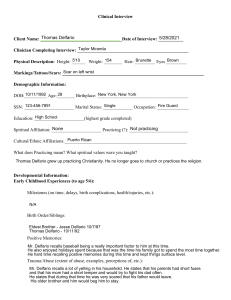
Clinical Interview Client Name: ______________________________________Date of Interview: ___________ Clinician Completing Interview: _________________________________________________ Physical Description: Height: ______ Weight: ________ Hair: _________ Eyes _________ Markings/Tattoos/Scars: Demographic Information: DOB:__________ Age:________ Birthplace: ________________________________________ SSN: ______________________ Marital Status: _____________ Occupation: ______________ Education: ______________________(highest grade completed) Spiritual Affiliation: ______________________ Practicing (?): __________________________ Cultural/Ethnic Affiliations:______________________________________________________ What does Practicing mean? What spiritual values were you taught? Developmental Information: Early Childhood Experiences (to age 5/6): Milestones (on time, delays, birth complications, health/injuries, etc.): Birth Order/Siblings: Positive Memories: Trauma/Abuse (extent of abuse, examples, perceptions of, etc.): Separations/Family Relationships: School Experiences (grades, friendships, etc.): Unusual Experiences: Middle Childhood/Adolescence: Positive Memories: Trauma/Abuse (extent of abuse, examples, perceptions of, etc.): What names were you called? Separations/Divorce/Family Relationships: School Experiences (grades, difficulties/friendships, etc.): Employment Experiences: Unusual Experiences: Adulthood: Major Changes (Life, Occupations, School, Family, Marriage/Divorce, Children, etc.): Friendships/Family and Other Relationships: How’s your relationship with Mom, Dad, now? Positive Experiences/Memories: Traumatic Experiences/Memories: Social Leisure Experiences: Employment History: Client’s statement of “Usual” or Current Occupation (obtain salary): First Job: Work History (include length of each job, reason for leaving, etc.) Work Relationships: Goals/Aspirations: Substance Use: Drug How Much How Often First Use Last Use 1. _______________________________________________________________________________ 2. _______________________________________________________________________________ 3. _______________________________________________________________________________ 4. _______________________________________________________________________________ Substance Abuse Treatment History: Related Problems (arrests, problems at work, peers, family, seizures, blackouts, etc.): How did they finance drug/alcohol use?: Psychiatric History: Current Medications (include side effects and target symptoms) Symptoms: Prior Hospitalizations/Treatment: Prior Diagnosis: How do they deal with and what causes stress/anxiety?: Family History of Mental Illness: Sexual Development: First Sexual Experience: Sexual Preference/Experiences: Current Sexual Practices (include whether gratifying or not): History of forced sexual experiences (include ages, age of other, description of each experiences): History of Sexual Experiences (include any homosexual experiences, age, descriptions): Use of Sexual Aids (magazines, videos, toys, etc.): Fetishes, Paraphilias, Fantasies, Masturbation, etc.: Medical History: Current medications (nonpsychiatric): History of major treatments/surgeries: History of head trauma (include description of each, ie., treatment, loss of consciousness, seizures, rehabilitation, dates and lengths and facilities): Criminal History: Juvenile (summarize charges, incarcerations, age, trial or plea, etc.): Adult (summarize charges, incarcerations, age, trial or plea, etc.): Responsibility (debts, child support, money owing, payments, bankruptcy, loans, etc.) Mental Status: Appearance/Hygiene: Oriented (person, place, time): Awareness/Attention/Concentration: Mood (statement of feeling state): Affect (Objective expression of mood): Thought (comment on content, continuity, fluidity): Speech (tone, volume, clarity): Motor (unusual movements, retardation, fluidity, gait, anxious movements, etc.) Cognition (estimate of intelligence – memory: recent/remote/working): Insight/Judgment: Psychiatric Stability How have you been feeling recently? Depressed Bouts of crying A lot of energy, decreased need for sleep Sleep Nightmares Appetite Concentration Attention Impulsivitey Self-esteem Difficulty making decisions Suicidal ideation Suicide attempts Homicidal ideation Auditory halucinations (hear voices) Are voices telling you to tell me no Visual halucinations Decreased need for sleep Thoughts racing Out to get you Poisoning you Communicate through the TV Fire setting in childhood Food hoarding in childhood (save and hide food) Running away Teasing animals Bullying kids Shoplifting Notes: