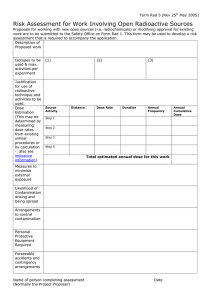
BRACHYTHERAP Y P RI NCI P L E AND METHODS DR. MANOJ KUMAR B MODERATOR:PROF. S.C. SHARMA DEPTT. OF RADIOTHERAPY AND ONCOLOGY PGIMER,CHANDIGARH BRACHYTHERAP Y Type of radiation treatment in which radioactive sources are arranged in such a fashion that radiation is delivered to the tumor at a short distance by interstitial, intracavitary or surface application. CLI NI CAL ADVANTAGES High biological efficacy Rapid dose fall-off High tolerance Tolerable acute intense reaction Decreased risk of tumor population High control rate Better cosmesis Minimal radiation morbidity Day care procedure LI MI TATI ONS & DI S ADVANTAGES Difficult for inaccessible regions Limited for small tumors (T1_T2) Invasive procedures, require GA Higher dose inhomogeneity Greater conformation –small errors in placement of sources lead to extreme changes from the intended dose distribution Radioactive hazards (not now) Costly S ELECTI ON CRI TERI A Easily accessible lesions Early stage diseases (Ideal implant ≤ 5 cm) Well localized tumor to organ of origin No nodal or distant metastases No local infections or inflammation Favorable histology- mod. diff. i.e. SCC Non DM / HTN Proliferative/ ulcerative lesions preferred I NDI CATI ONS RADICAL RADIATION Skin malignanciesBCC, SCC Head & neck cancers Ca cx Ca prostate BOOST AFTER EXT.RT±CCT Head & neck cancers Ca Breast Esophagus Anal canal I NDI CATI ONS . . . PERIOPERTIVE STS Ca Breast POSTOP Ca Endometrium Ca cx Ca Breast PALLIATIVE Bronchogenic Ca Biliary duct malignancy Ca Esophagus Recurrent tumors BENIGN Keloids / Pterygium OTHERS Endovascular/Rad. stent CLAS S I F I CATI ON Positioning of Radionuclide Dose rate of irradiation Classification Schemes Duration of irradiation Loading pattern CLAS S I F I CATI ON SURGICAL APPROACH / POSITIONING SOURCE IN TUMOR INTERSTITIAL INTRACAVITARY INTRALUMINAL ENDOVASCULAR SOURCE IN CONTACT BUT SUPERFICIAL SURFACE BRACHYTHERAPY/ MOULAGE DURATION OF IRRADIATION TEMPORARY-Cs137,Ir192 PERMANENT-I125,Au198 DOS E RATE( I CRU 3 8 ) LOW DOSE RATE (LDR) 0.4-2 Gy/hr Bed confinement LDR A/L : Cs137 MEDIUM DOSE RATE (MDR) 2-12 Gy/hr HIGH DOSE RATE (HDR) > 12 Gy/hr ULTRA LOW DOSE RATE 0.01-0.3 Gy/hr ROUGHLY LDR – 10 Gy/day MDR -10 Gy/hr HDR – 10 Gy/min ADVANTAGES LDR HDR Predictable clinical effects SHORT T/T TIME Superior radiobiological Geometry well maintained Less morbidity, control is comfort Day care procedure role best Well practised since long Minimum intersession variability in dose distribution Better patient compliance / OPTIMIZATION NO RADIATION HAZARDS SMALL APPLICATOR Less tissue trauma Better packing MDR BRACHYTHERAPY ADVANTAGES Comparative shorter T/T time One time treatment can be used Patient convenience Radio biologically acceptable nearer to LDR Brachytherapy DISADVANTAGES Late complications increases if correction not done S OURCE LOADI NG TECHNI QUE PRELOADING SYSTEM Live sources ADVANTAGES Clinical results are best Affordable Long term results with lesser morbidities DISADVANTAGES Radiation hazards Special instruments Difficult application / hasty Geometry not maintained ? Optimization AF TER LOADI NG TECHNI QUE MANUAL Avoids radiation protection issue of preloading Better applicator placement Verification prior to source placement Min. radiation hazard Advantages of preloading REMOTE CONTROLLED No radiation hazard Accurate placement Geometry maintained Better dose distribution Highly precise Short T/T time Day care procedure Mainly used for HDR I NTERS TI TI AL BRACHYTHERAPY Sealed Radioactive sources directly implanted into the tumor in a geometric fashion First suggested by Alexander Graham Bell ADVANTAGES Higher local dose in shorter time Rapid dose fall Better tumor control Lesser radiation morbidities Superior cosmetics Functional preservation of organs I NTERS TI TI AL BRACHYTHERAPY… DISADVANTAGES Radiation hazards in older days Costly Not applicable to inaccessible areas INTENTION OF TREATMENT Always RADICAL As radical brachytherapy alone (smaller lesions) Local boost in combination with EBRT (larger lesion) NEVER USED FOR PALLIATION S ELECTI ON CRI TERI A Easily accessible lesions, at least from one side Early stage disease T 1-T2 and sometimes early T3 Ideally total size of implant ≤ 5 cm Non DM /HTN No local infection Proliferative and ulcerative lesions preferred CLI NI CAL APPLI CATI ONS Head & neck tumors Early stage oropharyngeal cancers Ca breast- Boost /PBI Ca prostate Soft tissue sarcoma Gynecologic malignancies Ca anal canal and rectum Ca lung and pancreas TYPES OF I NTERS TI TI AL I MPLANTS ACCORDI NG TO S I ZE/LOCATI ON/PROXI MI TY OF TUMOR TO NORMAL S TRUCTURES TEMPORARY PERMANENT Radioactive sources Preloaded – rigid needle removed after desirable dose has been delivered Rigid stainless steel needles/flexible Teflon / nylon guides/plastic tubes Preloaded/After loaded eg. Ra226 ,Cs137 After loaded – Manual/ Remote Advantages Flexibility of implant design Reduction of radiation exposure levels resulting in more accurate placement of needles and guides S YS TEMS OF I MPLANT DOS I METRY OBJECTIVES OF TREATMENT PLANNING To determine the distribution & type of radiation sources to provide optimum dose distribution To provide complete dose distribution in irradiated volume SYSTEM USED Paterson-Parker (Manchester) system Quimby system (Memorial) system Paris system – Pierquin, Chassagne , Dutreix and Marinello Computer System S YS TEMS OF I MPLANT DOS I METRY These system designed during times when computers were not available for routine planning Extensive table & elaborate rules of source distribution were devised to facilitate the process of manual treatment planning These systems differ in rule of implantation, definition of dose uniformity & method used in reference dose specification RULES OF I NT. I MPLANT PARAMETERS MANCHESTER QUIMBY PARIS S YS TEM COMPUTER Linear strength Variable Constant Constant Constant Source distribution Planar implant:(periphery) Area <25 cm- 2/3 Ra; 25-100 cm- ½ Ra; >100 cm1/3 Volume implant::Cylinder:belt-4 parts,core-2,end-1 Sphere:shell-6,core-2 Cube :each side-1,core-2 Constant approx. 1 cm apart from each other or from crossing ends Uniform Uniform Uniform Uniform Line sources Line sources parallel Parallel or planes cylinderic volumes Same as Manchester Constant, Selective Separation 8-15 mm Constant Selective Required to enhance dose at implant ends Same Crossing needles not used;active length 3040% longer Crossing needles not used;active length 3040% longer Spacing line source Crossing needles COMPONENTS - CLAS S I CAL SYS TEM DISTRIBUTION RULES: given a target volume, distribution rules determine how to distribute RA sources & applicators in & around target volume DOSE SPECIFICATION & IMPLANT OPTIMIZATION CRITERIA: Each system has a definition of prescribed dose Above 2 criteria determine dose homogeneity, normal tissue sparing, no. of catheters implanted & margins around target DOSE CALCULATION AIDS: Older systems used tables that give dose delivered per mg Ra-Eq-hr as a function of treatment volume or area Recent Paris system uses computerized treatment planning to relate absorbed dose to source strength & PRI NCI PLE- MANCHES TER SFEATURES YS TEM DOSE & DOSE RATE 6000-8000 R in 6-8 days (1000 R/day; 40 R/hr) UNIT / USE OF RADIUM mg Ra hr – defined as amount of radium to give specified dose in 1 hr DOSE SPECIFICATION CRITERA Effective minimum dose 10% above absolute minimum dose LINEAR ACTIVITY Variable: 0.66 and 0.33 mg RaEq/cm QUI MBY S YS TEM Developed by Edith Quimby et al Dose 5000-6000 R in 3-4 days Equal linear intensity (mg RaEq/cm) needles distributed uniformly (fixed spacing) in each implant, although spacing selected in 1-2 cm range acc. to implant size Quimby tables (Nomogram ) give mg RaEq-hr to deliver stated exposure of 1000 R as function of T.V. or area (5000-6000 R over 3-4 days; 60-70 R/hour) No clear description of rules for distributing Ra needles Crossing recommended; peripheral needles placed on or beyond T.V. boundaries Dose specification criteria inconsistent NOT RECOMMENDED FOR CLINICAL USE PARI S S YS TEM- PRI NCI PLES RADIOACTVE SOURCES Rectilinear/parallel -arrangement so that centers are located in the same plane which is perpendicular to the direction of sourcesCENTRAL PLANE Equidistant Linear activity-uniform and identical Source geometries Linear- single-plane implants Squares/Equilateral triangles- two plane implants PARI S S YS TEM FEATURES DOSE AND DOSE RATE 6000 -7000 cGy in 3-11 days DOSE PRESCRIPTION Average of the minimum doses in the region defined by the POINT source REFERENCE DOSE & DOSE GRADIENT 85 % of the BASAL DOSE 15 % between the Reference dose and the Basal dose RA SOURCE PLACEMENT Reference isodose volume covers the treated volume PERMANENT I MPLANTS ADVANTAGES DISADVANTAGES Less accessible sites Environmental issue Cont. ultra low dose Dosimetric uncertainties > rate>Max biological effectiveness Better tissue heal Better effect in slow and radio resistant tumors Improved mobility Later part of T/T becomes less effective Source displacement Large tumor > Difficult procedure and geometry Radio biologically less effective for rapidly proliferating tumors COMPUTER S YS TEM Implant system evolved through use of computers Implantation rules: Sources of uniform strength Spaced uniformly (1-1.5 cm), larger spacing for larger implants to cover entire T.V. Active length 30-40% longer than Target length as ends uncrossed T.V.: sufficient safety margins; peripheral sources implanted on outer surface Dose specified by isodose surface that surrounds target Whole planning with help of computers COMPUTER DOS I METRY Possible to preplan implants & complete isodose distribution corresponding to final source distribution Rapid & fast; helps modify implant Isodose patterns can be magnified & superimposed on implant radiograph Localization of sources: Orthogonal Imaging method Stereo-shift method CT Dose Calculation: No. of milligrams or millicurie in implant Location of each source with respect to dose calculation point Type of isotope being used Filtration of the encapsulation COMPUTER DOS I MTERY Dose Computation: Dose calculation Formalisms’ (AAPM TG 43 algorithm) Use Sievert Integral directly Precalculated dose tables For Radium & other long lived sources: Dose rates in form of isodose curves For Iridium & relatively short lived implants: Computer calculates cumulative dose with decay correction CLI NI CAL AP P L I CATI ONS Oral Cavity: LIP: Indications: T1-2N0 Lesions T.V.: All visible & palpable tumour with 5-10 mm margin Dose: 50-70Gy in 5-7 days LDR Technique: Rigid afterloading needles maintained in place by Template Classical plastic tubes Spacers to decrease dose to gingiva, teeth & other lip CLI NI CAL APPLI CATI ONS … Buccal Mucosa: Indications: Brachytherapy alone indicated for small (<4cm), welldefined lesions in anterior 2/3rd As boost after EBRT for larger lesions T.V.: GTV + margins Dose: Alone 65-70 Gy Boost 25-30 Gy Technique: Guide Gutter Technique: Lesion < 2cm Plastic tube technique: For other lesions CLI NI CAL APPLI CATI ONS … Oral Tongue: Indications: T1 N0, T2 N0 < 3cm lesion T.V.: GTV + 5 mm margin Dose: Alone:60-65 Gy LDR Boost 20-25 Gy after EBRT dose of 45-50 Gy Techniques: Guide-gutter technique AP X-ray CLI NI CAL APPLI CATI ONS … Floor of Mouth: Indications: T1-2N0 lesions, ≥ 5 mm away from mandible Dose: Techniques same as for Tongue implants Complication: Osteoradionecrosis:5-15% Oropharynx: Indications: Ca BOT, soft palate, tonsillar fossa & vallecula usually as boost after EBRT Lesions < 5 cm (after EBRT) T.V.: GTV + 10 mm margin Dose: Tonsillar fossa-25-30 Gy; BOT 30-35 Gy Technique: Classical Plastic Loop technique CLI NI CAL APPLI CATI ONS … Breast Indications: Boost after BCS & EBRT Postoperative interstitial irradiation alone of the primary tumor site after BCS in selected low risk T1 and small T2N0 (PBI) As sole modality As Boost to EBRT Patient choice: cannot come for 5-6 wks treatment : Close, positive or unknown margins Distance Lack of time Elderly, frail, poor health patient EIC Large breasts: unacceptable toxicity Younger patients Deep tumour in large breast Irregularly thick target vol. Moderator: Prof. S. C. Sharma Chest wall recurrences CLI NI CAL APPLI CATI ONS … T.V.: Primary Tumor site + 2-3 cm margin Dose: As Boost: 10-20 Gy LDR AS PBI: 45-50 Gy in 4-5 days LDR (30-70 cGy/hour) 34 Gy/10#, 2# per day HDR Technique: Localization of PTV: Surgical clips (at least 6) USG, CT or MRI localization, Intraop USG During primary surgery Guide needle technique or Plastic tube technique using Template Double plane implant Skin to source distance: Minimum 5 mm CLI NI CAL APPLI CATI ONS … CLI NI CAL APPLI CATI ONS … Prostate: Indications Brachytherapy as monotherapy: Stage T1-2a & Gleason score 2-6 & PSA ≤ 10 ng/ml As boost after EBRT Stage T2b, T2c or Gleason score 7-10 or PSA > 10 ng/ml For brachytherapy, Prostate size < 50 cc Exclusion criteria: Life expectancy < 5 yrs Large or poorly healed TURP defect Distant Mets or operative risk T.V.: Whole prostate within capsule + 2-3 mm margin Methods: Permanent Implant (I125 or Pd103) or Temporary Implant (Ir192) CLI NI CAL APPLI CATI ONS … Technique for Permanent implant Retropubic approach with I125 seedsDisappointing results Modern technique: Transperineal Approach TRUS guided Two step approach Volume study of prostate Computer planning Seed positioning Coverage check -USG & Flouroscopy Check Cystoscopy Post-implant image based dosimetry CLI NI CAL APPLI CATI ONS Dose: I125: 145 Gy as sole RT 100-110 Gy as boost to 40-50 Gy EBRT Pd103: 125 Gy as sole RT 90-100 Gy as boost to 40-50 Gy EBRT Temporary Implants with Ir192 (LDR or HDR): Procedure same as above; lesser no. of plastic catheters required (8-15) Dose: LDR 30-35 Gy seeds left for 3 days(Boost to 45 Gy EBRT) HDR 20-25 Gy, 4-6 Gy/#(Boost to 45 Gy EBRT) CLI NI CAL APPLI CATI ONS Soft tissue Sarcomas (using Ir192 or I125) Indications: As sole postop RT: completely resected intermediate or high grade tumours of extremity or superficial trunk with -ve margins As boost to postop EBRT: Intermediate or high grade sarcoma with +/- margins Postop pts with small lesions & +ve/uncertain margins Deep lesions Low grade sarcomas T.V.: GTV + 2-5 cm margin GTV based on preop MRI & clinical findings Dose: LDR (Ir seeds or wires) as sole treatment 45-50 Gy in 4-6 days As boost to 45-50 Gy EBRT: 15-25 Gy in 2-3 days CLI NI CAL APPLI CATI ONS … Technique: Usually performed at time of surgery Basic or sealed end temporary implant technique CLI NI CAL APPLI CATI ONS … Brain: Permanent or temporary (using I125 or Ir192 seeds/wires ) Indications: As boost to EBRT or recurrence Anaplastic astrocytoma or GBM, unifocal, well cicumscribed, peripheral lesions & < 5 cm in diameter T.V.: Contrast enhancing area on MRI +/- 5mm margin Dose: LDR 50-60 Gy, 0.4-0.5 Gy/hr Technique: Planning CT/MRI done CLI NI CAL APPLI CATI ONS … Ca Anorectum Indications: As boost to EBRT/ChemoRT If T.V. doesnot exceeds 1/2 circumference, 5 mm thick, 5 cm long i.e. T1-2 & small T3 lesions T1N0 adenocarcinoma of rectum 3-10 cm above anus T.V.: Visible palpable tumor+5 mm Dose: LDR 15-20 Gy at 0.3-0.6 Gy/hr Technique: Guide needle technique with template CLI NI CAL APPLI CATI ONS … Gynecological Tumors (Ir192 LDR or HDR) Indications: Ca Cervix Ca Endometrium Postop local recurrence Ca Vagina & Vulva Radical BT in select early lesions (T1-2N0) Boost after EBRT in large lesions (T2-3N1) Technique: Guide-gutter technique Blind plastic tube implant (transperineal technique) Plastic or guide needles CLI NI CAL APPLI CATI ON – CA CX ABS Recommendations Bulky primary disease Prior hysterectomy-inability to place tandem Post hysterectomy vault recc./cut-through hysterectomy/cervical stump presentation Extesive parametrial involvement Distorted anatomy Narrow vagina & fornices Extensive / Distal vaginal wall involvement Re-irradiation after recurrences Prior course of RT to area of interest CLI NI CAL APPLI CATI ONS … PERINEAL IMPLANTS Martinez Universal Perineal Interstitial Template (MUPIT) Syed-Neblett template CLI NI CAL APPLI CATI ONS … Dose: Radical BT: LDR: 55-60 Gy @ 50-90 cGy/hr HDR: 3.5 Gy/#@ 2#/day/12-16# Boost LDR: 15-25 Gy , 50-90 cGy/hr HDR: as above, no. of # depend upon EBRT doses CLI NI CAL APPLI CATI ONS … Other sites: Lung: Permanent perioperative BT, I125 seeds, Au198 Grains Persistent or recurrent ds after EBRT or residual ds after surgery Pancreas: Permanent perioperative BT, I125 seeds Locally advanced unresectable ds Penis & Urethra: I NTRACAVI TARY APPLI CATI ON Radioactive sources are placed in a existing cavity usually inside a predefined applicator with special geometry Uses: Cervix Endometrium Vagina Maxilla Nasopharynx PARI S S YS TEM Single application of radium Two cork colpostats (cylinder) and an intrauterine tube Delivers a dose of 7000- 8000 mg-hrs of radium over a period of five days(45R/hr) (5500mg/hr Equal amount of radium used in the uterus and the vagina Intrauterine sources 3 radioactive sources, with source strengths in the ratio of 1:1:0.5 colpostats sources with the same strength as the topmost uterine source S TOCKHOLM S YS TEM Fractionated course of radiation delivered over a period of one month. Usually 2-3 applications, each for a period of 20- 30 hours (repeated 3weekly) Intravaginal boxes -lead or gold intrauterine tube -flexible rubber Unequal loading 30 - 90 mg of radium in uterus 60 - 80 mg in vagina Total prescribed dose -6500-7100 mg Ra 4500 mg Ra contributed by the vaginal box (dose rate-110R/hr or 2500mg/hr/#) DRAWBACKS OF PARI S AND S TOCKHOLM S YS TEMS Long treatment time Discomfort to the patient No dose prescription MANCHES TER S YS TEM To define the treatment in terms of dose to a point. Criteria of the point: Anatomically comparable Position where the dosage is not highly sensitive to small alteration in applicator position Allows correlation of the dose levels with the clinical effects To design a set of applicators and their loading which would give the same dose rate irrespective of the combination of applicators used To formulate a set of rules regarding the activity, relationship and positioning of the radium sources in the uterine tumors and the vaginal POINT A PARACERVICAL TRIANGLE where initial lesion of radiation necrosis occurs Area in the medial edge of broad ligament where the uterine vessel cross over the ureter The point A -fixed point 2cm lateral to the center of uterine canal and 2 cm from the mucosa of the lateral fornix POINT B Rate of dose fall-off laterally Imp. Calculating total dose-Combined with EBRT Proximity to important OBTURATOR LNs Same level as point A but 5 cm from midline Dose ~20-25 % of the dose at point A LOADI NG OF APPLI CATORS In order that point A receives same dosage rate no matter which ovoid combination is used ,it is necessary to have different radium loading for each applicator size Dose rate 57.5 R/hr to point A Not more than 1/3 dose to point A must be delivered from vaginal radium APPLICATORS LOADI NG PATTERN TUBE TYPE LENGTH TUBES RADIUM (mg) UNITS (FUNDUS to CX) LOADING TUBES (mg) LARGE 6 3 35 6-4-4 15-10-10 MEDIUM 4 2 25 6-4 15-10 SMALL 2 1 20 8 20 VAGINAL OVOIDS TUBES RADIUM (mg) UNITS LOADING TUBES(mg) LARGE 3 22.5 9 10-10-5 or 20/25 MEDIUM 2 20 8 20 SMALL 1 17.5 7 10-5-5 or 20/15 GUI DELI NES Largest possible ovoid Lesser dose to mucosa Longest possible tandem (not > 6 cm) Better lateral throwoff Smaller dose to mucosa Dose to point A- 8000R Dose to uterus wall -30,000R Dose to vaginal mucosa-20,000R Dose to recto-vaginal septum- 6750 R Dose limitation BLADDER <80 Gy RECTUM <75 Gy I NTRACAVI TARY APPLI CATORS MANCHESTER PGI I DEAL APPLI CATI ON Tandem 1/3 of the way between S1 –S2 and the symphysis pubis Midway between the bladder and S1 -S2 Bisect the ovoids Marker seeds should be placed in the cervix Ovoids against the cervix (marker seeds) Largest Separated by 0.5-1.0 mm Axis of the tandem-central Bladder and rectum -should be packed away from the implant I CRU REPORT NO. 3 8 DOSIMETRIC INFORMATION FOR REPORTING Complete description Technique Time-dose pattern Treatment prescription Total Reference Air Kerma Dose description Prescription points/surface Reference dose in central plane Mean central /peripheral dose Volumes: Treated/ point A/ reference volume Dose to Organs at Risk : bladder, rectum REFERENCE VOLUME Dimensions of the volume included in the corresponding isodose The recommended dose 60 Gy TREATED VOLUME Pear and Banana shape Received the dose appropriate to achieve the purpose of the treatment, e.g., tumor eradication or palliation, within the limits of acceptable complications IRRADIATED VOLUME Volumes surrounding the Treated Volume Encompassed by a lower isodose to be specified, e.g., 90 – 50% of the dose defining the Treated Volume Reporting irradiated volumes may be useful for interpretation of side effects outside CERVI CAL BRACHYTHERAPY ABS . DOS E AT REF ERENCE NTS POINT POI BLADDER RECTAL POINT LYMPHATIC TRAPEZOID OF FLETCHER LOW PA, LOW COMM.ILIAC LN & MID EXT ILIAC LNs PELVIC WALL POINTS DISTAL PART OF PARAMETRIUM & OBTURATOR LNs DOSE SCHEDULE LDR (<200cgy/hr) 35-40 Gy at point A MDR (200-1200cgy/hr) 35 Gy LDR EQUIVALENT at point A HDR(>1200cgy/hr) 9 Gy in 2 # 6.8Gy in 3# at point A EXTERNAL RT WI TH BRACHYTHERAP Y Brachytherapy can follow external irradiation SIMULTANEOUS Stage I - II with very minimal parametriun involvement HDR -5 sessions (9gy /#/ 5, 1week apart) 40 Gy by XRT simultaneously SANDWICH Stage I-II MDR 40 Gy LDR eq.—› XRT 40 Gy —› MDR 35 Gy LDR eq. In both above cases a MIDLINE SHIELD is used POS T OP/ VAULT BRACHYTHERAPY Vault RT No residual disease 8500 cGy at 5mm from the surface of the vault 2 sessions 1 week apart Residual disease CTV of 2 cm given to gross tumor and the prescription of 8500cgy encompassing the whole CTV is made 2 sessions 1 week apart Mostly after XRT POS T OP BRACHYTHERAPY CONTRAINDICATIONS Vaginal wall involvement ( middle- lower 1\3) Heavy parametrium infiltration VVF or VRF Inadequate space Medical contraindications Metastatic disease Supplementary radiation 2000 cGy \10# \ 2 weeks S URF ACE MOULDS Radiation is delivered by arranging RA sources over the surface of tumor Types Planar Circular Square Rectangular Line source Cylinder I NDI CATI ONS Superficial /Accessible tumors Skin ca Post mastectomy recurrence Oral tumor hard palate ,alveolus Penile carcinoma CI RCULAR MOULDS Amount of radium used is obtained from the table for a particular treating distance Circular arrangement is the best Space between the needles (end) should not be more than H S QUARE MOULDS An arrangement is considered to be linear if the distance between the active end of the sources does not exceed the height Length of the side of the square is less than twice the height No further radium is placed in the center RECTANGULAR MOULDS The dividing lines or bars are placed parallel to the longer side Elongation correction factor: Increase the reading in milligrams hour by a given factor This factor is proportional to the ratio of the sides of the rectangle 1.5:1 = 2.5% 2:1 = 5% 3:1 = 9% 4:1 = 12% CI RCULAR MOULDS CURVED SURFACES Irregular area Curved surfaces: convex, concave The smaller area is used for calculation of radium dose and implant rules Cylinder mould: Amount of radium is 30D2 COAXIAL RINGS DISTRIBUION RULES In case of coaxial rings radium is placed at a distance equal to 2H I NTRALUMI NAL BRACHYTHERAPY Radioactive source is passed through a tube and passed into a hollow lumen Sites Esophagus Bronchus : Bronchogenic carcinoma Definitive : T1-T2tumors Palliative Dyspnea Cough Atelectasis Biliary tract RADI OBI OLOGY Biological effects depend on Dose prescribed Treated volume Dose rate Fractionation Treatment duration Heterogeneous dose distribution Higher average dose Short treatment RADI OBI OLOGY – 4 Rs Repair Reassortment / redistribution Repopulation Reoxygenation RADI OBI OLOGY- LDR Repair of Sublethal damage Most significant- 1 Gy/min and 0.3 Gy /h DNA repair Dynamic process Special kinetics Simple exponential kinetics Reassortment - slow and imp. <1 Gy/min Repopulation-slowest and significant Reoxygenation - relative slow process may be a disadvantage LDR AND HDR LDR vs HDR EFFECTS OF HDR RADI OACTI VE S OURCES Naturally occurring Artificial Induced by neutron bombardment Induced by bombardment of protons Fission product CHARACTERISTICS HALF LIFE GAMMA ENERGY BETA ENERGY HALF VALUE LAYER EXPOSURE RATE CONSTANT BETA FILTRATION DECAY SCHEME I DEAL RADI ONUCLI DE Photon energy :low to medium- 0.03 to 0.5 MeV Monoenergetic beam preferred Moderate Gamma ray constant Long half life High specific activity Isotropic No gaseous disintegration/daughter product Nuclei should not disperse if source damaged Low beta energy Low or no self attenuation Insoluble and nontoxic Flexible Easily available and cost effective Withstand sterilization process Disposable without radiation hazards to environment RADI UM 2 2 6 Sixth member of the radio active series which starts with uranium and ends with lead Half life 1620 years Gamma energy 0.83 MeV Half value 12mm Pb Exposure rate constant 8.25 Rcm2/mCi-h Filtration 0.5 – 1 mm Pt RADI UM S UBS TI TUTES NAME ORIGIN T1/2 γ β β ENERG ENERGY FILTRATI Y-MeV ON Rn 222 NATURAL 3.83 days 0.83 Cs 137 FISSION 30.17 0.662 yrs Co 60 NEUTRON 5.26 yrs ACTIVAT. - do 73.8 Ir 192 yrs Stainless steel HVL ERC SPECI (Pb . -mm ACTI. )12 10.27 DECAY PRODU CT Ba 137 87 Pb 206 0.512 1.17 - do - 6.5 3.26 1.17, 1.33 0.38 - do- 11 13.07 1020 Ni 60 0.1361.06 0.0790.068 Platinum 4 4.69 Pt 192 - Platinum 12 6.87 - 7760 Tn 182 - do - 115 yrs 0.67 Au 198 - do - 2.7 days 1.0880.412 0.96 St. steel 3.3 2.376 - Hg 198 I 125 59.4 days 0.274, 0.314 No Titanium 0.01 10th 1.403 - Te 125 No Platinum 0.03 6.87 - Ru 103 - do - Pd 103 - do - 16.97 0.21 -