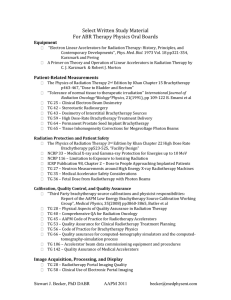
Brachytherapy Techniques: Radiation Protection in Radiotherapy
advertisement

IAEA Training Material on Radiation Protection in Radiotherapy Radiation Protection in Radiotherapy Part 6 Brachytherapy Lecture 2: Brachytherapy Techniques Brachytherapy • • • • Very flexible radiotherapy delivery Source position determines treatment success Depends on operator skill and experience In principle the ultimate ‘conformal’ radiotherapy • Highly individualized for each patient • Typically an inpatient procedure as opposed to external beam radiotherapy which is usually administered in an outpatient setting Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 2 Objectives • To be familiar with different implant techniques • To be aware of differences between permanent implants, low (LDR) and high dose rate (HDR) applications • To appreciate the potential for optimization in high dose rate brachytherapy • To be familiar with some special techniques used in modern brachytherapy (seed implants, endovascular brachytherapy) Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 3 Contents 1. Clinical brachytherapy applications 2. Implant techniques and applicators 3. Delivery modes and equipment 4. Special techniques • A. Prostate seed implants • B. Endovascular brachytherapy • C. Ophthalmic applicators Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 4 Clinical brachytherapy Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 5 History • Brachytherapy has been one of the earliest forms of radiotherapy • After discovery of radium by M Curie, radium was used for brachytherapy already late 19th century • There is a wide range of applications - this versatility has been one of the most important features of brachytherapy Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 6 Today • Many different techniques and a large variety of equipment • Less than 10% of radiotherapy patients receive brachytherapy • Use depends very much on training and skill of clinicians and access to operating theatre Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 7 A brachytherapy patient • Typically localized cancer • Often relatively small tumour • Often good performance status (must tolerate the operation) • Sometimes pre-irradiated with external beam radiotherapy (EBT) • Often treated with combination brachytherapy and EBT Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 8 Patient flow in brachytherapy Treatment decision Ideal plan - determines source number and location Implant of sources or applicators in theatre Localization of sources or applicators (typically using X Rays) Treatment plan Commence treatment Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 9 1. Clinical brachytherapy applications A. Surface moulds B. Intracavitary (gynaecological, bronchus,..) C. Interstitial (Breast, Tongue, Sarcomas, …) not covered here: unsealed source radiotherapy (Thyroid, Bone metastasis, …) - this is dealt with in the IAEA training material on radiation protection in Nuclear Medicine Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 10 A. Surface moulds • Treatment of superficial lesions with radioactive sources in close contact with the skin Hand A mould for the back of a hand including shielding designed to protect the patient during treatment Radiation Protection in Radiotherapy Catheters for source transfer Part 6, lecture 2: Brachytherapy techniques 11 Historical example Surface applicator with irregular distribution of radium on the applicator surface (Murdoch, Brussels 1933) Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 12 Other example Treatment of squamous cell carcinoma of the forehead Catheters for source placement Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 13 Source distance from the skin • Determines incident dose • Determines dose fall off in skin - the further the sources are from the skin the less influence has dose fall off due to inverse square law • Dose homogeneity - the further away the sources are the more homogenous the dose distribution is at the skin Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 14 Simulator films of forehead mould Dummy wires as markers for location Surface mould advantages • Fast dose fall off in tissues • Can conform the activity to any surface • Flaps available Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 17 B. Intracavitary implants • Introduction of radioactivity using an applicator placed in a body cavity • Gynaecological implants • Bronchus • Oesophagus • Rectum Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 18 Gynaecological implants • Most common brachytherapy application cervix cancer • Many different applicators • Either as monotherapy or in addition to external beam therapy as a boost Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 19 Gynecological applicators Different design - all Nucletron Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 20 Vaginal applicators • Single source line • Different diameters and length Gammamed - on the right with shielding Nucletron Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 21 Bronchus implants • Often palliative to open air ways • Usually HDR brachytherapy • Most often single catheter, however also dual catheter possible Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 22 Dual catheter bronchus implant • Catheter placement via bronchoscope • Bifurcation may create complex dosimetry Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 23 C. Interstitial implants • Implant of needles or flexible catheters directly in the target area • Breast • Head and Neck • Sarcomas • Requires surgery - often major Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 24 Interstitial implants - tongue implant Catheter loop tongue Button tongue Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 25 Breast implants • Typically a boost • Often utilizes templates to improve source positioning • Catheters or needles Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 26 2. Implant techniques and applicators • Permanent implants • patient discharged with implant in place • Temporary implants • implant removed before patient is discharged from hospital Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 27 Permanent implants • Implantation of sealed sources (typically seeds) into the target organ of the patient • Sources are NOT removed and patient is discharged with activity in situ (compare part 16 of the course) Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 28 Radiation protection issues • Patients are discharged with radioactive sources in place: • lost sources • exposure of others • issues with accidents to the patient, other medical procedures, death, autopsies and cremation Discussed in more detail in parts 9 (Medical Exposure), 16 (Discharge of patients) and 17 (Public exposure) Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 29 Source requirement for permanent implants • Low energy gammas or betas to minimize radiation levels outside of the patient (125-I is a good isotope) • May be short-lived to reduce dose with time (198-Au is a good isotope) • More details on most common 125-I prostate implants in section 4A of the lecture Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 30 Temporary implants • Implant of activity in theatre • Manual afterloading • Remote afterloading Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 31 Implant of activity in theatre • (Common for permanent implants) • For temporary implants common practice 40 years ago when radium was commonly used • for example gynecological implants of radium or 137-Cs needles • Today only very rarely used for temporary implants - one of few examples are 192Ir hairpins for tongue implants Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 32 Problems with handling activity in the operating theatre • Potential of lost sources • The time to place the sources in the best possible locations is typically limited • Radiation protection of staff may require awkward operation Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 33 Afterloading • Implant only empty applicator or needles/catheters in theatre • Once patient has recovered, dummy sources are introduced to verify the location of the applicators (typically using diagnostic X Rays) • The treatment is planned • The sources are introduced into the applicator or needle/catheter Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 34 Afterloading • Manual • Remote • The sources are placed • The sources are driven manually usually by a physicist • The sources are removed only at the end of treatment from an intermediate safe into the implant using a machine (“afterloader”) • The sources are withdrawn every time someone enters the room Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 36 Afterloading advantages • No rush to place the sources in theatre more time to optimize the implant • Treatment is verified and planned prior to delivery • Significant advantage in terms of radiation safety (in particular if a remote afterloader is used) Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 37 Quick question: Why is afterloading the method of choice from a radiation safety perspective? Some radiation safety aspects of afterloading • No exposure in theatre • Optimization of medical exposure possible • No transport of a radioactive patient necessary ‘Live’ implants should be avoided for temporary implants Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 39 Applicators for brachytherapy Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 40 Brachytherapy Applicators - lots to choose from, lots to learn Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 41 Some examples for applicators • Gynaecological applicators Fletcher Suit Henschke type Ring type Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 42 Rotterdam Applicator • A choice of sizes allows customized treatment of each patient Tandem Lengths (in mm) 40 50 60 70 Radiation Protection in Radiotherapy Ovoid Sizes Small Medium Large Part 6, lecture 2: Brachytherapy techniques 43 Close-up view Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 44 Other intracavitary applicators • Vaginal • Bronchus Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 45 Interstitial applicators • Needles • hollow and rigid • may use templates for placement • usually have pusher during implantation in tissue Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 46 Interstitial applicators • Catheters • flexible • open and closed end available • often introduced into tissue via an open end needle skin Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 47 3. Delivery modes and equipment • • • • Low Dose Rate (LDR) Medium Dose Rate (MDR) High Dose Rate (HDR) Pulsed Dose Rate (PDR) Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 48 Delivery modes - different classifications are in use • Low Dose Rate • Medium Dose Rate • High Dose Rate • Pulsed Dose Rate Radiation Protection in Radiotherapy • • • • • • < 1Gy/hour around 0.5Gy/hour > 1Gy/hour not often used >10Gy/hour pulses of around 1Gy/hour Part 6, lecture 2: Brachytherapy techniques 49 Low dose rate brachytherapy • The only type of brachytherapy possible with manual afterloading • Most clinical experience available for LDR brachytherapy • Performed with remote afterloaders using 137-Cs or 192-Ir Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 50 Low dose rate brachytherapy • Selectron for gynecological brachytherapy • 137-Cs pellets pushed into the applicators using compressed air • 6 channels for up to two parallel treatments Nucletron Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 51 Simple design • No computer required • Two independent timers • Optical indication of source locations • Permanent record through printout • Key to avoid unauthorized use Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 52 Treatment process • Implant of applicator (typically in the operating theatre) • Verification of applicator positioning using diagnostic X Rays (e.g. radiotherapy simulator) Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 53 Two orthogonal views allow to localize the applicator in three dimensions Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 54 Treatment planning • Most commercial treatment planning systems have a module suitable for brachytherapy planning: • Choosing best source configuration • Calculate dose distribution • Determine time required to give desired dose at prescription points • Record dose to critical structures Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 55 Treatment planning of different brachytherapy implants Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 56 High Dose Rate Brachytherapy • Most modern brachytherapy is delivered using HDR • Reasons? • Outpatient procedure • Optimization possible Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 57 HDR brachytherapy • In the past possible using 60-Co pellets • Today, virtually all HDR brachytherapy is delivered using a 192-Ir stepping source Source moves step by step through the applicator - the dwell times in different locations determine the dose distribution Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 58 HDR 192-Ir source Source length 5mm, diameter 0.6mm Activity: around 10Ci Radiation Protection in Radiotherapy From presentation by Pia et al. Part 6, lecture 2: Brachytherapy techniques 59 Optimization of dose distribution adjusting the dwell times of the source in an applicator Nucletron Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 60 HDR brachytherapy procedure • Implant of applicators, catheters or needles in theatre • For prostate implants as shown here use transrectal ultrasound guidance Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 61 HDR brachytherapy procedure • Localization using diagnostic X Rays Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 62 Treatment planning • Definition of the desired dose distribution (usually using many points) • Computer optimization of the dwell positions and times for the treatment Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 63 Treatment • Transfer of date to treatment unit • Connecting patient • Treat... Gammamed Nucletron Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 64 HDR unit interface Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 65 HDR brachytherapy • Usually fractionated (e.g. 6 fractions of 6Gy) • Either patient has new implant each time or stays in hospital for bi-daily treatments • Time between treatments should be >6hours to allow normal tissue to repair all damage Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 66 HDR units: different designs available Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 67 Catheters are indexed to avoid mixing them up Transfer catheters are locked into place during treatment - green light indicates the catheters in use Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 68 HDR systems • Can be moved between different facilities or into theatre for intra-operative work Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 69 Pulsed dose rate • Unit has a similar design as HDR, however the • • • • activity is smaller (around 1Ci instead of 10Ci) Stepping source operation - same optimization possible as in HDR Treatment over same time as LDR treatment to mimic favorable radiobiology In-patient treatment: hospitalization required Source steps out for about 10 minutes per hour and then retracts. Repeats this every hour to deliver minifractions (‘pulses’) of about 1Gy Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 70 Pulsed dose rate brachytherapy • Different dose/time pattern possible • Usually treatment about once per hour • Illustration form ICRU report 58 Radiation Protection in Radiotherapy Part 6, lecture 2: Brachytherapy techniques 71 Features of PDR: • Advantages • Disadvantages Emulates LDR Optimized dose distribution Visitors and nursing staff can use the time between pulses while the activity is in the safe Radiation Protection in Radiotherapy - Potential radiation safety hazard of a source stuck in the patient: In LDR - low activity, no severe problem In HDR - physicist is present during treatment In PDR - will someone with sufficient training be there within 10 minutes? Even at midnight??? Part 6, lecture 2: Brachytherapy techniques 72 Question: Please list advantages and disadvantages of High Dose Rate Brachytherapy as compared to Low Dose Rate brachytherapy. Assume both approaches are performed using remote afterloading equipment. The answer should include: • Advantages Out patient procedure Optimization of dose distribution using stepping source Possibly better geometry as patient anesthetized No exposure of nursing staff during procedure No source preparation Radiation Protection in Radiotherapy • Disadvantages Potential radiobiological disadvantage Fractionation required More shielding required There is no time to intervene if machine failure occurs More sophisticated (and expensive) Part 6, lecture 2: Brachytherapy techniques 74