the renal system affects every body system; therefore, it is ALWAYS relevant! Misc. Labs: CD 4 count (>500 cells HIV RNA level, (40-75 copies/mL) Current: 189 60,000 Stable High/Low/WNL? LOW HIGH What lab results are RELEVANT and must be recognized as clinically significant by the nurse? RELEVANT Lab(s): Clinical Significance: CD4: 189 <200 is dangerously low and indicates classification 3: AIDS has developed. the immune system is being destroyed, and the CD4 cells are being overtaken by HIV viral cells. HIV RNA level: 60,000 copies/mL A viral load test is a lab test that measures the number of HIV particles in a milliliter of your blood. These particles are called "copies." Clinical Reasoning Begins… 1. What is the primary problem your patient is most likely presenting ? • Newly diagnosed human immunodeficiency virus (HIV) infection • Pneumocystis pneumonia as a secondary opportunistic infection 2. What is the underlying cause/pathophysiology of this primary problem? HIV Acquired immunodeficiency syndrome (AIDS) is a life-threatening illness caused by the human immunodeficiency virus (HIV). AIDS is an acquired disease characterized by severe immune dysfunction. HIV targets CD4 + (helper) T lymphocytes and renders them incapable of augmenting B-lymphocyte production of antibodies. This breakdown of the immune system leaves the patient highly vulnerable to opportunistic infections such as Pneumocystis jiroveci (formerly known as P. carinii ) pneumonia (PCP) or tumors such as Kaposi's sarcoma (KS). According to the Centers for Disease Control and Prevention (CDC), the HIV epidemic in the United States continues to grow, with an estimated 56,300 new HIV infections per year (CDC, 2008). AIDS is the advanced phase of HIV infection. It is a chronic viral disease that covers a wide spectrum of illnesses and symptoms for a variable course of time. There is no classic disease progression (e.g., some individuals proceed from an asymptomatic, seropositive state to AIDS, whereas others may experience symptoms for many years). HIV disease is therefore considered a continuum of infection. © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) lOMoARcPSD|3134418 Pneumocystis pneumonia Pneumocystis is a fungal organism that are commonly found in the lungs of healthy individuals. Most children are believed to have been exposed to the organism by age 3 or 4 years, and its occurrence is worldwide. The disease occurs when both cellular immunity and humoral immunity are defective. Once inhaled, the trophic form of Pneumocystis organisms attach to the alveoli. Multiple host immune defects allow for uncontrolled replication of Pneumocystis organisms and development of illness. Activated alveolar macrophages without CD4+ cells are unable to eradicate Pneumocystis organisms. Increased alveolar-capillary permeability is visible in electron microscopy. Physiologic changes include the following: • Hypoxemia with an increased alveolar-arterial oxygen gradient • Respiratory alkalosis • Impaired diffusing capacity • Changes in total lung capacity and vital capacity (https://emedicine.medscape.com/article/225976-overview#a3) Collaborative Care: Medical Management Care Provider Orders: Establish peripheral IV Rationale: Will require IV access for both IV antibiotics and IV hydration. Expected Outcome: IV access obtained 0.9% Normal Saline at 100 mL/hour Initial presentation and tachycardia suggest dehydration. Rehydration is needed. HR decreases trimethoprim/sulfamethoxazole Treatment for PCP. Inhibits the metabolism of folic (Bactrim) 1 gram IVPB every acid in bacteria at two different points. 8 hours Improvement in oxygenation, resolution of PCP Fluconazole 200 mg PO BID Treatment for PCP. Inhibits synthesis of fungal sterols, a necessary component of the cell membrane. Treatment should be for 21 days. Improvement in oxygenation, resolution of PCP Prednisone 40 mg PO daily Corticosteroid that will reduce inflammation of airways that is present due to PCP Improvement in oxygenation, resolution of PCP Titrate oxygen to keep O2 sat >92% Initial O2 sat was low and expected with PCP. Ensure adequate oxygenation O2 sat >92% Truvada (tenofovir and Emtricitabine and tenofovir are combined in this pill. emtricitabine) 1 tablet PO daily Combination of two different Nucleoside analog reverse transcriptase inhibitors (NRTIs) that generate bad nucleoside/nucleotide building blocks Slow progression of HIV Reyataz (atazanavir) 300 mg PO daily Inhibits the action of HIV protease, preventing maturation of virions. Therapeutic Effects: CD4 cell counts and viral load with subsequent slowed progression of HIV CD4 cell counts and viral load with subsequent slowed progression of HIV Norvir (ritonavir) 100 mg PO daily Inhibits the action of HIV protease and prevents the cleavage of viral polyproteins. Therapeutic Effects: Increased CD4 cell counts and decreased viral load with subsequent slowed progression of HIV infection and its sequelae. Slow progression of HIV by increasing CD4 cell counts and decreases viral load © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) lOMoARcPSD|3134418 Admit to med/surg unit with telemetry monitoring Will require IV antibiotics and further evaluation of HIV and definitive diagnosis Stabilization of medical status 3. What additional treatment should you anticipate for Ms. Johnson by her HIV test results and CD4 results? • Pulmonary function test • Sputum culture • Screening for other sexually transmitted infections should be performed, including a rapid plasma reagin (RPR) test for syphilis, gonorrhea and chlamydia testing, and hepatitis B and C serologies • Mantoux/tuberculin test • Pregnancy test and Pap smear PRIORITY Setting: Which Orders Do You Implement First and Why? Care Provider Orders: • Establish peripheral IV • 0.9% Normal Saline at 100 mL/hour • trimethoprim/sulfamethoxazole (Bactrim) 1 gram IVPB every 8 hours • Fluconazole 200 mg PO BID • Prednisone 40 mg PO daily • Titrate oxygen to keep O2 sat >92% Order of Priority: 1. Titrate oxygen to keep O2 sat >92% 2. Establish peripheral IV 3. 0.9% Normal Saline at 100 mL/hour 4. trimethoprim/sulfamethoxazole (Bactrim) 1 gram IVPB every 8 hours 5. Fluconazole 200 mg PO BID 6. Prednisone 40 mg PO daily Rationale: 1. A/B priority. Always start with the ABCs! 2. C priority/circulation. Need to have IV before can give IV fluids 3. C priority/circulation 4. Start IV antibiotic first because it will have immediate onset 5. Fluconazole and prednisone PO specific order is not indicated since in real-world practice both PO meds would be given together 6. See above Collaborative Care: Nursing 4. What nursing priority (ies) will guide your plan of care? (if more than one-list in order of PRIORITY) Always use Maslow’s hierarchy of needs to guide nursing priorities in a complex scenario that has both physical as well as psychosocial priorities. Start with PHYSICAL priorities that include: • Maintain adequate oxygenation (NANDA-Impaired gas exchange) • Risk for infection/sepsis related to immune deficiency as a susceptible host The following PSYCHOSOCIAL priorities are also present and need to be addressed once the physical priorities have been taken care of. • Emotional and social support r/t to her daughters, finding a support system, medical costs • Education and guidance in HIV, its management, medications and social contact • Reduced self-esteem related to changes in body image, role, or independence • Potential loss of social contact related to stigma, virus transmissibility, infection control practices, or fear 5. What interventions will you initiate based on this priority? Nursing Interventions: Rationale: Oxygenation/Impaired gas exchange Assess respiratory status q2h during patient's awake period, and note rate, rhythm, depth, and regularity of respirations, use of accessory muscles, flaring of nares, the presence of adventitious sounds, cough, changes in color or character of sputum, or cyanosis. Signs of respiratory distress/worsening status Reposition patient q2h to prevent stasis of lung fluids and resulting pneumonia. Improve oxygenation Group nursing activities, optimally 90-120 min Promote rest which will enhance body’s ability © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) Expected Outcome: Maintain adequate oxygenation and perfusion and to have minimal dyspnea. Indicators include: •Rate and depth of respiration within the normal range •Pulse oximetry within the normal range •Absence of cyanosis lOMoARcPSD|3134418 at a time, to provide patient with uninterrupted rest periods. to fight infection Instruct patient to report changes in cough and dyspnea that increase with exertion. (Manual of Medical-Surgical Nursing, 7th ed. ClinicalKey for Nursing) Infection/Sepsis Perform a complete physical assessment at least every 4-8h to identify changes from the baseline assessment. Sign of worsening respiratory status Assess for signs of active infection or sepsis at frequent intervals (e.g., increased temperature, increased heart rate (HR), decreased blood pressure [BP], diaphoresis, confusion or mental status changes, decreased level of consciousness [LOC]). These signs are related to the vasodilator effect of increased body temperature. Assess for changes in breath sounds (crackles and/or wheezing). Indicate infiltrates from infection or bronchoconstriction from inflammation and/or infection. Assess for indicators of opportunistic infections (e.g., persistent fevers, night sweats, fatigue, involuntary weight loss, persistent and dry cough, persistent diarrhea, headache) Sign of worsening status Place the patient in a private room whenever possible. She is a susceptible host and can easily acquire other infections if exposed Use good handwashing technique or use alcohol-based hand rubs before touching the patient or any of his or her belongings. She is a susceptible host and can easily acquire other infections if exposed to other organisms Inspect the patient's skin and mucous membranes (especially the anal area) for the presence of fissures and abscesses at least every 8 hours She is a susceptible host and can easily acquire other infections if exposed to other organisms Inspect open areas, such as IV sites, every 4 hours for manifestations of infection. (Manual of Medical-Surgical Nursing, 7th ed. Clinical Key for Nursing) Psychosocial Provide a climate of acceptance for patients with AIDS by promoting a trusting relationship. She is a susceptible host and can easily acquire other infections if exposed to other organisms TRENDING of clinical assessment data from most recent will identify early changes of complication such as sepsis The essence of the psychosocial priorities is to support the patient in a time of crisis and provide empathetic caring. Help express feelings and identify positive aspects of themselves Allow her to cry and vent her frustration, demonstrate compassion toward her, and remain nonjudgmental. © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) or pallor and abnormal breath sounds The essence of all outcomes related to infection is that the patient status remains stable and has no complications related to PCP/HIV Supported and feels cared for by the nurse lOMoARcPSD|3134418 Promote patient interaction first by establishing a therapeutic nurse-patient relationship, and do not isolate the patient. Spend time with him or her, even when not performing a procedure or assessment, just to be present. Show understanding and concern while helping the patient find ways to reduce feelings of rejection and isolation. Assess her social support resources. Teach family and significant others about HIV transmission and the use of Standard Precautions to reduce anxiety and increase contact with the patient (Manual of Medical-Surgical Nursing, 7th ed. ClinicalKey for Nursing) 6. What body system(s) will you assess most thoroughly based on the primary/priority concern? Though most body systems are impacted by HIV/PCP directly or indirectly, in this scenario, the following body systems are the priority: • Respiratory • Cardiovascular 7. What is the worst possible/most likely complication to anticipate? • Respiratory failure • Sepsis 8. What nursing assessments will identify this complication EARLY if it develops? Respiratory failure • Increasing RR • Increasing oxygen needs • Decreasing O2 sat • Change in breath sounds from baseline • May become more pale, new onset of diaphoresis as the sympathetic nervous system is activated. Be sure to check inside the mouth for pallor as the client is African American. Sepsis • With an infection of any kind, sepsis is identified by having 2 or more of these criteria of Systemic Inflammatory Response Syndrome (SIRS): • Temp >100.4 or <96.8 • HR >90 • RR >20 • WBC >12,000 or <4000 • Bands >10% 9. What nursing interventions will you initiate if this complication develops? Respiratory failure • Increase O2 to maintain O2 sat >92% • Sit upright © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) lOMoARcPSD|3134418 • Contact primary care provider or activate rapid response team to assess emergently Sepsis • Once a concerning clinical TREND has been identified, contact primary care provider or activate rapid response team to emergently assess Education Priorities/Discharge Planning 1. What will be the most important discharge/education priorities you will reinforce with her medical condition to prevent future readmission with the same problem? The medical/nursing management and patient education outcomes for a person newly diagnosed with HIV include: • Maintain physical health ✓ Importance of maintaining a balanced diet; ways to supplement diet with multivitamins and other food sources, such as high-caloric substances (e.g., Isocal, Ensure). 2. • Manage the disease and prevent transmission ✓ Assess patient's knowledge about HIV disease, including pathophysiologic changes that will occur, ways the disease is transmitted, necessary behavioral changes, treatment regimen, and side effects of treatment, to correct misinformation and misconceptions. ✓ Involve significant other in the teaching and learning process, to facilitate accuracy of understanding. ✓ Provide literature that explores myths and realities of HIV disease process, to facilitate accuracy of understanding. ✓ Medical follow-up appointments. Stress the importance of keeping all scheduled appointments and under what circumstances the patient should seek emergency care. ✓ Partner needs to be tested • Prevent infectious complications ✓ Techniques of self-assessment for early signs of infection (e.g., erythema, tenderness, local warmth, swelling, purulent exudate) in all cuts, abrasions, lesions, or open wounds; fever, chills, diarrhea, or other changes from normal. Michelle Johnson asks why she has to take so many medications and is it alright if she misses any doses? How would you respond? Treatment with only one antiretroviral agent (i.e., monotherapy) promotes drug resistance and does not improve the patient's life span. Instead, multiple drugs are used together in combinations from different classes of antiretroviral agents. This approach is termed highly active antiretroviral therapy (HAART) and has reduced viral load, improved CD4+ T-cell counts, and slowed disease progression. There are currently six classes of antiretroviral drugs: nucleoside reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors (PIs), integrase inhibitors, fusion inhibitors, and entry inhibitors. As a general rule, patients are told they must take the drugs correctly 90% of the time, making sure that out of 10 doses, 9 are taken on time and correctly. This is a tall order when considering that this drug therapy is for the rest of one's life. (Medical Surgical Nursing 8th edition, Ignatavicius) Medication adherence is extremely important because it affects how well the HIV medications decrease viral load. The lower the viral load, the healthier the patient will be. Adherence also helps to prevent drug resistance. Skipped doses may develop strains of HIV that are resistant to the medications currently prescribed—and possibly even to medications haven’t yet taken. The result may be fewer HAART options. Instruct the patient to: • Not skip doses. • Have an adequate supply of medication on hand so there is no interruption in dosing. • Not increase or decrease the number of pills taken • Follow meal and fluid requirements. © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) lOMoARcPSD|3134418 • Contact provider if specific side effects occur. • Store all drugs as instructed. • Check with the provider before taking any OTC medication because of numerous interactions. • Keep follow-up appointments for laboratory monitoring. 3. Michelle Johnson asks “Should I tell Ken about my positive HIV result?” Discuss who should be told about the positive result. If Ms. Johnson has not done so, suggest that she talk to Ken about undergoing HIV testing because there is a possibility that Ken is not infected or is unaware that he has HIV infection. While telling her children and family about her status may seem hard, disclosure has many benefits—studies have shown that people who disclose their HIV status respond better to treatment than those who don't. It is better for the family to learn from her rather that someone else. Many states have partner notification laws that require HIV positive individuals to tell their sexual or needle-sharing partners of their status. Although HIV is now considered a chronic and treatable disease, it can lead to early death. Michelle and her family need to face the future together and be open and prepared for future changes with her health. 4. How can the nurse assess the effectiveness of patient and family teaching and discharge instructions? After any education has been completed with the patient or family, one of the more effective strategies to assess the effectiveness of teaching is to have them restate the essence or most important points of your teaching after it has been taught and then later in the shift to ensure retention. Include patient demonstration if possible. Caring and the “Art” of Nursing 1. What psychosocial needs will this patient and/or family likely have that will need to be addressed? • Emotional support • Spiritual support • Knowledge and education about what is taking place and what the care priorities will be in the days ahead 2. How can the nurse address these psychosocial needs? See care plan above, but be sure to include these principles to provide holistic care: • Emotional support o BE PRESENT and AVAILABLE. See the section on caring at the end of this case study for more information. • Spiritual support o Ask open-ended questions to assess. Those that I have found natural and effective include: ▪ What gives your life purpose? ▪ How has this illness affected the way you view life? ▪ What is the source of your strength to face the future? ▪ Are you involved/connected with a faith community? ▪ If answers yes to above question…How has your current health problem affected your spiritual; beliefs? • Knowledge and education about what is taking place and what the care priorities will be in the days ahead o The nurse can integrate patient/family education naturally while providing care by simply explaining at their level everything that the nurse/physician has ordered and WHY it needs to be done. This is why it is essential for the nurse to know and DEEPLY understand the rationale for both the physician and nursing plan of care; so it can be readily taught and explained to the patient/family at a level they can understand. 3. What is the patient likely experiencing/feeling right now in this situation? Because there is no cure for HIV, a diagnosis of HIV/AIDS is psychologically devastating to patients. The majority of patients are 15-45 years of age and have not previously confronted issues of mortality. HIV also carries a social stigma that may result in rejection by family and friends and social isolation at a time when the patient faces issues of grief and fear of dying and may also need assistance in complying with the treatment of maintaining self-care. © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com) lOMoARcPSD|3134418 4. What can you do to engage yourself with this patient’s experience, and show that she matters to you as a person? Regardless of the clinical setting, remember the importance of touch and your presence as you provide care. If you are using Swanson’s Caring framework (which I encourage you to do–see my “Teaching Caring” tab on KeithRN.com), the following practical caring interventions can be “tools” in your caring toolbox to use depending on the circumstance and the patient needs (Swanson, 1991) o Comforting ▪ Little things to comfort–whatever it may be–are needed and appreciated! i.e., hand or foot massage for pain control o Anticipating their needs ▪ Staying one step ahead and not behind, especially in a crisis, is essential! Is everything where the patient can reach it before you leave the room? o Performing competently/skillfully ▪ Remember that when a nurse or student nurse do their job well and competently, this demonstrates caring for the patient! o Preserving dignity ▪ Maintaining privacy at all times is essential and is all too easily forgotten because of the pressing physical needs that may be present. Pulling the curtain as well as covering exposed genitalia is all that is needed. They are little things, but so important to preserve human dignity. Accomplishing bodily functions which are disrupted by someone else present is significant. Be respectful of privacy issues. o Informing/explaining–patient education ▪ Even in a crisis, simply explain all that you are doing. If your patient is not able to respond but family is present, explaining to them all that you are doing and why. This is truly the “art” of nursing and makes such a difference when done in practice! Use Reflection to THINK Like a Nurse Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to intervention at the moment as the events are unfolding to make a correct clinical judgment. 1. What did I learn from this scenario? Have students share and reflect 2. How can I use what has been learned from this scenario to improve patient care in the future? Have students share and reflect Author Yolanda Simental, MSN, RN, CNS, CNE Reviewers Keith Rischer, RN, MA, CEN, CCRN Allison Shields, RN, MS, Nursing faculty, Fitchburg State University, Fitchburg, Massachusetts References Ignatavicius, D., Workman, L. (2016). Medical Surgical Nursing Patient Centered Collaborative Care. (8th ed.) St. Louis, Missouri; Elsevier. Manual of Medical-Surgical Nursing, 7th ed. (Clinical Key for Nursing) Swanson, K.M. (1991). Empirical development of a middle range theory of caring. Nursing Research, 40(3), 161–166. Tanner, C. A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45(6), 204–211. Vallerand, A.H., Sanoski, C.A., & Deglin, J.H. (2014) Davis’s drug guide for nurses. (14th ed.). Philadelphia, PA: F.A. Davis Company. Van Leeuwen, A. & Bladh, M.L. (2015). Davis’s comprehensive handbook of laboratory and diagnostic tests with nursing implications. (6th ed.). Philadelphia, PA: F.A. Davis Company. © 2018 Keith Rischer/www.KeithRN.com Downloaded by Danica Mijovic (danicamijovic@gmail.com)