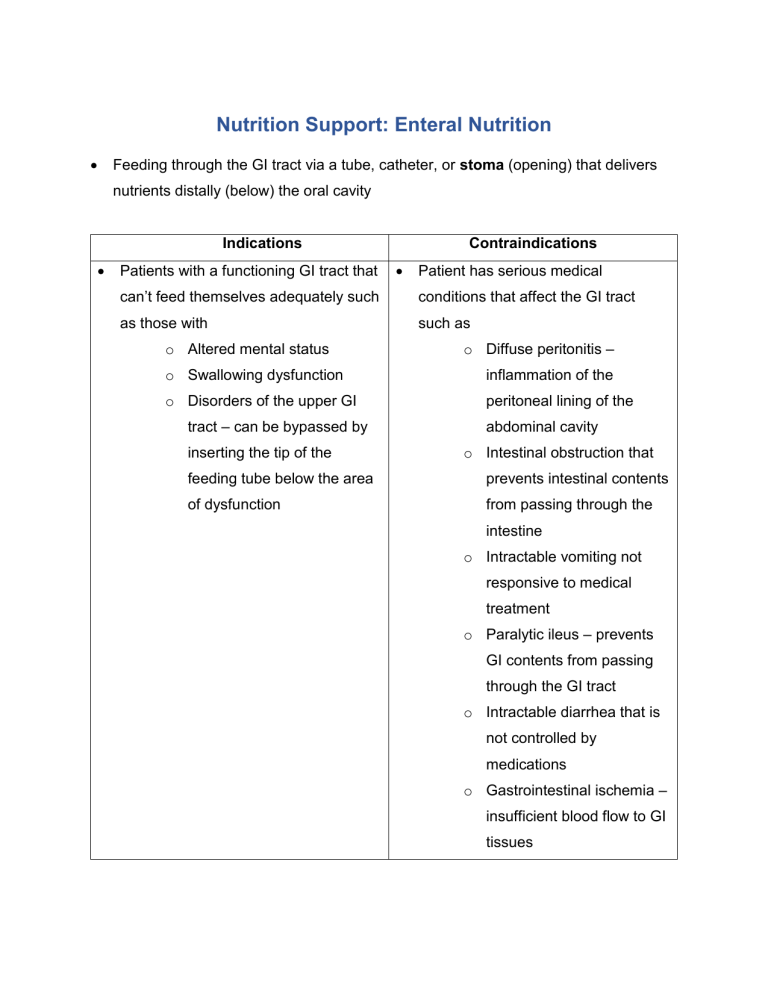
Nutrition Support: Enteral Nutrition Feeding through the GI tract via a tube, catheter, or stoma (opening) that delivers nutrients distally (below) the oral cavity Indications Patients with a functioning GI tract that Contraindications Patient has serious medical can’t feed themselves adequately such conditions that affect the GI tract as those with such as o Altered mental status o Diffuse peritonitis – o Swallowing dysfunction inflammation of the o Disorders of the upper GI peritoneal lining of the tract – can be bypassed by inserting the tip of the abdominal cavity o Intestinal obstruction that feeding tube below the area prevents intestinal contents of dysfunction from passing through the intestine o Intractable vomiting not responsive to medical treatment o Paralytic ileus – prevents GI contents from passing through the GI tract o Intractable diarrhea that is not controlled by medications o Gastrointestinal ischemia – insufficient blood flow to GI tissues Advantages Cost effective Reduced rate of infections in critically ill patients Improved wound healing Reduced surgical intervention Maintenance of GI tract functions Disadvantages Difficult to administer Poor tolerance Difficulty of meeting nutritional requirements of some patients Discomfort of the patient GI Access 1. Nasogastric Feeding tube A tube that is inserted through the nose into the stomach o Most common o Easiest to achieve o Easiest to maintain o Least expensive o Can be used in various conditions Disadvantages: o Can be easily dislodged o May need to be replaced frequently 2. Orogastric Feeding tube o Tube that is inserted through the mouth to the stomach 3. Nasointestinal Feeding tube o Tube that is inserted through the nose into the intestine bypassing the stomach to reside in the duodenum or jejunum used in cases of Gastroparesis – delayed gastric emptying Gastric outlet obstruction Previous gastric surgery preventing feeding into the stomach o Minimizes risk of accidental aspiration of formula into lungs Tubes entering through the nose or mouth are used for short term therapy (<6 weeks) More permanent feeding tube methods 4. Gastrostomy o Tube delivering feeds to the stomach 5. Jejunostomy o Tube delivering feeds through the abdominal wall into the jejunum Both methods involve placement of the tube by the following procedures: Surgical Gastrostomy o Physician places permanent feeding tubes when the patient is sedated Percutaneous Gastrostomy o Feeding tubes placed through the skin without a surgical incision Percutaneous Endoscopic Gastrostomy (PEG) o Inserting a feeding tube through the skin into the stomach using an endoscope Formulas Depends on where the tip of the tube is and on osmolality – number of water attracting particles per kg. 1. Protein Derived from soy or casein Most formulas require enzymes to split intact proteins into peptides before absorption – standard formulas Some contain proteins from peptides used in patients with enzyme deficiency or other conditions resulting in maldigestion – elemental or hydrolyzed formulas Specialized amino acid formulas – elemental formulas - are used for o Renal failure o Hepatic failure o Stress o Inborn errors of metabolism 2. CHO Large molecules (monosaccharides, oligosaccharides, dextrin, maltodextrins) Most have insoluble fibres (i.e. soy polysaccharides) o Less hydrophilic Some have soluble fibre added to improve bowel functions o Only small amounts as these formulas are hydrophilic – attracts water Causes formula to thicken and form a gel when added 3. Lipids Derived from corn and soy oil – long and medium chain fatty acids 4. Vitamins/Minerals Most provide DRIs for vitamins and minerals for adults within a specified volume (i.e. 1500 mL in 24 hours) 5. Fluid/Nutrient Density Some patients are unable to tolerate large volumes of fluid as they have impaired functions o Cardiac o Renal o Pulmonary Nutrient density determined by kcal/mL o Standard is 1 kcal/mL EN may be the sole source of fluid intake – monitor patient’s ins and outs to check for dehydration Precise water content of formulas are determined by the free water content o 80% water for 1 kcal/mL o 65 % water for 2 kcal/mL Partially hydrolyzed formulas have higher Osmolality o Number of water attracting particles per weight of water in kgs (mOsm/kg) Iso-osmolar – formulas that have the same osmolality of body fluids (300 mOsm/kg) o Was used to minimize the effects of dumping syndrome – diarrhea resulting from rapid movement of fluids into the GI tract to dilute hyperosmolar or concentrated fluids Typically most formulas have moderate osmolality (300 – 600 mOsm/kg) Feeding Techniques 1. Bolus Feeds Rapid administration of 250 – 500 mL of formula several times daily using a syringe 2. Intermittent Feeds Administered several times daily over 20 – 30 minutes Typically requires a pump to control flow rate or can use gravity feeds if container is suspended above the patient 3. Continuous Feeds Administered over 10 – 24 hours daily using a pump to control feeding rate preferred method in hospitals or nursing homes o May improve tolerance Can be restrictive on mobility Most polymeric, isotonic formulas can be initiated at 10 – 40mL/ hour - Rate is advanced in increments of 10 – 25mL/ hour every 4 - 8 hours until goal rate is reached Complications Mechanical Clogged, twisted or kinked tubes – flush with water Gastrointestinal most common is diarrhea o abnormal looseness of stool with increased liquidity or decreased consistency o output > 200 g/day for adults and 20 kg/day for children can be caused by medications – antibiotics containing sorbitol also due to infections by bacteria or viruses Aspiration fluid is inspired into the lungs common in patients who are o sedated o have endotracheal tubes – tube allowing oxygen into the lungs of patients receiving mechanical ventilation o have swallowing difficulties - elevate patient’s head about 45 during feeding - determine GI emptying by calculating residual volumes of liquid in stomach o stop EN if residual > 400 mL Tube Feeding Syndrome hyperosmolar-nonketotic dehydration over a short 2 to 4 day period caused by insufficient fluid intake in patients with EN Electrolyte Imbalances patients with organ failure require lower levels of electrolytes IV supplementation of electrolytes are preferred Underfeeding Delays nutritional repletion and wound healing May assist in preventing acute and respiratory complications in some patients Overfeeding Ureagenesis o Inability to clear by-products of protein breakdown resulting in toxicity Hyperglycemia o Impaired wound healing Hypertriglyceridemia Hepatic Steatosis – fatty liver o Due to an increase of liver enzymes that promotes increased storage of fatty acids o Congestion of the reticular endothelial system – increased serum tryglycerides Prolonged mechanical ventilation o Increased CO2 production due to increased metabolism of CHO Refeeding Syndrome Metabolic alterations that occur during the nutritional repletion of starved patients o In starved patients, major energy source is from fatty acids used to produce ketones resulting in decreased BMR Reintroduction of CHO results in shift of energy source from ketones to glucose Glucose requires large quantities of phosphorus to be metabolized o Magnesium, potassium and thiamin needs may increase as well Serum phosphate decreases (hypophosphatemia) resulting in o Hemolysis o Impaired cardiac function o Impaired respiratory function o Death Serum potassium decreases (hypokalemia) resulting in o Cardiac abnormalities Serum magnesium decreases (hypomagnesemia) results in o Tremors o Twitching muscles o Cardiac arrythmias o Paralysis Patients at highest risk are: Malnourished Have a history of long-term inadequate oral intake Have had minimal intake for several day Parenteral Nutrition Administration of nutrition directly into the circulatory system via IV – intravenously Central Parenteral Nutrition Administration of concentrated macronutrients, vitamins, minerals and electrolytes into a large central vein so that the volume of blood flow is sufficient to immediately dilute the concentrated PN solution Peripheral Parenteral Nutrition Administration of large volumes of dilute solutions of nutrients into a vein in the arm or the back of the hand Usually used for short-term Indications: Patient unable to meet needs by EN or oral intake Inability to digest and absorb nutrients – malabsorption o Massive bowel resection o Short bowel syndrome o Intractable vomiting o GI tract obstruction o Impaired GI motility o Abdominal trauma, injury or infection Venous Access Short Term: 1. Central Venous Catheter o IV access inserted into large veins at the centre of the body such as the Subclavian Jugular Femoral veins 2. Peripherally inserted central catheter (PICC) o IV access inserted into the arm and threaded into a subclavian vein to the vena cava o Threaded from smaller veins to larger veins o Inserted bedside – doesn’t need surgical placement Long Term 1. Tunneled Catheters o IV access placed in a vein on the upper chest wall and exits the body near the xyphoid process, axilla or abdominal wall o Surgically inserted directly into the superior vena cava o Better suited for long-term support Patient can use both hands to access it Less chance of displacement as it is sutured in place 2. Implantable Ports o IV access that is completely under the skin o Placed in the vein on the upper chest wall and exits the body near the xyphoid process, axilla or abdominal wall