Guided By:
Dr Dax Abraham
Dr. Ravjot Ahuja
Guided by:
Dr. Arundeep Singh
Head of the department
Dept. of Conservative Dentistry
and Endodontics
Presented by:
Dr. Mohana Pratima
MDS 1st Year
Dept of Conservative Dentistry and
Endodontics
CONTENTS
•
•
•
•
INTRODUCTION TO BLOOD CELLS
MECHANISM OF BLOOD COAGULATION
APPLIED ASPECTS
ORAL CONSEDERATIONS
INTRODUCTION:
• Blood is a connective tissue in fluid form.
• It is considered as the fluid of life because it carries oxygen
from lungs to all parts of body and carbon dioxide from all
parts of the body to lungs.
• Also called fluid of Growth and also fluid of health
K Sembulingam Essentials Of Medical Physiology
Properties of blood:
• Color: Red in color.
Arterial blood- scarlet
Venous blood-purple red because of more
carbon dioxide.
• Volume: in normal adult avg volume is 5L. In new born
volume is 450ml. In females slightly less and is about 4.5L.
• Reaction and Ph: slightly alkaline and ph is 7.4 in normal
condition.
• Viscosity: 5times more viscous than water. Due to RBC
cells and Plasma proteins.
K Sembulingam Essentials Of Medical Physiology
•
•
•
•
COMPOSITION OF BLOOD:
Blood cells
Plasma
Serum
K Sembulingam Essentials Of Medical Physiology
BLOOD CELLS
Red blood
cells or
erythrocytes
White
blood cells
or
leukocytes
Platelets or
thrombocytes
K Sembulingam Essentials Of Medical Physiology
Red blood cells:
• Ranges between 4 and
5.5 millions/cu.
• In adult
males it is 5millions/cu mm
• And in adult females is 4.5
Million/cu mm
• Are the non nucleated
formed elements in the
blood.
• Also known as
Erythrocytes.
• The red color is due to
coloring pigment called
Hemoglobin.
K Sembulingam Essentials Of Medical Physiology
Functions
• Transport of oxygen from lungs to the tissues.
• Transport of carbon dioxide from the tissues to
the lungs.
• Buffering action in blood.
• In blood group determination
K Sembulingam Essentials Of Medical Physiology
• White blood cells: Are the
colorless and the nucleated
formed elements of blood.
• Compared to RBC’s WBC’s are
larger in size and lesser in
number.
• Classifications
• Granulocytes:
Neutrophils:
Eosinophils:
Basophils:
• Agranulocytes:
Monocytes:
Lymphocytes:
K Sembulingam Essentials Of Medical Physiology
• Neutrophils
• 50 to 70
• 3000to6000
• Eosinophils
• 2 to 4
• 150 to 450
• Basophils
• 0 to1
• 0 to 100
• Monocytes
• 2 to 6
• 200 to 600
• Lymphocytes
• 20 to 30
• 1500 to
2700
K Sembulingam Essentials Of Medical Physiology
Functions
Neutrophils
Eosinophils
Basophils
Monocytes
Lymphocytes
First line of defense against the invading microorganisms.
Wander freely all over the body through tissues.
Provide defense to the body by acting the parasitic infections and
Allergic conditions like asthma. Are responsible for detoxification,
Disintegration, and removal of foreign proteins.
Important role in healing process
Motile and phagocytic in nature. First line defense along
Neutrophils
Responsible for development of immunity.
K Sembulingam Essentials Of Medical Physiology
Platelets:
Are the formed elements of the blood.
Small colorless, non-nucleated and
moderately refractive bodies.
Normal count:
Is 2,50,000.
It ranges between 2,00,000 and
4,00,000/cu mm of blood.
K Sembulingam Essentials Of Medical Physiology
Functions:
•
•
•
•
•
Role in blood clotting
Role in clot retraction
Role in prevention of blood loss(hemostasis)
Repair of ruptured blood vessel
Defense mechanism
K Sembulingam Essentials Of Medical Physiology
PLASMA
Solids(7-8%)
Water:92-93%
Organic substances
Gases
Oxygen
Carbon dioxide
Nitrogen
Inorganic substances
K Sembulingam Essentials Of Medical Physiology
Organic substances
I. Plasma proteins
II. Amino Acids
III. Carbohydrate
IV.Fats
V. Internal secretions
VI.Enzymes
VII.Non protein
nitrogenous
substances
VIII.Antibodies
Inorganic substances
1. Sodium
2. Calcium
3. Potassium
4. Magnesium
5. Bicarbonate
6. Chloride
7. Phosphate
8. Iodide
9. Iron
10.copper
K Sembulingam Essentials Of Medical Physiology
•
•
•
•
•
•
•
•
•
•
In coagulation system
Defense mechanism of body
Transport mechanism
Maintenance of osmotic pressure in blood.
Regulation of acid base balance.
Viscosity of blood
Erythrocyte sedimentation rate
Suspension stability of BBC’s
Production of Trephone substances
As reserve protein.
K Sembulingam Essentials Of Medical Physiology
• Platelet rich plasma:
• PRP is a blood plasma that has been enriched with platelets. As
concentrated source of autologous platelets, PRP contains
several growth factors and cytokines that stimulate healing of
bone and soft tissues.
Clinical applications include:
Tendinitis, cardiac muscle injury, Bone repair and regeneration, Oral
surgery.
SERUM
• Clear straw colored fluid that is left after blood is
clotted.
• When the blood is collected in a container, it clots.
• In this process, the
fibrinogen is converted into
fibrin and the blood cells
are trapped in this fibrin
forming the clot.
• So fibrinogen is absent in
serum.
• Serum= Plasma-Fibrinogen.
K Sembulingam Essentials Of Medical Physiology
FUNCTIONS OF BLOOD:
•
•
•
•
•
•
•
•
•
Nutrient function
Respiratory function
Excretory function
Transport of hormones and
enzymes
Regulation of water balance
Regulation of acid balance
Body temperature
Storage function
Defense function
K Sembulingam Essentials Of Medical Physiology
COAGULATION OF BLOOD
• Definition: As the process in which the blood
looses its fluidity and becomes a jelly like mass
few minutes after it is shed out or collected in
a container.
K Sembulingam Essentials Of Medical Physiology
FACTORS INVOLVED IN BLOOD CLOTTING:
•
•
•
•
•
•
•
•
•
•
•
•
•
Factor I: Fibrinogen
Factor II: Prothrombin
Factor III: Thromboplastin
Factor IV: Calcium
Factor V: Labile factor
Factor VI: Prescence has not been proved
Factor VII: Stable Factor
Factor VIII: Antihemophilic
Factor IX: Christmas factor
Factor X: Stuart factor
Factor XI: Plasma Thromboplastin antecedent
Factor XII: Hagan factor
Factor XIII: Fibrin stabilizing factor
K Sembulingam Essentials Of Medical Physiology
Sequence of clotting mechanism:
Enzyme cascade theory::
• Most of the clotting factors in the form of enzymes.
• Normally all the factors are present in the form of
inactive proenzyme.
• This theory explains how various reactions involved in
the conversation of proenzymes to active enzymes take
place in form of cascade.
• Cascade refers to a process that occurs through a series
of steps, each step initiating the next, until the final
step is reached.
K Sembulingam Essentials Of Medical Physiology
Stages of blood clotting :
1. Formation of prothrombin
activator
2. Conversion of prothrombin into
thrombin
3. Conversion of fibrinogen into fibrin
K Sembulingam Essentials Of Medical Physiology
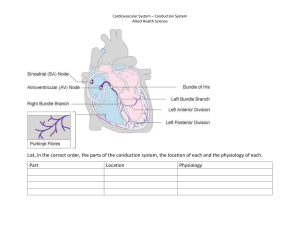
Stage 1
Intrinsic pathway
Endothelial damage + collagen exposure
kallikrein
HMWKinogen
XII
XIIa
Platelets
HMW
XI
XIa
calcium
IX
IXa
Phospholipid
VIII,calcium
X
Xa
V
+
Thrombin
Extrinsic pathway
Tissue Trauma + Tissue Thromboplastin
Glycoprotein Phospholipids
Xa
X
Calcium
V
+
Thrombin
Prothrombin activator
Stage 2 positive feedback
Prothrombin
Stage3
Polymerisation
Positive feedback
Thrombin
Fibrinogen a
Fibronogen
Loose strands of fibrin
XIII
Calcium
Fibrin tight blood clot
K Sembulingam Essentials Of Medical Physiology
HEMOSTASIS
Defined as arrest or stoppage of bleeding.
Stages:
Vasoconstriction.
Formation of platelet plug.
Coagulation of blood.
K Sembulingam Essentials Of Medical Physiology
Blood clot
• Defined as the mass of coagulated
blood which contains RBC’s WBC’s
and platelets entrapped in fibrin
meshwork.
• RBC’s and WBC’s are not necessary
for clotting process. However when
clot is formed these cells are trapped
in it along with platelets.
• The trapped RBC’s are responsible for
the red color of the clot.
• The external blood clot is also called
scab. It adheres to the opening of
damaged blood vessel and prevents
blood loss.
Blood clot
K Sembulingam Essentials Of Medical Physiology
Clot retraction:
• After the formation, the blood clot starts contracting.
And after about 30-45 minutes, a straw colored fluid
called serum oozes out of the clot.
• This process is called
Clot retraction.
• The contractile proteins
namely, actin, myosin,
thrombosthenin are
responsible for
clot retraction.
K Sembulingam Essentials Of Medical Physiology
Fibrinolysis:
• Lysis of blood clot inside the blood vessel is called
fibrinolysis.
• Helps to remove the clot from the lumen of the blood
vessel.
• This process requires a substance called plasmin or
fibrinolysin.
Plasmin formation:
• Formed from inactivated glycoprotein called
plasminogen.
• Synthesized in liver and is Incorporated with other
proteins in the bloodclot.
K Sembulingam Essentials Of Medical Physiology
• Plasminogen is converted into plasmin by Plasminogen
activator (t-PA), lysosomal enzymes and thrombin.
• The t-PA is inhibited a substance called t-PA inhibitor. And
also by factors V and VIII.
• Besides t-PA, there is another Plasminogen activator
called urokinase Plasminogen activator (u-PA).
K Sembulingam Essentials Of Medical Physiology
• Sequence of events involved in the activation of
Plasminogen
• During intravascular clotting the endothelium of the
blood vessel secretes a thrombin binding protein called
Thrombomodulin.
K Sembulingam Essentials Of Medical Physiology
Damaged tissue and endothelium
Thrombomodulin
+
Lysosomal enzymes
Thrombin
Thrombomodulin-thrombin complex
Protein C
Activated protein C
Protein S
Inactivation of V and VIII
Inactivation of t-PA inhibitor
Activation of t-PA
thrombin u-PA
Plasminogen
Plasmin
Lyses of clot(fibrin)
K Sembulingam Essentials Of Medical Physiology
Anticlotting mechanism in the body:
• Under physiological conditions, intravascular clotting
does not occur. Because of some physiochemical factors
in the body:
• Physical factors:
• i. Continuous circulation of blood.
• ii. Smooth endothelium lining of the blood.
• Chemical factors:
• Prescence of natural anticoagulant heparin that is
produced by the liver.
• All the clotting factors are in inactive state.
• Inactivation of factor V and VIII prevents clot formation.
K Sembulingam Essentials Of Medical Physiology
Anticoagulants
• The substances, which
prevent or postpone
coagulation of blood, are
called anticoagulants.
• Three types:
• Used to prevent blood
clotting inside the body,
i.e. in vivo
• Used to prevent clotting of
the blood that is collected
from the body i.e. in vitro
• Used to prevent clotting
both i.e. in vivo and in vitro
K Sembulingam Essentials Of Medical Physiology
Heparin:
• Naturally produced anticoagulant in the body.
• It is produced by mast cells which are abundant in liver
and lungs. Basophiles also secrete heparin.
• Heparin is a conjugated polysaccharide. Commercial
heparin is produced from liver and other organs of
animals.
• Available in liquid form or dry form as sodium, calcium,
ammonium, or lithium salts.
K Sembulingam Essentials Of Medical Physiology
Mechanism of action:
• Prevents blood clotting by its antithrombin activity.
• Combines with antithrombin III
and removes from circulation.
• Activates antithrombin III
• Inactivates other factors like IX,
X, XI, XII.
K Sembulingam Essentials Of Medical Physiology
HEPARIN
SUPRESSES
THROMBIN ACTION
INACTIVATES FACTORS
IX, X, XI XII
ACTIVATES
ANTITHROMBIN III
REMOVES
THROMBIN
NO BLOOD
CLOTTING
K Sembulingam Essentials Of Medical Physiology
Uses of heparin:
As an anticoagulant both in vivo and in vitro.
Clinical use
Intravenous injection of heparin(0.5-1 mg/kg body weight)
postpones clotting for 3-4 hours. So widely used in
clinical practice.
i. To prevent intravascular blood clotting surgery.
ii. During dialysis when blood is passed through artificial
kidney.
iii. During cardiac surgery, which involves passing blood
through heart lung machine.
iv. Anticoagulant to preserve the blood transfusion
K Sembulingam Essentials Of Medical Physiology
In laboratory:
Initial condition
• Used as anticoagulant
in vitro while collecting
blood for various
Effective clotting
investigations.
• About 0.1-0.2 mg is
sufficient for 1ml of
blood.
• Effective for 8-12
hours.
• Most expensive
anticoagulant
Thrombus
formation
Low dose
heparin
High dose
heparin
K Sembulingam Essentials Of Medical Physiology
• Coumarin derivatives
• Dicoumoral and Warfarin
Mechanism of action:
• Prevents blood clotting by inhibiting the action of
Vitamin K
• Essential for formation of various clotting factors namely
VII, IX, X.
K Sembulingam Essentials Of Medical Physiology
Uses:
• Oral anticoagulants in clinical practice (in vivo)
K Sembulingam Essentials Of Medical Physiology
EDTA:
• Ethylenediaminetetra acetic acid (EDTA) is a strong
anticoagulant.
Available in two forms:
• Disodium salts(Na2EDTA)
• Tripotassium salt(K3EDTA)
Mechanism of action:
• Prevents clotting by removing calcium.
Uses:
• I.V in case of lead poising.
• In-vitro 0.5-2.0 mg of EDTA per ml of blood sufficient to
preserve the blood for at least 6hours.
• In refrigerator it can prevent blood for up to 24 hours
K Sembulingam Essentials Of Medical Physiology
Oxalate Compounds:
• Prevents clotting by forming calcium oxalate. Thus these
compound of reduce calcium level.
• Earlier sodium and potassium oxalates were used.
• Nowadays mixture of ammonium oxalate and potassium
oxalate in ratio of 3:2 were used.
• Each salt is an anticoagulant by itself.
• Potassium oxalate causes shrinkage of RBC’s.
• Ammonium oxalate causes swelling of RBC’s.
K Sembulingam Essentials Of Medical Physiology
Mechanism of action:
• Combines with calcium and forms insoluble calcium
oxalate.
• Thus it removes calcium from blood and lack of calcium
prevents coagulation.
Uses:
• In vitro anticoagulant.
• 2mg of mixture is necessary for 1ml of blood.
• Oxalate is poisonous so it cannot be used in vivo
K Sembulingam Essentials Of Medical Physiology
Citrates:
• Sodium, ammonium and potassium citrates are used as
anticoagulants.
• Mechanism of action:
• Combines with calcium in blood to form insoluble
calcium citrate.
• Like oxalate, citrate also removes calcium from blood and
lack of calcium prevents coagulation.
K Sembulingam Essentials Of Medical Physiology
Uses:
• To store blood in blood banks availabl in two forms:
• Acid citrate dextrose(ACD) – 1part of ACD with 4 parts of
blood.
• Citrate phosphate dextrose(CPD) – 1 part of CPD with 4
parts of blood.
• Used in laboratory in vitro. Formol-citrate solution
(Dacie’s solution) is used for RBC and platelet counts.
K Sembulingam Essentials Of Medical Physiology
Other substances which prevent blood
clotting:
• Peptone, proteins, from venom of copperhead snake and
hirudin (from leach) are the known coagulants.
K Sembulingam Essentials Of Medical Physiology
Physical method to prevent blood clotting:
• 1. Cold:
• Reducing the temperature to about 5 c postpones
coagulation of blood.
• 2. Collecting blood in a container with smooth surface:
• Like silicon coated container prevents clotting. This
inhibits the activation of factor XII and platelets.
• So formation of prothrombin activator is prevented.
K Sembulingam Essentials Of Medical Physiology
Procoagulants
• Or hemostatic agents are the substances , which
accelerate the process of blood coagulation.
• Procoagulants are:
• Thrombin: Sprayed upon bleeding surface to arrest
bleeding by hastening blood clotting.
• Snake venom: Venom of snakes contains proteolytic
enzymes which enhance blood clotting by activating the
clotting factors.
K Sembulingam Essentials Of Medical Physiology
Extracts of lungs and thymus
• Obtained from lungs and thymus has Thromboplastin,
which causes rapid blood coagulation.
Sodium or calcium alginate:
• Enhance blood clotting by activating hegman factor.
Oxidized cellulose:
• Clotting by activating hegman factor.
K Sembulingam Essentials Of Medical Physiology
Tests for clotting
•
•
•
•
•
Bleeding time
Clotting time
Prothrombin time
Partial prothrombin time
Thrombin time.
K Sembulingam Essentials Of Medical Physiology
Bleeding time:
• Time interval from oozing of blood after a cut or injury
till arrest of bleeding.
• Determined by Duke method using blotting paper or
filter paper method.
• Its normal duration is 3-6 min
• Prolonged in purpura
K Sembulingam Essentials Of Medical Physiology
Clotting time:
• Time interval from oozing of blood after cut or injury till
the clot formation.
• Usually determined by capillary tube method.
• Normal duration is 3-8 minutes
• Prolonged in Hemophilia.
K Sembulingam Essentials Of Medical Physiology
Prothrombin time:
• Time taken by blood to clot after adding tissue Thromboplastin to it.
• Blood is collected and oxalated so that, the calcium is precipitated and
prothrombin is not converted into thrombin.
• Large quantity of tissue thromboplastin with calcium is added.
• Tissue thromoplastin activates prothrombin and blood clotting occurs.
• During this procedure, the time taken by blood to clot after adding
tissue Thromboplastin is determined.
• Normal duration is 12 seconds
• Prolonged in prothrombin
Deficiency and other factors like
factor I, V, VII and X.
• Normal in hemophilia
K Sembulingam Essentials Of Medical Physiology
PARTIAL PROTHROMBIN TIME:
• Is the time taken for blood to clot after adding
phospholipid and calcium to blood.
• It is also called activated prothrombin time.
• Done to investigate bleeding disorders and to detect the
Prescence of heparin in patients treated with heparin.
• Carried out by observing clotting time after adding
phospholipid, surface activator and calcium to patients.
• Phospholipid is platelet substitute and surface activator
is Kaolin.
• Normal duration is 30-50 sec.
• Prolonged in heparin therapy deficiency of factors II, V,
VIII, IX, X, XI, XII
K Sembulingam Essentials Of Medical Physiology
THROMBIN TIME:
• Time taken for the blood to clot after adding thrombin to
it.
• Done to investigate the presence of heparin in plasma or
to detect fibrinogen abnormalities.
• Involves the observation of clotting time after adding
thrombin to patients plasma.
• Normal duration is 12-20 sec.
• Prolonged in heparin therapy
and during dysfibrinogenimia.
K Sembulingam Essentials Of Medical Physiology
• HAEMORRHAGIC DIATHESES DUE TO
PLATELET DISORDERS.
• Disorders of platelets produce bleeding disoreders by
one of the following 2 mechanisms.
i. Due to reduction in the number of platelets
ii. Due to defective platelets
Harsh Mohan Essential Pathology for Dental Students
THROMBOCYTOPENIAS:
• Reduction in the peripheral blood platelet count below the lower
limit of normal i.e. 150,000/ul.
• Associated with abnormal bleeding.
•
•
•
•
May result from 4 main groups of causes:
Impaired platelet production.
General bone marrow failure
Selective suppression of platelet production.
Accelerated platelet destruction
Immunological thrombocytopenias
Increased consumption.
Splenic sequestration.
Splenomegaly
Dilutional loss.
Massive transfusion of old stored blood to bleeding patients
Harsh Mohan Essential Pathology for Dental Students
Drug-induced thrombocytopenia
• Many commanly used drugs cause
thrombocytopenia by depressing megakaryocyte
production.
• Drugs include:
Chemotherapeutic agents(antimetabolites,
anthracyclines), certain antibiotics (sulfonamides,
rifampacin,pencillins), drugs used in
cardiovascular disesases (digitoxin, thiazide
diuretics), heparin and excessive consumption of
ethanol.
Harsh Mohan Essential Pathology for Dental Students
• Disorders of platelet functions:
Herediatry disorders:
Defective platelet adhesion.
Defective platelet aggregation.
Disorders of platelet release reaction.
Aquired disorders:
Aspirin therapy:
Others:
Harsh Mohan Essential Pathology for Dental Students
COAGULATION DISORDERS
• Are the diseases characterized by prolonged bleeding or
clotting time.
• Disorders are of three types.
i. Hemophilia
ii. Purpura
iii. von Willebrand disease.
iv. Vitamin K defeciency.
v. Coagulation disorders in liver diseases.
vi. Fibrinolytic defects.
Harsh Mohan Essential Pathology for Dental Students
HEMOPHILIA.
• Group of sex linked inherited disorders featured by
prolonged clotting time.
• Usually affects males, females being the carriers.
• Damage of skin while falling
or extraction of tooth cause
excess bleeding for few
weeks.
• Easy bruising and
hemorrhage in muscles and
joints are also
common.
Harsh Mohan Essential Pathology for Dental Students
CAUSES
• Due to lack of formation of
prothrombin activator.
• Bleeding time and prothrombin
time are normal.
• Function of prothrombin time
is effected due to deficiency of
factor VIII, IX, or XI.
Types of hemophilia:
Hemophilia A or classic
hemophilia:
• Due to the deficiency of factor
VIII. 85% of people are
affected.
Hemophilia B or Christmas
Factor IX:
• It is due to the deficiency of
factor IX. 15% are affected.
Hemophilia C or factor XI
deficiency:
• Due to deficiency of factor XI. It
is a very rare disorder.
Harsh Mohan Essential Pathology for Dental Students
SYMPTOMS:
• Spontaneous bleeding.
• Prolonged bleeding due to cuts, tooth extraction and
surgery.
• Hemorrhage in gastrointestinal and urinary tract.
• Bleeding in joints followed by
swelling and pain.
• Appearance of blood and urine.
TREATMENT :
• Replacing the missing
clotting factor.
Harsh Mohan Essential Pathology for Dental Students
PURPURA:
• Characterized by prolonged bleeding time.
• Characteristic feature is spontaneous bleeding under
skin from ruptured capillaries.
• Causes small tiny hemorrhagic spots in many areas of
the body.
• These spots under the skin are called purpuric spots.
• Blood also sometimes collects in large areas beneath the
skin which are called Ecchymoses.
• But clotting time is normal
Harsh Mohan Essential Pathology for Dental Students
• Types and causes:
• Depending upon causes classified as
i. Thrombocytopenic purpura:
• Due to deficiency of platelets.
• In bone marrow disease platelet production is affected
leading to deficiency of platelets.
ii. Idiopathic thrombocytopenic purpura:
• Due to some unknown cause called idiopathic
thrombocytopenic purpura.
• Platelet is count is decreased due to development of
antibodies against platelets
Harsh Mohan Essential Pathology for Dental Students
• iii. It is due to structural or functional
abnormality of platelets.
• Platelet count is normal.
• Normal clotting time, normal or prolonged bleeding
time but defective clot retraction.
Harsh Mohan Essential Pathology for Dental Students
von Willebrand
disease:
• Characterized by excess bleeding
disorder even with a mild injury.
• Due to inherited deficiency of von
willebrand factor.
• Responsible for adherence of
platelets to endothelium of blood
vessels during hemostasis after an
injury.
• This deficiency suppresses platelet
adhesion and also causes deficiency
of factor VIII.
• This results in excess bleeding that
occurs during platelet dysfunction.
Harsh Mohan Essential Pathology for Dental Students
• TypeI. Most common characterized by mild to
moderate decrease in plasma vWF.
• TypeII. Much less common and is characterized by
normal or near normal levels of vWF which is
functionally defective.
• TypeIII. Extremely rare and most severe form of disease.
Bleeding episodes are treated by
Cryoprecipitates.
Harsh Mohan Essential Pathology for Dental Students
VITAMIN K DEFICIENCY:
• Is a fat soluble vitamin which plays important role in hemostasis as
a co-factor in the formation of 6 prothrombin complex proteins
synthesised in the liver: factor II, VII, IX, X. protein C and S.
• Vitamin K deficiency may present in new born or in subsequent
childhood or adult life.
• NEONATAL vitamin K deficiency.
• Vitamin K deficiency in children and adult.
Harsh Mohan Essential Pathology for Dental Students
COAGULATION DISORDERS IN LIVER DISEASE:
• Liver also produces inhibitors of coagulation such as antithrombin
III and protein C and S and plays a role in the clearance of activated
factors and fibrinolytic enzymes.
• The major causes of bleeding in liver disease are :
I. Anatomic lesion:
Portal hypertension
Peptic ulceration
Gastritis
II. Hepatic dysfunction:
Impaired hepatic synthesis of coagulation factors.
Impaired hepatic synthesis of coagulation inhibitors.
Impaired absorption and metabolism of vitamin K.
III. Complications of therapy:
Massive transfusion
Infusion of activated coagulation proteins.
Following heparin therapy
Harsh Mohan Essential Pathology for Dental Students
THROMBOSIS:
• Thrombosis or intravascular blood clotting refers to
coagulation of blood inside the blood vessel.
Causes of thrombosis:
•
•
•
•
•
•
Injury to blood vessel.
Roughened endothelial lining.
Sluggishness of blood flow.
Agglutination of RBC’s.
Toxic thrombosis.
Congenital absence of protein C.
Harsh Mohan Essential Pathology for Dental Students
COMPLICATIONS OF THROMBOSIS
• Thrombus:
The solid mass of platelets, red cells and/0r clot, which
obstructs the blood vessel is called Thrombus.
• This thrombus formed due to agglutination of RBC is
called agglutinative thrombus.
• Embolism and embolus:
• Process in which the thrombus or part of it is detached
and carried in bloodstream and occludes the small blood
vessels results in arrests of blood flow to any organ or
region of the body.
• Common in lungs, brain or heart.
Harsh Mohan Essential Pathology for Dental Students
Harsh Mohan Essential Pathology for Dental Students
ISCHEMIA:
• Insufficient blood supply to an organ or area of body by
the obstruction of blood vessels is called ischemia.
• Results in tissue damage because of hypoxia.
• Also causes discomfort, pain, and tissue death.
• Death of body tissue is called necrosis.
Harsh Mohan Essential Pathology for Dental Students
NECROSIS AND
INFRACTION:
• Necrosis in general term refers to
tissue death caused by loss of blood
supply, injury, infection, inflammation,
physical agents or chemical
substances.
• Infraction means the tissue death due
to loss of blood supply.
• Loss of blood supply is usually caused
occlusion of an artery by thrombus or
embolus and sometimes by
atherosclerosis.
• Infraction commonly occurs in heart,
brain, lungs, kidneys and spleen.
Harsh Mohan Essential Pathology for Dental Students
DISSEMINATED INTRAVASCULAR
COAGULATION:
• Also termed as defibrination syndrome or consumption
coagulopathy.
• Etiology:
• Massive tissue injury.
• Infections
• Widespread edothelial damage
• Miscellanious
Clinical features:
2main features of DIC:
Bleeding as the most common manifestation and Organ
damage due to ischemia caused by effects of wide spread
intravascular thrombosis such as kidney and brain.
Harsh Mohan Essential Pathology for Dental Students
ORAL HEALTH CONSIDERATIONS
• Platelet deficiency and vascular wall disorders result in
extravasations of blood into connective tissues of the skin and
mucosa creating pinpoint hemmorages called petechiae and
larger patches called Ecchymoses.
• Hemarthrosis is a common complications in hemophiliac’s.
• An acute TMJ arthrosis associated with FIX deficiency was
resolved with factor replacement.
Burket’s Oral Medicine
Dental management:
• Dental modifications required for patients with bleeding disorders
depend on both the type and invasiveness of dental procedure and
the type and severity of the bleeding disorder.
• Less modification is needed for patients with mild- coagulopathies
in dental procedures.
• When significant bleeding is expected, the goal of management is
to preoperatively restore the hemostatic system.
• For reversible coagulopathies the best to remove the causative
agents or primarily treat the illness.
• For irreversible coagulopathies the treatment is missing or
defective element may be replaced from exogenous source to
allow control of bleeding.
Burket’s Oral Medicine
• PLATELET DISORDERS:
• When medical management is unable to
restore the platelet level of 50,000/mm3
required for surgical hemostasis , platelet
transfusions must be required prior to
dental extractions or other oral surgical
procedures.
• Six units of platelets are commanly
expected to infuse at a time.
• Local hemostatic methods are also
important .
• The thromosthenic patients needing
dental extractions may be succesfully
treated with microfibrillar collagen and
antifibrinolytic drugs.
• If using of aspirin, avoidance of aspirin is
recommended, when possible for 1 week
prior to extensive oral procedures
• Adjunctive local hemostatic agents are
useful in preventing post operative oozing
when aspirin therapy is in use at the time
of minor surgical procedures.
Burket’s Oral Medicine
• Adjunctive local hemostatic agents are useful in preventing post
operative oozing when aspirin therapy is in use at the time of
minor surgical procedures.
• When extensive surgery is emergently indicated DDAVP can be
used to decrease the aspirin induced prolongation of the BT or
to treat aspirin related postoperative oozing.
Burket’s Oral Medicine
• HEMOPHILIAS A and B and vWD:
• To make certain preoperative factors levels of at least 40 to 50% of
normal activity have been obtained, transfusion recommendations
generally aim for replacement of missing coagulation factors to
levels of 50-100%.
• Postsurgical bleeding occurs due to fibrinolysis it commonly starts
3 to 5 days after surgery and can be easily controlled by local
measures and use of antifibrinolytics. Continuous oozing from
unstable fibrinous clots require removal and repacking of the
extraction socket with hemostatic agents.
• Gingival or dental bleeding unresponsive to antifibrinolytics
require 20-30% of clotting FVIII or FIX.
• Higher hemostatic factor levels are needed with large wound
cavities like extraction of multiple or multi rooted teeth, gingival
inflammation, bleeding, tooth mobility, or apical lesions
Burket’s Oral Medicine
• Fibrin sealants or fibrin glue has been used effectively as an
adjunct with adhesive and hemostatic effects to control bleeding
at wound or surgical sites.
Preventive and periodontal therapies:
• Periodontal probing and suprgingival scaling can be routinely
done.
• Subgingival scaling rarely warrents replacement therapy.
• Severly inflammed and swollen tissues are best treated initially by
chlorhexidine oral rinses or by gross debridement with hand
instruments to allow gingival shrinkage.
• Deep subgingival and root plannning performed by quadrent to
reduce potential bleeding
• Locally applied pressure and antifibrinolytic mouth rinses are
usually succesful
• Periodontal packing material aids hemostasis and protects the
surgical site.
Burket’s Oral Medicine
• Restorative and
prosthodontic therpy:
• Rubber dam isolation is advised ti
minimize the risk of laceration soft
tissue in operative field and to avoid
creating ecchymoses and
hematomes.
• Care is taken to select tooth clamp.
Matrices, wedges and hemostatic
gingival retraction cord are used
with caution to protect soft tissues.
• Endodnotic therapy:
• Is often the treatment of choice for
patient with severe bleeding.
• Generally no contraindications for
root canal treatment, provided that
instrument does not extend beyond
the apex.
• Application of epinephrine
intrapulpally to apical area is
succesful in providing hemostasis.
Burket’s Oral Medicine
Pediatric dental therapy:
• Administration of factor concentrate and extraction of decidious
teeth with curretage may be neccesary for patient comfort and
hemorrhage control.
• Hemorrhage control is obtained by guage pressure and seepage
generally stops by 12 hours.
• Pulpotomies can be performed without excessive pulpal bleeding.
• Topical fluoride applications and pit and fissure sealants decrease
the need for extensive therapy.
Orthodontic therapy:
• Avoid mucosal lacerations,
• Minor cuts usually respond to
local pressure.
Burket’s Oral Medicine
• PATIENTS ON ANTICOAGULANTS:
• It is generally held that non surgical dental treatment can be
successfully accomplished without alterations of the anticoagulant
regimen that INR is not grossly above the therapeutic range and
trauma is minimized.
• The AHA recommends that patients undergoing dental procedures,
Tranexamic acid or EACA mouth wash can be applied without
interrupting anticoagulant therapy.
• ACCP recommends
i.) for patients going dental procedures who are not considered to
be at high risk of bleeding, ACCP recommends Warfarin therapy
not to be discontinued. In patients high risk for bleeding Warfarin
can be discontinued.
ii.) in whom local bleeding must be controlled, Tranexamic acid or
EACA mouth wash must be administered without interrupting
anticoagulant therapy.
Burket’s Oral Medicine
• For surgical procedures, physician consultation is advised in order
to determine the patients most recent INR level and the best
treatment approach based on patients relative hemorrhagic
risks.
Burket’s Oral Medicine
Dental treatment
Suboptimal INR range Nor mal target INR range
Of anticoagulants
Of anticoagulants
Anticoagul
-ants Out
of range
<1.5
>3.5
1.5<2.0
2.0<2.5
2.5<3.0
3.0<3.5
Examination, radiographs,
impressions, orthodontics
Simple restorative dentistry,
supragingival prophylaxis
Complex restorative
dentistry, scaling and root
planning, endodontics
Simple extractions,
curettage, gingivoplasty,
biopsy
Caution:
probably
safe
Probably:
safe
Caution:
Local
measures
Caution:
Local
measures
Hospital
procedure
Burket’s Oral Medicine
Suboptimal INR range
Normal INR range
<1.5
1.5<2.0
2.0<2.5
Gingivectomy, apicectomy,
minor periodontal flap,
placement of single implant
Probably:
safe
Caution:
Probably
safe
Caution:
Probably
safe
Full mouth or arch
extractions
Caution:
Probably
safe
Caution:
Local
measures
Extensive flap surgery,
extraction of multiple bony
impactions, multiple
implant placement
Caution:
Probably
safe
Open fracture reduction,
orthognathic surgery.
Hospital
procedure
Dental treatment
2.5<3.0
Out of
range
<3.0 to 3.5
>3.5
Multiple extraction,
removal of single bony
impaction
Burket’s Oral Medicine
• PRP
• The first step of the treatment plan was
to complete the root canal therapy
obturation was done on the day of
surgery. The surgical protocol included a
routine medical history followed by
blood investigations. The surgical
procedure included reflection of a full
thickness mucoperiosteal flap by
sulcular incision and two relieving
vertical incisions. Debridement of
tissues at the defect site was followed
by irrigation with sterile saline solution.
Root planing was performed on the root
surface under the apical portion of the
root. No root resection was done.
Bony cavity filled
with Platelet-Rich
plasma gel
Journal of Conservative Dentistry | Apr-Jun 2011 | Vol 14 | Issue 2
• Wound closure was obtained with a 3-0 black silk suture.
• Analgesics (Combiflam {ibuprofen 400 mg + paracetamol 325 mg}
twice a day)
• Antibiotics (Amoxycillin 500 mg twice a day) and 0.2%
Chlorhexidine mouthwash was prescribed for five days post
surgically.
• The sutures were removed after seven days. The patients were
reviewed at regular intervals of one week, and one, three, six,
nine, and twelve months.
Journal of Conservative Dentistry | Apr-Jun 2011 | Vol 14 | Issue 2
Journal of Conservative Dentistry | Apr-Jun 2011 | Vol 14 | Issue 2