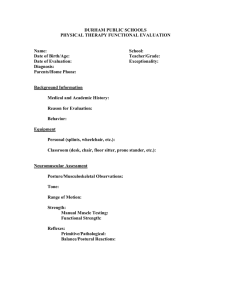
Neuroscience Letters 737 (2020) 135304 Contents lists available at ScienceDirect Neuroscience Letters journal homepage: www.elsevier.com/locate/neulet Review article Alterations of neuromuscular junctions in Duchenne muscular dystrophy Richard M. Lovering a, b, *, Shama R. Iyer a, Benjamin Edwards c, Kay E. Davies c a Departments of Orthopaedics and Physiology, University of Maryland School of Medicine, Baltimore, MD, USA University of Maryland School of Medicine, Baltimore, MD, USA c MDUK Oxford Neuromuscular Centre, Department of Physiology, Anatomy and Genetics, University of Oxford, Oxford, UK b A R T I C L E I N F O A B S T R A C T Keywords: mdx NMJ Duchenne muscular dystrophy Eccentric injury The focus of this review is on Duchenne muscular dystrophy (DMD), which is caused by the absence of the protein dystrophin and is characterized as a neuromuscular disease in which muscle weakness, increased sus­ ceptibility to muscle injury, and inadequate repair appear to underlie the pathology. Considerable attention has been dedicated to studying muscle fiber damage, but data show that both human patients and animal models for DMD present with fragmented neuromuscular junction (NMJ) morphology. In addition to pre- and post-synaptic abnormalities, studies indicate increased susceptibility of the NMJ to contraction-induced injury, with corre­ sponding functional changes in neuromuscular transmission and nerve-evoked electromyographic activity. Such findings suggest that alterations in the NMJ of dystrophic muscle may play a role in muscle weakness via impairment of neuromuscular transmission. Further work is needed to fully understand the role of the NMJ in the weakness, susceptibility to injury, and progressive wasting associated with DMD. 1. Introduction The area of synaptic contact between motor neurons and their target muscle fibers is the neuromuscular junction (NMJ). This synapse occurs at a specialized area of the sarcolemma called the end-plate. The “pretzel-shape” of a typical, healthy end-plate in mammalian muscle (Fig. 1) results from the several twisting branches of the motor neuron. The distal aspect of each branch is enlarged and these expansions form the terminal synaptic boutons, which contain synaptic vesicles filled with the neurotransmitter, acetylcholine (ACh). Boutons are located over invaginations of the sarcolemma called junctional folds [89], at the top of which high-density clusters of acetylcholine receptors (AChRs) reside. When released into the synaptic cleft, ACh binds to its post-synaptic receptors, causing an end-plate potential (EPP), a local depolarization spreading along the muscle fiber as a conducted action potential. Accumulating evidence has made it clear that the NMJ in mature skeletal muscle is not a fixed permanent structure [27,28], but instead is continually remodeling, thereby possessing a large degree of functional plasticity [30]. The morphology and physiology of the NMJ can display alterations in synaptic organization due to exercise [26,89], inactivity [66,67,83], denervation [49,92], aging [24,41,76], crushing of the nerve/muscle [44,80], or the absence of associated proteins [1,3,16,45, 48]. Ultrastructural changes in the NMJ have been documented following muscle disuse and nerve injury or denervation [9,49]. The motor end-plate (the post-synaptic membrane of NMJ) is a specialized area of the sarcolemma that rapidly and consistently re­ sponds to release of a neurotransmitter from the overlying nerve ter­ minal. Neuromuscular transmission is normally highly reliable, as each nerve impulse results in the release of more neurotransmitter (acetyl­ choline) than is required for evoking an action potential in the muscle fiber. This release of surplus transmitter and consequent excess depo­ larization of the postsynaptic membrane via AChRs is often referred as the ‘safety factor’ [91], which ensures that a post-synaptic action po­ tential will occur in response to each nerve impulse, at least in healthy tissue. Proper development and organization at the NMJ is necessary for effective neuromuscular transmission [79,90], but a number of patho­ logical conditions affecting the distribution of AChRs can lead to a reduction in the safety factor and impairment of neuromuscular trans­ mission [63,91]. Although there are diseases caused by defective syn­ aptic transmission at the NMJ (congential myasthenic syndromes)[61], this review focuses on muscular dystrophies, specifically Duchenne muscular dystrophy. 2. NMJ morphology is altered in muscular dystrophy Duchenne muscular dystrophy (DMD), the most common and severe form of muscular dystrophy, is caused by the absence of dystrophin, a * Corresponding author at: University of Maryland School of Medicine, Department of Orthopaedics, 100 Penn St., AHB, Room 540, Baltimore, MD21201USA. E-mail address: rlovering@som.umaryland.edu (R.M. Lovering). https://doi.org/10.1016/j.neulet.2020.135304 Received 30 April 2020; Received in revised form 9 August 2020; Accepted 11 August 2020 Available online 17 August 2020 0304-3940/© 2020 Elsevier B.V. All rights reserved. R.M. Lovering et al. Neuroscience Letters 737 (2020) 135304 structural protein found on the cytoplasmic surface of the sarcolemma. Dystrophin is the central component of a molecular link that connects the contractile apparatus inside the muscle fiber to the extracellular matrix outside the muscle fiber, and binds directly or indirectly to a group of proteins at the sarcolemma collectively known as the dystrophin-associated protein complex (DAPC or DPC) or the dystrophin-glycoprotein complex (DGC). The DGC of the sarcolemma accumulates at the post-synaptic membrane (motor end-plate) of the NMJ, and the absence of associ­ ated proteins can cause changes in NMJ structure and function [6]. The NMJ is noticeably disrupted in muscles from mdx and other DMD mouse models [3,43,55,82]. Dystrophin appears to be involved in synaptic homeostasis [64]; it is not required for NMJ formation, but is required for endplate maintenance [45] and likely for endplate remodeling in regenerating fibers. dx mice show NMJ fragmentation in adult muscle fibers and excessive nerve sprouting compared to wild-type mice [56], and ultrastructural studies using electron microscopy indicate a loss in the number and depth of synaptic folds of the motor end-plate in mdx muscles [3,55]. Patients with DMD and mdx mice have muscles with weakness and increased susceptibility to injury compared to their non-dystrophic counterparts. Over time, this damage/degeneration exceeds the ability to repair/regenerate muscle, leading to irreversible muscle wasting throughout life. The increased force loss after contraction-induced injury is typically attributed to structural weakness of the muscle fiber cytoskeleton and changes in signaling within muscle fibers secondary to the loss of dystrophin [53]. However, studies have reported that loss in whole muscle function after injury is also associated with alterations in NMJ end-plate morphology in mdx mice [68–70]. Some studies report strong evidence showing that disrupted NMJ morphology is the conse­ quence of muscle fiber degeneration and regeneration [37,50,51,59], but others have suggested that NMJ fragmentation in mdx muscle is independent of degeneration and regeneration [3,46]. In support of the latter, NMJ post-synaptic morphology, including AChR area, is normal in fibers of muscle subjected to toxin-induced degeneration [75,88]. It is thought that the motor neuron in DMD and mdx mice is unaffected, except for axonal sprouting near the NMJ and changes in the terminal bouton. However, recent data suggest that the persistent, chronic NMJ remodeling that occurs over the lifespan of the mdx mouse can adversely affect the motor neuron [47]. Utrophin, short for “ubiquitous dystrophin,” is a protein highly ho­ mologous to dystrophin [52]. During fetal muscle development, utro­ phin is found along the entire muscle sarcolemma. Once dystrophin is expressed, however, utrophin disappears from most of the sarcolemmal membrane so that, in normal adult muscle, it is located only at the neuromuscular and myotendinous junctions [85]. One reason mdx mice do not display pathology equivalent to that seen in DMD may be that utrophin is up-regulated to levels sufficient to compensate, in part, for Fig. 1. Top panels show representative images of neuromuscular junctions (NMJ) stained with α-bungarotoxin conjugated to Alexa-594 in muscles from WT (wild type), mdx (lacking dystrophin), dko (double knockout, lacking both dystrophin and utrophin), and Fiona (lacking dystrophin but upregulation of utrophin) mice. Bottom panels show representative skeletonized images of the corresponding NMJ. Total stained area, total stained perimeter, total area, and total perimeter were calculated using binarized images using Image J. Dispersion index was calculated by total stained area/total area, and is a measure of density of acetylcholine receptors. Discontinuity and number of branching were calculated using the skeletonized images. Number of clusters was calculated by counting the number of separate acetylcholine receptor aggregates. * indicates significant difference from WT, # indicated significant difference from Fiona, p < 0.05; one-way ANOVA, approximately 10 NMJs in each genotype, with 5 muscles analyzed). 2 R.M. Lovering et al. Neuroscience Letters 737 (2020) 135304 the lack of dystrophin. Although studies have suggested that NMJ disruption is not dependent on utrophin [88], NMJ morphology appears more disrupted when dystrophin and utrophin are absent [74], and the upregulation of utrophin (through artificial transcription factors) ap­ pears to rescue NMJ morphology [65]. In the Fiona mouse, a transgenic mdx mouse in which utrophin is upregulated in skeletal muscles, using established methods [68–71] (detailed methods in supplemental material) we have found a partial rescue of NMJ morphology (Fig. 1). Muscles from mice that lack genes for other components of the DGC, such as α-dystrobrevin, dystroglycan, or syntrophin, have altered NMJ morphology [1,6,33,35,39], even though absence of other DGC com­ ponents, such as α- or ϒ-sarcoglycan, does not appear to affect NMJ morphology [23,36]. Aberrations in NMJ morphology have also been observed in laminopathies, which are typically caused by mutations in the LMNA gene, resulting in cardiac and skeletal disorders. Patients often have abnormal EMG, indicating myopathy [8,58]. In mouse models with LMNA mutations, NMJ morphology is disorganized and fragmented, with mislocalized synaptic nuclei [58]. Furthermore, the NMJ disorganization was observed before myopathic phenotype, furthering the notion of NMJ aberrations as a driver of disease phenotype. proximal muscles have attributed reduced muscle excitability to changes in the NMJ [68,69]. Synaptic transmission becomes more variable with age in the mdx mouse model of DMD [12,44], which could provide one explanation why, despite the consistent lack of dystrophin, mdx skeletal muscle generates less specific force and becomes more susceptible to damage with age [15]. EMG changes are measurable in patients with various muscular dystrophies, including DMD [18,31,72]. Some animal studies report changes in EMG activity between WT and mdx mice [38,68], while others do not [13]. The study of different muscles might be one reason for such conflicting data; for example, proximal muscles are affected earlier and to a greater extent in DMD [17,57] and a similar pattern of increased damage in more proximal muscles has been docu­ mented in young mdx mice [60]. Patients with DMD have similar intramuscular fatigability, neuro­ muscular transmission, and central activation as controls [81]. Such observations might argue against a significant role for NMJ dysfunction in DMD in the absence of injury, however increased sensitivity to neuromuscular blocking drugs (and a slower recovery from them) in­ dicates NMJ is vulnerable in DMD, with more obvious findings in older-aged and ambulatory patients with DMD [88]. Furthermore, although the reduced safety factor and miniature end-plate potentials might not be sufficient to result in overt changes to the compound muscle action potentials (CMAPs), they could render the NMJ dysfunctional under certain intense activity [88]. 3. Disrupted NMJ morphology in dystrophic muscle contributes to impairment of nerve-evoked muscle contraction Structure is clearly a major determinant of function: as the devel­ opment of force relies on the controlled overlap of actin and myosin, so does effective neuromuscular transmission on the apposition of the nerve terminal and the underlying motor end-plate [79,90]. Moreover, maintenance of the neuromuscular apparatus relies on bidirectional communication between muscle and nerve [34]. However, several pathological conditions affecting the distribution of AChRs can lead to a reduction in the safety factor and impairment of neuromuscular trans­ mission [63]. The increased muscle weakness and susceptibility to injury (exag­ gerated loss in force to a mechanical insult) in patients with DMD and in the mdx murine model, is hypothesized to be due to structural weakness of the cytoskeleton or changes in signaling secondary to the loss of dystrophin [53], but additional mechanisms are still being clarified. A mechanical model [4,7] suggests that the absence of dystrophin results in structural fragility of the cytoskeleton [53]. In an attempt to under­ stand mechanisms underlying muscle weakness, much of the focus has been on structural damage within the myofiber. The NMJ is clearly disrupted in muscles from DMD mouse models and associated deficits in neuromuscular function have now also been identified [3,14]. We have reported that loss in whole muscle contractile force after muscle injury in mdx mice is also associated with alterations in NMJ morphology, such as increased discontinuity and branching, and corresponding aberrant synaptic transmission, such as decreased EMG amplitudes and increased neuromuscular transmission failure [68–70]. Other groups have also shown disruption at the NMJ in dystrophic mouse muscles with corre­ sponding changes in function, such as reduced amplitude of miniature endplate potentials, reduction of postsynaptic sensitivity for the neurotransmitter acetylcholine and exhaustion of presynaptic acetyl­ choline release during intense synaptic activity [88]. After contraction-induced injury, there is a loss of force in both the WT and mdx muscles, but only mdx mice show significant additional changes in NMJ morphology, neuromuscular transmission, and EMG activity [68, 69]. Although other factors, such as sarcolemma damage could be a factor, these findings suggest that NMJ structural and functional changes may contribute to the greater force loss seen after injury in dystrophic muscle. While some studies attribute changes in myofiber action potential conductivity as the primary reason for reduced muscle excitability in mdx muscles after injury, these studies typically utilize a low-strain, high-repetition injury protocol in distal muscles [5,11,77]; other studies utilizing a high-strain, lower repetition injury protocol in 4. Therapeutic approaches to affect NMJ form and function Several approaches of gene therapy are being examined to amelio­ rate the pathophysiology that results from the absence of dystrophin. Although transgenic expression of a short isoform of dystrophin in mdx muscle can prevent muscle degeneration, NMJ morphology remains fragmented [3]. Indeed, the threshold of dystrophin lies between 19% and 50% for correction of NMJ morphology in muscles of mdx mice [87]. Muscle-specific Kinase (MuSK) is a transmembrane tyrosine kinase crucial for forming and maintaining the NMJ, and activation of the MuSK complex that drives AChR clustering [10,32]. MuSK inactivation at the NMJ of adult muscle is known to cause a reduction in AChR density and a change in the gross synaptic arborization of the endplate, which can lead to the complete loss of AChRs and disappearance of the synaptic structure [40]. MuSK levels differ between various adult skel­ etal muscles, which may correlate with muscle specific differences in the response to agrin [25,73]. In our previous work, we assessed transcripts for the multi-protein MuSK signaling complex responsible for AChR clustering in WT and mdx mice [69]; interestingly, the only significant difference between WT and mdx muscleswas a decrease in MuSK inthe latter. Since MuSK plays a critical role in the aggregation, or clustering, of AChRs, it is conceivable that this reduction directly contributes to the altered morphology of mdx NMJs and is therefore a potential therapeutic target. Indeed, increasing expression of MuSK or rapsyn (a cytoplasmic MuSK effector protein) with adeno-associated viral vectors protected mdx muscles from contraction-induced injury [86]. Utrophin upregulation results in a positive effect on NMJ postsynaptic morphology, including an increase in the number of AChRs and improved NMJ morphology [65]. This is accompanied by an improvement in muscle contractility, but it is difficult to tease apart the contribution of the NMJ versus other changes in the cell (e.g., improvement in sarcolemma stability, mechanotransduction of force, etc.). Interestingly, drugs commonly used for myasthenia gravis and myasthenic syndromes (autoimmune disease and inherited conditions, respectively, affecting the NMJ) do not seem to have a significant benefit for muscular dystrophies. Exercise can exert beneficial effects not only on muscle, but also to the NMJ morphology and function [22,78]. Endurance training affects the morphology of NMJs in young adults, and has been studied as a measure to counter changes in the NMJ with aging [2]. Specific 3 R.M. Lovering et al. Neuroscience Letters 737 (2020) 135304 adaptations to exercise training include increases in the length and number of nerve terminal branches, a higher number of pre-synaptic vesicles, and increase number and distribution of AChRs [20,22,78, 89]. Thus, the benefits attained from endurance training are likely beyond just muscle fiber remodeling and extend to the NMJ. Exercise can induce activation of neurotrophic factors and other molecules, which have a positive impact on NMJ morphology [29,62]. Further­ more, alterations of structure induced by endurance training are asso­ ciated with significant NMJ functional changes, such as synaptic transmission. Resistance exercise appears to yield similar benefits for the NMJ, but to a lesser degree [19,21]. It is established that heavy resistance training has deleterious effects on dystrophic skeletal muscle, particularly if it involves eccentric con­ tractions [54]; in addition to the risk of further muscle damage, there is no evidence of beneficial adaptation to heavy resistance training in dystrophic animals, or in humans with muscular dystrophy. Although historically exercise has been used sparingly in the treatment of muscular dystrophies, evidence suggests beneficial impact from mod­ erate exercise [42]. Several well-controlled studies indicate that light to moderate exercise can have beneficial effects in patients with muscular dystrophies, such as increased strength. Unfortunately, there are rela­ tively few controlled studies available that are easily translated to the human population. There is therefore a great need for careful studies to determine the forms of exercise that are most beneficial to patients with different types of muscle diseases, and the effects of exercise on the NMJ in dystrophic muscle. Appendix A. Supplementary data Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.neulet.2020.135304. References [1] M.E. Adams, N. Kramarcy, S.P. Krall, S.G. Rossi, R.L. Rotundo, R. Sealock, S. C. Froehner, Absence of alpha-syntrophin leads to structurally aberrant neuromuscular synapses deficient in utrophin, J.Cell Biol. 150 (2000) 1385–1398. [2] M.H. Andonian, M.A. Fahim, Effects of endurance exercise on the morphology of mouse neuromuscular junctions during ageing, J. Neurocytol. 16 (1987) 589–599. [3] G.B. Banks, J.S. Chamberlain, S.C. Froehner, Truncated dystrophins can influence neuromuscular synapse structure 1, Mol.Cell Neurosci. 40 (2009) 433–441. [4] C.L. Batchelor, S.J. Winder, Sparks, signals and shock absorbers: how dystrophin loss causes muscular dystrophy, Trends Cell Biol. 16 (2006) 198–205. [5] C.W. Baumann, G.L. Warren, D.A. Lowe, Plasmalemma function Is rapidlyrestored in mdxmuscle after eccentriccontractions, Med. Sci. Sports Exerc. 52 (2020) 354–361. [6] D.C. Belhasan, M. Akaaboune, The role of the dystrophin glycoprotein complex on the neuromuscular system, Neurosci. Lett. 722 (2020) 134833. [7] R.J. Bloch, H. Gonzalez-Serratos, Lateral force transmission across costameres in skeletal muscle, Exerc. Sport Sci. Rev. 31 (2003) 73–78. [8] G. Bonne, S. Quijano-Roy, Emery-Dreifuss muscular dystrophy, laminopathies, and other nuclear envelopathies, Handb. Clin. Neurol. 113 (2013) 1367–1376. [9] M.C. Brown, W.G. Hopkins, R.J. Keynes, Importance of pathway formation for nodal sprout production in partly denervated muscles 15, Brain Res. 243 (1982) 345–349. [10] S.J. Burden, SnapShot: neuromuscular Junction 7, Cell 144 (2011), 826-826. [11] J.A. Call, G.L. Warren, M. Verma, D.A. Lowe, Acute failure of action potential conduction in mdx muscle reveals new mechanism of contraction-induced force loss 1, J. Physiol 591 (2013) 3765–3776. [12] C.G. Carlson, D.M. Roshek, Adult dystrophic (mdx) endplates exhibit reduced quantal size and enhanced quantal variation 2, Pflugers Arch. 442 (2001) 369–375. [13] G.T. Carter, K.J. Longley, R.K. Entrikin, Electromyographic and nerve conduction studies in the mdx mouse 2, Am. J. Phys. Med. Rehabil. 71 (1992) 2–5. [14] J.S. Chamberlain, J. Metzger, M. Reyes, D. Townsend, J.A. Faulkner, Dystrophindeficient mdx mice display a reduced life span and are susceptible to spontaneous rhabdomyosarcoma 3, FASEB J. 21 (2007) 2195–2204. [15] S. Chan, S.I. Head, J.W. Morley, Branched fibers in dystrophic mdx muscle are associated with a loss of force following lengthening contractions, Am. J. Physiol Cell Physiol. 293 (2007) C985–C992. [16] P.H. Chipman, C.K. Franz, A. Nelson, M. Schachner, V.F. Rafuse, Neural cell adhesion molecule is required for stability of reinnervated neuromuscular junctions 1, Eur. J. Neurosci. 31 (2010) 238–249. [17] D. Cros, P. Harnden, J.F. Pellissier, G. Serratrice, Muscle hypertrophy in duchenne muscular dystrophy. a pathological and morphometric study 1, J. Neurol. 236 (1989) 43–47. [18] K.L. Derry, S.L. Venance, T.J. Doherty, Decomposition-based quantitative electromyography in the evaluation of muscular dystrophy severity 1, Muscle Nerve 45 (2012) 507–513. [19] M.R. Deschenes, D.A. Judelson, W.J. Kraemer, V.J. Meskaitis, J.S. Volek, B. C. Nindl, F.S. Harman, D.R. Deaver, Effects of resistance training on neuromuscular junction morphology, Muscle Nerve 23 (2000) 1576–1581. [20] M.R. Deschenes, C.M. Maresh, L.E. Armstrong, J. Covault, W.J. Kraemer, J. F. Crivello, Endurance and resistance exercise induce muscle fiber type specific responses in androgen binding capacity, J. Steroid Biochem. Mol. Biol. 50 (1994) 175–179. [21] M.R. Deschenes, C.M. Maresh, J.F. Crivello, L.E. Armstrong, W.J. Kraemer, J. Covault, The effects of exercise training of different intensities on neuromuscular junction morphology, J. Neurocytol. 22 (1993) 603–615. [22] M.R. Deschenes, M.A. Roby, E.K. Glass, Aging influences adaptations of the neuromuscular junction to endurance training, Neuroscience 190 (2011) 56–66. [23] F. Duclos, V. Straub, S.A. Moore, D.P. Venzke, R.F. Hrstka, R.H. Crosbie, M. Durbeej, C.S. Lebakken, A.J. Ettinger, M.J. van der, K.H. Holt, L.E. Lim, J. R. Sanes, B.L. Davidson, J.A. Faulkner, R. Williamson, K.P. Campbell, Progressive muscular dystrophy in alpha-sarcoglycan-deficient mice, J. Cell Biol. 142 (1998) 1461–1471. [24] M.K. Elkerdany, M.A. Fahim, Age changes in neuromuscular junctions of masseter muscle 9, Anat. Rec. 237 (1993) 291–295. [25] A. Eusebio, F. Oliveri, P. Barzaghi, M.A. Ruegg, Expression of mouse agrin in normal, denervated and dystrophic muscle 1, Neuromuscul. Disord. 13 (2003) 408–415. [26] M.A. Fahim, Endurance exercise modulates neuromuscular junction of C57BL/ 6NNia aging mice 1, J. Appl. Physiol. 83 (1997) 59–66. [27] D.M. Fambrough, Control of acetylcholine receptors in skeletal muscle 7, Physiol. Rev. 59 (1979) 165–227. [28] D.M. Fambrough, P.N. Devreotes, J.M. Gardner, D.J. Card, The life history of acetylcholine receptors 6, Prog. Brain Res. 49 (1979) 325–334. [29] L. Ferraiuolo, J.P. De Bono, P.R. Heath, H. Holden, P. Kasher, K.M. Channon, J. Kirby, P.J. Shaw, Transcriptional response of the neuromuscular system to exercise training and potential implications for ALS, J. Neurochem. 109 (2009) 1714–1724. 5. Conclusions Knowledge of NMJ dysfunction in DMD animal models is incom­ plete, and sometimes conflicting, but findings suggest that, in addition to mechanical damage to the myofiber, structural and functional changes at the NMJ may be another contributor to the greater force loss seen after injury in dystrophic muscle. In terms of functional impact, the relative roles of muscle fiber injury, degeneration, and denervation that contribute to the changes seen in NMJ morphology of dystrophic mus­ cles are not yet known, but will be important to determine, as NMJ dysfunction is fundamental to understanding impairment of muscle. The notion that structure determines function is a key tenet in biology, yet it is possible that disruption of NMJ morphology in dystrophic muscle represents an effective repair process that maintains efficacy; there is still no clear evidence showing correlation between the degree of NMJ fragmentation and the efficacy of transmission [84]. Continued experi­ mentation is paramount for elucidating mechanisms underlying the dystrophic progression. The specific role of the NMJ in neuromuscular health and its relationship to dystrophy is still being defined, but the NMJ might play a role in the exacerbated response to injury. The electrophysiological NMJ features of one muscle might not necessarily be identical in all skeletal muscles [88], but there is now sound evidence indicating a role for the NMJ in muscle weakness, sus­ ceptibility to damage, and loss of functional performance in dystrophic muscle. Future work is needed to systematically study constituents of the MuSK signaling complex, compare various muscles, and to follow the morphology and function of the NMJ at various time points after injury and throughout the lifespan. Funding This work was supported by grants to RML from the National In­ stitutes of Health (R56AR073193), to SRI from the National Institutes of Health (K01AR074048) and the Muscular Dystrophy Association development grant (MDA 577897), and to KD from the Medical Research Council, UK 4 R.M. Lovering et al. Neuroscience Letters 737 (2020) 135304 [59] E. Minatel, N.H. Santo, M.J. Marques, Acetylcholine receptors and neuronal nitric oxide synthase distribution at the neuromuscular junction of regenerated muscle fibers 1, Muscle Nerve 24 (2001) 410–416. [60] F. Muntoni, A. Mateddu, F. Marchei, A. Clerk, G. Serra, Muscular weakness in the mdx mouse 2, J. Neurol.Sci. 120 (1993) 71–77. [61] S. Nicole, Y. Azuma, S. Bauche, B. Eymard, H. Lochmuller, C. Slater, Congenital myasthenicsyndromes or inheriteddisorders of neuromusculartransmission: recentdiscoveries and Open questions, J. Neuromuscul. Dis. 4 (2017) 269–284. [62] H. Nishimune, J.A. Stanford, Y. Mori, Role of exercise in maintaining the integrity of the neuromuscular junction, Muscle Nerve 49 (2014) 315–324. [63] K.E. Personius, R.P. Sawyer, Variability and failure of neurotransmission in the diaphragm of mdx mice, Neuromuscul. Disord. 16 (2006) 168–177. [64] G.S. Pilgram, S. Potikanond, R.A. Baines, L.G. Fradkin, J.N. Noordermeer, The roles of the dystrophin-associated glycoprotein complex at the synapse, Mol. Neurobiol. 41 (2010) 1–21. [65] C. Pisani, G. Strimpakos, F. Gabanella, M.G. Di Certo, A. Onori, C. Severini, S. Luvisetto, S. Farioli-Vecchioli, I. Carrozzo, A. Esposito, T. Canu, E. Mattei, N. Corbi, C. Passananti, Utrophin up-regulation by artificial transcription factors induces muscle rescue and impacts the neuromuscular junction in mdx mice, Biochim. Biophys. Acta Mol. Basis Dis. 1864 (2018) 1172–1182. [66] Y.S. Prakash, H. Miyata, W.Z. Zhan, G.C. Sieck, Inactivity-induced remodeling of neuromuscular junctions in rat diaphragmatic muscle 1, Muscle Nerve 22 (1999) 307–319. [67] Y.S. Prakash, W.Z. Zhan, H. Miyata, G.C. Sieck, Adaptations of diaphragm neuromuscular junction following inactivity 4, Acta Anat. (Basel) 154 (1995) 147–161. [68] S.J. Pratt, S.B. Shah, C.W. Ward, M.P. Inacio, J.P. Stains, R.M. Lovering, Effects of in vivo injury on the neuromuscular junction in healthy and dystrophic muscles 1, J. Physiol. 591 (2013) 559–570. [69] S.J. Pratt, S.B. Shah, C.W. Ward, J.P. Kerr, J.P. Stains, R.M. Lovering, Recovery of altered neuromuscular junction morphology and muscle function in mdx mice after injury, Cell Mol. Life Sci. (2014). [70] S.J. Pratt, A.P. Valencia, G.K. Le, S.B. Shah, R.M. Lovering, Pre- and postsynaptic changes in the neuromuscular junction in dystrophic mice, Front. Physiol. 6 (2015) 252. [71] S.J.P. Pratt, S.R. Iyer, S.B. Shah, R.M. Lovering, Imaging analysis of the neuromuscular Junction in dystrophicmuscle, Methods Mol.Biol. 1687 (2018) 57–72. [72] A. Priez, J. Duchene, F. Goubel, Duchenne muscular dystrophy quantification: a multivariate analysis of surface EMG 1, Med. Biol. Eng. Comput. 30 (1992) 283–291. [73] A.R. Punga, M. Maj, S. Lin, S. Meinen, M.A. Ruegg, MuSK levels differ between adult skeletal muscles and influence postsynaptic plasticity 3, Eur. J. Neurosci. 33 (2011) 890–898. [74] J.A. Rafael, E.R. Townsend, S.E. Squire, A.C. Potter, J.S. Chamberlain, K.E. Davies, Dystrophin and utrophin influence fiber type composition and post-synaptic membrane structure, Hum. Mol. Genet. 9 (2000) 1357–1367. [75] M. Rich, J.W. Lichtman, Motor nerve terminal loss from degenerating muscle fibers, Neuron 3 (1989) 677–688. [76] N. Robbins, Compensatory plasticity of aging at the neuromuscular junction 10, Exp. Gerontol. 27 (1992) 75–81. [77] P. Roy, F. Rau, J. Ochala, J. Messeant, B. Fraysse, J. Laine, O. Agbulut, G. ButlerBrowne, D. Furling, A. Ferry, Dystrophin restoration therapy improves both the reduced excitability and the force drop induced by lengthening contractions in dystrophic mdx skeletal muscle, Skelet Muscle 6 (2016) 23. [78] R. Rudolf, M.M. Khan, S. Labeit, M.R. Deschenes, Degeneration of neuromuscular junction in age and dystrophy, Front. Aging Neurosci. 6 (2014) 99. [79] J.R. Sanes, J.W. Lichtman, Development of the vertebrate neuromuscular junction, Annu. Rev. Neurosci. 22 (1999) 389–442. [80] N.H. Santo, A.J. Martins, E. Minatel, M.J. Marques, Axonal sprouting in mdx mice and its relevance to cell and gene mediated therapies for Duchenne muscular dystrophy 1, Neurosci. Lett. 343 (2003) 67–69. [81] K.R. Sharma, M.A. Mynhier, R.G. Miller, Muscular fatigue in duchenne muscular dystrophy, Neurology 45 (1995) 306–310. [82] T. Shiao, A. Fond, B. Deng, M. Wehling-Henricks, M.E. Adams, S.C. Froehner, J. G. Tidball, Defects in neuromuscular junction structure in dystrophic muscle are corrected by expression of a NOS transgene in dystrophin-deficient muscles, but not in muscles lacking alpha- and beta1-syntrophins 1, Hum. Mol.Genet. 13 (2004) 1873–1884. [83] D.C. Sieck, W.Z. Zhan, Y.H. Fang, L.G. Ermilov, G.C. Sieck, C.B. Mantilla, Structureactivity relationships in rodent diaphragm muscle fibers vs. Neuromuscular junctions 1, Respir. Physiol. Neurobiol. 180 (2012) 88–96. [84] C.R. Slater, ’Fragmentation’ of NMJs: a sign of degeneration or regeneration? A long journey with many junctions, Neuroscience 439 (2020) 28–40. [85] J. Tinsley, N. Deconinck, R. Fisher, D. Kahn, S. Phelps, J.M. Gillis, K. Davies, Expression of full-length utrophin prevents muscular dystrophy in mdx mice, Nat. Med. 4 (1998) 1441–1444. [86] S. Trajanovska, J. Ban, J. Huang, P. Gregorevic, M. Morsch, D.G. Allen, W. D. Phillips, Muscle specific kinase protects dystrophic mdx mouse muscles from eccentric contraction-induced loss of force-producing capacity, J. Physiol. 597 (2019) 4831–4850. [87] E.M. van der Pijl, M. van Putten, E.H. Niks, J. Verschuuren, A. Aartsma-Rus, J. J. Plomp, Low dystrophin levels are insufficient to normalize the neuromuscular synaptic abnormalities of mdx mice, Neuromuscul. Disord. 28 (2018) 427–442. [88] E.M. van der Pijl, M. van Putten, E.H. Niks, J.J. Verschuuren, A. Aartsma-Rus, J. J. Plomp, Characterization of neuromuscular synapse function abnormalities in [30] J. Ferre, E. Mayayo, R. Brunet, Morphometric study of the neuromuscular synapses in the adult rat with special reference to the remodelling concept 1, Biol. Cell 60 (1987) 133–144. [31] M. Frascarelli, L. Rocchi, I. Feola, EMG computerized analysis of localized fatigue in Duchenne muscular dystrophy 3, Muscle Nerve 11 (1988) 757–761. [32] N. Ghazanfari, K.J. Fernandez, Y. Murata, M. Morsch, S.T. Ngo, S.W. Reddel, P. G. Noakes, W.D. Phillips, Muscle specific kinase: organiser of synaptic membrane domains 1, Int. J. Biochem. Cell Biol. 43 (2011) 295–298. [33] R.M. Grady, H. Zhou, J.M. Cunningham, M.D. Henry, K.P. Campbell, J.R. Sanes, Maturation and maintenance of the neuromuscular synapse: genetic evidence for roles of the dystrophin–glycoprotein complex, Neuron 25 (2000) 279–293. [34] A.D. Grinnell, Dynamics of nerve-muscle interaction in developing and mature neuromuscular junctions 1, Physiol. Rev. 75 (1995) 789–834. [35] J.D. Gumerson, C.S. Davis, Z.T. Kabaeva, J.M. Hayes, S.V. Brooks, D.E. Michele, Muscle-specific expression of LARGE restores neuromuscular transmission deficits in dystrophic LARGE(myd) mice, Hum. Mol. Genet. 22 (2013) 757–768. [36] A.A. Hack, C.T. Ly, F. Jiang, C.J. Clendenin, K.S. Sigrist, R.L. Wollmann, E. M. McNally, Gamma-sarcoglycan deficiency leads to muscle membrane defects and apoptosis independent of dystrophin, J.Cell Biol. 142 (1998) 1279–1287. [37] S.G. Haddix, Y.I. Lee, J.N. Kornegay, W.J. Thompson, Cycles of myofiber degeneration and regeneration lead to remodeling of the neuromuscular junction in two mammalian models of Duchenne muscular dystrophy, PLoS One 13 (2018) e0205926. [38] J.J. Han, G.T. Carter, J.J. Ra, R.T. Abresch, J.S. Chamberlain, L.R. Robinson, Electromyographic studies in mdx and wild-type C57 mice 3, Muscle Nerve 33 (2006) 208–214. [39] R. Herbst, T. Iskratsch, E. Unger, R.E. Bittner, Aberrant development of neuromuscular junctions in glycosylation-defective large(myd) mice, Neuromuscul. Disord. 19 (2009) 366–378. [40] B.A. Hesser, O. Henschel, V. Witzemann, Synapse disassembly and formation of new synapses in postnatal muscle upon conditional inactivation of MuSK 1, Mol. Cell Neurosci. 31 (2006) 470–480. [41] Y.C. Jang, H. Van Remmen, Age-associated alterations of the neuromuscular junction 2, Exp. Gerontol. 46 (2011) 193–198. [42] M. Jansen, N. van Alfen, A.C. Geurts, I.J. de Groot, Assisted bicycle training delays functional deterioration in boys with Duchenne muscular dystrophy: the randomized controlled trial “no use is disuse”, Neurorehabil. Neural Repair 27 (2013) 816–827. [43] F. Jerusalem, A.G. Engel, M.R. Gomez, Duchenne dystrophy. II. Morphometric study of motor end-plate fine structure, Brain 97 (1974) 123–130. [44] M. Kawabuchi, H. Tan, S. Wang, Age affects reciprocal cellular interactions in neuromuscular synapses following peripheral nerve injury 1, Ageing Res. Rev. 10 (2011) 43–53. [45] J. Kong, J.E. Anderson, Dystrophin is required for organizing large acetylcholine receptor aggregates 1, Brain Res. 839 (1999) 298–304. [46] J. Kong, L. Yang, Q. Li, J. Cao, J. Yang, F. Chen, Y. Wang, C. Zhang, The absence of dystrophin rather than muscle degeneration causes acetylcholine receptor cluster defects in dystrophic muscle, Neuroreport 23 (2012) 82–87. [47] V.S. Krishnan, A. Aartsma-Rus, M. Overzier, C. Lutz, L. Bogdanik, M.D. Grounds, Implications of increased S100beta and Tau5 proteins in dystrophic nerves of two mdx mouse models for Duchenne muscular dystrophy, Mol. Cell. Neurosci. (2020) 103484. [48] S.A. Kulakowski, S.D. Parker, K.E. Personius, Reduced TrkB expression results in precocious age-like changes in neuromuscular structure, neurotransmission, and muscle function 1, J. Appl. Physiol 111 (2011) 844–852. [49] S.S. Labovitz, N. Robbins, M.A. Fahim, Endplate topography of denervated and disused rat neuromuscular junctions: comparison by scanning and light microscopy 1, Neuroscience 11 (1984) 963–971. [50] Y. Li, Y. Lee, W.J. Thompson, Changes in aging mouse neuromuscular junctions are explained by degeneration and regeneration of muscle fiber segments at the synapse 1, J. Neurosci. 31 (2011) 14910–14919. [51] Y. Li, W.J. Thompson, Nerve terminal growth remodels neuromuscular synapses in mice following regeneration of the postsynaptic muscle fiber 1, J. Neurosci. 31 (2011) 13191–13203. [52] D.R. Love, D.F. Hill, G. Dickson, N.K. Spurr, B.C. Byth, R.F. Marsden, F.S. Walsh, Y. H. Edwards, K.E. Davies, An autosomal transcript in skeletal muscle with homology to dystrophin, Nature 339 (1989) 55–58. [53] R.M. Lovering, L. Michaelson, C.W. Ward, Malformed mdx myofibers have normal cytoskeletal architecture yet altered EC coupling and stress-induced Ca2+ signaling, Am. J. Physiol. Cell Physiol. 297 (2009) C571–C580. [54] R.M. Lovering, N.C. Porter, R.J. Bloch, The muscular dystrophies: from genes to therapies, Phys. Ther. 85 (2005) 1372–1388. [55] P.R. Lyons, C.R. Slater, Structure and function of the neuromuscular junction in young adult mdx mice 1, J. Neurocytol. 20 (1991) 969–981. [56] M.J. Marques, A.P. Taniguti, E. Minatel, H.S. Neto, Nerve terminal contributes to acetylcholine receptor organization at the dystrophic neuromuscular junction of mdx mice 2, Anat. Rec. (Hoboken.) 290 (2007) 181–187. [57] S. Mathur, D.J. Lott, C. Senesac, S.A. Germain, R.S. Vohra, H.L. Sweeney, G. A. Walter, K. Vandenborne, Age-related differences in lower-limb muscle crosssectional area and torque production in boys with Duchenne muscular dystrophy 2, Arch. Phys. Med. Rehabil. 91 (2010) 1051–1058. [58] A. Mejat, V. Decostre, J. Li, L. Renou, A. Kesari, D. Hantai, C.L. Stewart, X. Xiao, E. Hoffman, G. Bonne, T. Misteli, Lamin A/C-mediated neuromuscular junction defects in emery-dreifuss muscular dystrophy, J. Cell Biol. 184 (2009) 31–44. 5 R.M. Lovering et al. Neuroscience Letters 737 (2020) 135304 multiple duchenne muscular dystrophy mouse models, Eur. J. Neurosci. 43 (2016) 1623–1635. [89] M.H. Wilson, M.R. Deschenes, The neuromuscular junction: anatomical features and adaptations to various forms of increased, or decreased neuromuscular activity 2, Int. J. Neurosci. 115 (2005) 803–828. [90] S.J. Wood, C.R. Slater, The contribution of postsynaptic folds to the safety factor for neuromuscular transmission in rat fast- and slow-twitch muscles, J. Physiol. 500 (Pt 1) (1997) 165–176. [91] S.J. Wood, C.R. Slater, Safety factor at the neuromuscular junction, Prog. Neurobiol. 64 (2001) 393–429. [92] R. Xu, M.M. Salpeter, Acetylcholine receptors in innervated muscles of dystrophic mdx mice degrade as after denervation 2, J.Neurosci. 17 (1997) 8194–8200. 6