rustypipesyndrome
advertisement

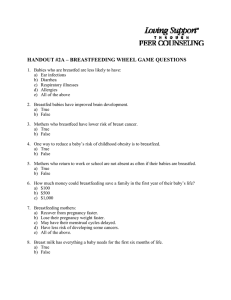
Case studies MMA Faridi Pooja Dewan Prerna Batra Rusty pipe syndrome: counselling a key intervention ABSTRACT Presence of blood in the breastmilk renders a rusty or brownish colour to it; this entity is known as 'rusty pipe syndrome'. Although this is a self-limiting condition, it can be particularly intimidating for mothers and may act as a psychological barrier to successful breastfeeding. We describe this entity in two mothers who had spontaneous blood-stained breastmilk from both breasts in the early post-partum period and were worried about feeding their infants. Subsequent to proper counselling with the use of skills like active listening, accepting their concerns, building confidence by providing relevant information in simple language and by giving suggestions and avoiding commands, both mothers were able to successfully breastfeed their offspring. Keywords: breastfeeding, blood, breastmilk, counselling, rusty pipe syndrome Breastfeeding Review 20^3•, 21(3): 27-30 INTRODUCTION 'Rusty pipe syndrome' is a condition wherein the breastmilk produced during early lactation appears dark brown in colour due to the presence of blood (Virdi, Goraya & Khadwal 2001). It is usually a benign condition and usually resolves in 2-5 days (Merlob 1990). We describe two mothers who presented with rusty pipe syndrome between March 2012 and May 2012, along with a review of literature and management of this condition by proper counselling, enabling mothers to successfully breastfeed. Case 1 A 28-year-old, second grávida woman delivered a full-term (38 weeks' gestation) healthy female baby weighing 2800 g in Guru Tegh Bahadur Hospital, a tertiary care hospital in Delhi. Within an hour of birth, the baby was handed over to the mother who was advised by the staff nurse to initiate breastfeeding. But the mother expressed her breastmilk before putting the baby to the breast and found that it was brownish-red in colour (Figures la and b). She did not breastfeed her baby and informed the staff nurse. A trained lactation consultant evaluated her. Detailed history revealed that her firstborn infant was admitted in the NICU soon after birth and when she was asked to express breastmilk for Breastfeeding Review • VOLUME 21 • NUMBER 3 • NOVEMBER 2013 her baby it was brown-red coloured which persisted for about 10 days. She consulted a surgeon and underwent mammography and other relevant investigations for breast malignancy but the results were normal. However, she opted not to breastfeed her first offspring who was formula fed. The previous history of rusty coloured breastmilk prompted her to express the milk before breastfeeding her second baby. On examination, breasts were soft, the local temperature was not raised and the nipples were protractile and healthy with no cracks or ulcers. She denied any history of breast pain, breast lumps, any other abnormal nipple discharge, trauma to her breast, or a history of breast cancer in her family. She also did not have any constitutional symptoms such as loss of appetite or weight, or any fever. A manual expression revealed reddish brown milk discharge from both breasts. The mother and other family members were counselled by a lactation consultant. Mother was comforted and an icebreaking session was conducted by observing nonverbal communication strategies such as maintaining head level, keeping eye contact, maintaining appropriate distance without barriers, appropriate touching and patting, and showing interest in the discussion. Listening and learning skills like asking non-judging 27 questions studded with empathy, reflecting back and acknowledging the mother's apprehensions were used to build her confidence. The use of open-ended questions during counselling allowed the mother to vent her concerns and emotions. We showed the mother breast models to simplify her understanding of physiology of lactation and provided her with copies of published literature on rusty pipe syndrome to emphasise its innocuous nature. Figure 1. (A) Mother expressing the blood-stained colostrum from her breast on post-partum day 1, (B) Rusty appearing breastmilk expressed on postpartum day 1, (C) Mother expressing her breast on post-partum day 5, (D) Clearer breastmilk expressed on post-partum day 5. To facilitate continued communication between the lactation consultant and the mother, we shifted the mother-infant pair to the lying-in ward of the neonatal intensive care unit (step down unit of the neonatal intensive care area where mother-infant dyads are kept together on the same bed]. She was advised to express her breastmilk every 2-3 hours and discard it as she was not confident to feed it to her baby. The expressed breastmilk was subjected to biochemical and cytopathological analysis. Breastmilk analysis revealed: pH 8; haematocrit 14%; cytopathology: foamy macrophages seen against a haemorrhagic background but no malignant cells were seen. At the mother's insistence, the neonate was fed formula milk by cup while she continued to discard her expressed breastmilk. By day 5, colour ofthe breastmilk had started clearing (Figure lc] and by day 7, it was almost clear (Figure Id]. On day 7, the mother was willing to breastfeed her baby which was tolerated well by the infant. The mother-infant pair was subsequently followed up in the lactation clinic; at 4 months follow-up the baby was gaining weight well and was exclusively breastfed. Case 2 A 27-year-old primigrávida delivered a term (37 weeks' gestation] male infant weighing 2500 g, by vaginal route. The neonate was started on breastfeeds at 1 hour of life, which he accepted well. Fourteen hours after the delivery, the mother informed the attending paediatrician that she noticed discharge of blood-stained breastmilk from both breasts while the infant was being taken off the breast. A trained lactation management counsellor evaluated her. The mother did not complain of any régurgitation of breastfeed or vomiting by the neonate. The local breast examination was normal, except for bilateral bloodstained breastmilk. Detailed history revealed she also noticed blood-stained breastmilk from both the breasts at 7 months of gestation, which subsided on its own within 2 to 3 days, and no investigations were done. The expressed breastmilk analysis revealed pH of 7.0, haematocrit of 5% and no abnormal cells. A surgical consultation was obtained and surgeon ruled out intraductal papilloma as the blood-stained breastmilk was bilateral and seen to emanate from the multiple ducts. We counselled this mother to breastfeed her newborn on similar lines as described previously. She was quite comfortable and confident and continued 28 Breastfeeding Review • VOLUME 21 • NUMBER 3 • NOVEMBER 2013 to breastfeed. The colour of the breastmilk started improving on third post-partum day. The infant breastfed well without any vomiting or régurgitation. DISCUSSION Breastfeeding is important preventive, promotive and curative health behaviour with health implications for the infant, her mother and family. The World Health Organization [2003) recommends exclusive breastfeeding for the flrst 6 months of life, with continued breastfeeding until 2 years and beyond with appropriate complementary foods. Although the importance of breastfeeding is undeniable, assisting new mothers as they breastfeed can be a challenging task. Since breastfeeding is a bebaviour which is not performed only by instinct, there could be several socio-cultural factors and medical reasons which could hamper breastfeeding in the mothers [Shaheen Premani, Kurji & Mithani 2011). One such condition can be blood-stained breastmilk. The presence of blood-stained breastmilk during lactation can impart various shades of red-brown colour to the breastmilk, and is described as 'rusty pipe syndrome'. Occurring more commonly in primiparous women, bloodmixed milk is seen more often from both breasts [Merlob et al 1990; Virdi, Goraya & Khadwal 2001). It is generally noticed at birth or in early lactation, but it may be seen as early as the fourth month of gestation [Guèye et al 2013). The blood-stained breastmilk production is a consequence of accelerated growth of alveoli and their vascularisation during pregnancy and lactation [Sabate et al 2007). The blood in the breastmilk may arise from capillaries broken due to trauma to the breast, which can be due to faulty techniques of breastfeeding, manual breastmilk expression, or the use of a breast pump. Intraductal papilloma is another cause of presence of blood-strained breastmilk. However, it should be looked for in mothers with prolonged blood-stained breastmilk [Levèque et al 1990) and unlike rusty pipe syndrome, intraductal papilloma is mostly unilateral and associated with bloodstained breastmilk from a wart-like growth on the lining of a duct that bleeds as it erodes [Sainsbury 2008). As was seen in both our cases, rusty-pipe syndrome is a self-limited condition and most cases clears within 2 to 7 days of onset of lactation [Cizmeci et al 2013; Virdi, Goraya & Khadwal 2001). The fact that the second mother managed to breastfeed her baby despite the colostrum being blood-tinged supports that blood in the milk is not a gut irritant. Despite the condition being benign, it might be intimidating for some mothers. The presence of blood in breastmilk can cause significant psychological, aesthetic and functional concerns in the mother. In a survey, conducted amongst health professionals in neonatal intensive care units regarding the practice of feeding blood-tinged colostrum, 75% of Breastfeeding Review • VOLUME 21 • NUMBER 3 • NOVEMBER 2013 respondents reported that their practice was not to feed the blood-stained breastmilk [Phelps et al 2009). About 57% ofthe neonatologists and the lactation consultants and only 22% ofthe neonatal nurse practitioners, nurses and dietitians recommended feeding moderately bloody milk [p<0.001). The most common reason for not feeding blood-stained breastmilk was that it was believed to cause gastrointestinal upset and feeding intolerance. However, in the light of the obvious importance of breastmilk, scientiflc evidence is needed to prove that feeding blood-stained breastmilk will actually result in the perceived problems [Bua et al 2012). As was seen in our second case, wben mothers exclusively breastfeed, without expressing, they are unaware of their 'rusty pipes' unless a baby happens to regurgitate some ofthe blood-stained breastmilk [Guèye et al 2013). Also any blood in the breastmilk undergoes considerable dilution with milk and as such is not much of a problem. Therefore, we must emphasise that mothers must not withhold breastfeeding even if the breastmilk is bloodstained. In such cases, it would be very rewarding to provide mothers breastfeeding support and counselling to enable them to continue breastfeeding. As seen in our cases, one mother did not breastfeed her flrst offspring at all but could do so with the second child after active communication and counselling, albeit after few days when the colour of the breastmilk started changing to normal. Counselling encouraged the second mother to continue breastfeeding in spite of rusty colour of the breastmilk. It is to be reiterated that feeding bloodstained breastmilk is tolerated well without risk of régurgitation and vomiting. With proper counselling and help, it is possible to foster breastfeeding even in cballenging situations. One mother did not breastfeed ber flrst-born due to lack of proper counselling. However, sbe managed to successfully breastfeed her second offspring with appropriate help and proper counselling. We recommend continued breastfeeding in mothers producing blood-stained breastmilk and advocate breastfeeding support and reassurance to these mothers. REFERENCES Bua J, Travan L, Davanzo R, Demarini S 2012, More on professionals' attitudes on blood-tinged milk: a survey from Italy/Per/nato/32(3]: 243-244. Cizmeci MN, Kanburoglu MK, Akelma AZ, Tatli MM 2013, Rusty-pipe syndrome: a rare cause of change in the color of breastmilk. Breastfeed Med 8(3]: 340-341. doi:10.1089/ bfm.2012.0143 Guèye M, Kane-Guèye SM, Mbaye M, Ndiaye-Guèye MD, Faye-Diémé ME, Diouf AA, Moreau JC 2013, Rusty pipe syndrome in a 22-year-old primigrávida at 26 weeks' gestation. SAfrJ Obstet Gynaecol 19(1]: 17-18. 29 Levèque J, Priou G, Palaric JC, De Korvin B, Marcorelles P, Poulain P 1990, Nipple discharge without palpable tumor. Apropos of 46 cases. Rev Fr Cynecol Oèsiet 85(5]: 329-335. Merlob P, Aloni R, Präger H, Mor N, Litwin A 1990, Bloodstained maternal milk: prevalence, characteristics and counselling. Eur] Obs Gynecol Reprod Biot 35(2): 153-157. Phelps MM, Bedard WS, Henry E, Christensen SS, Gardner RW, Karp T, Wiedmeier SE, Christensen RD 2009, Attitudes of NICU professionals regarding feeding blood-tinged colostrum or milk./Pennato/29(2]: 119-123. Sabate JM, Clotet M, Torrubia S, Gomez A, Guerrero R, de las Heras P, Lerma E 2007, Radiologie evaluation of breast disorders related to pregnancy and lactation. Radiographies 27:S101-124. AUTHORS Dr MMA Faridi MD DCH, MNAMS FIAP FNNF Professor and Head Dr Pooja Dewan MD MNAMS Assistant Professor Dr Prerna Batra MD Associate Professor Affiliation Department of Paediatrics, University College of Medical Sciences and Guru Tegh Bahadur Hospital, Delhi 110095 India Sainsbury R 2013, The breast. In William NS, Bulstrode CJK, O'Connell PR (eds) Bailey and Love's short practice of surgery. 26th edn. Hodder Arnold, London. pp798-822. Shaheen Premani Z, Kurji Z, Mithani Y 2011, To explore the experiences of women on reasons in initiating and maintaining breastfeeding in urban area of Karachi, Pakistan: an exploratory study /S/?A/Peci;atrdoi:10.5402/2011/514323 Virdi VS, Goraya JS, Khadwal A 2001, Rusty-pipe syndrome. Indian Pediatr 38(8]: 931-932. World Health Organization 2003, Global strategy for infant and young child feeding. WHO, Geneva. URL: http://www.who. int/nutrition/publications/gs_infant_feeding_ text_eng.pdf Accessed 6/05/13. Mary Paton Research Aivard 2013 Presented by the Australian Breastfeeding Association for the best original paper on breastfeeding to Australian Breastfeeding Association O college of lactation consultants victoria inc. Dr Karleen Gribble Adjunct Fellow, School of Nursing a n d M i d w i f e r y University of Western Sydney For her original research A better alternative: w h y w o m e n use peer-to-peer shared milk The Mary Paton Research Award is presented by the Australian Breastfeeding Association and is kindly sponsored by the College of Lactation Consultants Victoria Inc. Photograph of Mary Paton: courtesy Prue Carr 2004 30 Breastfeeding Review • VOLUME 21 • NUMBER 3 • NOVEMBER 2013 Copyright of Breastfeeding Review is the property of Australian Breastfeeding Association and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.