Nursing Care Plan: Impaired Gas Exchange, Airway Clearance, Falls
advertisement
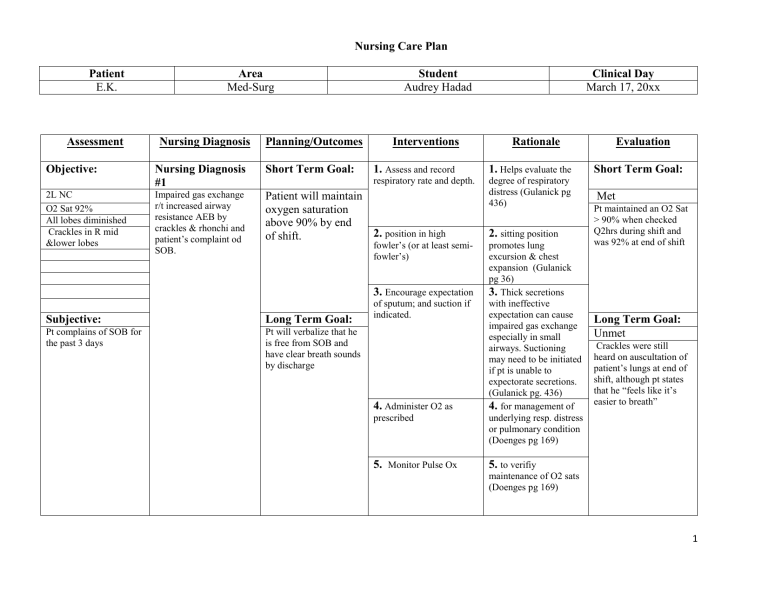
Nursing Care Plan Patient E.K. Assessment Objective: 2L NC O2 Sat 92% All lobes diminished Crackles in R mid &lower lobes Area Med-Surg Nursing Diagnosis Planning/Outcomes Student Audrey Hadad Interventions Nursing Diagnosis #1 Short Term Goal: Impaired gas exchange r/t increased airway resistance AEB by crackles & rhonchi and patient’s complaint od SOB. Patient will maintain oxygen saturation above 90% by end 2. position in high of shift. 1. Helps evaluate the respiratory rate and depth. degree of respiratory distress (Gulanick pg 436) 3. Encourage expectation Long Term Goal: Pt complains of SOB for the past 3 days Pt will verbalize that he is free from SOB and have clear breath sounds by discharge Rationale 1. Assess and record fowler’s (or at least semifowler’s) Subjective: Clinical Day March 17, 20xx of sputum; and suction if indicated. 4. Administer O2 as prescribed 5. Monitor Pulse Ox 2. sitting position promotes lung excursion & chest expansion (Gulanick pg 36) 3. Thick secretions with ineffective expectation can cause impaired gas exchange especially in small airways. Suctioning may need to be initiated if pt is unable to expectorate secretions. (Gulanick pg. 436) 4. for management of underlying resp. distress or pulmonary condition (Doenges pg 169) Evaluation Short Term Goal: Met Pt maintained an O2 Sat > 90% when checked Q2hrs during shift and was 92% at end of shift Long Term Goal: Unmet Crackles were still heard on auscultation of patient’s lungs at end of shift, although pt states that he “feels like it’s easier to breath” 5. to verifiy maintenance of O2 sats (Doenges pg 169) 1 Nursing Care Plan Assessment Objective: Pt has ineffective cough, diminished breath sounds in both lungs and crackles and rhonchi are auscultated in Rt lung Subjective: Pt states that he “coughs and nothing comes out” Audrey Hadad Nursing Diagnosis Planning/Outcomes Nursing Diagnosis #2 Short Term Goal: Ineffective airway clearance r/t immobilized secretions AEB crackles and rhonchi in lungs Patient will demonstrate effective cough and expectorate sputum by end of shift Interventions Rationale 1. Auscultate patient’s 1. to evaluate/establish chest baseline of characteristics of and presence of breath sound (Doenges pg 168) 2. fluids prevents dehydration and help keep secretions thin (Gulanick pg 436) 2. Encourage intake of fluid 3. Encourage activity and 3 Activity helps position changes q2hrs mobilize secretions and prevent pooling in lungs (Gulanick pg 436) Long Term Goal: Patient will maintain a patent airway and 4. Encourage pt to cough out secretions / sputum have clear breath sounds by discharge 5. Teach controlled cough techniques ie Huff Evaluation Short Term Goal: Met Client demonstrates controlled cough – huff and acknowledges an understanding of the rationale, he also began to cough up small amounts of sputum Long Term Goal: Unmet 4. Coughing is the most Crackles were still heard helpful way to clear secretions (Gulanick pg 436) 5. Forced expiration coughing may be effective to move trapped mucus into larger airways for pt to couch up (Gulanick pg 436) on auscultation of patient’s lungs at end of shift 2 Nursing Care Plan Assessment Objective: Age 78 Has weak gait Has DM IV peripheral line Acute illness (pneumonia ) Audrey Hadad Nursing Diagnosis Nursing Diagnosis #3 Risk for Falls r/t presence of an acute illness AEB client’s statement of lightheadedness Planning/Outcomes Short Term Goal: Interventions 1.Evaluate degree of risk 1. standard fall risk for falls on admission assessment tool can determine level of risk (Gulanick pg65) Patient will be free from injury- falls during this shift 2. Review med regimen 2. Certain meds (anti – and how it can effect client locked position and raise upper half of side rails hypertensives) can contribute to weakness & gait/balance disturbances (Doenges pg 365-366) 3. These have been by research to reduce falls (Gulanick pg66) 4. Encourage and teach Pt 4. Non-skid footwear to wear non-skid socks while in the hospital and at home non-skid socks/slippers/shoes 5. Place personal items with-in close reach including call light provides sure footing (Gulanick pg66) 3. Place bed in low, Subjective: Stated that he was feeling light-headed when he was SOB Long Term Goal: Pt will verbalizes behaviors to protect self from injury – falls before discharge Rationale 6. Instruct Pt to use call light to request assistance before getting out of bed 5. Stretching for items can disturb Pt’s balance and contribute to falls (Gulanick pg66) Evaluation Short Term Goal: Met No falls during this shift Long Term Goal: Met Patient states that he will wear hir nonskid socks while in the hospital and use his call light to get assistance before getting out of bed 6. Assistance in ambulation reduces risk for falls (Doenges pg 366) 3 Nursing Care Plan Audrey Hadad References Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2013). Nurse's pocket guide: diagnoses, prioritized interventions, and rationales (13th ed.). Philadelphia: F.A. Davis. Gulanick, M., & Myers, J. L. (2014). Nursing care plans: Diagnoses, interventions, and outcomes (8th ed.). Philadelphia: Elsevier Mosby Vallerand, A. H., Sanoski, C. A., & Deglin, J. H. (2015). Davis's drug guide for nurses (14th ed.). Philadelphia: F.A. Davis Company 4