Biopharmaceutics: Drug Absorption, Distribution, Elimination
advertisement

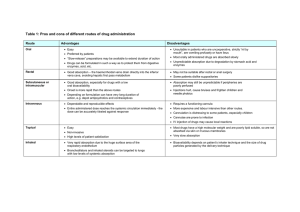
Biopharmaceutics It is the relationship between physicochemical properties of drug substance and its delivery system to its absorption into the systemic circulation when taken by all route of administration except I.V route. Absorption ▪ ▪ ▪ Distribution ▪ ▪ ▪ ▪ Volume of distribution ▪ Considered with only orally administration and absorption for GIT. This phase is irreversible as if drug absorbed from GIT to blood, it won’t return back against to GIT. Distribution will be in equilibrium state as after absorption, drug distributed within blood, body fluids and tissues always in equilibrium This phase is reversible as if drug cab be transported from blood into tissues or reverse to attain the body in complete equilibrium Example: The concentration of mepacrine in liver to plasma at distribution equilibrium is 25000: 1 امتحااااااااااااااااااااان This phase is irreversible Elimination done by major routes and some minor routes: Minor elimination routes (5%) Elimination ▪ Lung excretions ▪ Skin excretions ▪ Excretion by saliva ▪ It is a parameter shows the relative amount of drug outside blood (in tissue) amount of drug in body Volume of distripution = Cpo o ▪ If Cp increases → Vd decreases → drug localized in blood ▪ If Cpo decreases→ Vd increases → drug localized in tissue ❑ Significance of determining Vd: ➢ Detection of tissue localization as: 1- Drugs with high lipid solubility (non-polar) or has low ionization rates → localized in tissues 2- Drugs with high water solubility (polar) or has high ionization rates→ localized in Blood Tubocurarine ▪ ▪ ▪ ▪ Mepacrine Muscle relaxant Have short T1/2 Have high water solubility → drug localized in blood By increasing Cpo → Vd decreases ▪ ▪ ▪ ▪ Have long T1/2 Have High lipid solubility → drug localized in tissues By decreasing Cpo → Vd increases Its conc. In tissue is 25.000 times its conc. in plasma A. ABSORPTION PHASE Major elimination routes (95%) Composition of biological membrane: ▪ Urinary excretion ▪ Liver metabolism (biotransformation) 1) Lipids ➢ Glycero lipid ➢ Neutral lipid ➢ Phospho lipids (phosphatidyl serine, phosphatidyl choline, phosphatidyl ethanolamine) 2) Protein 3) Lipoprotein 4) Polysaccharide • Only phospholipid has the important role of absorption. امتحان • • • Gastrointestinal membrane act as lipoidal sieve which allow passage of lipid soluble drugs and prevent passage of water-soluble drugs. If the drug is completely lipid soluble without any water solubility it will not absorbed The drug must be lipid soluble with slightly water solubility. Biological factors Mechanisms of drug absorption 1) Passive diffusion Pharmacokinetics Bioavailability Absolute bioavailability Relative bioavailability Half life Drug disposition Tissue localization ▪ Rate process of absorption, distribution, metabolism and elimination of drug. ▪ It is the rate and extent of absorption of an administered dose into systemic circulation given by all routes except I.V route ▪ in which we compare any route of administration with I.V route ▪ in which we compare any route of administration to each other e.g. (rectal to oral, transdermal to oral) or different dosage form to each other e.g. (cap.to tablet, syrup to tab) ▪ It is the time needed for drug to decline to its half of initial concentration at any given time ▪ Loss of drug from blood compartment due to distribution to other tissues and elimination phase. ▪ Selective uptake of drug into the tissue or affinity in localization in certain tissues. • Drug transfer along concentration Gradient i.e. From high conc. to low conc. • Follow Fick’s low of diffusion Fick’s law: • Rate of diffusion across membrane is directly proportional to difference in drug conc. On both side of membrane 𝛥𝐶 − = 𝐾𝑎 [𝐶1 − 𝐶2 ] 𝛥𝑡 Where: 𝛥𝐶 𝛥𝑡 is rate of diffusion Ka is diffusion constant (proportionality constant) C1 is the concentration outside the C2 is the concentration inside the membrane Diffusion is affected by: 1- Thickness of the membrane as decreasing thickness will increase the diffusion 2- Area of the membrane as increasing surface area will increase the diffusion 3- Diffusion coefficient of drug 𝛥𝐶 In body: − = 𝐾𝑎 [𝐶1 ] 𝛥𝑡 2)Active diffusion ▪ 1- Size of pores & molecules 2- Solvent drag by increasing of water influx, absorption increase 3- Conc of drug in the intestinal lumen as by increasing conc. the probability of presence of drug adjacent to pores of mucosa increase pore transport increases Highly water-soluble material is very difficult to be absorbed in GIT which consist of lipid, so this method is important for transfer of essential substances as - Amino acid - glucose. Characters of active transport: o o o o o o Physiological factors Particles moves against concentration gradient (from low conc. To high conc) Carrier mediated transport (depend on carriers for transport) Saturable process (saturation of carriers occurs as the number of carriers in fixed). Site specificity as carriers located only in the upper part of the small intestine no carriers in stomach, colon, large intestine. Structure specificity each carrier is specific for certain molecule (i.e. carrier searches for specific structure for binding). Competitive process when more drugs have the same groups, competition on carriers will occur Energetic process i.e. needs energy affected by metabolite inhibitors such as anoxia (lack of oxygen), fluorides, dinitrophenol Not affected by pH or surface area Cannot be used by rectal route (ex. suppository) Follows zero order kinetics the absorption increases till all carriers are consumed and extra increase leads to stopping of the absorption Active transport Zero order kinetics absorb fixed amount passive transport First order kinetics absorb fixed percent Anatomy of GI tract Physiological Factors Affacting Drug Absorption o o o o Example: o In treatment of diarrhea, we use glucose in concentration of 5%, if the concentration increased to 50-60%, only 5% will be absorbed and the excess amount will be concentrated in large intestine and dissolve in water causing more diarrhea. pH of GI tract Food volume of food Temperature of food body posture Gatric emptying rate Viscosity Diatery Effect Drugs Intestinal Motility Acidity Drug Stability in GI tract Hepatic Metabolism particle size Emotional state Local disease GastricSurgery Diarrhea Micellaneous Age 3)Facilitated diffusion Stress The same as active transport but differs in: ▪ Drug transfer along conc. Gradient and Not require energy Examples: Quaternary ammonium compounds and Vitamin B12 مهم Bed ridden patient 4) Ion Pair Mechanism Unionized form lipid soluble absorbed Ionized form water soluble not absorbed ▪ Each ion attached to membrane another ion of the opposite charge in the GIT to form neutral ion (ion pair) which have high lipid solubility so can pass gastrointestinal mucosa. Quaternary ammonium compounds and tetracycline: مهم جدا ▪ These drugs are highly ionized in the GIT so lipid insoluble and not absorbed ▪ They are too large molecules to pass through pores of the cell membrane of GIT but it found that these drugs can pass in large amounts due to ion pair mechanism. ▪ There in a drug interaction with endogenous materials or organic ions of opposite charges forming neutral ions with high lipid solubility. 5)Pinocytosis = phagocytosis ▪ ▪ ▪ ▪ Drug molecules not have to be in solution to be absorbed. It is important for absorption of macro molecules by engulfing ex: protein It’s specialized for absorption of Macromolecules (large M.wt.) as: (Fats, proteins, vitamins A, D, E) It is essential for absorption of milk protein in infants. 6) Pore transport ▪ Size of the radius of aqueous field pores is 4Ao so drugs which have this molecular size or less, can be absorbed by pore transport. ▪ Examples Urea, H2O and low molecular weight sugars. Factors affecting absorption by ore transport: 1. Anatomy of GIT • • • Stomach Small intestine, subdivided to (Duodenum, jejunum and ileum) Large intestine ❑ Small Intestine: ➢ Small intestine is the main site of absorption as: مهم a. It has a large surface area due to presence of villi (finger like projection) which increase surface area of absorption millions of time rather than normal cylinder. b. It is the longest part of GI tract. c. Exhibit a long residence time. Length of Various region of GI tract Overall length of GI tract Small intestine (duodenum, jejunum and ileum) Large intestine About 4.5 meter About 2.75 meter 1 meter Physiological conditions of GIT Part Residence time Mouth & Esophagus Stomach Small intestine Large intestine Few minutes 0.5 – 3 hours 6 – 8 hours 10 hours PH Secretions 5 – 8.5 1 – 1.5 7.5 – 8.5 No secretions Chyme No 3–5 6–8 7 – 7.5 Absorption area (Meter2) No 0.1 – 0.2 100 0.5 – 1 2. pH of the GIT Emotional state pH of Stomach → about 1 – 1.5 pH of duodenum → about 5.5 – 6.5 pH of colon → about 7 – 7.5 pH is about 1 – 1.5 Fasting pH increases after meal so absorption decreases Fats in food Anticholinergic Decrease the secretion of HCL so pH increases Antispasmodic Antacids Increase the pH by Neutralizing acidity of the stomach Peptic ulcers increase the secretion of HCL so pH decreases • • Acidity مهم جدا جدا • The stomach empties its contents into the small intestine. Because the duodenum has the greatest capacity for the absorption of drugs from the GIT, a delay in the gastric emptying time for the drug to reach the duodenum will slow the rate and possibly the extent of drug absorption, thereby prolonging the onset time for the drug. • Generally, we prefer rapid gastric emptying rateمهمة جدا Repulsive Movement 5 mg 10 mg 30 mg 2.4 mg 3 mg 4.7 mg Absorption after meals 3.1 mg 6.3 mg 18.2 mg Effect of food on Griseofulvin Increased % of absorption 29 % 110 % 287% • When taken with fatty meals, GER decreased and absorption increased as it makes contraction of gall bladder which make stimulation of secretion of bile which increase emulsification of fats so increased absorption • They found that griseofulvin when taken with fatty meals, its concentration in blood is 8 times more than if taken before meals. ❑ Factors affecting GER: Food • Volume of the • • food Temperature of food Body posture Viscosity • • • • • • Food (fat, protein and carbohydrate) decreases GER Fat > Protein > Carbohydrate Small volumes → initial lag time of GER is slow, then become rapid. Large Volumes → initial lag time of GER is rapid, then become slow. Temp up to 37 oC → GER increased. Temp above 37 oC → GER decreased. In case of hot meals, GER is decreased as a protective reflex mechanism occur to protect duodenum cells which cause contraction of sphincter to prevent passage of food to delay GER. Lying on the right side enhance the GER more than the left side. Increasing viscosity will decrease GER Decreasing viscosity will increase GER Duodenal ulcers Reflex action will be low as duodenal contents are acidic and cannot differentiate between acidic drugs and its contents so it will increase GER Circular (mixed) Movement • Contraction occurs longitudinally by longitudinal • muscles • • Can affect Transit time and residence time. • Hypermotility (increasing motility) decreases • residence time and absorption. • Hypomotility (decreasing motility) increase residence time and absorption. Contraction occurs due to circular muscles. Affects increasing dissolution rate of poorly soluble drugs. Allow drug molecules to leave chyme and contact with intestinal mucosa so increase absorption. ❑ Importance of intestinal residence: ➢ It is important for: 1) drugs absorbed by intestinal carrier mediated active transport mechanism. 2) sustained and prolonged release formulations. 3) Enteric coated formulations. 4) Drugs dissolves slowly in the intestinal fluids. Effect of food on Riboflavin Absorption in fasting state Hyperacidity stimulate the GER Achlorhydria decreases the GER Peptic ulcers Firstly, increasing acidity will increase the GER but excessive increasing cause reflex mechanism which leads to contraction of sphincter to protect duodenal cells from high acidity leading to decrease GER 4. Intestinal Motility Rapid gastric emptying rate is preferred in Slow gastric emptying rate is preferred in Dose Excitation will increase GER due to increasing GIT motility. Depression will decrease GER due to decreasing GIT motility. Particle size • Fine particles increase GER while coarse particles decrease it Effect of drugs • Antacids, antispasmodics and anticholinergics decrease GER 3. Gastric Emptying rate 1- Drugs that are unstable in stomach as 1. Active transport as riboflavin (vitamin B2) if erythromycin and benzyl penicillin. taken in empty stomach → their absorption will ↓ 2- Enteric coated formulations. so they are better absorbed when taken after meals 3- Anthelmintic drugs to optimize the 2. Lipid soluble drug as Griseofulvin If taken with therapeutic effect. fatty meals → its bioavailability will be enhanced. 4- Anti-amoebic drugs Why? As with fatty meals the biliary secretion 5- Basic drugs. occur which enhance absorption of the lipid soluble 6- Drugs that are irritant to stomach. drugs so slow gastric emptying rate is required to allow the biliary secretions to take place • • 5. Drug Stability in GI Tract and Interaction of Drug with Components of GI Tract • • Mucin → is Viscous mucopolysaccharide acts as protective layer that covers the mucosae of stomach and intestine. Enzymes may convert prodrugs to active metabolites as: 𝐸𝑠𝑡𝑒𝑟𝑎𝑠𝑒 𝑒𝑛𝑧𝑦𝑚𝑒 Acetoxy methyl ester of penicillin → penicillin 𝐸𝑠𝑡𝑒𝑟𝑎𝑠𝑒 𝑒𝑛𝑧𝑦𝑚𝑒 • • Chloramphenicol palmitate → chloramphenicol Enzymes may convert drug in the active form to inactive form as insulin by enzymatic hydrolysis gives amino acids that is inactive Drugs may be hydrolyzed in the GIT by: 6. Hepatic Metabolism Physico chemical factors affect drug absorption ❑ first pass effect: • Drugs which absorbed from the GI tract always pass in hepatic portal vein before reaching blood so liver degrades part of drug. ❑ Solution for first pass effect: PH partition theory a. Give the drug by another route than oral route such as injection, suppositories or inhalation. b. Increase the oral dose c. Increase dissolution rate of the drug Dissolution rate Complexation Adsorption Surface active agent (SAA) ❑ N.B. • • If we increase oral dose, molecules that received by liver will be exceed the capacity of liver enzymes so some will be broken by liver and other will pass unchanged. If we intended to use rectal suppositories, administration must be in lower part of rectum. 1- pH Partition Theory ❑ It is a relationship between: ➢ the dissolution constant of drug ➢ lipid solubility for drug ➢ pH of the absorption site Example: Isoprenaline (Antiasthmatic) Route Dose Injection 200 µg/ml Inhalation 80 µg/ml Oral 30000 µg/ml 7. Dietary Food • • Generally, gastrointestinal absorption is Preferred by an empty stomach The effect of food on the absorption rate of drugs is probably result of delay in the GER and decrease bioavailability. • Alteration in the rate of gastric emptying especially (solid - hot - fatty) meals so delay gastric emptying and ↓ bioavailability of drug • Cellulosic food with high viscosity may absorb some drugs so decrease the absorption of these drugs. • Tetracycline when taken with antacids (contains Ca+2 or Mg+2) or dietary products containing calcium or iron ions, it will form non-absorbable complex. • Bile acids may form insoluble non-absorbable complex with neomycin, nystatin and kanamycin. • The absorption of few drugs is actually promoted when administered following a meal for example Griseofulvin, its absorption increases with fatty meals. مهمة • After meals, blood flow to liver and GI tract increase leading to increasing absorption rate. • Gastric secretions may increase the absorption of drugs that is stable in acidic pH, on the other hand, it decreases the absorption of the unstable drugs. • Fats stimulate secretion of bile → so ↑ rate of dissolution of lipid soluble drugs and ↑ bioavailability ❑ Henderson-Hasselbalch equation: For Acidic drugs pKa − pH = log • Gastric surgery Diarrhea Age Stress Bed ridden • • • • • • • • • Cause alteration of the gastric pH pH elevates to 6.9 or 7 with gastric cancer total or partial gastrectomy if drugs slowly dissolute, absorption decreases and bioavailability decrease. If drugs rapidly dissolute to small intestine, it will increase its GER, absorption and bioavailability. Hypermotility leads to decrease of residence time so absorption decreases. Increasing age will decrease absorption Stress will decrease absorption. Decrease absorption. Physicochemical Factors Affecting Drug Absorption Ci Cu Cu=concentration of ionized fraction pKa − pH = log • ❑ Examples: • • • • • 2 Acidic drugs Drug A with pKa 5 Drug B with pKa 10 Drug A is more acidic than drug B so drug A is • more ionized than drug B so drug B is more absorbed. • • 2 Basic drugs Drug A with pKa 5 Drug B with pKa 10 Drug B is more basic than drug A so drug B is more ionized than drug A so drug A is more absorbed. pKa of basic drug & pKa of acidic drugs → ionization → absorption For acidic drugs, High pKa means weak acid so less ionized and highly absorbed For basic drugs, High pKa means strong acid so more ionized and poorly absorbed Drugs with PKa 1 or 2 will be strongly acidic and in ionized form then absorption decreased. Drugs with PKa 13 or 14 will be strongly basic and in ionized form then the absorption decreased ❑ Partition coefficient: 8. Miscellaneous factors Local disease Cu Ci Cu=concentration of unionized fraction For basic drugs Barbiturates absorption in rat colon is defined as the ratio of the concentration of a solute in the organic solvent or lipid phase to its concentration in the water phase. By increasing Partition coefficient, absorption increases conc. of drug in lipid partition coefficient = conc. of drug in water Drug Barbital Phenobarbital Cyclobarbital Pentobarbital Secobarbital Partition coefficient 0.7 4.8 13.9 28 50.7 % absorbed 12 20 24 30 40 2- Dissolution Rate • When a drug is given orally, the rate of absorption is often controlled by how fast the drug dissolves in the absorption site. 𝑑𝑖𝑠𝑠𝑜𝑙𝑢𝑡𝑖𝑜𝑛 𝑎𝑏𝑠𝑜𝑟𝑝𝑡𝑖𝑜𝑛 Solid drug → drug solution at absorption site → • Absorption of different dosage forms: drug in systemic circulation • • To improve the dissolution of Acidic drugs in acidic medium, we formulate the drug in its Basic salts. And for Basic drugs in alkaline medium we formulate it in its Acidic salt as: a. Atropine → Atropine sulphate b. Codeine → Codeine phosphate Salt Formation ❑ Aluminum salt of aspirin: • Aluminum salts of aspirin is used for showable tablets to minimize the taste of the drug but unfortunately it is more slowly absorbed. • At pH 8, dissolution rate decreased due to formation of basic insoluble Al (OH)3 upon reaction with water. • Al (OH)3 is insoluble gelatinous form that retard penetration of water so take long time for disintegration and dissolution decreased. • To solve this problem, Adding EDTA as chelating agent to chelate free Al ions to prevent formation of Al (OH)3 Generally, we prefer high dissolution rates for drugs. ❑ Drugs requires slow dissolution rates: o Irritant drugs as nitrofurantoin. o Unstable drugs as erythromycin and benzyl penicillin. ❑ Factors affecting dissolution rate of drugs: a) b) c) d) Noye’s and Whitney equation. Crystallization Surface area. Hydration and solvation a) Noye’s and Whitney equation dC DSCs = dt h ▪ • • • • For example: Acidic drug (Salicylic acid) Solution: • Addition of nahco3 to the salicylic acid, it will result in the formation of Na. Salicylate and increase PH of the diffusion layer leading to enhancement of the dissolution of salicylic acid. • Once Na. Salicylate diffuse to the bulk, it will react with HCL → and predicated as very fine particles in very huge surface area which enhance diffusion → become ready for absorption • • • For basic drugs • • • Particle size → surface area → rate of dissolution →rate of absorption. ❑ Types of Surface Area: Effective surface area ❑ Solubility in the diffusion layer and salt formation: • decrease hydrogen ion conc and increase dissolution so drug transfer from diffusion layer to bulk (stomach) where it precipitates as fine particles so increasing of surface area will increase dissolution b) Surface Area Where: ▪ dc/dt → is the dissolution rate. ▪ K → dissolution rate constant (equals D/h) ▪ D→ is the diffusion coefficient of the dissolving material ▪ h → the thickness of the diffusion layer (membrane) ▪ S → surface area of the dissolving solid. ▪ Cs → is the saturation solubility of the drug in solvent. ▪ C → concentration of drug in the solvent at time t • 1.7 1870 < 0.1 550 • Salicylic acid will decrease dissolution rate so by adding NaHCO3, it will give Na. salicylate which In body: ▪ The C is negligible compared to Cs, so equation can be written as: dc Ka = K’Co [1 + + ] [H ] dt Rate of dissolution is inversely proportional to hydrogen ion concentration. hydrogen ion conc. (pH) →dissolution rate. pH of the stomach is about (1-2) so increasing H+ ion conc will decrease the dissolution rate and the rate of absorption also decreases. To solve this problem, we should decrease H+ ion conc by salt formation Benzoic acid Sodium benzoate salt Phenobarbital Sodium phenobarbital salt Salicylic acid Sodium salicylate salt Sulfathiazole Sodium sulfathiazole salt Dissolution rate at pH 1-2 2.1 980 0.24 200 Buffering system dC DS(Cs − 𝐶) = KS(CS − C) = dt h For acidic drugs Compound [H + ] dc = K’Co [1 + ] dt Ka Rate of dissolution is directly proportional to hydrogen ion concentration. hydrogen ion conc. (pH) →dissolution rate. pH of the stomach is about (1-2) so increasing H+ ion conc will increase the dissolution rate and the rate of absorption also decreases. But stomach not the good site for absorption of basic drugs so when dissolution rate of basic drugs increases in stomach, this increases the absorption of these drugs in intestine. Specific (absolute) surface area It is the surface area of drug in body. • It is the surface area of solid surface that • exposed to the dissolution medium. It is less than specific surface area. • It is the surface are of drug measured in labs. It is the total surface area of solid surface of any particle. It is more than effective surface area. ❑ Effect of surface area on griseofulvin: Effect of particle size on dissolution rate of Griseofulvin • • • GROUP DOSE PARTICLE SIZE BLOOD LEVEL Group 1 1g 10 µ Drug Blood conc is equal Group 2 0.5 g 2.5 µ The experiment was done on 2 different groups of experimental animals. Each group received a different dose with different particle size of griseofulvin. The observed result was that both drug blood conc of drug is equal in the two groups however there was a difference in the administered dose. ❑ Effect of surface area on Chloramphenicol: • • • • Chloramphenicol exists in three doses with different particle sizes (50, 400, 500). The three doses have the same extent of absorption and the same bioavailability, but differs in the residence time. They have different plasma peak (conc time curve) but have the same AUC (bioequivalent). The more residence time will affect the beneficial normal flora in the GI tract, so we should decrease residence time to prevent effect on normal flora, so increasing the dissolution rate is a must. مهم جدا Residence Time → Effect on Normal Flora c) Polymorphism ▪ It is the presence of substance in more than one crystalline form. ▪ ▪ • • Amphetamine + CMC (carboxymethyl cellulose) → give non-absorbable complex. Phenobarbital + PEC 4000 (polyethylene glycol) → give non-absorbable complex. • Tetracycline + heavy metals (Ca+2, Mg+2, iron)→ give non-absorbable Polymorphism includes Amorphous and crystalline state. They may differ in: 1. Density, 2. Melting point, 3. Solubility, 4. Dissolution rate. Amorphous 4- Adsorption ❑ Types of Adsorption: Crystalline Metastable form (unstable) Stable form • Highest energy state • Lowest energy state • Lowest melting point • Highest melting point • Higher solubility • Lower solubility • Active form • Inactive form • Better absorption and bioavailability. • Lower bioavailability ❑ Conversion between amorphous and crystalline: ▪ Amorphous form which is active form, may be converted to inactive crystalline form so we can prevent this conversion by addition of methyl cellulose as suspending agent ❑ Examples: 1- Insulin: ➢ Amorphous state → highly soluble so increases dissolution rate and give immediate action. ➢ Crystalline state → lower solubility so decreases dissolution rate and gives sustained action 2- Chloramphenicol & Novobiocin: ➢ Amorphous → active form with high absorption rate ➢ Crystalline → inactive form with low absorption rate 3- Riboflavin (Vit B2): ➢ Have 3 different polymeric forms that differ in dissolution rate and the range are from 60 to 1200 mg/l d) Solvation and Hydration ▪ Crystallization of one molecule of substance combined with one or more molecule of solvent ➢ Hydrates → when the solvent is water. ➢ Solvates → when the solvent is Organic solvent. ❑ For Hydration: Anhydrous form has greater dissolution rates that hydrous form. Examples: 1. Ampicillin (anhydrous) and Ampicillin trihydrate 2. Mercaptopurine ❑ For solvation: Solvated form has greater dissolution rates that A solvated form. Examples: 1. Grisofalvin chloroformate (solvated form) and Grisofalvin (asolvated form) 3- Complexation • Interaction of the drug with materials in GI tract or with inert or active compound of the dosage form. ❑ Complexation may affect: مهم جدا a. b. c. d. Molecular size, Diffusibility, Solubility, Partition coefficient ❑ Compounds which can interact with drugs: 1. 2. 3. 4. Methyl cellulose derivatives Gum Tragacanth High molecular weight polyethylene glycol Non-ionic surfactant ❑ Examples for complexation reactions: Physical adsorption • Reversible • Not affect the bioavailability. Chemical adsorption • Irreversible • Affects the bioavailability. ❑ Examples of Adsorbents: 1- Charcoal 2- Bentonite 3- Vegum 4- MgO, 5- MgCO3 6- Mg trisilicate 7- Clays include Bentonite, vegum Attapulgite 8- Attapulgite ❑ Examples for adsorption reactions: A. PROMAZINE • If taken alone, there is a maximum bioavailability about 100% • If taken with attapulgite, the bioavailability decreased to 80% • If taken with charcoal, the bioavailability become 50% • If taken alone, bioavailability about 100% B. LINCOMYCIN • If taken before attapulgite - pectin suspension, the bioavailability is 100% • If taken with the mixture at the same time, the bioavailability is 20% • If taken alone, there is a maximum bioavailability about 100% • If taken before kaolin-pectin suspension, the bioavailability is 100% C. DIGOXIN • If taken with the mixture at the same time, the bioavailability is 40% • If it taken alone, the bioavailability is 100% D. Quinidine sulfate • مهم جداIf taken with kaolin pectin suspension, bioavailability is 46% 5- Surface Active Agent Types of S.A.A: Anionic → not taken orally Cationic → not taken orally Non-ionic → taken orally Effect of S.A.A on absorption: Below Critical Micelle Conc. ➢ Increasing concentration of the surfactant is accompanied by increasing of the absorption. 2. Above Critical micelle conc. ➢ Increasing the concentration of surfactant, absorption decreases due to micellization which entraps the drug inside it. ❑ Role of Surface-active agent: ➢ Affect permeability of GI tract by causing disorganization of lipid in cell membrane causing: 1. Fluidity of lipid in the biological membrane. 2. Increase flexibility. 3. Decrease interfacial tension. 4. Allow the passage of water-soluble drugs. ❑ Effect of surfactant on organic and inorganic materials: 1- Organic materials: ➢ Such as iodoform ➢ Surfactant decreases absorption of organic materials due to micellization. 2- Inorganic materials: ➢ Such as Potassium iodide ➢ Surfactant increases absorption of inorganic materials due to disorganization of membrane so increases fluidity and absorption ❑ • • • ❑ 1. B. Distribution phase • After absorption, drug distributed to body compartments such as (tissue and blood). • Blood volume in adult (5.5 – 6) liters which flow one cycle per minute. • Volume of plasma is about 3 liters. • Blood flow is different from part to part. ❑ Types of organs according to blood flow: A. Highly perfused organs: ➢ Have high blood supply so have rapid drug distribution ➢ as Kidney, liver, brain, Lungs and heart B. Low perfused organs: ➢ Have low blood supply so slow drug distribution ➢ As Muscles and adipose tissue C. Poorly perfused organs: ➢ very low blood flow or Nearly absence of blood flow ➢ as Skeleton ❑ Factors affecting distribution phase: ➢ Lipid solubility: • lipid soluble drug will permeate through lipid membranes. • Water soluble drugs with low molecular size diffuse through pores. • Large molecules of low lipid solubility have special transport (active transport). A- CELLULAR DISTRIBUTION ❑ Extracellular fluids: ➢ Examples: • Administration of phenobarbital (weak acidic drug) to 2 group of dogs, Dogs are subjected to drug in acid and alkaline medium. GROUP A ▪ ▪ ▪ Acidosis through inhalation of CO2 leading to ▪ acidification of blood. Drug will be in unionized form ▪ absorption and distribution increased → low ▪ conc. in blood → high lipid solubility GROUP B Alkalosis through administration of NaHCo3 leading to alkalization of blood. Drug will be in ionized form absorption and distribution decreased → high conc. in blood → low lipid solubility B- DISTRIBUTION TO TUMER CELLS • • • There is limited vascular supply to tumor cell due to increased proliferation cells. The drug cannot distribute to that area with effective conc. And to obtain effective conc. We should increase the dose but this will increase side effects. • To solve this problem, Continuous IV dripping to get constant and continuous blood level should be used. C- DISTRIBUTION TO CNS • • Capillaries of brain differ in their permeability characters from other capillaries in body. Because they have blood brain barrier (BBB) which is less permeable to water soluble substance. ❑ Examples: Thiopental Barbital Dopamine ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ ▪ High partition coefficient High lipid solubility Can pass BBB Has short duration of action Used in general anesthesia Low partition coefficient Low lipid solubility Slowly penetrate BBB eliminated from body before reach to effective conc Used as sedative and hypnotic Used in treatment of parkinsonism which caused by decrease dopamine conc. in ▪ ▪ Penicillin & tetracycline ▪ brain but dopamine is less effective as it is water soluble and can't pass BBB. To solve this problem, use pro drug levodopa (inactive) form which can penetrate BBB then metabolize in CNS and converted to dopamine (active) Low lipid solubility so it is highly ionized and can't pass BBB so tetracycline can’t be use in treatment of meningitis Use sulfa drugs instead of tetracycline as prophylactic dose as sulfa is high lipid soluble and can penetrate BBB. D- PLACENTAL DISTRIBUTION • Transfer of drugs from maternal blood to fetal blood by placenta ❑ Placental distribution affected by: 1. Lipid water solubility 2. Plasma protein binding 3. PH 4. Pka ❑ Examples of drugs that can transfer to fetus: ▪ Alcohol ▪ Nicotine ▪ Codeine ▪ Narcotics ▪ Barbiturates ▪ Analgesics ▪ Used as analgesics for pregnant women but found that it causes: Thalidomide a. 50 % of fetus dies مهم جدا b. 50 % of fetus with teratogenic effect. Alcohol May cause delayed response Nicotine Cause infant suffer from Abdominal cramps, pains, nausea and vomiting Plasma Protein Binding • • Major plasma proteins are albumin and globulin Albumin is most generally bind with acidic drugs more than basic drugs while Globulin is bind with corticosteroids ▪ More involved in the binding process - Acidic drugs are bound more than Albumin basic drugs because pH of the blood is slightly alkaline (pH 7.4) Globulin ▪ Not widely involved in binding process - Corticosteroids bound to globulin ❑ Characters: 1. Increase half-life so increase duration of action and increase residence time so called store house. 2. Can't cross biological membrane. 3. Low glomerular filtration. 4. Act as physiological solubilizer as if drug is not bind by fixed percentage, it will ppt. → bishydroxy coumarin (anti-coagulant) binds with 98 % so only 2% can give therapeutic effect. 5. Reduce absorption and distribution. 6. Displacement → one drug displaces another one from binding site due to its high affinity to protein so increases free drug causing side effects. ❑ Conc of Mepacrine : مهمـــــــــــــــة ➢ Plasma → 5000 Spleen → 9000 Liver → 21000 Elimination Phase • • Distribution and absorption affect onset time but elimination affect duration of action. Duration of action is related to: a. frequency of administration. b. The dose administered each time • Drug with high T1/2 → have low frequency of administration • Drug with low T1/2 → have high frequency of administration ❑ Elimination of drugs occurs through: امتحان Major eliminating organs • • Renal “through kidney” Biotransformation “through liver metabolism). Minor eliminating organs • • • • Saliva excretion Skin excretion Biliary excretion Pulmonary A.RENAL EXCRETION • Removal of unchanged drug from the body through kidney ❑ Characters of drugs eliminated by renal execration: creatine phosphate in muscle • If half-life increases this indicates kidney dysfunction. • Rate of production of creatinine equal to rate of Characters of substances that used as exogenous elimination diagnostic agents: • Normal individual conc. in blood (1 – 2 mg/100 1. Filterable and Non-toxic ml) 2. Unbound to plasma protein • If conc. of creatinine increases, this indicates 3. Easily analyzed kidney dysfunction 4. Remain chemically uncharged a. Water soluble b. Low molecular weight c. Slowly bio transformed ❑ Mechanisms of Renal Elimination: 1. Glomerular filtration. 2. Active secretion. 3. Active and passive tubular reabsorption. Molecules that can pass Molecules that cannot pass Glomerular • Liquid plasma. • Blood filtration • Dissolved solute with low Molecular weight. • Plasma proteins • • Active secretion • Drug that binds with plasma proteins Energetic process in which acidic and basic drugs are execrated. Characters: ✓ Need energy. ✓ Site specificity. ✓ Transfer against conc. Gradient. B. BIOTRANSFORMATION • It is a process by which drug converted to another form that may be either active, less active or inactive. ❑ There is a difference between biotransformation and metabolism: Metabolism Biotransformation ✓ Process of biotransformation of food staff ✓ Accompanied by producing energy ❑ Examples: مهمة جدا جدا Drug Upon Biotransformation Methanol (non-toxic) Phenyl butazone (active) Phenacetine (Active) Codeine (Active) Prednesol (Active) Diazepam (Active) Formaldehyde (toxic) Oxyphene butazone (more active) Paracetamol (more active) Morphine (more active) Prednisolone (more active) Nor diazepam (more active) Active Reabsorption • Reabsorption Include reabsorption of all essential substances • Glucose, vitamins, water, Na, K Passive reabsorption Depend on PH partition theory For acidic drugs For basic drugs Make alkalization of urine by NaHCO3 so Make acidification of urine by NH4Cl so basic drugs acidic drugs will be ionized (low lipid will be ionized (low lipid solubility) so increase solubility) so increase secretion. secretion ❑ Notes: • • • • • • Daily Rate of blood flow to kidney is 1700 L/ day Half of this amount is plasma (850 L / day) Only 20 % filtered by glomerular filtration (170 L /day) This means that execration per hour is 7 – 8 L/hr This means that execration per minute is 130 ml/min مهم جدا but they found that only 60 ml / hr are execrated in urine and the rest of the quantity is reabsorbed by reabsorption ❑ Renal Clearance: ❑ Why does biotransformation mostly cause deactivation of drugs? As it converts drugs to more water-soluble compound (less lipid soluble) which can easily clean by kidney ❑ Two phases of biotransformation: Phase I Phase II ✓ Include addition of functionally reactive group ✓ Include conjugation of reactive group with by oxidation, reduction, hydrolysis or other conjugating agent such as glycine – glutathione methods. –glucuronic acid ✓ If drug have a functional group, it will pass directly through phase II without undergoing phase I ❑ Examples of Phase I: Reaction S-oxidation Aromatic hydroxylation Aliphatic hydroxylation Oxidative – o – de alkylation Azo reduction Hydrolysis Acetylation • The operative mechanism of renal excretion. urinary excretion rate U×V • Renal clearance (R.C) = drug plasma conc = Cp • U→ amount of unchanged drug in urine. • V→ Volume of drug excreted per minute. • Cp → plasma conc of drug ❑ Clearance ratio: Example ✓ ✓ ✓ ✓ ✓ ✓ ✓ Chlorpromazine → chlorpromazine sulfoxide Phenyl butazone → Oxyphene butazone Meprobamate → hydroxyl meprobamate Phenacetine → paracetamol. Prontosil → sulfanilamide Acetyl salicylic acid → salicylic acid Sulfa drugs → N – 4 – acetyl sulfanilamide ❑ Problem and solution: • Relation between renal clearance of drug and glomerular. Renal Clearance R.C • Clearance ratio= glomerular filtration rate = G.F (130 ml/min) • • If the clearance ratio = 1 (R.C=G.F)→ the drug is completely excreted by glomerular filtration • If the clearance ratio <1 (R.C<G.F) → So drug is reabsorbed again • If the clearance ratio >1 (R.C>G.F)→ So drug execrated by GF and active secretion ❑ Kidney function test: ➢ Can be done by 2 methods: Endogenous substance ✓ Process by which drug converted by another form. ✓ Accompanied by formation of more active, less active or inactive form of drug Exogenous substance • Substance which secreted in body as creatinine. • Substance which injected IV as inulene. • Creatinine is the metabolite of creatine and • Rapidly execrated from the body half-life is 6 min • Problem → Sulfa drugs lead to formation of renal calculi as acetylated sulfa drugs is less water soluble so present in high conc. in blood and exceed saturation conc. so ppt forming calculi Solution → By using an additive combination of 4 – 5 types of sulfa drugs so conc. of sulfa drugs decreases and ability to ppt decrease and can't reach saturation conc ❑ Examples of phase II: Reaction Benzoic acid (less water sol.) + glycine Chloramphenicol + glucuronic acid by glucouronyl transferees Salicylamide + sulfate ❑ Factors affecting biotransformation: Product Hippuric acid (water sol.) Chloramphenicol glucuronide Salicylamide sulfate Different species (rats-cats-human) have different metabolizing enzyme so show different biotransformation. • Chlorpromazine is bio transformed by different mechanisms مهم جدا: a. Hydroxylation. b. Sulfoxidation. c. N-oxidation. d. N-de methylation. • Rate of biotransformation in human slower than animal so human show slow inactivation & animal show rapid inactivation. (Half-life In animal < Half-life in human). • Metabolizing enzyme varies with time. In geriatrics In fetus • Limited renal function. • Have low hepatic enzymes. • Decreasing liver microsomal enzyme. • Have low metabolizing enzymes such as glucouronyl transferase enzyme. • Decrease Function of liver & kidney so should ↓ dose to avoid agglomeration. • No conjugation so leads to accumulate substances so dose should be decreased • Low rate of biotransformation. • Limited renal excretion ❑ Hepatitis: ✓ Hepatic enzyme decreased so biotransformation decreased & ↑ t1/2 so may cause accumulation ❑ Acetylation of PAPA: ✓ Biotransformation increase in diabetic patient as it may cause high biotransformation so low half-life ✓ Biotransformation decrease in hyperthyroidism patient as it may cause low biotransformation so high half-life. • Variation between individuals. • An average dose may under medicate group of patient and cause toxicity in another group. • Resistant individuals, need more dose than normal dose to give same effect. • Sensitive individuals need low dose than normal dose to give same effect. ❑ Examples: Di phenyl hydantoin Average plasma level of same dose is (2.5 – 40 ug/ml) so 16-fold difference. Bis hydroxyl coumarin Used as anti-coagulant with 14-fold variation in blood level • Variation based on genetic difference ❑ Isoniazid: When some dose of drug is administered to Caucasians, it shows that: ✓ 50 % rapid in activator and have short half-life so high biotransformation. ✓ 50 % slow in activator and have long half-life so low biotransformation. ✓ So, they need different doses from the same drug. ✓ Drug may change metabolism due to inhibition or stimulation of hepatic enzymes Hepatic Enzyme Induction Hepatic Enzyme Inhibition ✓ One drug increase rate of biotransformation of ✓ They decrease metabolism and increase halfthe other drug when taken together so high life metabolism and low half-life. Examples: Examples: • Alcohols metabolism of phenobarbital and • Warfarin metabolism of tolbutamide. tolbutamide. • Chloramphenicol metabolism of hexobarbital. • Phenyl butazone metabolism of • Isoniazid metabolism of phenytoin. aminopyridine. • Methandrostolone metabolism of oxyphenyl • Barbiturates metabolism of digoxin, bilirubin butazone. & bis hydroxycoumarin. • Chloral hydrate metabolism of bis hydroxyl coumarin. Effect of drug Pharmacogenetics Inter subject variation Pathological conditions Age Species difference • ❑ Notes: • Bilirubin found in plasma in conjugated form. • When present in unconjugated form (free form) tis increase bilirubin and cause hyper bilirubinemia causing jaundice. • To solve this problem, give phenobarbital which stimulate biotransformation of decomposition of bilirubin and increase conjugation of free bilirubin but it is unsuitable in case of infants as barbiturates or phenobarbital have a great sedative effect which may be harmful for baby. • Using phototherapy as bilirubin is photo-sensitive. C. BILIARY EXCRETION ✓ Liver excrete (0.5 – 1) L/day of bile into the duodenum through bile duct but 90% of excreted bile is actively reabsorbed ✓ As it is highly ionized with low lipid solubility and move against conc. gradient so can't be absorbed by passive diffusion and it is actively reabsorbed. ✓ After meals, gall bladder is contract and this increase delivery of biliary excretion. ❑ Composition of Bile: ➢ Cholic acid, Deoxy cholic acid & other sodium salts. ❑ Entero-Hepatic Circulation: ✓ Many drugs excreted by liver cells into the bile by active process for acidic and basic drugs. ✓ Most are reabsorbed from intestine then secreted again from liver until complete excretion. ❑ Examples of biliary excretion: • Ovulation inducing agent. Clomiphene • Completely excreted through biliary excretion by any route of administration Quaternary • Completely ionized and not reabsorbed ammonium • Excreted through biliary excretion compounds Rifamycin & • (50% - 100%) of dose excreted in bile stilbsterol ❑ Storage in gall bladder: • Drugs may store in gall bladder then release to small intestine. Why the second peaks appear? • Co inside with food intake due to storage of drug in gall bladder and after meal, contraction of gall bladder release bile salt. • Ex. Diazepam – digitalis. ❑ Physical factors affecting biliary excretion: • Fat soluble substances of high M.wt expected to excrete through bile rather than in urine. • Minimum M.wt required for biliary excretion of cations differs from anion which demonstrates different mechanism. Molecular weight • Drugs with M.wt 500 will excrete in bile. • Drugs with M.wt (300 – 400) excreted in both urine and bile. • Drugs with M.wt less than 300 excreted in the urine Polarity • Strongly polar groups fond to be responsible for biliary excretion Structural factors of no. of sulfonamides in the rats demonstrated their effect by one of the following factors: Molecular a. Changing lipid solubility. Structure b. Shape of molecules. c. Intramolecular relationship of polar or non-polar part of molecule. D. SALIVARY EXCRETION • Depend on PH partition theory. • Saliva acts as lipoid membrane allow passage lipid soluble substances only. • Allow lipid soluble compounds to move from plasma to saliva. • PH of saliva (5.5 – 8.5). ❑ Excretion in saliva may be: • Active: if conc. of drug in saliva > conc. in blood so transfer against conc. ingredient from low conc. (blood) to high conc. (saliva) by active secretion. • Passive: if conc. of drug in blood < conc. in saliva so transfer with conc. ingredient from high conc. (blood) to low conc. (saliva) by passive excretion. ✓ Actively secreted in saliva. Lithium ✓ Its conc. in saliva 2- 3 times more than in blood Penicillin ✓ Actively secreted in saliva. & ✓ There is a competition between them for excretion through saliva so long Probenecid half-life of penicillin ❑ Examples of drug excreted in saliva: 1) Sulfonamides 2) Phenobarbital 3) Phenytoin 4) 5) 6) 7) Salicylates Theophylline Quinidine Digoxin ❑ Side effects: ➢ Excretion through saliva may cause localized side effects such as: a. Certain antibiotics excretion of certain antibiotics from blood to saliva gives black hairy tongue b. Phenytoin Excretion through saliva cause gingival hyperplasia. E. MAMARY EXCRETION ✓ Excretion through breast milk. ✓ Depend on PH partition theory. ✓ PH of breast milk (6.8 – 7.3). ✓ In normal conditions: ▪ Conc. of weakly acidic drugs in milk is lower than in blood. ▪ Conc. of weakly basic drugs in milk is equal or more than in blood. ✓ Ethanol and tetracycline have low molecular weight so it diffuses through membranes pores so conc. at plasma and milk may equal F. SKIN EXCRETION ✓ Drugs excreted through skin into sweat ✓ PH of skin (5 – 5.5) acidic act as a protective mechanism so prevent growth of M.O. ✓ Concerned mainly with acidic drugs. ✓ We can identify if the substance excreted from skin by taking a skin swap. Examples of drugs excreted through skin: • Br2 – I2 - Salicylic acid – benzoic acid. • Alcohols – iron – lead. • Anti-purine. G. GIT EXCRETION • Basic drugs can be excreted to GIT after IV administration • Ex. Nicotine – quinine • In stomach: highly ionized, low lipid soluble, so not reabsorbed and excreted. • In intestine: highly unionized so reabsorbed H. PULMONARY EXCRETION • Volatile & gases excreted through lung. • Drug released through expired air. Examples: • Ether: used in general anesthesia. • Paraldehyde: used as sleep inducing agent. Breath test for drinking drivers: • Breath is received on sheet of paper (TLC) treated with material sensitive to alcohol. • If breath contains alcohol, color of sheet will change. Bioavailability Studying ❑ Drugs not required in vivo bioavailability:امتحاااااان اقسم باهلل 1- Intravenous solutions → as there is no absorption phase 2- Topically applied drugs but transdermal drugs require in vivo bioavailability مهم جدااااااااااا 3- Substances not intended to be absorbed as antacids, antidiarrheal and diagnostic drugs such as radio-opaque media. 4- Drugs administered by inhalation as asthmatic attack drugs 5- Oral solutions as elixirs, syrup and tincture مهم جدااااا ❑ Oral dosage forms: Advantages 1. Patient acceptability. 2. Large surface area in small intestine which Disadvantages 1- Variabilities affecting absorption: • pH → stomach is acidic while intestine is cause high absorption. 3. Rich of blood supply so increase absorption. 4. Can be formulated as Sustained release formulation as it is simply increase absorption so we may decrease the dose. 5. Zero order-controlled release which prevents formulation of peaks & troughs so reduce the dose frequency and avoid fluctuations. 6. Commercial cost in comparison to parenterals. 23456- alkaline. • Presence of food • Difference in Gastric emptying rate • Body posture. • Drug interaction. • Pathologic conditions. • Gender variance (Male and Female) • Race difference • Disease state Adverse reactions as irritant drugs that can damage mucosa First pass effect and metabolic activity Enzymatic reactions and secretions of GIT Effect of extreme acidic pH → acid labile drugs degraded by acidity of stomach. Difference in intestinal motility (hyper and hypo motility) ❑ Factors affecting drug Half-Life: 1- Age: ➢ In elderly people, decrease liver function so increase half-life of drug ➢ In infants, Enzyme system not completed so increase half-life 2- Species difference: ➢ Biotransformation is: Slow in human and rapid in animals so this increase half-life in human and decrease half-life in animals. 3- Physiological properties: ➢ Change in PH which may cause changing in plasma protein binding. 4- Pathological properties: ➢ Kidney and liver disease affect execration and half-life 5- Tissue localization: ➢ Affinity of drug to be in tissue 6- Protein binding ❑ Factors affecting dosing of drugs to elderly: 1. 2. 3. 4. 5. 6. 7. Physiologic condition. Increasing of fatty tissue and decreasing of metabolic process. Fat soluble drugs may alter Vd. Free drug increased due to reduced drug protein binding. Perfusion of drug to GIT region decreased and drug absorption affected. Sensitivity of liver and kidney. Receptor Sensitivity or response to drug may be modified Experimental methods to study GIT absorption A. In Vitro (Everted Sacs) ❑ Advantages: • Not consumed many animals • Simple for screening • Distinguish between active and passive absorption. ❑ Disadvantages: • Non-physiologic as no blood vessels. • Permeability may be changed outside the body. ❑ Steps: ▪ 1. 2. 3. 4. 5. A rat is anesthetized with pentobarbal. A midline abdominal incision is made. The small intestine with a length of 10- 15 cm is rapidly removed and everted with a glass rod. The sac is securely ligated at both ends and filled with bicarbonate buffer solution. The sac is incubated at 37°C in a glass vessel containing the same buffer solution and gassed with 95% O2 /5% CO2 6. After 5 min, the drug solution is added to the glass vessel and the preparation is further incubated. 7. After given time intervals, the fluid from the everted sac is removed and the volume determined. 8. The concentration of the drug transported from the mucosal to the serosal side is determined by appropriate analytical methods. Used to compare between the 2 results and determine if the 2 drugs are significant and bioequivalent or not Important practical problem Following I.V administration of a dose of 1.5 mg of digoxin dissolved in diluted alcohol to a patient with congestive heart failure. The following urinary excretion data were obtained: Time (day) 0-1 1-2 2-3 3-5 B. In Situ a) Perfusion technique. b) Loop technique. انظر للشرح العربى فى المحاضرة C. In Vitro ❑ Criteria for in vivo bioavailability tests: • It should be designed to reduce as many possible sources of variation. Urine Conc. (µg/ml) 0.01386 0.00815 0.0050 0.0033 Determine a. T1/2 graphically b. Overall elimination rate constant (KE) c. Urinary excretion rate constant (Ke) d. biotransformation excretion rate constant (Kb) e. Percentage of Ke & Kb f. T1/2 in patient suffering from anuria g. T1/2 in patient with 40% reduction in biotransformation ❑ Factors that reduce variation: A. Subject to subject variation (intersubject variation( : ▪ Normal healthy volunteers ▪ Age should be 20 – 50 years ▪ Body weight between 55 – 90 Kg ▪ Experimental must be done on healthy volunteers. ▪ Numbers of males and females must indicate. ▪ Normal body fluid (urine – blood sample) B. Cross over study: ▪ Individuals or volunteers divided into 2 groups then Group A take drug A and group B take drug B. ▪ Wait wash out period to be sure that complete elimination of drugs from body ▪ Then each group receive dose of other group (Group A take drug B and Group B take drug A ❖ Wash out period امتحان: ▪ It is the time which allowed all dose to be execrated from body ▪ At least 10 times of half-lives of drugs. C. Bioavailability study conditions: ➢ Condition must be identical before and after administration of tested drug for the 2 groups of volunteers: a. Time before studying. b. Period of fasting before and after administration. c. Type of food & drink must be controlled. d. Degree of physical activity must be identical as physical activity increase absorption and bioavailability D. Frequency and duration of taking blood samples: ▪ We must take at least 3 points for each phase to draw bioavailability curve. ▪ Blood level curve must define absorption and elimination phase. ▪ Blood samples should be continued until (87 – 95 %) of drug eliminated or until ▪ plasma drug level decreased to (5 – 10 %) of peak conc E. Assay procedures: ▪ Blood sample should be stored and treated under the same condition. ▪ It is better to assay drug by 2 different methods such as: ✓ HPLC. ✓ Spectrophotometry. ✓ Radio-immunoassay F. Statistical analysis of blood level: Urine volume (ml) 1000 1200 1400 2520 urinary excretion rate after midpoint = Urine volume × urine conc time interval 100 Mid-point Urinary exec. Rate after mid-point (1000 × 0.01386)/1 = 13.86 (1000 ×0.00815)/1= 9.78 (1000 ×0.0050)/1= 7 (1000 ×0.0033)/2= 4.2 (0+1)/2 =0.5 (1+2)/2 =1.5 (2+3)/2 = 2.5 (3+5)/2 =4 10 1 0 1 2 3 4 5 a. Half-life = 2.1 day b. K E = c. K e = 0.693 T1/2 = 0.693 2.1 Y−intercept dose = 0.341 𝑑𝑎𝑦 −1 16 = 1500 = 0.011 day −1 مهم d. KE=Ke + Kb → Kb= KE-Ke = 0.341 – 0.011 = 0.33 day −1 ke 0.011 e. % Ke = K × 100 = 0.341 × 100 = 3.2 % E Kb 0.33 f. % K b = K × 100 = 0.341 × 100 = 96.8 % E g. In case of anuria→ no urine → Ke= zero KE=Ke + Kb = 0 + 0.33 = 0.33 day −1 T1/2 = 0.693 KE = 0.693 0.33 = 2.1 day h. Kb (remain) = 60% So, KE = Ke + Kb KE = Ke + (0.6× Kb) = 0.011 + (0.6× 0.33) → KE = 0.209 day −1 T 1/2 = 0.693 / 0.209 = 3.31 day ❑ Modification to increase bioavailability: A. Mucoadhesive drug delivery: • Hydrophilic polymer that interact with mucosal membrane forming H-bond with mucosal membrane. • It enhances absorption by prolonging the residence time, increase local conc. in the absorption region and protect drug from degradation by gastrointestinal fluids. Solutions Suspensions A. Social drugs: • Coffee and Tea stimulate the acid production in the stomach so gastric emptying initially increases then followed by reduction as Ergotamine and nitrofurantoin by increasing rate and extent of absorption. • Caffeine increases Plasma concentration of epinephrine and norepinephrine and increases blood flow. • Tobacco and nicotine stimulate salivation and decrease blood flow to mucosa • Caffeine: • Ethanol decrease gastric emptying rate and increase acid secretion and blood flow so increase bioavailability of chloralhydrate and chlordiazepoxide, meprobamate. B. Body posture: Effect of superior position (lying on back): • Decreases rate and extent of absorption on sodium salicylate. • Decreases rate of absorption of aspirin without affecting extent of absorption. Determination of bioavailability of drugs 1) Direct method: 2) Indirect method: • Blood data • Acute pharmacologic effect • Urine data • Clinical response A. Acute pharmacologic effect: • Used in case of quantitative measure is not available or there is no sufficient accuracy in analysis or drug may be potent. • We determine the AUC after 3 half-lives of drugs • Examples: ✓ Heart rate ✓ Blood pressure ✓ Pupil diameter B. Clinical response: • Used if drug is: 1. Unavailable, this cause lack of response. 2. Reasonally available, cause good response. 3. Highly available, cause toxicity. • Disadvantages: • Require high number of volunteers. • Inter subject variation is high. Dosage form factors affecting GIT absorption • May affect bioavailability due to forming of poorly soluble non-absorbable complex Excipients Examples: ✓ Phenobarbital + PEG. ✓ Tetracycline + Ca+2 • May affect bioavailability Phenytoin (antiepileptic drug): Diluent ✓ Calcium sulfate dehydrate diluent, decrease absorption of phenytoin. ✓ Calcium sulfate dehydrate changed to lactose which is highly soluble in water so cause overdose of drug leading to toxicity • Affect biological membrane so affect permeability and affect absorption Surfactant • If present in form of monomer, it causes disruption to the intermolecular structure of lipid and Soft gelatin capsule ❑ Other factors affecting bioavailability: cause changing of permeability and decrease integrity. • Increasing conc. Above CMC will decrease bioavailability and absorption. • If increase viscosity, GER decreased, GIT motility decreased, dissolution rate decreased and diffusion of drug decreased so affect absorption of drug. • Increasing viscosity may increase absorption in case of acidic drugs because of decreasing GER may permit the long contact of these drugs with the stomach leading to increasing Viscosity absorption any bioavailability Examples: ✓ Phenobarbital sodium + sucrose, increase viscosity so cause decrease of absorption ✓ Na salicylate +methyl cellulose, increase viscosity so cause decrease of absorption ✓ Na salicylate + gum solution, increase viscosity so cause decrease of absorption The Influence of the Dosage Form on the Bioavailability of Drugs • The absorption of drugs from solution dosage forms (syrups) is a fast & complete process, where the drug will be available in a soluble form ready for direct absorption, it doesn’t need to be broken or disintegrated first, because it is already available in a direct liquid form • bioavailability of solution may be affected by: ✓ Chemical stability of drug in solution. ✓ Occurrence of a Complexation reaction. ✓ Solubilization or micellization ✓ Viscosity of solution • Bioavailability of suspensions may be affected by: ✓ Particle size of drug as the reduction of the drug particle size will increase the effective surface area & enhance the dissolution rate & the absorption rate of the drug. ✓ Crystal form (amorphous or crystalline) ✓ Complexation between excipients. ✓ Inclusion of surfactant, surfactants are added as wetting agents to suspensions to enhance the wettability of hydrophobic drugs and may give a deflocculated or flocculated suspension • These are soft or elastic gelatin shells encapsulating a drug which is dissolved, dispersed or suspended in a non-aqueous vehicle or solvent, because aqueous solvent will dissolve gelatin shell • Bioavailability of soft gelatin capsules may be affected by: ✓ The solubility of the drug in the vehicle which will control the release of that drug from that vehicle. ✓ The particle size of the drug if formulated as a suspension in the vehicle ✓ The addition of wetting agents to the formulation. ✓ Complexation reaction. ✓ Crystal form • Bioavailability of tablets may be affected by: a. All physio-chemical properties of the drug b. Diluents c. Binders d. Disintegrants e. Lubricants f. Compression or compaction pressure applied g. Method of tablet manufacturing employed h. Storage Tablet and coated tablet B. Lipidization strategies: • Oral absorption of peptides and proteins (hydrophilic) increased 140 times by addition of palmitic acid with protease inhibitor C. Natural transport system: • Competition such as uracil and 5-fluorouracil. • L – Methyl dopa is actively absorbed 7 times more than passively absorption. • Formation of L-valyl ester pro-drug of acyclovir increase absorption D. Co-administration of drugs which help in increasing absorption: • Surfactants, Bile salts & chelating agents دُمتم ساملني