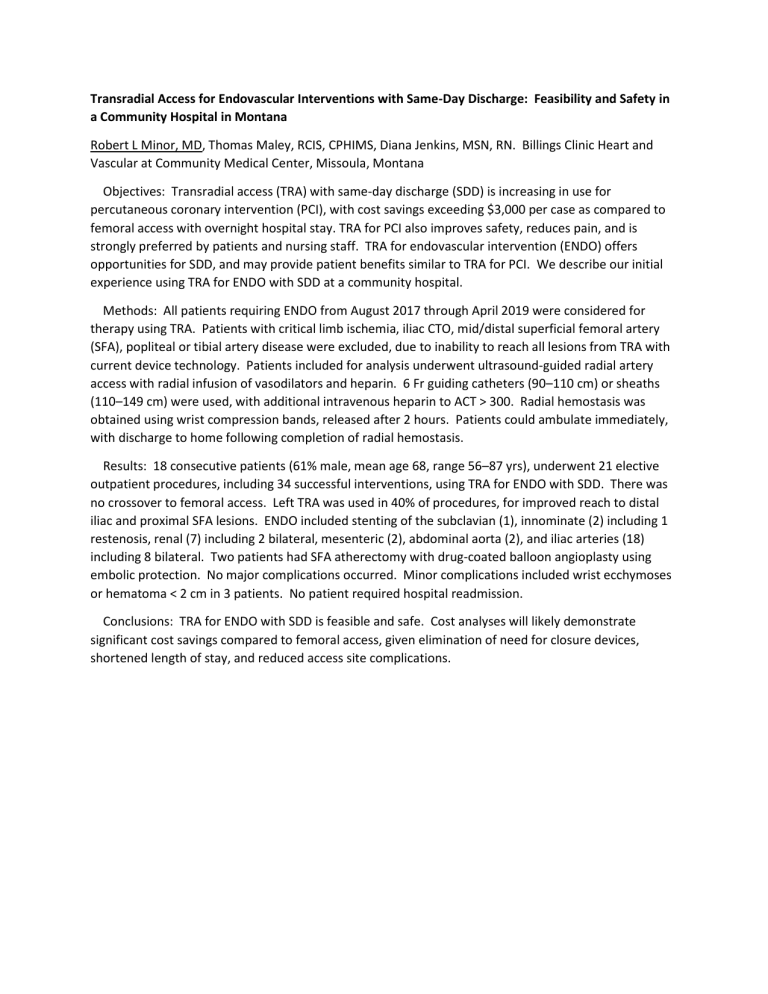
Transradial Access for Endovascular Interventions with Same-Day Discharge: Feasibility and Safety in a Community Hospital in Montana Robert L Minor, MD, Thomas Maley, RCIS, CPHIMS, Diana Jenkins, MSN, RN. Billings Clinic Heart and Vascular at Community Medical Center, Missoula, Montana Objectives: Transradial access (TRA) with same-day discharge (SDD) is increasing in use for percutaneous coronary intervention (PCI), with cost savings exceeding $3,000 per case as compared to femoral access with overnight hospital stay. TRA for PCI also improves safety, reduces pain, and is strongly preferred by patients and nursing staff. TRA for endovascular intervention (ENDO) offers opportunities for SDD, and may provide patient benefits similar to TRA for PCI. We describe our initial experience using TRA for ENDO with SDD at a community hospital. Methods: All patients requiring ENDO from August 2017 through April 2019 were considered for therapy using TRA. Patients with critical limb ischemia, iliac CTO, mid/distal superficial femoral artery (SFA), popliteal or tibial artery disease were excluded, due to inability to reach all lesions from TRA with current device technology. Patients included for analysis underwent ultrasound-guided radial artery access with radial infusion of vasodilators and heparin. 6 Fr guiding catheters (90–110 cm) or sheaths (110–149 cm) were used, with additional intravenous heparin to ACT > 300. Radial hemostasis was obtained using wrist compression bands, released after 2 hours. Patients could ambulate immediately, with discharge to home following completion of radial hemostasis. Results: 18 consecutive patients (61% male, mean age 68, range 56–87 yrs), underwent 21 elective outpatient procedures, including 34 successful interventions, using TRA for ENDO with SDD. There was no crossover to femoral access. Left TRA was used in 40% of procedures, for improved reach to distal iliac and proximal SFA lesions. ENDO included stenting of the subclavian (1), innominate (2) including 1 restenosis, renal (7) including 2 bilateral, mesenteric (2), abdominal aorta (2), and iliac arteries (18) including 8 bilateral. Two patients had SFA atherectomy with drug-coated balloon angioplasty using embolic protection. No major complications occurred. Minor complications included wrist ecchymoses or hematoma < 2 cm in 3 patients. No patient required hospital readmission. Conclusions: TRA for ENDO with SDD is feasible and safe. Cost analyses will likely demonstrate significant cost savings compared to femoral access, given elimination of need for closure devices, shortened length of stay, and reduced access site complications.