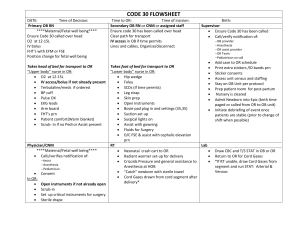
UMBILICAL CORD PROLAPSE Mariyam Riaz WHAT IS THE UMBILICAL CORD? • The umbilical cord is a flexible, tube-like structure that, during pregnancy, connects the fetus to the mother. • The umbilical cord is the baby's lifeline to the mother. • It transports nutrients to the baby and also carries away the baby's waste products. • It is made up of three blood vessels – two arteries and one vein. UMBILICAL CORD PROLAPSE • Umbilical cord prolapse occurs when the umbilical cord comes out of the uterus with or before the presenting part of the fetus. • It is a relatively rare condition and occurs in fewer than 1% of pregnancies. • Cord prolapse is more common in women who have had rupture of their amniotic sac. • Whenever there is a sudden decrease in fetal heart rate or abnormal fetal heart tracing, umbilical cord prolapse should be considered. • Due to the possibility for fetal death and other complications, umbilical cord prolapse is considered an obstetric emergency during pregnancy or labor. CLASSIFICATION There are three types of umbilical prolapse that can occur: 1. Overt umbilical cord prolapse: descent of the umbilical cord past the presenting fetal part. In this case, the cord is through the cervix and into or beyond the vagina. Overt umbilical cord prolapse requires rupture of membranes. This is the most common type of cord prolapse. 2. Occult umbilical prolapse: descent of the umbilical cord alongside the presenting fetal part, but has not advanced past the presenting fetal part. Occult umbilical prolapse can occur with both intact or ruptured membranes. 3. Funic (cord) presentation: presence of the umbilical cord between the presenting fetal part and fetal membranes. In this case, the cord has not passed the opening of the cervix. In funic presentation, the membranes are not yet ruptured. EPIDEMIOLOGY The incidence of umbilical cord prolapse ranges from 0.1-0.6% of all pregnancies. A recent study estimates 77% of cord prolapses occur in singleton pregnancies, or those where there is only one fetus. In twin pregnancies, cord prolapses occur more frequently in the second twin to be delivered, with 9% in the first twin and 14% in the second twin. PATHOGENESIS The pathogenesis of umbilical cord prolapse is not always clear. One probable mechanism is high outward flow of amniotic fluid at rupture of membranes that carries the umbilical cord past an unengaged fetal presenting part. Another probable mechanism is disengagement of the presenting part during obstetric procedures, allowing the cord to prolapse. WHAT CAUSES AN UMBILICAL CORD PROLAPSE? The most common cause of an umbilical cord prolapse is a premature rupture of the membranes that contain the amniotic fluid. Other causes include: 1. Premature delivery of the baby 2. Delivering more than one baby per pregnancy (twins, triplets, etc.) 3. Excessive amniotic fluid 4. Breech delivery (the baby comes through the birth canal feet first) 5. An umbilical cord that is longer than usual DIAGNOSIS • Feeling the cord dropping into the vagina or your midwife seeing the cord come out before the presenting part of the baby are the most obvious ways to confirm a UCP. • Pelvic examination • Fetal heart rate on a fetal Doppler following the waters breaking (A prolapse is suspected in case it suddenly drops below 120 beats a minute, as it might indicate a lack of oxygen supply through the cord.) • An ultrasound scan performed before delivery to check the cord compression may also detect the problem. MANAGEMENT C-section, especially if the woman is in early labor. Vaginal delivery, if clinical judgment determines that is a safer or quicker method. The following maneuvers are among those used in clinical practice: Manual elevation of the presenting fetal part Repositioning of the mother to be head down with feet elevated Filling of the bladder with a foley catheter, or tube through the urethra to elevate the presenting fetal part. Use of tocolytics (medications to suppress labor) have been proposed, usually in addition to bladder filling rather than a standalone intervention. If the mother is far from delivery, funic reduction (manually placing the cord back into the uterine cavity) has been attempted, with successful cases reported. RISK FACTORS T h e two m a jo r ca tego ri es o f ri s k f a cto r s a r e s p o n ta neous a nd i a tr ogeni c , o r th o s e th a t r es u lt fr o m m ed i ca l i n ter venti on . • Spontaneous factors: • Fetal malpresentation: abnormal fetal lie tends to result in space below the fetus in the maternal pelvis, which can then be occupied by the cord. Multiple gestation, or being pregnant with more than one fetus at a given time: more likely to occur in the fetus that is not born first. • Spontaneous rupture of membranes about half of prolapses occur within 5 minutes of membrane rupture, two-thirds within 1 hour, 95% within 24 hours. • Polyhydramnios, or an abnormally high amount of amniotic fluid. • Prematurity: likely related to increased chance of malpresentation and relative polyhydramnios. • Low birth weight: usually described as <2500 g at birth, though some studies will use <1500g. Cause is likely similar to those for prematurity. Iatrogenic factors: • Artificial rupture of membranes • Placement of internal monitors (for example, internal scalp electrode or intrauterine pressure catheter • Manual rotation of fetal head