ACCEPTANCE AND COMMITMENT THERAPY
FOR THE TREATMENT OF PERFECTIONISM
A Dissertation
Presented to the Faculty of the
School of Human Services Professions
Widener University
In Partial Fulfillment
Of the Requirements for the Degree
Doctor of Psychology
By
Steven Bisgaier
Institute for Graduate Clinical Psychology
January 2018
ProQuest Number: 10816869
All rights reserved
INFORMATION TO ALL USERS
The quality of this reproduction is dependent upon the quality of the copy submitted.
In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion.
ProQuest 10816869
All rights reserved.
This work is protected against unauthorized copying under Title 17, United States Code
Microform Edition © ProQuest LLC.
ProQuest LLC.
789 East Eisenhower Parkway
P.O. Box 1346
Ann Arbor, MI 48106 - 1346
Copyright by
Steven Bisgaier
2018
Abstract
Perfectionism is prevalent in a wide range of psychiatric disorders (e.g., depression, anxiety, disordered eating, OCD, PTSD) and physical health problems (e.g., chronic pain, migraine, asthma, fatigue). Acceptance and Commitment Therapy (ACT) protocols have been developed to treat perfectionism, yet no studies have evaluated its effectiveness. This pilot study examined the effectiveness of ACT in treating perfectionism in five undergraduate students with perfectionism as a primary feature of either generalized anxiety disorder or depression. The study used a one-group pretest-posttest design. Individual treatment lasted between seven and twelve sessions and was administered flexibly (i.e., non-manualized). Acknowledging the small sample size, significant improvement with large effect sizes were found on measures of depression ( p =
.012, d = 1.98), general anxiety ( p
= .011, d = 2.01), social anxiety ( p
= .009, d = 2.11), general distress ( p
= .008, d = 2.17), frequency and awareness of thoughts related to perfectionism ( p
=
.003, d = 3.00), psychological flexibility ( p
= .017, d = 1.76), cognitive fusion ( p
= .013, d =
1.89), and commitment to values-consistent action ( p
= .050, d = 1.24). These findings provide preliminary support for the effectiveness of ACT as a treatment for perfectionism and the need for a future randomized control trial. The study suggests three primary mechanisms of change: 1) reduction in experiential avoidance; 2) increase in cognitive defusion; and 3) clarification of personal values. The study adds to existing evidence indicating that direct and explicit treatment of perfectionism can provide remittance of symptoms of other mental health issues.
Key words: perfectionism, acceptance and commitment therapy, ACT, case study, college students
Table of Contents
Abstract .......................................................................................................................................... iv
List of Tables ................................................................................................................................ vii
List of Appendices ....................................................................................................................... viii
Acceptance and Commitment Therapy for the Treatment of Perfectionism .................................. 1
The Clinical Importance of Perfectionism .................................................................................. 2
Measures and Definitions of Perfectionism ................................................................................ 3
Perfectionism as a Maladaptive Construct .................................................................................. 4
Treatment for Perfectionism ....................................................................................................... 6
Overview of ACT ....................................................................................................................... 7
ACT for the Treatment of Perfectionism .................................................................................... 8
Method ............................................................................................................................................ 9
Participants .................................................................................................................................. 9
Therapist ................................................................................................................................... 10
Design ....................................................................................................................................... 10
Measures ................................................................................................................................... 10
Treatment Overview and Core Process Targets........................................................................ 12
ACT introduction and creative hopelessness ........................................................................ 13
Cognitive defusion ................................................................................................................ 15
Experiential avoidance and acceptance ................................................................................ 17
Values-consistent action ....................................................................................................... 18
Present-moment awareness and exposure ............................................................................. 20
Self-as-context ...................................................................................................................... 22
Self-compassion .................................................................................................................... 22
Results and Case Descriptions ...................................................................................................... 24
The Case of Daniel.................................................................................................................... 26
The Case of Sara ....................................................................................................................... 29
The Case of Chloe ..................................................................................................................... 33
The Case of Margaret................................................................................................................ 36
The Case of Tamara .................................................................................................................. 40
General Discussion ....................................................................................................................... 42
Limitations ................................................................................................................................ 46
Conclusion ................................................................................................................................ 46
References ..................................................................................................................................... 48
List of Tables
Table 1: Pre and Post Data for Psychological Flexibility and Perfectionism Measures … ... 25
Table 2: Pre and Post Data for CCAPS-34 ………………………………………………… 25
Table 3: Pre and Post Data for Group Means ……………………………………………… 25
List of Appendices
Appendix A: Acceptance and Action QuestionnaireII…………………………………… 62
Appendix B: Short Form of the Revised Almost Perfect Scale…………………………… 63
Appendix C: Perfectionism Cognitions Inventory………………………………………… 64
Appendix D: Valuing Questionnaire……………………………………………………….
65
Appendix E: Cognitive Fusion Questionnaire……………………………………………..
66
Appendix F: Study Recruitment Flyer……………………………………………………..
67
Acceptance and Commitment Therapy for the Treatment of Perfectionism
Broadly, perfectionism is commonly defined as the propensity to set and demand excessively high standards for oneself, accompanied by excessive self-criticism, regardless of performance (Frost, Marten, Lahart, & Rosenblate, 1990; Stoeber & Otto, 2006). It is a
1 transdiagnostic process that is predominant in numerous clinical disorders and has been associated with a wide range of physical health problems and social dysfunction. Various psychotherapeutic interventions, including psychodynamic and cognitive behavioral therapies, have been developed and utilized in the treatment of perfectionism with mixed results.
Recently, Acceptance and Commitment Therapy (ACT) has been identified as a a potentially applicable intervention for perfectionism. Protocols have been developed for utilizing ACT to treat perfectionism as a primary problem (Crosby, Armstrong, Nafziger, &
Twohig, 2013), or when it manifests as an underlying feature of other psychological problems, including eating disorders (Sandoz, Wilson, & DuFrene, 2011) and body image dissatisfaction
(Pearson, Heffner, & Follette, 2010). However, studies do not exist that were designed to evaluate the effectiveness of ACT interventions for the treatment of perfectionism.
This dissertation evaluated the use of ACT in the psychotherapeutic treatment of five students who presented at a university counseling center with perfectionism as a primary problem. Students were evaluated at the start and end of treatment on measures designed to determine the efficacy of ACT in reducing symptoms of perfectionism and other mental health conditions and in improving psychological flexibility. The interventions were catalogued to explore how patients experienced and responded to ACT as a treatment for their condition. I predicted that perfectionism, perfectionistic thoughts, and symptoms of various mental health conditions would be significantly reduced, and that psychological flexibility would be
significantly increased.
The Clinical Importance of Perfectionism
While the American Psychiatric Association (APA) has not yet identified perfectionism as an independent diagnosis, perfectionism is recognized as a possible feature of generalized
2 anxiety disorder, obsessive-compulsive disorder, body dysmorphic disorder, hoarding disorder, narcissistic personality disorder, and obsessive-compulsive personality disorder (APA, 2013).
Perfectionism has been described as a transdiagnostic process, appearing as “a major factor that can explain the maintenance of numerous disorders that an ind ividual may experience” (Egan,
Wade, & Shafran, 2012, p. 280). Indeed, an abundance of research has revealed it to be prevalent in a wide range of clinical disorders (Egan, Wade, & Shafran, 2011, 2012), including depression
(Enns, Cox, & Borger, 2001; Hewitt & Flett, 1991a; Huprich, Porcerelli, Keaschuk, Binienda, &
Engle, 2008), anxiety (Frost & DiBartolo, 2002; Gentes & Ruscio, 2014; Hayward & Arthur,
1998), social anxiety (Alden, Ryder, & Mellings, 2002; Antony, Purdon, Huta, & Swinson,
1998; Saboonchi, Lundh, & Öst, 1999), eating disorders (Bardone-Cone et al., 2007; Sassaroli et al., 2008), obsessive-compulsive disorder (Frost & Steketee, 1997; Frost, Novara, & Rhéaume,
2002), and posttraumatic stress disorder (Egan, Hattaway, & Kane, 2014). Additionally, perfectionism has been linked to a variety of physical health problems, including asthma, chronic pain, fatigue, headaches, migraines, and the management of chronic illnesses (Molnar, Sirois, &
Methot-Jones, 2016). Finally, perfectionism has been seen to contribute to various other forms of dysfunction, ranging from suicidality (Hewitt, Flett, Sherry, & Caelian, 2006; O’Connor, 2007) to relationship problems (Habke, Hewitt, & Flett, 1999; Habke & Flynn, 2002; Matte &
Lafontaine, 2012).
Measures and Definitions of Perfectionism
The three most prevalent measures of perfectionism are the Frost Multidimensional
Perfectionism Scale (F-MPS; Frost, Marten, Lahart, & Rosenblate, 1990), the Hewitt and Flett
Multidimensional Perfectionism Scale (HF-MPS; Hewitt & Flett, 1991b), and the Revised
3
Almost Perfect Scale (APS-R; Slaney, Rice, Mobley, Trippi, & Ashby, 2001). These scales all embrace the current view of perfectionism as multidimensional construct. The F-MPS consists of
6 subscales: personal standards (PS; setting high standards for performance); doubts about actions (DA; doubting the quality of performance); concern over mistakes (CM; tendency to be critical of one’s mistakes ); organization (O; placing an emphasis on organization); parental expectations (PE ; placing value on parent’s expectations ); and parental criticism (PC; placing value on parent’s criticism ). The HF-MPS consists of 3 subscales: self-oriented perfectionism
(SOP; setting high standards , stringently evaluating one’s behavior, striving to attain perfection and avoid failure); other-oriented perfectionism (OOP; setting high standards for others, stringently evaluating other’s behavior ); and socially prescribed perfectionism (SPP; believing that others have high standards for you and are stringently evaluating you). The APS-R consists of 3 subscales: high standards (HS; self-performance expectations and standards); order (OR; self-preferences for order and organization); and discrepancy (D; perceived difference between the standards one has for oneself and one’s actual performance). Recently, as part of their
Comprehensive Model of Perfectionistic Behavior (CMPB), Hewitt and colleagues (2017) have expanded their conceptualization of perfectionism, adding interpersonal components (namely, perfectionistic self-promotion, nondisplay of imperfections, and nondisclosure of imperfections) and intrapersonal or self-relational components (automatic ruminative self-statements regarding the attainment of perfection) to the 3 subscales of the HF-MPS.
Each of these measures is highly regarded (Flett & Hewitt, 2015); however, factor analytic studies have consistently winnowed the many subscales identified above down to two
4 central components, commonly referred to as perfectionistic strivings and perfectionistic concerns
(Bieling, Israeli, & Antony, 2004; Cox, Enns, & Clara, 2002; Frost, Heimberg, Holt,
Mattia, & Neubauer, 1993). “ Perfectionistic Strivings ” denotes the perfectionist’s tendency to set excessively high personal standards and to expect perfection of one’s self. These characteristics are captured by the PS subscale of the F-MPS, the SOP subscale of the HF-MPS, and the HS subscale of the APS-R. “ Perfectionistic Concerns ” denotes the perfectionist’s tendency to be highly self-critical regardless of performance and to be overly concerned with the evaluations of others. These characteristics are captured by the DA, CM, PE, and PC subscales of the F-MPS, the SPP subscale of the HF-MPS, and the D subscale of the APS-R. In consideration of these two central constructs of perfectionism, the following working definition of perfectionism was utilized in this study: Perfectionism is the propensity to set and demand unachievably high standards for oneself, accompanied by excessive self-criticism, regardless of performance.
Perfectionism as a Maladaptive Construct
Originally, theorists viewed perfectionism as purely maladaptive and unidimensional.
Early researchers saw perfectionists as people who set unattainably high standards as a consequence of a fear of failure and low self-esteem (Beck, 1976; Horney, 1950; Missildine,
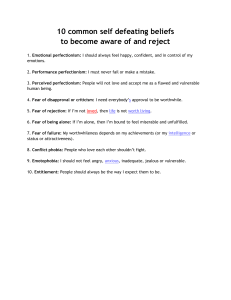
1963). Accordingly, one of the earliest assessments of perfectionism, The Burns Perfectionism
Scale (BPS; Burns, 1980), featured a unidimensional, maladaptive view of perfectionism, with ten questions designed to capture a person’s perfectionism through the lens of various self defeating attitudes (e.g., “If I don’t set the highest standards for myself, I am likely to end up a second-rate person ” ).
This view of perfectionism as exclusively maladaptive was soon contested. In an early, influential work on perfectionism, Don Hamachek (1978) differentiated between “neurotic
5 perfectionists” and “normal perfectionists.” He defined “ normal perfectionism ” as a desirable trait, characterized by a relaxed and careful attitude, increased potential for success, enhanced self-esteem, and a personal sense of satisfaction (Hamachek, 1978). Contrarily, he defined
“neurotic perfectionism” as maladaptive, characterized by a person setting performance standards so unattainable that even his best efforts leave him unsatisfied (Hamachek, 1978). In the years since, other theorists have argued in favor of a positive conceptualization of perfectionism (see Stoeber & Otto, 2006 for a review). Components of the various multidimensional perfectionism scales have been organized by researchers into measures of positive or adaptive perfectionism (e.g., PS and O from the F-MPS, SOP and OOP from the HF-
MPS, and HS and OR from the APS-R), and in some cases these components of perfectionism have been shown to associate with adaptive traits, such as higher levels of positive affect (Frost et al., 1993), conscientiousness and endurance (Stumpf & Parker, 2000), and satisfaction with life (Chang, Watkins, & Banks, 2004).
The counterarguments to the identification of perfectionism as a positive trait are persuasive. The evidence that links perfectionism to psychological and physical health dysfunction are well documented; outweighing evidence to the contrary. Additionally, researchers have argued that what others call adaptive perfectionism is more accurately a separate and distinct personality trait better described as “excessive conscientiousness” or
“ striving for excellence ” (Greenspon, 2000; Hewitt, Flett, & Mikail, 2017).
Ultimately, the apparent disagreement may come down to a case of semantics and practicality. There is a reason why diagnoses in the DSM5 come with the word “disorder”
attached. Perhaps all that is needed to help resolve this issue is a more formal name, such as
Perfectionistic Disorder, Clinical Perfectionism, or Anxiety Disorder with Perfectionistic
Features.
Treatment for Perfectionism
6
Research on the clinical treatment of perfectionism has grown dramatically in the past two decades. Interventions featuring brief psychoeducation (Aldea, Rice, Gormley, & Rojas,
2010), transcendental meditation (Burns, Lee, & Brown, 2011), mindfulness-based bibliotherapy
(Wimberley, Mintz, & Suh, 2016), and coherence therapy (Rice, Neimeyer, & Taylor, 2011) have all been used to reduce symptoms of perfectionism significantly. Additionally, theorists have argued for treating perfectionism with various psychodynamic interventions (Brustein,
2014; Greenspon, 2008; Hewitt et al., 2015; Hewitt et al., 2017). Finally, most perfectionism treatment research features cognitive-behavioral therapy (CBT) interventions. CBT interventions featuring individual therapy (DiBartolo, Frost, Dixon, & Almodovar, 2001; Egan & Hine, 2008;
Ferguson & Rodway, 1994; Glover, Brown, Fairburn, & Shafran, 2007; Hirsch & Hayward,
1998; Riley, Lee, Cooper, Fairburn, & Shafran, 2007; Shafran, Lee, & Fairburn, 2004), group therapy (Handley, Egan, Kane, & Rees, 2015; Kearns, Forbes, & Gardiner, 2007; Richards,
Owen, & Stein, 1993; Steele, Waite, Egan, Finnigan, Handley, & Wade, 2013), manual-based self-help therapy (Pleva & Wade, 2007; Steele & Wade, 2008), and web-based therapy (Arpin-
Cribbie, Irvine, Ritvo, Cribbie, Flett, & Hewitt, 2008; Radhu, Daskalakis, Arpin-Cribbie, Irvine,
& Ritvo, 2012) have all significantly decreased symptoms of perfectionism. Additionally, many of these studies reported that the treatment had a significant effect on measures of depression and/or anxiety (Glover et al., 2007; Handley et al., 2015; Richards et al., 1993; Riley et al., 2007;
Shafran et al., 2004; Steele et al., 2013), eating-disorder symptoms (Handley et al., 2015;
Shafran et al., 2004; Steele & Wade, 2008), and obsessive-compulsive symptoms (Pleva &
Wade, 2007). In a recent review and meta-analysis, Samantha Lloyd and colleagues (2015) concluded that while CBT interventions can significantly reduce aspects of perfectionism in adults with perfectionism appearing as a primary problem or as a problem coinciding with other
7 psychiatric diagnoses , “further research is required to investigate the most effective format of perfectionism interventions” (p. 727).
Overview of ACT
ACT is a transdiagnostic cognitive behavioral therapy with empirical evidence demonstrating it to be an effective treatment for a wide range of clinical problems (Smout,
Hayes, Atkins, Klausen, & Duguid, 2012), including: anxiety (Arch et al., 2012), depression
(Forman, Herbert, Moitra, Yeomans, & Geller, 2007), obsessive compulsive disorder (Twohig et al., 2010), psychosis (White et al., 2011), chronic pain (Wetherell et al., 2011), substance use disorder (Luoma, Kohlenberg, Hayes, & Fletcher, 2012), and disordered eating (Weineland,
Arvidsson, Kakoulidis, & Dahl, 2012). The ACT model views human suffering and maladaptive functioning as a product of psychological inflexibility or rigidity (Hayes, Strosahl, & Wilson,
2012). Psychological inflexibility has been described as a “ rigid, literal, and inflexible style of responding to internal experiences (thoughts, feelings, and physical sensations)” (Crosby et al.,
2013, p. 144). It is defined operationally by six core processes: inflexible attention, disruption of chosen values, inaction or impulsivity, attachment to a conceptualized self, cognitive fusion, and experiential avoidance. Correspondingly, psychological flexibility is defined as a product of six core oppositional processes: flexible attention to the present moment, chosen values, committed action, self-as-context, defusion, and acceptance (note: these terms explained more fully in
“Treatment Overview”). With the goal of improving a person’s psychological flexibility, ACT
seeks to help a person develop the ability to be mindful of – and adopt an accepting attitude towards – her internal experience and to commit to act consistently with her freely chosen values.
ACT for the Treatment of Perfectionism
Although multiple interventions have proven effective to varying degrees for the treatment of perfectionism, researchers and theorists continue to explore alternative avenues for treatment. Recently, ACT has been identified as a potentially applicable intervention for perfectionism. As a transdiagnostic treatment, ACT seems particularly suitable for a transdiagnostic mechanism like perfectionism (Egan et al., 2012). By definition, transdiagnostic
8 treatments like ACT are designed to target underlying critical processes that maintain a wide range of problems.
ACT views the processes of cognitive fusion and experiential avoidance as the “siren songs” of human suffer ing (Strosahl & Robinson, 2008). Both processes are hallmarks of perfectionism.
“ Cognitive fusion ” is the tendency for humans to get caught up or entangled in their internal experiences such that they respond to these experiences literally, without proper regard for context (Hayes et al., 2012). Crosby and colleagues (2013) write, perfectionists ’ thoughts
“ are characterized by rigid and inflexible concern over mistakes, doubts about actions, evaluation of the discrepancy between achievement and standards, self-cr iticism, and a fear of failure” (p.
144) . Hewitt and colleagues (2017) state, “perfectionistic thinking may be so ingrained for some people that it can be activated automatically as a cognitive filter. However, there is still a role for conscious cognition, in the form of preoccupation with shortfalls and ruminating about imperfections” (p. 57).
“ Experiential avoidance ” refers to any attempt to control, suppress, eliminate, or escape from unwanted internal experiences (Hayes et al., 2012). Perfectionists characteristically utilize
9 experiential avoidance to help control or avoid perfectionistic thoughts, feelings, and/or physical sensations (Crosby et al., 2013; Hewitt et al., 2017). Moroz & Dunkley’s (2015) research
“indicate that experiential avoidance is used to deal or cope with the negative feelings associated with self-critical perfectionism, specifically the harsh self-scrutiny and perceived criticism from others” (p. 178). In multiple studies, it has been demonstrated that perfectionism has a significant relationship with measures of experiential avoidance (Crosby, Bates, & Twohig, 2011; Moroz &
Dunkley, 2015; Santanello & Gardner, 2007).
ACT interventions are designed to explicitly target cognitive fusion and experiential avoidance as well as several other complimentary processes. The treatment overview section that follows provides a further elaboration of how ACT processes are utilized in treating expressions of perfectionism.
Method
Participants
The five participants were students at the university at which the researcher was a therapist in the university’s counseling center. Three students enrolled in the study after seeing a flyer (Appendix F) posted on campus. Two students were already receiving services at the counseling center and were transferred to the study based on a determination by the student and their respective therapist that they were appropriate candidates for this treatment. All students completed a comprehensive intake assessment in-person with the researcher. They were deemed eligible for participation based on a subsequent determination by the researcher and his supervisors that the student had perfectionism as a primary problem or as an underlying feature
10 of a secondary problem for which treatment of the perfectionism was deemed indicated. Notably, all participants met DSM-5 (APA, 2013) diagnostic criteria for generalized anxiety disorder (4 students) or major depressive disorder (1 student) upon entering the study.
Therapist
Therapy was conducted by the author who was in his third year of doctoral training at
Widener University ’s Institute fo r Graduate Clinical Psychology. The therapist was trained in
ACT theory and methods as part of his doctoral education, and had attended ACT workshops conducted separately by Steven Hayes, Frank Masterpasqua, Daniel Joseph Moran, John
Armando, and Dennis Tirch. He was supervised weekly by a licensed psychologist with over ten years of clinical experience practicing ACT and over five years of academic experience teaching
ACT at a doctoral-level clinical psychology program.
Design
A one-group pretest-posttest quasi-experimental design was used. Patients were evaluated at intake to determine appropriate candidacy for the intervention. Measures ( see “Measures” ) were administered at the start and end of treatment. The treatment (see “Treatment overview and core process targets”) was designed to be delivered with the intention of no more than twelve weekly, 45-minute sessions.
Measures
The patients completed the Acceptance and Action Questionnaire-II (AAQ-II; Bond et al., 2011; Appendix A). This 7-item self-report measure was used to evaluate each patients’ psychological inflexibility, or their inability to accept negative internal experiences and pursue meaningful action in the presence of these experiences. Patients rated the extent to which each statement described them on a 7-point Likert scale (scores can range from 7 to 49). It has high
internal consistency ( D =.78-.88; Bond et al., 2011), test-retest reliability (r=.81; Bond et al.,
11
2011), construct validity (Fledderus, Oude Voshaar, ten Klooster, & Bohlmeijer, 2012), and convergent, discriminant, and predictive validity (Bond et al., 2011).
The Short Form of the Revised Almost Perfect Scale (SAPS; Rice, Richardson, &
Tueller, 2014; Appendix B), an 8-item self-report measure, was used to identify patients ’ perfectionism. This measure features two subscales (High Standards and Discrepancy) that seek to capture the essential dimensions of perfectionism: high performance expectations and selfcritical attitudes associated with performance evaluation. Patients rated the extent to which they agree with each statement on a 7-point Likert scale (scores can range from 8 to 56). It has high internal consistency and test-retest reliability ( U =.85, .87 for high standards and discrepancy subscales, respectively; Rice et al., 2014). The measure has high convergent and discriminant validity with other perfectionism measures, including the Revised Almost Perfect Scale and the
Frost Multidimensional Perfectionism Scale (Rice et al., 2014).
The Perfectionism Cognitions Inventory (PCI; Flett, Hewitt, Blankstein, & Gray, 1998;
Appendix C), a 25-item self-report measure, was used to identify the frequency of patients ’ automatic thoughts about the need to be perfect and their cognitive awareness of imperfections over the preceding seven days. Patients rated the extent to which they experience each thought
(i.e., from “Not at all” to “All of the Time”) on a 5-point Likert scale (scores can range from 0 to
100). It has high internal consistency ( D =.91; Flett et al., 2012), test-retest reliability (r=.76;
Mackinnon, Sherry, & Pratt, 2013), construct validity (Flett et al., 2012) convergent validity
(Flett et al., 1998), discriminant validity (Flett et al., 2012), and predictive validity (Flett et al.,
2012; Hill & Appleton, 2011).
The Valuing Questionnaire (VQ; Smout, Davies, Burns, & Christie, 2014; Appendix D),
a 10-item self-report measure, was used to evaluate further patients’ commitment to valuesconsistent action. Patients rated the extent to which each statement describes them on a 7-point
Likert scale (scores can range from 0 to 60). It has high internal consistency ( D =.79-.81) and
12 construct validity (Smout et al., 2014).
The Cognitive Fusion Questionnaire (CFQ; Gillanders et al., 2014; Appendix E), a 7-item self-report measure, was used to measure the degree to which patients get embroiled in their thoughts such that these thoughts dominate their actions. Patients rated the extent to which each statement describes them on a 7-point Likert scale (scores can range from 7 to 49). It has high internal consistency ( D =.88-.93), test-retest reliability (r=.81), construct, discriminant, and incremental validity (Gillanders et al., 2014).
The Counseling Center Assessment of Psychological Symptoms-34 (CCAPS-34; Locke et. al., 2012), a 34-item self-report measure, was used to evaluate patients’ level of psychopathology and symptom severity in the areas of depression, generalized anxiety, social anxiety, general distress, and academic distress. Patients rated the extent to which each statement described them on a 4-point Likert scale. It has been shown to be a reliable instrument for both diagnostic assessment and as a measure of treatment progress (Locke et al., 2012). It has high internal consistency ( D =.76-.892), test-retest reliability (r=.742-.866), construct, convergent, and discriminant validity (Locke et al., 2012).
Treatment Overview and Core Process Targets
The treatment program outlined below is arranged in the order in which the described interventions were typically introduced. While all five patients whose treatment is the subject of this paper received ACT-consistent treatment that approximated this guideline, the therapy was delivered flexibly and was not rigidly bound to a specific protocol. Consequently, the order in
which exercises were introduced (or whether they were introduced at all) was determined on a
13 case-by-case basis. ACT is intended to be delivered flexibly, with the therapist cognizant of what intervention seems most beneficial to the patient at any point in time (Hayes et al., 2012). Once a concept was introduced, it became available to be woven into future sessions when indicated. For practical purposes, exercises are listed once under their primary process target. ACT exercises generally are usable to address multiple, if not all, core processes.
ACT introduction and creative hopelessness. Most patients come to therapy with a change agenda. Their internal experiences are unpleasant, and they hope that therapy can help them learn to better control and change these experiences. Perfectionistic patients commonly state, “I just want to feel better,” or ask, “Can you teach me to stop worrying?” ACT treats this desire to cont rol one’s internal experiences as a fundamental contributor to the individual’s suffering (Hayes et al., 2012). As such, it is essential, from the outset of treatment, to help a patient see the unworkability of their efforts to try to control internal experiences, clarify the alternative way that ACT attempts to help them handle these experiences, and receive buy-in to begin treatment utilizing the ACT philosophy.
In this intervention, an ACT exercise called “creative hopelessness” was utilized to initiate this process. The aim of creative hopelessness is to help a patient recognize, from his own experience
, that the strategies he has been using in his life have been ineffective (Hayes et al.,
2012). This goal is accomplished first by helping the patient identify what he has been struggling with, focusing particularly on specific “bad” or “negative” internal experiences. The patient is then asked to identify: 1) what strategies he has been using to try to deal with these experiences;
2) how those strategies have worked; and 3) what is the cost of using those strategies. To illustrate, a common thought process of a perfectionistic student may be : “I sometimes have the
thought that the work I’m doing won’t be good enough or people will think it’s stupid. So, I
14 either spend a million hours working on the thing, making myself crazy, or, if I can, I just decide pretty much right from the beginning not to do it at all. Sometimes this helps me feel better, at least in the short-term. But there are a lot of problems. I spend so much time doing an assignment that I don’t have time for other stuff in my life, including other assignments! Or I feel guilty for not doing something that I know I should have d one.”
Often, the patient will recognize that while their control techniques may provide some short-term benefits, those benefits are outweighed by short- and long-term consequences. Once the patient appreciates the futility of his existing strategies, he is ready for an explicit introduction to ACT. Russ Harris’ (2009) “ ACT in a Nutshell ” exercise provides a way to accomplish this goal metaphorically. Metaphors are generally preferred over traditional didactics and dialogue in the ACT model because they encourage an experiential exploration of issues and are especially advantageous in making abstract concepts quickly accessible (Stoddard & Afari,
2014). The “ACT in a Nutshell” exercise features five sections.
First, a clipboard is utilized to represent a p atient’s internal struggles metaphorically
(alternatively, a large note card can be used and the patient’s previously identified difficult internal experiences can be written on it). The patient is told to hold the clipboard tightly, directly in front of his face, and asked wha t that experience is like. What’s his view of the room like? How much could he accomplish in this state? This part of the exercise helps the patient identify that, while he is focused on his negative experiences, it is difficult for him to connect to the world around him and do things that are important to him.
Second, with the therapist pushing on one side of the clipboard, the patient is asked to attempt to push the clipboard as far away from himself as possible and asked what that
experience is like. For example, how much energy does it take to do this? How much can he
15 accomplish in this state? Here, the patient can identify that his attempt to push away his negative experiences creates the same problems he experienced with the clipboard directly in front of his face.
In the creative hopelessness exercise, the therapist has already helped the patient identify how he becomes consumed by negative experiences (“holding the c lipboard tightly in front of his face) and strategies for fighting or avoiding these experiences (“pushing the clipboard away”).
These specific examples can be woven into “ ACT in a Nutshell ” to improve its salience for the patient.
Third, the patient is told to place the clipboard in his lap and asked what this experience is like. How well can he see and engage with the therapist and his environment? How capable is he of doing things that might be important to him?
Fourth, the therapist acknowledges that surely the patient would prefer not to have these difficult experiences on his lap and would much rather throw the clipboard into the other room.
The therapist then reviews with the patient all the ways the patient has tried to do just that and helps the patient identify that these strategies have been ineffective.
Fifth, the therapist details the alternative path that ACT suggests. The goal is to get the patient to accept or at least be open to the thought that the patient will learn how to handle these difficult internal experiences more effectively so that he can be free to engage in actions that are meaningful to him.
Cognitive defusion. The ACT model is built on the belief that “human suffering predominantly emerges from normal psychological processes, particularly those involving human language” (Hayes et al., 2012, p. 11). Humans have a unique ability to worry: to
continuously scan the environment for threat; to replay and analyze prior experiences; and to
16 make predictions about the future. Primitive humans used their ability to “think negatively” (i.e., to have negative thoughts about their situation) to survive with relatively limited resources in a world of stronger, faster animals. While an antelope presumably stops fearing a lion once it has reached safety, humans can continue to worry endlessly about that lion — and anything that the mind associates with the lion. Although this ability is undoubtedly helpful, it also can be deeply problematic. Since the human mind engages in a threat detection process, it is critical to psychological and behavioral functioning that we have a realistic perspective on that process.
“ Cognitive fusion ” refers to the tendency for humans to get caught up or entangled in their internal experiences such that they respond to these experiences literally, without proper regard for context (Hayes et al., 2012). For example, while giving a hypothetical presentation, a perfectionistic patient may have the thought, “These people think I’m stupid .
” A patient who cognitively fuses with that thought will treat the thought as factually true and respond accordingly.
“ Cognitive defusion ” refers to the ACT process of recognizing and accepting that thoughts are just thoughts, and not factual truths that demand a response. Developing the ability to defuse from thoughts enables a patient to take action consistent with his actual goals. One simple technique for defusion is just to add the phrase, “I’m having the thought that,” to any thought. For example, the patient would be asked to say, “I’m having the thought that these people think I’m stupid.” Ideally, this technique enables the patient to notice his thought as a thought and not as a factually true statement that must guide his behavior.
Various other cognitive defusion techniques were utilized in this treatment (see Harris,
2009 and Hayes et al., 2012 for numerous examples). Additionally, a frequently used daily
17 practice assignment , utilizing the “Getting Hooked” worksheet (Harris, 2009, p. 133), involved a patient noticing when her mind had “negative thoughts” and documenting whether she was
“hooked” (i.e., fused) by the thought or able to “unhook” (i.e., defuse) herself.
Experiential avoidance and acceptance. “ Experiential avoidance ” refers to any attempt to control, suppress, eliminate, or escape from unwanted internal experiences (Hayes et al.,
2012). Like cognitive fusion, ACT views experiential avoidance as an inherent component of human suffering. Taking nearly any patient through the creative hopelessness exercise described earlier is likely to reveal numerous forms of experiential avoidance taken in his life and its similarly numerous destructive effects. In ACT, a patient is asked to learn to accept his difficult internal experiences in the service of constructive, meaningful action. To be clear, acceptance does not
mean passively tolerating or resigning oneself to a situation. It does not mean desiring or liking a situation, nor does it mean judging a situation as right, fair, or just. Acceptance means voluntarily taking an “open, receptive, flexible, and nonjudgmental” attitude towards internal experiences (Hayes et al., 2012, p. 272). When a patient rejects the word ‘acceptance,’
‘willingness’ can be used in its place.
The goal is to enable the patient to be open to experiencing his thoughts, feelings, and bodily sensations, however unpleasant, in the service of taking action consistent with the person he wants to be. Both the creative hopelessness and “ ACT in a Nutshell ” exercises (described above) are utilized in part to introduce patients to the futility of experiential avoidance and to open them up to the idea of acceptance as an alternative path.
The “ Passengers on the Bus ” metaphor (Hayes, Strosahl, & Wilson, 1999), or the
“ Demons on a Boat ” variation (Harris, 2007), is used to help a patient overcome experiential avoidance. Further, this metaphor can act as a framework through which the entire ACT model
can be brought to bear on any situation that presents itself in treatment. In this metaphor, the
18 patient is asked to imagine that he is the driver of a bus. The bus has many passengers, which represent the pat ient’s internal experiences (i.e
., thoughts, feelings, bodily sensations, memories).
For example, suppose a perfectionistic patient is “driving” towards the completion of an important goal. The thought, “You’re going to fail!” is one of the pa ssengers. Whenever this passenger speaks up, he’s often joined by his friends: the feeling of fear and the bodily sensation of stomach pain. The patient does not
like it when these passengers speak up. They are very ugly, say horrible things to him, and look as though they could truly harm him. Consequently, when they do speak up, he does whatever he can do to get them to quiet down. Unfortunately, there is no way to get them off the bus, so the patient makes a deal with them: “Okay, I’ll stop working on th is goal if you hide in the back of the bus.” In this c ase, the patient has changed his behavior in hopes of avoiding his unpleasant internal experiences (note the link here between cognitive fusion and experiential avoidance). He is the driver of the bus in name only. His internal experiences are in control. Fortunately, the patient is shown that he has made a common and understandable, but problematic error in judgment. While the passengers on his bus seem like they can harm him in horrible ways, the only thing they can actually do is exist. Whether they harm him or not is his choice. If he can learn to tolerate them standing up and yelling at him, he can drive the bus wherever he wants.
Values-consistent action. In ACT, values have been defined as “state ments about what we want to be doing with our life: about what we want to stand for, and how we want to behave on an ongoing basis” (Harris, 2009, p. 189). They are freely chosen and constructed by the individual and are continually evolving (Hayes et al., 2012). Importantly, “values are not goals or ends in themselves, but can be thought of as principles for living that organize and direct current
action” (Lundgren, Luoma, Dahl, Strosahl, & Melin, 2012 , p. 518). It could be argued that the
19 whole point of ACT is to help a person construct a rich and meaningful, or values-consistent, life. Put another way, the skills of cognitive defusion and experiential acceptance are developed precisely to enable a person to take values-consistent action. Seen through the lens of the
“ Passengers on the Bus ” metaphor, our values serve as our compass, letting us know which direction to drive our “ bus.
”
Clarifying values is an important step in any ACT intervention. Two techniques were predominantly used in this treatment to help patients identify their values: 1) The “Values Bull’s
Eye ” (Dahl & Lundgren, 2006; Harris, 2009; Lundgren et al., 2012), and 2) the “ Imagine Your
80 th Birthday ” exercise (Harris, 2009).
The “ Values Bull ’s Eye ” exercise is a simple, one-page worksheet designed to help a patient identify his values in four key domains: 1) work/education, 2) relationships, 3) personal growth/health, and 4) leisure. The patient is asked to list his values under each domain. This part of the exercise typically requires some prompting on the part of the therapist and some brainstorming on the part of the patient (the “ Imagine Your 80 th Birthday ” exercise, described shortly, can be used to facilitate this process). On the bottom half of the page is a “dartboard” divided into the same four quadrants, with six concentric circles surrounding the bullseye. In each quadrant, the patient is asked to place an “X” on the circle of the dartboard that represents the degree to which he is living his life in accordance with his values (e.g., an X in the center of the dartboard represents living fully consistent with his values in that domain).
This exercise tends to be novel to perfectionists in three ways. First, perfectionists have spent much of their lives fused with the belief that perfection itself is of utmost value. Either its attainment has driven them, or its unattainability has overwhelmed them. The opportunity to
explore what really
matters to them, deep down, is an enlightening and inspiring experience.
20
Second, perfectionists have similarly spent most of their lives with one measuring stick:
“Was I perfect or not perfect? Was I the best or not the best?” The “Values Bull’s Eye” is, itself, a new measuring stick, introducing a new way to evaluate one’s performance: “Did I take a ctions today that are consistent with my values?”
Third, many perfectionists evaluate themselves and their performance based on a desire to win the approval of others. Historically, their behavior has revolved around other people’s values. The “Values Bull’s Eye” asks them to explore what really matters to them .
In the “ Imagine Your 80 th Birthday ” exercise, the patient is asked to indulge in the fantasy that, at 80-years-old, he has lived his own ideal life and that all the important people in this fantasy life, living or dead, are there to attend his birthday party. The patient is asked to imagine that someone (e.g., a friend, child, partner, or colleague) stands up to make a short speech, no more than a few sentences. The patient is told that the person talks about what the patient had stood for in his life, what the patient had meant to them, and the role that the patient had played in his life. The patient is asked to imagine the person saying whatever, deep down in his heart, he would most love to hear the person say. The patient is then told that another person wants to make a speech and then another. The exercise is then debriefed with the patient helped to consolidate what the “speeches” revealed about what the patient values.
Present-moment awareness and exposure. Since the goal of ACT is to enable a person to take values-consistent action in the present moment, an obvious skill that must be developed is the ability to be
in the here and now. In ACT, present-moment awareness, or mindfulness, is defined as “paying attention with flexibility, openness, and curiosity” (Harris, 2009, p. 8). In some ways, this ability to be “mindful” is foundational to all ACT’s core processes.
As such,
21 integrated into all ACT interventions is an attitude of openness and curiosity to present-moment processes.
Present-moment awareness exercises are introduced implicitly in the first session. To understand what brought the patient to treatment, the therapist gets the patient to describe a current situation that exemplifies her broader struggle. As the patient describes her issue, unpleasant internal experiences are generated, and she will likely attempt to stray from presentmoment experience as part of an experiential avoidance process. The therapist guides the patient back to her story, while periodically asking the patient to describe what she is thinking or how she is feeling as she tells it. These exercises serve a myriad of functions, including exposing the patient to her unpleasant internal experiences.
Exposure exercises are a frequent part of treatment, and patients are encouraged to practice them throughout the week between sessions. The previously mentioned “Getting
Hooked” worksheet was utilized to help facilitate this process. Additionally, the “Passengers on the Bus” metaphor was frequently utilized as a conduit to present -moment awareness processes.
For example, the therapist might ask the patient, “What passengers are showing up for you right now?”
Finally, other present-moment awareness exercises were utilized, including: “Take Ten
Breaths” (patient is instructed to take ten slow, deep breaths, while noticing the physical sensations of her body and attempting to let thoughts come and go without hooking her);
“Dropping Anchor” (patient is instructed to stand and push her feet into the floor, noticing the physical sensations of being anchored to the floor and other present-moment experiences); and
“Notice Five Things” (patient is instr ucted to see five things, hear five things, and feel five things) (Harris, 2009, p. 171).
22
Patients were given a handout describing these exercises. They are encouraged to try them daily, doing so at a convenient time of day at first and then at moments when they noticed themselves getting caught up in their thoughts and feelings.
Self-as-context. In ACT, “s elf-as-context ” refers to a “viewpoint from which we can observe thoughts and feelings… a place from which we can observe our experience without being ca ught up in it” (Harris, 2009, p. 173 ). It has been called the “transcendent sense of self, the observing self, noticing self, continuity of consciousness, pure consciousness, [and] pure a wareness” (Hayes et al., 2012, p. 85). It exists in contrast to “ self-as-concept, ” which is “all the beliefs, thoughts, ideas, facts, images, judgments, memories, and so on that form [one’s] selfconcept” (Harris, 2009, p. 174 ). A popular ACT metaphor describes a person’s observing self as being like the sky, and her thoughts and feelings as the continually changing weather (Harris,
2009). Patients presenting for treatment often exist almost exclusively in their conceptualized selves. That is, they believe themselves literally to be
their beliefs and thoughts. In this treat ment, the “ACT in a Nutshell” exercise, “Passengers on the Bus” metaphor, and various mindfulness exercises were utilized to help patients cultivate an awareness of their observing selves.
Self-compassion. Compassion involves noticing another person’s suff ering and having a deep desire to help that person. Most simply, self-compassion is compassion directed towards one’s self and has been operationalized as consisting of three primary components: 1) kindness,
2) a sense of common humanity, and 3) mindfulness (Neff, 2003). Self-compassion has been demonstrated to predict positive psychological health, to associate positively with measures of positive affect, personal initiative, and conscientiousness, and to associate negatively with measures of negative affect and neuroticism (Neff, Kirkpatrick, & Rude 2007). A recent meta-
analysis found “robust, replicable findings linking increased self -compassion to lower levels of
23 mental health symptoms,” including anxiety and depression (MacBeth & Gumley, 2012, p. 55 1).
While self-compassion is not an explicit part of the ACT model, theorists have suggested its consistency with the ACT model (Hayes, 2008; Neff & Tirch, 2013). It also has been explicitly integrated into ACT treatment guides (Forsyth & Eifert, 2016; Harris, 2009; Tirch, Silberstein, &
Schoendorff, 2014).
Perfectionists are often plagued by hostile, punishing thoughts (e.g., “You’re not good enough,” “They all thought you were stupid,” and “Nobody loves you”). Self -compassion exercises can provide a constructive context for engaging with and defusing from those thoughts and enabling values-consistent action.
In this treatment, specific self-compassion exercises were introduced when a patient was identified as needing a new approach for handling her punishing thoughts. A primary exercise involves asking the patient to try to remember the first time she experienced the painful thought that is currently troubling her, and then bringing out the patient’s compassion for that younger version of herself. For exa mple, a perfectionist may be able to identify first telling herself “I need to perform perfectly or nobody will care about me” upon returning home from a sporting event at age 10. This patient is asked to imagine her 10-year-old self as vividly as she can, and then to bring that 10-year-old into the room in front of her. If done well, this exercise helps the patient easily connect with the compassion they feel for that little girl, and, consequently, herself. The patient can then be guided in how best to help that little girl, in an ACT-consistent manner (i.e., acknowledging the little girl’s feelings and providing her with unconditional acceptance and love). An extension of this exercise can be to then ask the patient to visualize a much older, 60year-old version of herself and to imagine that 60-year-old meeting her present-day self. The
patient is typically able to identify that her older self would have the same compassion for her
24 present-day self as she does for her 10-year-old self.
Another exercise utilized in this treatment involves asking the patient to imagine that a friend was having the same struggle that he was having and how he would treat his friend in that situation (Neff, 2016). The patient is helped in identifying strategies that would be most useful to help a friend who was having this experience, and then enabled to put those strategies to good use on himself.
Results and Case Descriptions
Data were collected successfully from all five participants at the time of their first and final visits to the counseling center for participation in this study (see Tables 1 and 2). For every instrument used, a higher score is reflective of maladaptive functioning (i.e., lower scores are more desirable). The study ’s hypotheses that participants would see reductions in perfectionism, perfectionistic thoughts, and symptoms of mental illness, and that participants would see improvements in measures of psychological flexibility were supported. These gains were analyzed by averaging the data from all five participants and conducting paired sample t-tests
(see Table 3). Significant gains ( p
< .05) were found on nearly all measures with concurrent strong effect sizes (Cohen’ s d > .80). Linear regressions revealed that baseline scores on the
SAPS did not predict pre- to post-test changes in perfectionistic thoughts (PCI), psychological flexibility (AAQ-II), or psychological symptoms (CCAPS). A first order correlation revealed no correlation ( r
= .115, p
= .853
) between patients’ pre - to post-test changes in perfectionistic thoughts (PCI) and their changes in psychological flexibility (AAQ-II).
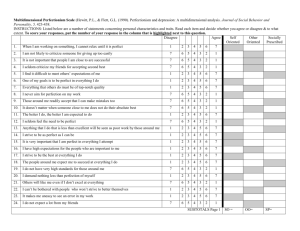
Table 1
25
Pre and Post Data for Psychological Flexibility and Perfectionism Measures
Measure Daniel Sara Chloe Margaret Tamara
Pre Post Pre Post Pre Post Pre Post Pre Post
AAQ-II
SAPS
PCI
31 29 25 13 40 31 27 23 28 19
43 42 45 40 40 33 52 47 42 45
67 43 83 60 49 31 66 56 74 60
VQ 37 31 13 12 45 24 23 15 29 19
CFQ 36 35 26 21 45 36 35 29 37 30
Note. AAQ-II=Acceptance and Action Questionnaire, 2 nd edition; SAPS=The Short Form of the
Revised Almost Perfect Scale; PCI=Perfectionism Cognitions Inventory; VQ=Valuing
Questionnaire; CFQ=The Cognitive Fusion Questionnaire.
Table 2
Pre and Post Data for Counseling Center Assessment of Psychological Symptoms (CCAPS-34)
Measure Daniel Sara Chloe Margaret Tamara
Pre Post Pre Post Pre Post Pre Post Pre Post
Distress Index 43 22 41 17 88 39 31 12 67 45
Depression 58 21 42 21 68 42 42 16 63 58
Generalized Anxiety 41 35 41 20 73 41 35 15 86 52
Social Anxiety 62 48 92 68 95 55 68 35 55 42
Academic Distress 66 44 37 37 89 30 23 23 44 30
Table 3
Pre and Post Data for Group Means
Measure
AAQ-II
SAPS
PCI
VQ
Pre Post p Cohen ’s d
30.2 23.0 .017 1.76
44.4 41.4 .169 0.75
67.8 60.0 .003 3.00
29.4 20.2 .050 1.24
CFQ 35.8 30.2 .013 1.89
Distress Index 54.0 27.0 .008 2.17
Depression 54.6 31.6 .012 1.98
Generalized Anxiety 55.2 32.6 .011 2.01
Social Anxiety 74.4 49.6 .009 2.11
Academic Distress 51.8 32.8 .155 0.78
The Case of Daniel
Daniel (names and identifying details have been changed to preserve anonymity) was a
20-year-old African American male in his 2 nd year of undergraduate education. He was single with married parents and an older brother who lived thirty minutes away. Daniel reported
26 persistent anxiety regarding his ability to perform up to his high academic standards and his ability to navigate social situations. He described an “always racing” mind occupied with selfcriticism and self-doubt about prior and future actions. Daniel traced this anxiety back to lifelong pressure to perform from his demanding father coupled with insecurity about how he compared to his extremely high-achieving older brother. Already pursuing treatment for his anxiety at the university’s counseling center , Daniel was given the recruitment flyer for this study (Appendix
F). He agreed that he would be a good fit and began this treatment for perfectionism.
As Daniel was already a patient in the counseling center, the first session was dedicated to cultivating an understanding of how this treatment would be different from the work he had been doing previously. To this end, the therapist utilized the “ ACT in a Nutshell ” exercise.
Daniel identified his most frequent and distressing thoughts: “I’m not good enough.” “As a black man, I have to be perfect in order to succeed.” “I should have done better.” “What’s the p oint,
I’ll never be good enough.” These thoughts provided insight into the roots of Daniel’s perfectionism. Fro m a very early age, Daniel’s father consistently conveyed the message that, as an African American, Daniel would always be at a disadvantage and that to succeed would mean he would have to achieve at a much higher level than his Caucasian peers. While Daniel believed there was some truth to this message, he felt it had placed too great a burden on him. He explained that he normally handled these burdensome thoughts in various ways, including: ruminating on the thoughts; debating with himself; artificially lowering his standards by deciding
27 that the chal lenging situation didn’t matter; and avoiding challenging situations in various other ways. During a “ Creative Hopelessness ” exercise, Daniel recognized that while his coping techniques often provided short-term stress relief, they ultimately were ineffective. The stress always returned, and he was failing to achieve at a level he knew he could. For example, his 3.25
GPA was below his capabilities, and he was not participating in those activities he knew were essential to his succeeding in his field of study.
In the second session, the “ Demons on a Boat ” metaphor was introduced. Daniel was asked to begin tracking times between therapy sessions when he noticed himself getting “ caught up ” in his difficult i nternal experiences (“demons”) and to notice how that experience effected the choices he made (“the path of the boat”). Because his perfectionistic anxiety manifested in all areas of his life, Daniel was asked to pay particular attention to just one life domain. Daniel chose his academics and identified what values-consistent action in that domain would be for the upcoming week.
In the third session, Daniel reported that the “Demons on a Boat” metaphor had been extremely helpful in enabling him to see how his difficult internal experiences effect his behavior. Though he had made dramatic improvement in recognizing his stress in the moment,
Daniel continued to struggle to take values-consistent action. For example, Daniel stated that in the week prior he had not adequately prepared for a quiz. Daniel identified that his reaction to the thoughts (“Demons”) that arrived when he began to study for the quiz ("This class doesn't matter" and "This book is a waste of time") was to stop studying. This behavior helped him temporarily feel less anxious and avoid the "Demons" that were even deeper down and scarier
("You're going to fail" and "You're not going to achieve anything"). However, on reflection,
Daniel recognized that fusing with these thoughts (i.e., taking them literally and allowing them to
guide his behavior) ultimately contributed to him feeling worse and led to a disappointing
28 performance on the quiz. Daniel’s difficulty was normalized with psychoeducation regarding the sympathetic nervous system’s fight -flight response. He was taught how this is a historically adaptive response that evolved in humans to help us respond to threats such as encountering a lion on the savanna. However, unlike a lion encounter, these internal experiences were not deadly, were not even technically “real,” and could not be dealt with effectively in the same way one would avoid a lion.
Throughout the next few sessions, Daniel was asked to mark his difficult internal experiences in session. Through these exposure exercises he began to make progress in defusing from his negative thoughts and began to recognize that they were not “real” in the same way that a lion is real. Concurrently, his ability to take values-consistent action while having these difficult thoughts improved.
Part of each of the fourth through ninth sessions was dedicated to identifying an anxietyprovoking values-consistent action for Daniel to perform between sessions and then functionally analyzing the experience of undertaking that action. The “Values Bull’ s E ye” and “Imagine Your
80 th Birthday” exercises were utilized to aid Daniel in identifying personally meaningful values in four key life domains.
Daniel was a passionate musician whose music was meaningful to him. He struggled to play creatively although he knew it was essential for his growth as a musician. During the fourth and fifth weeks of treatment, he made playing creatively a nightly goal . Daniel’s tracking sheet evidenced the same anxiety and negative selftalk each night (e.g., “This isn’t very good,” “You aren’t clever,” and “This is a waste of time”). However, he committed t o playing nearly every night and reported being very pleased with himself following his playing. He was progressively
more capable of “losing himself” in his music.
29
In the sixth week of treatment, Daniel reported anxiety about participating in a voluntary campus-wide art competition, where the task at hand involved creating a performance that would be displayed to an audience and judged on its merit. With the submission deadline approaching,
Daniel would have ideally started this project much earlier, but he was paralyzed by various perfectionistic thoughts (e.g., “N obody is going to like what you do, ” “Your ideas aren’t good enough, ” and “These competitions are stupid”).
In the sixth and seventh weeks of treatment, Daniel was encouraged to practice defusing from those thoughts and let his values “drive his boat” (i.
e., guide his behaviors) rather than his goals (i.e., creating a masterpiece and winning the competition). Ultimately, Daniel completed his project. He reported that, although his participation was anxiety-provoking and he did not win the competition, he was proud of the work he had done, had learned a lot by doing so, and had found the experience “more fulfilling than anything I’ve done in a while.”
In the final weeks of treatment, Daniel’s goals range d across domains. These included studying for exams and participating in social activities with classmates.
In Daniel’s 10 th and final session, he reported pleasure in his newfound ability to take values-consistent action despite difficult internal experiences. He stated satisfaction with the progress he had made. An agreement was reached that it was time to end treatment.
The Case of Sara
Sara was a 23-year-old Caucasian female in the second year of undergraduate education.
Born in the United States, but having lived abroad with her parents and siblings for most of her life, Sara had recently returned to the U.S. to commence her secondary education. She was happily married and had an infant daughter.
30
Early in her intake session, Sara reported uncertainty about committing to treatment and great discomfort talking to people, including the therapist, about herself. However, having seen the recruitment flyer (Appendix F), she recognized herself in its description of a perfectionist and was hopeful for some help. Sara successfully maintained a 4.0 GPA, but she was experiencing growing anxiety about her ability to be both a “perfect student and a perfect mom.” In describing the balancing act dictated by her very busy life, she stated, “if I let down a smidge, I will fail.”
On exploration, Sara revealed that failing meant having to abandon her academic pursuits. She dreamt of a life that included a successful career and a family with children.
However, Sara had been raised in a culture in which women predominantly worked as homemakers and caretakers. Although her own parents and husband were uniformly supportive of her professional aspirations, Sara had developed a core belief that her desire to “have it all” was a near-impossible dream and that she would have to be “perfect” to achieve it.
Consequently, any indication that she was falling short of her high standards was a warning sign to Sara that she was at risk of losing her dream. Signs that she was falling short included all internal experiences of stress, which Sara interpreted as weakness and found intolerable. Sara had no outlet for these concerns, as she never acknowledged her insecurities to others. Fearing that her loved ones would interpret her insecurities as weakness and attempt to persuade her to give up on her academic pursuits, she kept these concerns to herself. Consequently, she often felt misunderstood by her friends and loved ones. Having never complained or evidenced her struggles, people seemed to believe that everything came easily to her. On the contrary, Sara was an extremely diligent worker. Sara increasingly found it difficult to avoid or contain her anxiety, which led to her apprehensively entering treatment.
Though Sara had presented for treatment voluntarily, she was extremely hesitant to
engage in and commit to treatment. In the second session, to help Sara reconcile her
31 ambivalence, a creative hopelessness exercise was used in which she was asked to: 1) explore the various methods she had historically utilized to cope with her anxiety and 2) evaluate how well those methods were working. In addition to providing clear motivation for treatment, this exercise opened the door to a discussion about Sara’s willingness to discuss the difficult internal experiences that were challenging for her. At the outset of the third session, Sara declared a willingness to commit to continuing treatment, but she stated that she did not want to talk about difficult or unpleasant thoughts and feelings. Sara’s desire to avoid her distress was normalized with psychoeducation about the sympathetic nervous system’s fight -flight response, which was presented as a historically adaptive response that evolved in humans to help us respond to threats such as a lion encounter on the savanna. The therapist explained to Sara that unlike a lion confrontation , these internal experiences were not deadly, were not even technically “real,” and could not be responded to effectively in the same way one would a lion. Expanding on some of the work she had done earlier, she worked through each of these statements to determine their accuracy. Sara agreed that they were accurate and for the first time began to defuse from her unpleasant internal experiences. The lion-in-the-savanna analogy helped Sara more willingly look at and talk about her perfectionistic thoughts and feelings, and she seemed ready for an insession exposure exercise. Sara was asked to identify a current thought that made her anxious
(“I’ll have to choose between being a mom and being a professional”) and the whole-body experience of having that thought. After some time noticing the discomfort that the thought engendered, Sara was asked to compare the thought to an actual, real-life lion walking into the room. Encouraging Sara not to dispel or contradict her thought, she was asked simply to keep the thought while also recognizing how different it was from a real-life lion. Using a classic defusion
32 exercise, Sara was asked to say, “
I’m having the thought that
I’ll have to choose between being a mom and being a professional” and to notice the difference. Following the exercise, Sara reported that she found the exercise very interesting. She was encouraged to try to notice her anxious thoughts between sessions, and, if she could, to try to defuse from the thought rather than try to suppress it or escape it. These in- and between-session anxiety exposure exercises continued to be utilized in the ensuing weeks of treatment and helped Sara begin to learn how to mindfully notice and cognitively defuse from her distressing thoughts.
In the fourth and fifth sessions, values identification work (i.e., the “Values Bull’s Eye”) was utilized to help Sara clarify what was important to her. Sara highly valued being a loving mother, wife, sibling, and friend. Additionally, she valued being intellectually stimulated, having a career that made a difference in the world by helping people, and being someone that younger women would look up to. Sara was impressed by the realization that it was not actually that important or meaningful to her to do any of these things perfectly and that there was no
“mountain to climb” to achieve being the person she wanted to be. She could be the person she wanted to be (i.e., a person living in a way that was consistent with her values) at any moment.
In a particularly potent exercise, Sara was asked to imagine two possible lives. In both lives she was living in a values-consistent way in the domains of relationships, personal growth/health, and leisure. However, in one life she had no career and in the other she did. Sara stated that she would not be happy or fulfilled with a life without a career. Referring to her current life as a student and a future life as a professional in her field, Sara stated, "I love it, want to do it, enjoy it, and am passionate about it." Clarifying how important, satisfying, and achievable a life with a career was to Sara, helped her begin to believe that achieving that life was not as precarious or impossible as she had long believed. Sara began to realize that, even
though she would often fall short of being “perfect” and that these times may be emotionally
33 difficult for her, she could still fulfill her dreams.
In the fifth and sixth sessions, the “Passengers on the Bus” me taphor was introduced and utilized to help provide a conceptualization of Sara’s relationship with her challenging thoughts
("passengers") and her values-based vision for her future (where she's driving her "bus"). Sara identified frequent thoughts that pertained to her fear of losing her career (e.g., "You'll give up if you have too much fun," "If you express your fears or vulnerabilities to other people, they will push you off your path," and "Be extremely careful, this could fall apart easily") and ways in which these thoughts affected her behaviors (e.g., not having fun, not being open with people in her life, and a broad sense of insecurity/fragility). Sara practiced applying this metaphor in and between sessions. She began to cultivate an ability to notice distressing internal experiences in the moment, acknowledge them for what they were, identify her values and supports (which included her work ethic, resilience, persistence, strong support network of family and friends, and strong anchoring in her religious faith), and then make a conscious decision to take valuesconsistent action.
In the seventh and final session, Sara reported experiencing “confidence and relief.” She stated a newfound awareness of being in control of her life. She acknowledged that she used to
“push bad thoughts a way” and “feel bad for having certain thoughts,” but that she had become more comfortable with these internal experiences and felt confident in her “strength and ability to face them.”
The Case of Chloe
Chloe was a 21-year-old African American female in the 4 th year of undergraduate education. Chloe was single, with separated parents and a younger brother who lived two hours
away. She had been in treatment with different therapists for several years with complaints of
34 depression and anxiety, but she had experienced limited progress on these issues. Having seen the recruitment flyer (Appendix F), Chloe, with the agreement of her former provider, elected to enter this treatment for perfectionism.
As Chloe was already a patient in the counseling center, the first and second sessions were dedicated to cultivating an understanding of how this treatment would be different from her previous therapy. This explanation was achieved by utilizing the “ACT in a N utshell ” exercise.
Chloe identified her most frequent and distressing thoughts: “I’m not good enough,” “I’m afraid
I might fail,” “I’m going to fail,” “I should just give up.” She then clarified that she normally handles these thoughts in various ways, including: distracting herself with video games and the website YouTube; not participating in something if she thinks she might do poorly; and
“endlessly” ruminating on how she should have done or should do something. As part of a
“ Creative Hopelessness ” exercise, Chloe recognized that while her coping techniques often provided short-term stress relief, they ultimately were ineffective. The stress always returned, and she was failing to achieve at a level she knew she could attain. For example, her 3.45 GPA was beneath her capabilities and her frequent procrastination and avoidance contributed to a feeling that s he was “meandering through life.”
In the third and fourth sessions , Chloe’s extreme avoidance of internal experiences emblematic of her perfectionistic anxiety was targeted by in-session exposure exercises. She frequently attempted to change the topic of conversation — often speaking very rapidly and tangentially — any time her internal anxiety was triggered. Chloe was gently interrupted, guided to see this behavior as an avoidance technique, and encouraged to experience her “ anxiety ” without trying to change it. Her difficulty in this task was validated and normalized with
education on how the brain has evolved to be the ultima te “don’t get killed machine,” (Harris,
35
2009, p. 101) using the example of early humans having to respond to extreme threats like a lion on the savanna. Chloe was helped to realize that while her thoughts were indeed distressing, they were not deadly, were not even technically “real,” an d could not be dealt with effectively in the same way one would a lion. Various defusion exercises were employed to help Chloe cultivate an ability to disengage from her thoughts . The “Demons on a Boat” metaphor was introduced to help Chloe begin to concep tualize how her sometimes painful internal experiences (“demons”) altered her behaviors (“the path of her boat”). Chloe was asked to begin tracking times during her day when she felt particularly consumed by her distressing thoughts. She was instructed to note what triggered these thoughts and how they ultimately affected her behavior.
Part of each of the fifth through eleventh sessions was dedicated to identifying an anxiety-provoking, values-consistent action for Chloe to take between sessions and then, at a later session, functionally analyzing her experience of undertaking that action. The “Values
Bull’s Eye” exercise was utilized in helping Chloe identify her values in four central domains of living. Her short-term goals included completing her academic assignments with enough time to do high quality work and attending a resume-building workshop and job fair. Over time, she developed the skill of noticing her negative self-talk in the moment and choosing to commit to a valuesconsistent action. Reflecting on the work she had done on a term paper, she stated, “I started procrastinating and believing the ‘You’ll get it done eventually’ demon, but I knew that the quality of the paper would suffer, or that I might not even get it done. I was down for a minute, but I didn’t give up. I kept doing it , and it came out well.” As Chloe’s mindfulness and defusion skills improved, she noticed that she seemed to lack time management skills, perhaps due to a life spent avoiding challenges through procrastination. Happily, she found the use of a
scheduler on her phone and a proactive approach to planning her week very helpful.
In the eighth session, selfcompassion was emphasized, as Chloe’s self -talk was particularly hostile and formidable. Chloe’s self -identified trait of being a compassionate and supportive person to her friends and family members was utilized in an exercise where Chloe
36 was asked to embody that value in how she treated herself. Practicing self-compassion in an
ACT-consistent way (i.e., not using it to debate her negative self-talk) required an exploration of how Chloe thought she was most effective at helping her friends and family members when they were feeling negatively about themselves. Chloe identified that she seemed to be most helpful when she didn’t try to invalidate other people’s thoughts about themselves, but instead listened to them and provided a needed hug or supportive statements.
In the twelfth and final session, Chloe reported being in good spirits, proud of the work she had done in treatment which had contributed to her anticipated accomplishment of graduating with honors. She noted that she was “the sailor of my boat,” and that she was hopeful in her ability to “not let my ‘ demons ’ ste er it anymore.”
The Case of Margaret
Margaret was a 22-year-old Caucasian female in the fourth year of undergraduate education. She had a “fairly serious” relationship with a boyfriend of two years, and her married parents and older brother lived in a town about thirty minutes away. She reported excessive worry about meeting her extremely high performance standards (particularly in her academics) and frequent self-criticism regarding her performance despite its objectively high quality (i.e.,
3.95 GPA). Margaret stated that she had “ always been this way, ” reporting an early-life desire to please her demanding parents and compete with her similarly high-achieving brother. Although she no longer felt pressure from her parents or brother, she reported that she was continuing to
37 put that same pressure on herself. Margaret decided to seek treatment after seeing the recruitment flyer (Appendix F) and reflecting on escalating feedback from her boyfriend and peers that she was too hard on herself.
In the first session, Margaret complained of increased difficulty making time for anything but her studies, which had a particularly troubling effect on her relationship with her boyfriend.
Margaret found it difficult to spend time or even talk on the phone with her boyfriend without becoming overwhelmed by thoughts that the time should be spent on school work. She had the same difficulty when spending time with her friends. Additionally, Margaret reported having discontinued making time to exercise regularly throughout the week and was troubled that she had gained “about twenty pounds” in the past year . She attributed her weight gain both to a lack of exercise and to an unwillingness to spend time cooking (an activity for which she has skill and passion). Margaret revealed that she kept a detailed daily schedule (which she filled up with plans to do school work as a way of coping with her anxiety) and that she was extremely rigid in adhering to this schedule. This pattern contributed to her inability to make time for activities outside of her school work. Beyond her concern about the way she utilized her time, Margaret also reported that she was losing her enjoyment of her schoolwork although she was passionate about her field of study and was excelling. She reported periodic escape fantasies of quitting school.
In the second session, Margaret was introduced to ACT using the “ ACT in a Nutshell ” metaphor. This exercise was personalized for Margaret in various ways, including having her keep a list of her most common distressing thoughts (e.g., “You’re not good enough,” “I’m going to fail,” and “Why would you have fun?”), and having her provide examples of the various strategies she had historically used to cope with those thoughts (e.g., agreeing with them, making
choices based on them, and excessively ruminating on them). Margaret’s responses to her anxiety were normalized with education about the brain having evolved to be the ultimate
“don’t -get-killed machine, ” using the example of early humans having to respond constantly to extreme threats like an encounter with a lion on the savanna. In so doing, Margaret came to
38 realize that although her thoughts were indeed distressing, they were not deadly and were not even technically “real,” and could not be dealt with in the same way one would a lion encounter.
Margaret was asked to begin tracking times during her day when she felt particularly consumed by her distressing thoughts and to note what triggered these thoughts and how they ultimately affected her behavior.
In the third session, Margaret was introduced to the “ Passengers on the Bus ” metaphor and to the concept of values-guided action. Margaret was aided in identifying personally meaningful values with the “Imagine Your 80 th Birthday” exercise. For the next few sessions,
Margaret was asked each week to identify a measurable, non-academic, values-consistent goal for that week (e.g., go to the gym three times and talk to your boyfriend on the phone every night for at least two minutes), and to track her internal experiences in the context of pursuing those goals and the outcome of her endeavors. These experiences were then reviewed in session with the therapist modeling an attitude of non-judgment and curiosity, and utilizing an approach that valued looking at the function of different decisions as opposed to whether they were ‘right’ or
‘wrong.’
This process proved extremely useful for Margaret, and her growth in only a few weeks was remarkable. Initially, the exercise enabled her to conceptualize accurately the power she gave to her distressing thoughts (e.g., allowing her negative thoughts to guide the decisions she made). Margaret acknowledged that she had never been so aware of her thoughts and how she
39 would “let them take over.” As Margaret refined her ability to notice her internal experiences in the present moment, she began practicing various techniques to defuse from them. Among numerous defusion techniques, t hese included: calling the distressing thoughts “Tiger Margaret” and identifying the distressing thoughts as “ passengers ” who, while sometimes valuable, did not get final say in the actions she took. More and more, Margaret found herself able to take valuesconsistent action regardless of her internal experiences.
In the sixth session, Margaret and the therapist noted that while Margaret’s ability to take values-consistent action was vastly improving, her treatment-related homework consistently revealed some very punishing self-talk centered around the thought that she was “not good enough.
” As part of a self-compassion exercise, Margaret traced this thought back through time, and she recalled an early memory of herself having this thought as a 9-year-old. Margaret was then guided through an exercise in which she was asked to visualize that 9-year-old girl, bring her into the room, and offer that little girl what she needed. Margaret believed that little girl needed a hug and to be told that “she was loved no matter what.” Margaret was then as ked to visualize herself as a 55-year-old, sitting in the room where Margaret was currently sitting and to bring present day Margaret into the room with her. She was asked to imagine what 55-year-old
Margaret would want to offer her present-day self. Margaret identified the same message: a hug and “you’re good enough/loved no matter what.” While Margaret found this exercise emotionally draining, she reported later being able to use it to bring self-compassion into difficult moments.
In the eighth and final session, Margaret reported that she was now frequently utilizing the skills she had developed in treatment to positive effect. This resulted in her ability to engage in and be present for a spontaneous weekend trip with her boyfriend, regular exercise, engage in
activities with her roommates, and make time to watch a television show that she enjoyed.
Margaret noted that she had been able to prioritize many non-academic activities and had still
40 performed up to her standards in her academics. Margaret pointed out that “Tiger Margaret” had told her many times throughout these weeks that she would not be able to do that.
The Case of Tamara
Tamara was a 21-year-old Asian female in the fourth year of undergraduate education.
She was single, an international student, and her married parents and older brother lived in her country of origin. Tamara reported achievement-oriented anxiety accompanied by frequent performance-related self-criticism, primarily revolving around her academics. She held this belief despite a 3.91 GPA and a recent award from the university as the most accomplished member within her academic department of her soon-to-be-graduating class. Tamara was concerned with the techniques she had been using to cope with her anxiety (e.g., over-preparing, rigidly keeping to an extreme study schedule at the cost of social engagement, periodic use of alcohol and marijuana). When she saw the recruitment flyer (Appendix F), she decided to enter treatment.
Tamara’s first and second sessions were spent exploring the nature and history of her perfectionistic anxiety. She reported pressure for her entire life from her parents to perform at a high level in all things, particularly academics. Additionally, at age 8, she began to participate in competitive soccer (Tamara was presently on a full-scholarship for soccer at this university) and remembers similarly high pressure from her coaches. Tamara identified that she had received the following messages as a child: “ People expect you to be perfect; ” “People won’t be prou d of you unless you’re the best;” and “People won’t care about you unless you’re the best.” Over time,
Tamara had adopted these beliefs herself:
I expect to be perfect.
I
am not proud of myself unless
I’m the best.
In the third session, Tamara was guided through the “ Values Bull’s Eye” exercise with
41 the goal of helping her identify personally meaningful values in four key life domains. Tamara reported finding the exercise novel and enlightening. She stated it was helpful to clearly articulate what was important to her. She found it interesting that achieving perfection academically or athletically was not actually meaningful to her. Rather, she described doing challenging work, doing work that she believed in, doing work that helped people, taking care of herself physically, challenging herself physically, and being a good colleague and teammate as fulfilling and meaningful.
In the fourth session, Tamara acknowledged that she seemed to have difficulty staying with her internal experiences in the present moment, particularly when feeling anxious. She reported that this was one of the reasons she rigidly kept to a busy schedule: to avoid or escape these anxious moments. On reflection, Tamara acknowledged that this strategy had not been working for her. Her response to her anxiety was normalized, and she was taught some simple grounding exercises (e.g., take ten slow breaths and notice five things) to help her begin to experience bringing her whole self into the present moment. Tamara was encouraged to practice these exercises regularly throughout the week and later reported finding them very helpful coping skills in times of stress. As an additional tool to help Tamara talk about and work with her difficult thoughts and their effect on her life, the “ Passengers on the Bus ” metaphor was introduced. For practice between sessions, Tamara was asked to begin tracking times during her day when she felt particularly consumed by her distressing thoughts, to note what triggered these thoughts, and to report how the thoughts ultimately affected her behavior.
In the fifth and sixth sessions, in reviewing the work that Tamara was doing between
42 sessions, Tamara realized that, although she was frequently very critical of herself, her behaviors were predominantly values-consistent. In areas where she was not quite living her values,
Tamara noticed that she was often limited by the constraints of her environment (e.g., sometimes as a student you must do work that is not particularly meaningful as part of her degree requirements and sometimes the work she did as a student was not intellectually challenging for her). Utilizing the “ Passengers on the Bus ” metaphor, Tamara was asked to identify if there were any short-term changes she would like to make in the direction her life. Tamara reported a new awareness that she was, in fact, living the life that she desired.
In the sixth session, Tamara acknowledged that she was plagued by self-punishing thoughts of not being good enough. To help address these concerns, she was led through a selfcompassion exercise in which she was asked to visualize her 8-year-old self, bring that little girl into the room, and attempt to provide for that girl whatever it is that Tamara thought she needed and wanted. Tamara identified wanting to tell her 8-year-old self that she was good enough and worthy of love just the way she was. Tamara recognized that she deserved the same compassion as that little girl. She later described the exercise as a powerful tool for helping her “be nicer to myself.
”
In the seventh and final session, Tamara took stock of the gains she had made in treatment. She reported an increased ability to pause in distressing moments, take a step back, notice her thoughts and other internal experiences, acquire some perspective on what she could control, and ensure that her actions were consistent with the person she wanted to be. Tamara remarked that at times she could recognize that “I’m actually a pretty outstanding bus driver.”
General Discussion
The five case studies reveal five important points about the utilization of ACT for the
treatment of perfectionism. First, while symptom reduction is explicitly not the primary goal of
43
ACT therapy, patients reported significant reductions with large effect sizes from pre- to posttreatment in depression ( p = .012, Cohen’s d = 1.98) , general anxiety ( p = .011, Cohen’s d =
2.01), social anxiety ( p
= .009, Cohen’s d = 2.11) , and general distress ( p
= .008, Cohen’s d =
2.17).
Second, while patients did not report a significant change in their perfectionism (SAPS; p
= .169, Cohen’s d = .75), they evidenced a dramatic reduction in t he frequency and awareness of thoughts related to perfectionism (PCI; p = .003, Cohen’s d = 3.00). Notably, this shift occurred in the context of a treatment that encouraged patients to try to be more
aware of their perfectionistic thoughts, albeit with a much different attitude towards those thoughts. This result provides further support for the belief that attempting to control or eliminate unwanted internal experiences may be counterproductive, and that the ACT approach of taking a willing attitude towards these unwanted internal experiences produces a reduction in their saliency.
Third, the intervention produced significant quantitative and qualitative shifts in multiple targeted change processes. Patients reported significant improvements in psychological flexibility (AAQ-II; p
= .017, Cohen’s d = 1.76), cognitive fusion (CFQ; p
= .013, Cohen’s d =
1.89), and commitment to values-consistent action (VQ; p
= .050, Cohen’s d = 1.24). A review of the qualitative data evidences three key components of the treatment (i.e., change mechanisms) consistent across all five patients: reductions in experiential avoidance, increases in the ability to disentangle from unwanted thoughts, and clarification of personal values.
Daniel learned to defuse from the belief, “I’ll never be good enough,” and identified the values of expressing himself through his music and having a strong work ethic. He transitioned from avoiding challenging activities and artificially lowering his personal standards to regularly
writing, playing, and enjoying his own music for the first time in “years,” reengaging in his studies, and participating in a campus-wide art competition.
44
Sara defused from the beliefs, “I am barely hanging on” and “I can’t talk to anyone about my true feelings,” and identified the value s of being a kind, patient, and authentic person in her relationships and doing work that was intellectually stimulating and helped people. She transitioned from avoiding acknowledging or talking about her feelings to anyone, not making time for her relationship with her sister and friends, and finding it difficult to enjoy her time with her child, to beginning to disclose her anxieties to her husband and sister, making time for activities with her loved ones, and experiencing a renewed freedom to enjoy her studies and her home life.
Chloe began to defuse from the beliefs, “I am going to fail” and “I should just give up,” and identified the value of doing work that moved her in the direction of having a career she was passionate about. She transitioned from using videogames and YouTube to avoid challenging activities in her final semester, to attending a job fair, turning in her work on time, and graduating with honors.
Margaret defused from the beliefs, “You’re going to fail” and “You should have done better,” and identified the values of being a thoughtful and caring partner to her boyfriend and taking care of her physical health. She transitioned from avoiding activities that triggered her unwanted anxious thoughts (e.g., spending time with her boyfriend or at the gym) and finding her schoolwork progressively less enjoyable, to experiencing a renewed intimacy with her boyfriend, regularly exercising, and experiencing a renewed satisfaction with her academic endeavors.
Tamara defused from the belief, “I have to be perfect to be loved,” and identified the
values of doing challenging work that helps people and being genuine in her relationships. She
45 transitioned from finding no satisfaction in a life filled with worry and fear to experiencing herself as purposeful and accomplished.
Notably, of the various techniques used in this intervention to help patients achieve these gains , all patients reported finding the “Passengers on the Bus” exercise (or the “Demons on a
Boat” variation) as particularly meaningful both in understanding themselves and in their ability to utilize functionally the new skills they had learned. Additionally, the patients with whom selfcompassion exercises were utilized (Chloe, Margaret, and Tamara), each reported the saliency of these exercises in enabling their ability to contact, defuse from, and accept their unwanted internal experiences.
Fourth, baseline scores on a broad measure of perfectionism (SAPS) did not predict pre- to post-test changes in perfectionistic thoughts (PCI), psychological flexibility (AAQ-II), or psychological symptoms (CCAPS). While this finding is limited by the low variability in the participants’ baseline SAPS scores, it suggests that the ACT intervention utilized in therapy is effective regardless of the severity of a patient’s perfectionism.
Additionally, no correlation ( r =
.115, p
= .853) was found between patients’ pre - to post-test changes in perfectionistic thoughts
(PCI) and their changes in psychological flexibility (AAQ-II). This suggests that the ACT intervention has a broad effect on patients, one that is not tied to the frequency of patients’ automatic thoughts about the need to be perfect and their cognitive awareness of imperfections.
Fifth, the effectiveness of the treatment provides initial support for treating perfectionism in a relatively diverse population (i.e., multiple genders, sexual orientations, races, ethnicities, nationalities, and religious backgrounds were included in the sample) with a flexibly delivered
(i.e., no rigid adherence to a session-by-session protocol), short-term (i.e., treatment was
delivered in seven, seven, eight, ten, and twelve sessions), transdiagnostic (i.e., patients were
46 included with comorbid diagnoses of generalized anxiety disorder and major depressive disorder) ACT intervention.
Limitations
A study of this nature has inevitable limitations. The sample featured only five students of similar age from the same university, which might affect the generalizability of these results.
Without a comparison or control group, the author could not assess for the influence of confounding variables or control for certain threats to internal validity (e.g., regression to the mean and measurement effects). Additionally, we cannot be sure how the intervention compares to an alternative intervention or to no intervention at all. Also, the intervention was delivered by just one practitioner using a flexible approach in a real-life setting without adherence to a rigid protocol. Although mechanisms of change and intervention techniques have been well-described, replicability may be an issue. Future research could address this in one of two ways. First, one could create a manualized treatment administered by multiple therapists. Second, one could recognize the value in implementing ACT flexibly, further delineate the mechanisms of change and intervention techniques, and study whether adhering to these guidelines (without rigidly adhering to a session-by-session protocol) is effective regardless of the individual differences in therapists and patients.
Conclusion
The obtained results provide preliminary support for the effectiveness of ACT as a treatment for perfectionism. Further, the study provides evidence for three primary mechanisms of change: reductions in experiential avoidance, increases in the ability to disentangle from unwanted thoughts, and clarification of personal values. Finally, the study adds to the body of
evidence indicating that treating perfectionism directly and explicitly can provide remittance of
47 symptoms of other mental health issues.
References
Aldea, M. A., Rice, K. G., Gormley, B., & Rojas, A. (2010). Telling perfectionists about their
48 perfectionism: Effects of providing feedback on emotional reactivity and psychological symptoms.
Behaviour Research and Therapy
,
48,
1194-1203. doi:10.1016/j.brat.2010.09.003
Alden, L. E., Ryder, A. G., & Mellings, T. B. (2002). Perfectionism in the context of social fears:
Toward a two-component model. In G. L. Flett, P. L. Hewitt (Eds.),
Perfectionism:
Theory, research, and treatment (pp. 373-391). Washington, DC, US: American
Psychological Association. doi:10.1037/10458-015
American Psychiatric Association (APA). (2013). Diagnostic and statistical manual of mental disorders,
(5 th ed.). Arlington, VA: American Psychiatric Association.
Antony, M. M., Purdon, C. L., Huta, V., & Swinson, R. P. (1998). Dimensions of perfectionism across the anxiety disorders.
Behaviour Research & Therapy
,
36
(12), 1143-1154.
Arch, J., Eifert, G. H., Davies, C., Plumb Vilardaga, J. P., Rose, R. D., & Craske, M. G. (2012).
Randomized clinical trial of cognitive behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for mixed anxiety disorders.
Journal of Consulting and
Clinical Psychology
,
80
(5), 750 – 765.
Arpin-Cribbie, C. A., Irvine, J., Ritvo, P., Cribbie, R. A., Flett, G. L., & Hewitt, P.L. (2008).
Perfectionism and psychological distress: A modeling approach to understanding their therapeutic relationship.
Journal of Rational-Emotive & Cognitive-Behavior Therapy
,
26
(3), 151-167.
Bardone-Cone, A. M., Wonderlich, S. A., Frost, R. O., Bulik, C. M., Mitchell, J. E., Uppala, S.,
& Simonich, H. (2007). Perfectionism and eating disorders: Current status and future
directions.
Clinical Psychology Review
,
27
(3), 384-405.
Beck, A. T. (1976).
Cognitive therapy and the emotional disorders
. New York, NY:
International Universities Press.
Bieling, P. J., Israeli, A. L., & Antony, M. M. (2004). Is perfectionism good, bad, or both?
49
Examining models of the perfectionism construct. Personality & Individual Differences ,
36
(6), 1373. doi:10.1016/S0191-8869(03)00235-6
Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., Orcutt, H. K., & ... Zettle,
R. D. (2011). Preliminary psychometric properties of the acceptance and action questionnaire – II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy , 42, 676-688. doi:10.1016/j.beth.2011.03.007
Brustein, M. (2014).
Perfectionism: A guide for mental health professionals
. New York, NY:
Springer Publishing Company.
Burns, D. D. (1980, November). The perfectionist’s script for self -defeat.
Psychology Today,
34-
52.
Burns, J. L., Lee, R. M., & Brown, L. J. (2011). The effect of meditation on self-reported measures of stress, anxiety, depression, and perfectionism in a college population.
Journal of College Student Psychotherapy
,
25
(2), 132-144.
Chang, E. C., Watkins, A., & Banks, K. H. (2004). How adaptive and maladaptive perfectionism relate to positive and negative psychological functioning: Testing a stress-mediation model in black and white female college students.
Journal of Counseling Psychology
,
51
(1), 93-102.
Cox, B. J., Enns, M. W., & Clara, I. P. (2002). The multidimensional structure of perfectionism in clinically distressed and college student samples.
Psychological Assessment, 14
(3),
50
365 – 373.
Crosby, J. M., Armstrong, A. B., Nafziger, M. A., & Twohig, M. (2013). Using acceptance and commitment therapy (ACT) to treat perfectionism in college students. In J. Pistorello
(Ed.),
Mindfulness and acceptance for counseling college students: Theory and practical applications for intervention, prevention, and outreach (pp. 139-158) . Oakland, CA: New
Harbinger Publications, Inc.
Crosby, J. M., Bates, S. C., & Twohig, M. P. (2011). Examination of the relationship between perfectionism and religiosity as mediated by psychological inflexibility. Current
Psychology: A Journal for Diverse Perspectives on Diverse Psychological Issues
,
30
(2),
117-129. doi:10.1007/s12144-011-9104-3
Dahl, J., & Lundgren, T. (2006).
Living beyond your pain: Using acceptance and commitment therapy to ease chronic pain
. Oakland, CA: New Harbinger Publications, Inc.
DiBartolo, P. M., Frost, R. O., Dixon, A., & Almodovar, S. (2001). Can cognitive restructuring reduce the disruption associated with perfectionistic concerns?
Behavior Therapy
,
32,
167-184. doi:10.1016/S0005-7894(01)80051-4
Dunkley, D. M., Zuroff, D. C., & Blankstein, K. R. (2003). Self-critical perfectionism and daily affect: Dispositional and situational influences on stress and coping.
Journal of
Personality and Social Psychology
,
84
, 234 – 252.
Egan, S. J., Hattaway, M., & Kane, R. T. (2014). The relationship between perfectionism and rumination in post traumatic stress disorder.
Behavioural and Cognitive Psychotherapy
,
42
(2), 211-223. doi:10.1017/S1352465812001129
Egan, S. J., & Hine, P. (2008). Cognitive behavioural treatment of perfectionism: A single case experimental design series.
Behaviour Change
,
25
(4), 245-258.
doi:10.1375/bech.25.4.245
Egan, S. J., Wade, T. D., & Shafran, R. (2011). Perfectionism as a transdiagnostic process: A
51 clinical review. Clinical Psychology Review , 31 , 203-212. doi:10.1016/j.cpr.2010.04.009
Egan, S. J., Wade, T. D., & Shafran, R. (2012). The transdiagnostic process of perfectionism.
Revista De Psicopatologia Y Psicologia Clinica , 17 (3), 279-294.
Enns, M. W., Cox, B. J., & Borger, S. C. (2001). Research report: Correlates of analogue and clinical depression: a further test of the phenomenological continuity hypothesis.
Journal of Affective Disorders , 66, 175-183. doi:10.1016/S0165-0327(00)00305-0
Ferguson, K. L., & Rodway, M. R. (1994). Cognitive behavioral treatment of perfectionism:
Initial evaluation studies. Research on Social Work Practice , 4 (3), 283-308.
Fledderus, M., Oude Voshaar, M. H., ten Klooster, P. M., & Bohlmeijer, E. T. (2012). Further evaluation of the psychometric properties of the acceptance and action questionnaire-II.
Psychological Assessment
,
24
(4), 925-936.
Flett, G. L., & Hewitt, P. L. (2015). Measures of perfectionism. In G. J. Boyle, D. H. Saklofske,
G. Matthews, (Eds.), Measures of personality and social psychological constructs (pp.
595-618). San Diego, CA, US: Elsevier Academic Press. doi:10.1016/B978-0-12-
386915-9.00021-8
Flett, G. L., Hewitt, P. L., Blankstein, K. R., & Gray, L. (1998). Psychological distress and the frequency of perfectionistic thinking.
Journal of Personality and Social Psychology
,
75
(5), 1363-1381. doi:10.1037/0022-3514.75.5.1363
Flett, G., Hewitt, P., Demerjian, A., Sturman, E., Sherry, S., & Cheng, W. (2012). Perfectionistic automatic thoughts and psychological distress in adolescents: An analysis of the perfectionism cognitions inventory.
Journal of Rational-Emotive & Cognitive-Behavior
52
Therapy
,
30
(2), 91. doi:10.1007/s10942-011-0131-7
Forman, E. M., Herbert, J. D., Moitra, E., Yeomans, P. D., & Geller, P. A. (2007). A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression.
Behavior Modification
,
31
(6), 772 – 799.
Forsyth, J. P., & Eifert, G. H. (2016). The mindfulness & acceptance workbook for anxiety: A guide to breaking free from anxiety, phobias, and worry using acceptance and commitment therapy
, (2 nd ed.). Oakland, CA: New Harbinger Publications.
Frost, R. O. & DiBartolo, P. M. (2002). Perfectionism, anxiety, and obsessive-compulsive disorder. In G. L. Flett, P. L. Hewitt, (Eds.),
Perfectionism: Theory, research, and treatment (pp. 341-371). Washington, DC, US: American Psychological Association. doi:10.1037/10458-003
Frost, R. O., Heimberg, R. G., Holt, C. S., Mattia, J. I., & Neubauer, A. L. (1993). A comparison of two measures of perfectionism.
Personality and Individual Differences
,
14
(1), 119-
126. doi:10.1016/0191-8869(93)90181-2
Frost, R. O., Marten, P., Lahart, C., & Rosenblate, R. (1990). The dimensions of perfectionism.
Cognitive Therapy and Research
,
14
(5), 449-468.
Frost, R. O., Novara, C., & Rhéaume, J. (2002). Perfectionism in obsessive-compulsive disorder.
In R.O. Frost & G. Steketee (Eds.),
Cognitive approaches to obsessions and compulsions
,
(pp. 91-105). NY, USA: Pergamon. doi:10.1016/B978-008043410-0/50007-6
Frost, R. O., & Steketee, G. (1997). Perfectionism in obsessive-compulsive disorder patients.
Behaviour Research and Therapy
,
35
(4), 291-296. doi:10.1016/S0005-7967(96)00108-8
Gentes, E. L., & Ruscio, A. M. (2014). Perceptions of functioning in worry and generalized anxiety disorder.
Cognitive Therapy and Research, 38,
518-529.
53
Gillanders, D. T., Bolderston, H., Bond, F. W., Dempster, M., Flaxman, P. E., Campbell, L., …
Remington, R. (2014) The development and initial validation of the cognitive fusion questionnaire. Behavior Therapy, 45 , 83-101. doi: 10.1016/j.beth.2013.09.001
Glover, D. S., Brown, G. P., Fairburn, C. G., & Shafran, R. (2007). A preliminary evaluation of cognitive-behaviour therapy for clinical perfectionism: a case series. The British Journal of Clinical Psychology
,
46
(1), 85-94.
Greenspon, T. S. (2000). ‘Healthy perfectionism’ is an oxymoron!: Reflections on the psychology of perfectionism and the sociology of science. Journal of Secondary Gifted
Education, 11
(4), 197-208.
Greenspon, T. S. (2008). Making sense of error: A view of the origins and treatment of perfectionism.
American Journal of Psychotherapy
,
62
(3), 263-282.
Habke, A. M., & Flynn, C. A. (2002). Interpersonal aspects of trait perfectionism. In G. L. Flett
& P. L. Hewitt (Eds.),
Perfectionism: Theory, research, and treatment
(pp. 151-180).
Washington, DC: American Psychological Association. doi:10.1037/10458-006
Habke, A. M., Hewitt, P. L., & Flett, G. L. (1999). Perfectionism and sexual satisfaction in intimate relationships.
Journal of Psychopathology and Behavioral Assessment, 21
(4),
307-322. Doi:10.1023/A:1022168715349
Hamachek, D. E. (1978). Psychodynamics of normal and neurotic perfectionism.
Psychology: A
Journal of Human Behavior
,
15
(1), 27-33.
Handley, A. K., Egan, S. J., Kane, R. T., & Rees, C. S. (2015). A randomised controlled trial of group cognitive behavioural therapy for perfectionism.
Behaviour Research and Therapy
,
68,
37-47. doi:10.1016/j.brat.2015.02.006
Harris, R. (2009).
ACT made simple: An easy-to-read primer on acceptance and commitment
54 therapy.
Oakland, CA: New Harbinger Publications.
Hayes, S. C. (2008, November).
The Roots of Compassion
. Keynote address presented at the
Association for Behavioral and Cognitive Therapies 42 nd Annual Convention, Orlando,
FL.
Hayes, S. C., Strosahl, K., & Wilson, K. G. (1999). Acceptance and commitment therapy: An experiential approach to behavior change
. New York, NY: Guilford Press.
Hayes, S. C., Strosahl, K., & Wilson, K. G. (2012).
Acceptance and commitment therapy: The process and practice of mindful change , (2 nd ed.). New York, NY: Guilford Press.
Hayward, L., & Arthur, N. (1998). Perfectionism and post-secondary students.
Canadian Journal of Counselling, 323 , 187 – 199.
Hewitt, P. L., & Flett, G. L. (1991a). Dimensions of perfectionism in unipolar depression.
Journal of Abnormal Psychology
,
100
(1), 98-101. doi:10.1037/0021-843X.100.1.98
Hewitt, P. L., & Flett, G. L. (1991b). Perfectionism in the self and social contexts:
Conceptualization, assessment, and association with psychopathology.
Journal of
Personality and Social Psychology , 60 (3), 456-470.
Hewitt, P. L., Flett, G. L., & Mikail, S. F. (2017).
Perfectionism: A relational approach to conceptualization, assessment, and treatment
. New York, NY, US: Guilford Press.
Hewitt, P. L., Flett, G. L., Sherry, S. B., & Caelian, C. (2006). Trait perfectionism dimensions and suicidal behavior. In T. E. Ellis (Ed.),
Cognition and suicide: Theory, research, and therapy
(pp. 215-235). Washington, DC: American Psychological Association. doi:10.1037/11377-010
Hewitt, P. L., Mikail, S. F., Flett, G. L., Tasca, G. A., Flynn, C. A., Deng, X., & ... Chen, C.
(2015). Psychodynamic/interpersonal group psychotherapy for perfectionism: Evaluating
the effectiveness of a short-term treatment.
Psychotherapy
,
52
(2), 205-217. doi:10.1037/pst0000016
Hill, A. P., & Appleton, P. R. (2011). The predictive ability of the frequency of perfectionistic cognitions, self-oriented perfectionism, and socially prescribed perfectionism in relation to symptoms of burnout in youth rugby players. Journal of
Sports Sciences
,
29
(7), 695-703.
Hill, R. W., Huelsman, T. J., Furr, R. M., Kibler, J., Vicente, B. B., & Kennedy, C. (2004). A new measure of perfectionism: The perfectionism inventory. Journal of Personality
Assessment
,
82
(1), 80-91.
55
Hirsch, C. R., & Hayward, P. (1998). The perfect patient: Cognitive-behavioural therapy for perfectionism.
Behavioural and Cognitive Psychotherapy
,
26
(4), 359-364.
Horney, K. (1950).
Neurosis and human growth; the struggle toward self-realization
. Oxford,
England: W. W. Norton.
Huprich, S. K., Porcerelli, J., Keaschuk, R., Binienda, J., & Engle, B. (2008). Depressive personality disorder, dysthymia, and their relationship to perfectionism. Depression and
Anxiety
,
25
(3), 207-217. doi:10.1002/da.20290
Kearns, H., Forbes, A., & Gardiner, M. (2007). A cognitive behavioural coaching intervention for the treatment of perfectionism and self-handicapping in a nonclinical population.
Behaviour Change
,
24
(3), 157-172. doi:10.1375/bech.24.3.157
Lloyd, S., Schmidt, U., Khondoker, M., & Tchanturia, K. (2015). Can psychological interventions reduce perfectionism? A systematic review and meta-analysis.
Behavioral and Cognitive Psychotherapy, 43
(6), 705-731. doi:10.1017/S1352465814000162
Locke, B. D., McAleavey, A. A., Zhao, Y., Lei, P., Hayes, J.A., Cast onguay, L. G., & … Lin, Y.
(2012) Development and initial validation of the counseling center assessment of psychological symptoms-34.
Measurement and Evaluation in Counseling and
Development, 45 (3), 151-169.
Lundgren, T., Luoma, J. B., Dahl , J., Strosahl, K., & Melin, L. (2012). The bull’s -eye values
56 survey: A psychometric evaluation. Cognitive and Behavioral Practice, 19 (4), 518-526.
Luoma, J. B., Kohlenberg, B. S., Hayes, S. C., & Fletcher, L. (2012). Slow and steady wins the race: A randomized clinical trial of acceptance and commitment therapy targeting shame in substance use disorders. Journal of Consulting and Clinical Psychology , 80 (1), 43 – 53.
MacBeth, A., & Gumley, A. (2012). Exploring compassion: A meta-analysis of the association between self-compassion and psychopathology. Clinical Psychology Review, 32 , 545-
552. doi:10.1016/j.cpr.2012.06.003
Mackinnon, S. P., Sherry, S. B., & Pratt, M. W. (2013). The relationship between perfectionism, agency, and communion: A longitudinal mixed methods analysis.
Journal of Research in
Personality
,
47,
263-271. doi:10.1016/j.jrp.2013.02.007
Matte, M., & Lafontaine, M. (2012). Assessment of romantic perfectionism: Psychometric properties of the Romantic Relationship Perfectionism Scale.
Measurement and
Evaluation in Counseling and Development, 45
(2), 113-132. doi:10.1177/0748175611429303
Missildine, W. H. (1963).
Your inner child of the past
. New York, NY: Simon and Schuster.
Molnar, D. S., Sirois, F. M., & Methot-Jones, T. (2016). Trying to be perfect in an imperfect world: Examining the role of perfectionism in the context of chronic illness. In F. M.
Sirois & D. S. Molnar, (Eds.),
Perfectionism, health, and well-being
. (pp. 69-99) Cham,
Switzerland: Springer International Publishing. doi:10.1009/978-3-319-18582-8
57
Moroz, M., & Dunkley, D. M. (2015). Self-critical perfectionism and depressive symptoms: Low self-esteem and experiential avoidance as mediators.
Personality and Individual
Differences, 87 , 174-179. doi:10.1016/j.paid.2015.07.044
Neff, K. (2016, July 15).
Self-compassion guided meditations and exercises
. Retrieved from http://self-compassion.org/category/exercises/#exercises
Neff, K., & Tirch, D. (2013). Self-compassion and ACT. In T. B. Kashdan & J. Ciarrochi (Eds.),
Mindfulness, acceptance, and positive psychology: The seven foundations of well-being
(pp. 78-106). Oakland, CA, US: Context Press/New Harbinger Publications.
Neff, K. D. (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2 , 85-102.
Neff, K. D., Kirkpatrick, K. L., & Rude, S. S. (2007). Self-compassion and adaptive psychological functioning.
Journal of Research in Personality, 41
, 139-154. doi:10.1016/j.jrp.2006.03.004
O’Connor, R. C. (2007). The relations between perfectionism and suicidality: A systematic review. Suicide and Life-Threatening Behavior, 37 (6), 698-714. doi:10.1521/suli.2007.37.6.698
Pearson, A. N., Heffner, M., & Follette, V. M. (2010).
Acceptance and commitment therapy for body image dissatisfaction: A practitioner's guide to using mindfulness, acceptance, and values-based behavior change strategies.
Oakland, CA: New Harbinger Publications,
Inc.
Pleva, J., & Wade, T. D. (2007). Guided self-help versus pure self-help for perfectionism: A randomised controlled trial.
Behaviour Research and Therapy
,
45,
849-861. doi:10.1016/j.brat.2006.08.009
Radhu, N., Daskalakis, Z. J., Arpin-Cribbie, C. A., Irvine, J., & Ritvo, P. (2012). Evaluating a
58 web-based cognitive-behavioral therapy for maladaptive perfectionism in university students. Journal of American College Health , 60 (5), 357-366. doi:10.1080/07448481.2011.630703
Rice, K. G., Ashby, J. S., & Slaney, R. B. (1998). Self-esteem as a mediator between perfectionism and depression: A structural equations analysis.
Journal of Counseling
Psychology
,
45
(3), 304-314. doi:10.1037/0022-0167.45.3.304
Rice, K. G., Neimeyer, G. J., & Taylor, J. M. (2011). Efficacy of coherence therapy in the treatment of procrastination and perfectionism.
Counseling Outcome, Research, and
Evaluation , 2 (2), 126.
Rice, K. G., Richardson, C. E., & Tueller, S. (2014). The short form of the revised almost perfect scale.
Journal of Personality Assessment
,
96
(3), 368-379. doi:10.1080/00223891.2013.838172
Richards, P. S., Owen, L., & Stein, S. (1993). A religiously oriented group counseling intervention for self-defeating perfectionism: A pilot study. Counseling and Values ,
37
(2), 96-104.
Riley, C., Lee, M., Cooper, Z., Fairburn, C. G., & Shafran, R. (2007). A randomised controlled trial of cognitive-behaviour therapy for clinical perfectionism: a preliminary study.
Behaviour Research and Therapy
,
45
(9), 2221-2231.
Saboonchi, F., Lundh, L., & Öst, L. (1999). Perfectionism and self-consciousness in social phobia and panic disorder with agoraphobia.
Behaviour Research and Therapy
,
37,
799-
808. doi:10.1016/S0005-7967(98)00183-1
Sandoz, E., Wilson, K., & DuFrene, T. (2011).
Acceptance and commitment therapy for eating
59 disorders: a process-focused guide to treating anorexia and bulimia
. Oakland, CA: New
Harbinger Publications.
Santanello, A. W., & Gardner, F. L. (2007). The role of experiential avoidance in the relationship between maladaptive perfectionism and worry.
Cognitive Therapy and Research
,
31
(3),
319-332. doi:10.1007/s10608-006-9000-6
Sassaroli, S., Romero Lauro, L. J., Maria Ruggiero, G., Mauri, M. C., Vinai, P., & Frost, R.
(2008). Perfectionism in depression, obsessive-compulsive disorder and eating disorders.
Behaviour Research and Therapy , 46 (6), 757-765. doi:10.1016/j.brat.2008.02.007
Shafran, R., Lee, M., & Fairburn, C. G. (2004). Clinical perfectionism: A case report.
Behavioural and Cognitive Psychotherapy , 32 (3), 353-357.
Slade, P. D., & Owens, R. G. (1998). A dual process model of perfectionism based on reinforcement theory.
Behavior Modification
,
22
(3), 372-390. doi:10.1177/01454455980223010
Slaney, R. B., Rice, K. G., Mobley, M., Trippi, J., & Ashby, J. S. (2001). The revised almost perfect scale. Measurement and Evaluation in Counseling and Development , 34 (3), 130-
145.
Smout, M., Davies, M., Burns, N., & Christie, A. (2014). Development of the valuing questionnaire (VQ).
Journal of Contextual Behavioral Science, 3
(3), 164 – 172. doi:10.1016/j.jcbs.2014.06.001
Smout, M. F., Hayes, L., Atkins, P. B., Klausen, J., & Duguid, J. E. (2012). The empirically supported status of acceptance and commitment therapy: An update.
Clinical
Psychologist, 16
(3), 97-109. doi:10.1111/j.1742-9552.2012.00051.x
Steele, A. L., & Wade, T. D. (2008). A randomised trial investigating guided self-help to reduce
60 perfectionism and its impact on bulimia nervosa: A pilot study.
Behaviour Research and
Therapy
,
46
(12), 1316-1323. doi:10.1016/j.brat.2008.09.006
Steele, A. L., Waite, S., Egan, S. J., Finnigan, J., Handley, A., & Wade, T. D. (2013). Psycho- education and group cognitive-behavioural therapy for clinical perfectionism: A caseseries evaluation. Behavioural and Cognitive Psychotherapy , 41 (2), 129-143. doi:10.1017/S1352465812000628
Stoddard, J. A., & Afari, N. (2014).
The big book of ACT metaphors: A practitioner’s guide to experiential exercises and metaphors in acceptance and commitment therapy.
Oakland,
CA: New Harbinger Publications.
Stoeber, J., & Otto, K. (2006). Positive conceptions of perfectionism: Approaches, evidence, challenges.
Personality and Social Psychology Review, 10,
295-319.
Stumpf, H., & Parker, W. D. (2000). A hierarchical structural analysis of perfectionism and its relation to other personality characteristics.
Personality and Individual Differences
,
28
,
837-852. doi:10.1016/S0191-8869(99)00141-5
Strosahl, K., & Robinson, P. J. (2008). The mindfulness and acceptance workbook for depression: Using acceptance and commitment therapy to move through depression and create a life worth living
. Oakland, CA: New Harbinger.
Terry-Short, L. A., Glynn Owens, R., Slade, P. D., & Dewey, M. E. (1995). Positive and negative perfectionism.
Personality and Individual Differences
,
18
(5), 663-668. doi:10.1016/0191-8869(94)00192-U
Tirch, D. D., Silberstein, L. R., & Schoendorff, B. (2014).
The ACT practitioner’s guide to the science of compassion: Tools for fostering psychological flexibility.
Oakland, CA: New
Harbinger Publications.
Twohig, M. P., Hayes, S. C., Plumb, J. C., Pruitt, L. D., Collins, A. B., Hazlett-Stevens, H., &
61
Woidneck, M. R. (2010). A randomized clinical trial of acceptance and commitment therapy vs. progressive relaxation training for obsessive compulsive disorder. Journal of
Consulting and Clinical Psychology
,
78
, 705 – 716.
Weineland, S., Arvidsson, D., Kakoulidis, T. P., & Dahl, J. (2012). Acceptance and commitment therapy for bariatric surgery patients, a pilot RCT.
Obesity Research & Clinical Practice
,
6
(1), e21 – e30.
Wetherell, J. L., Afari, N., Rutledge, T., Sorrell, J. T., Stoddard, J. A., Petkus, A. J., . . .
Atkinson, J. H. (2011). A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain , 152 , 2098 – 2107.
White, R. G., Gumley, A. I., McTaggart, J., Rattrie, L., McConville, D., Cleare, S., & Mitchell,
G. (2011). A feasibility study of acceptance and commitment therapy for emotional dysfunction following psychosis.
Behaviour Research and Therapy
,
49
, 901 – 907.
Wimberley, T., Mintz, L., & Suh, H. (2016). Perfectionism and mindfulness: Effectiveness of a bibliotherapy intervention. Mindfulness , 7 (2), 433-444. doi:10.1007/s12671-015-0460-1
Appendix A
Acceptance and Action Questionnaire-II
Instructions
Below you will find a list of statements. Please rate how true each statement is for you by circling a number next to it. Use the scale below to make your choice.
1 2 3 4 5 6 never
true very seldom true seldom true sometimes true frequently true almost always true
62
7 always true
1.
My painful experiences and memories make it difficult for me to live a life that I would value.
2.
I’m afraid of my feelings.
1 2 3 4 5 6 7
1 2 3 4 5 6 7
3.
I worry about not being able to control my worries and feelings.
4.
My painful memories prevent me from having a fulfilling life.
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
5.
Emotions cause problems in my life.
6.
It seems like most people are handling their lives better than I am.
7.
Worries get in the way of my success.
Appendix B
Short Form of the Revised Almost Perfect Scale
Instructions
The following items are designed to measure certain attitudes people have toward themselves, their performance, and toward others. It is important that your answers be true and accurate for you. In the space next to the statement, please enter a number from 1 ( strongly
63 disagree ) to 7 ( strongly agree ) to describe your degree of agreement with each item.
1 2 3 4 5 6 7
Strongly Slightly Slightly
Disagree Disagree Disagree Neutral
Strongly
Agree Agree Agree
______ I have high expectations for myself.
______ Doing my best never seems to be enough.
______ I set very high standards for myself.
______ I often feel disappointment after completing a task because I know I could have done
better.
______ I have a strong need to strive for excellence.
______ My performance rarely measures up to my standards.
______ I expect the best from myself.
______ I am hardly ever satisfied with my performance.
64
Appendix C
Perfectionism Cognitions Inventory
Instructions
Listed below are a variety of thoughts that pop into people’s heads. Please read each thought and indicate how frequently, if at all, the thought has occurred to you over the last week
. Please read each item carefully and circle the appropriate number.
1 2 3 4 5
1. Why can’t I be perfect ?
Not at Sometimes Moderately Often All the all time
1 2 3 4 5
2. I need to do better 1 2
3. I should be perfect 1 2
4. I should never make the same mistake 1 2 twice
5. I’ve got to keep working on my goals 1 2
3 4 5
3 4 5
3 4 5
6. I have to be the best
7. I should be doing more
8. I can’t stand to make mistakes
1
1
1
2
2
2
3 4 5
3 4 5
3 4 5
3 4 5
3 4 5
3 4 5
9. I have to work hard all the time 1 2
10. No matter how much I do, it’s never 1 2 enough
11. People expect me to be perfect
12. I must be efficient at all times
1 2
1 2
13. My goals are very high 1 2
14. I can always do better, even if things 1 2
3 4 5
3 4 5
3 4 5
3 4 5 are almost perfect
15. I expect to be perfect
16. Why can’t things be perfect?
1 2
1 2
17. My work has to be superior 1 2
18. It would be great if everything in my 1 2 life were perfect
19. My work should be flawless
20. Things are seldom ideal
21. How well am I doing?
22. I can’t do this perfectly
23. I certainly have high standards
24. Maybe I should lower my goals
25. I’m too much of a perfectionist
1
1
1
1
1
1
1
2
2
2
2
2
2
2
3 4 5
3 4 5
3 4 5
3 4 5
3 4 5
3 4 5
3 4 5
3 4 5
3 4 5
3 4 5
3 4 5
65
Appendix D
Valuing Questionnaire
Please read each statement carefully and then circle the number which best describes how much the statement was true for you DURING THE PAST WEEK, INCLUDING TODAY.
1 2 3 4 5
Not at all True
1.
I spent a lot of time thinking about the past or future, rather than being engaged in activities that mattered to me
2.
I was basically on “auto-pilot” most of the time
6 7
Completely
True
1 2 3 4 5 6 7
1 2 3 4 5 6 7
3.
I worked toward my goals even if I didn’t feel motivated to
4.
I was proud about how I lived my life
5.
I made progress in the areas of my life I care most about
6.
Difficult thoughts, feelings or memories got in the way of what I really wanted to do
7.
I continued to get better at being the kind of person I want to be
8.
When things didn’t go according to plan, I gave up easily
9.
I felt like I had a purpose in life
10.
It seemed like I was just ‘going through the motions’, rather than focusing on what was important to me
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
66
1 2
Appendix E
Cognitive Fusion Questionnaire
3 4 5 6 7 never
true very seldom true seldom true sometimes true frequently true
1.
My thoughts cause me distress or emotional pain
2.
I get so caught up in my thoughts that I am unable to do the things that I most want to do almost always true always true
1 2 3 4 5 6 7
1 2 3 4 5 6 7
3.
I over-analyse situations to the point where it’s unhelpful to me 1 2 3 4 5 6 7
4.
I struggle with my thoughts 1 2 3 4 5 6 7
5.
I get upset with myself for having certain thoughts
6.
I tend to get very entangled in my thoughts
7.
It’s such a struggle to let go of upsetting thoughts even when I know that letting go would be helpful
1 2 3 4 5 6 7
1 2 3 4 5 6 7
1 2 3 4 5 6 7
67
Appendix F
Study Recruitment Flyer (Note: University’s identifying information has been removed)