![Paper EGQ english 4 [690]](http://s3.studylib.net/store/data/025277462_1-5e52cfaadeaa775c8d468bbb6421d2e4-768x994.png)
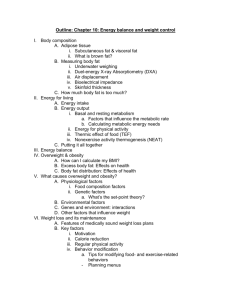
1. PÁGINA DE TÍTULO 1. Título do artigo: INTER-RELAÇÃO DE OBESIDADE VISCERAL, OBESIDADE GLÚTEO-FEMORAL E DOENÇA PERIODONTAL EM MULHERES 2. Autor / Co-autores: Prof. Dra. Dóris Hissako Sumida (Prof. Titular da Faculdade de Odontologia de Araçatuba-SP – FOA-UNESP); Prof. Dr. Fernando Shiba (Prof. Colaborador do Programa de Pós Graduação Multicêntrico em Ciências Fisiológicas – FOA-UNESP). 3. Angelo César |Fernandes Jacomossi – Médico Endocrinologista – Pósgraduando (mestrado) do Programa de Pós Graduação Multicêntrico em Ciências Fisiológicas – FOA-UNESP) – Endereço para correspondência: Rua Antônio Afonso de Toledo, 874 CEP: 16015-270 Araçatuba-SP – jacomed@hotmail.com - (18)997112702 / Fone/Fax(18)36223504. 4. Título abreviado: Inter-relação de Obesidade e Periodontite 5. Palavras-chave: visceral obesity; gluteofemoral obesity; intra-abdominal fat; periodontal diseases; periodontitis 6. Número de palavras: 2911 7. Tipo de Manuscrito: artigo original !1 ABSTRACT Objectives: To evaluate the severity of Periodontal Disease (PD) in obese women from the same community considering the distribution of body fat. Materials and Methods: 39 women were evaluated, 15 with visceral obesity (VOb), 10 with gluteofemoral obesity (GFOb) and 14 with normal weight (C). All were submitted to periodontal evaluation and scored according to the Community Periodontal Index (CPI). Anthropometric measurements and bioimpedanciometry were performed in order to discriminate the regionalization of body fat. A collect of blood sample was made for fasting dosage of glycemia and insulinemia for calculation of HOMA-IR determination and laboratory quantification of insulin resistance. The three groups were compared in relation to the severity of PD. Correlation analyzes were performed between CPI and the following parameters: Body Mass Index (BMI), waist circumference (WC), waist / hip circumference ratio (C / Q), percentage of visceral fat in relation to body weight (% GV) and HOMA-IR. Results: The mean CPI score was significantly higher (p = 0.0045) in the ObV group than in the C group. There was no difference in the GFOb group when compared to the VOb group and the C group. There was a significant positive correlation between the CPI score (p = 0.0173), C / Q (p = 0.0004), and WC (p = 0.0082). Conclusion: the present study confirms previous literature data associating Obesity with PD, suggesting that such association may not occur in all obese individuals, but especially in those with accumulation of intra-abdominal fat. INTRODUTION There are some evidences associating Obesity and Periodontal Disease (PD) (1,2). The Obesity is characterized by fat body accumulation. The main parameter used to diagnose in adulthood is Body Mass Index (BMI), calculated by ratio between the squared height and the weight. Values equal or greater than 30kg/m² is considered condition diagnoses (3). DP consist in a conditions group affecting the dental support tissues: the gingiva, periodontal ligament, cementum and alveolar bone. It represents the result of persistent infection and inflammation in response to local pathogens (4). Both of them are considered chronic diseases, highly prevalent that course with systemic, persistent and low-grade inflammation (5,6). Obese individuals, as well as those affected by PD, show augmented circulating levels of inflammatory markers. Although the pathophysiological mechanisms responsible by the Obesity/PD association are not yet clear, it has been postulated a possible double way characterizing this interrelation. The abnormal fat tissue expanding is accompanied by increased pro-inflammatory cytokines secretion, notably the Tumoral Necrosis Factor (TNF-∝) and the Interleukin-6 (IL-6), by adipose cells !2 and infiltrates macrophages in the vascular-stroma. These cytokines can also stimulate the osteoclast cells differentiate through Receptor Activator of Nuclear Factor kappa-Β ligand (RANKL) expression, increasing the bone reabsorption. Furthermore TNF-∝ acts recruiting neutrophil polymorphonuclear cells (PMN) and intensifying the host immune response. Such phenomena contributing to the PD chronicity and progressivity (7,8). By the other hand the PD also represents an inflammatory mediators producer source, which can spread systemically and decrease the cellular response to insulin receptor stimulation, accentuating the insulin resistance, the cornerstone of the Metabolic Syndrome (MS) diagnosis (9,10). Although the Obesity, in general, represents an increased risk to Cardiovascular Diseases (CVD) and others comorbidities, exist a group of fat people which must not be included in this scenario. Differently of the most of obese individuals, which show fat accumulation mainly in the intra-abdominal compartment, these individuals response to weight gain through subcutaneous fat tissue expansing, specially in the gluteofemoral area. They are individuals that, although they may have increased BMI, they do not develop CVD or metabolic complications frequently (11). The most of studies has sought to demonstrate the relationship between obesity, in general terms, and PD, without consider the regionalization of the fat deposit (12). In the present study we analyze both obese women with fat predominance in the intra-abdominal compartment and those with fat predominance in the gluteofemoral (subcutaneous) compartment regarding the risk of having PD or the PD severity. MATERIALS AND METHODS: A cross-sectional analysis was performed comparing 39 women between the ages of 20 and 40 years. Twenty-five were obese [Body Mass Index (BMI) ≥ 30 and <40 kg / m²] and fourteen had normal weight (BMI ≥ 18.5 and <25 kg / m²) which served as control group (C). All were users of the Unified Health System (SUS) of the municipality of Santo Antônio do Aracanguá-SP, Brazil, being regularly attended by the family health team and invited to participate in the study. Among the obese women, 15 had visceral obesity (VOb), according to the resulting value obtained by the ratio between waist circumference (WC) and hip circumference (cm) (W/H > 0,85), and 10 carriers of gluteofemoral obesity (GFOb) (W/H ≤ 0.85). The following exclusion criteria were obeyed: Diabetes mellitus (DM), smoking, alcoholism, illicit drug use, climacteric or postmenopausal status, plastic surgery in the hip, abdomen or chest region, oral contraceptive use and chronic inflammatory diseases. Blood sample for laboratory evaluation was collected within the first week of the menstrual cycle. All participants signed a free and informed consent form agreeing to participate in the research. The study was approved by the Ethics Committee of the Universidade Estadual Paulista - FOA/UNESP (CAAE: !3 72005317.5.0000.5420), in accordance with the criteria of Resolution 466 of the National Health Council on human research. The anthropometric evaluation was performed with the participants wearing light and barefoot clothing. Obesity was defined by a BMI (Weight in kilograms divided by the square of the height in meters) equal to or greater than 30 kg/m² (13). The weight was measured on an electronic scale (Filizola®), and the height was measured by a portable stadiometer. The body fat distribution was characterized by W/H ratio, measured by a tape measure. The WC measurement was made with the tape positioned comfortably in the midline, located between the last palpable rib and the apex of the iliac crest, in the orthostatic position, with the reading being recorded at the end of the expiration. The hip measurement was performed on the side of the person, who was standing with arms at the side of the body and feet together, placing the tape around the buttocks in a horizontal plane, at the level where the glutes reach their maximum amplitude. Measurements were taken after overnight fasting of at least eight hours in order to minimize the influence of gastric contents on WC measurement. Each calibration was repeated twice; when the difference between them was less than 1 cm, the mean was calculated. If the difference exceeded 1cm, the measurements were repeated (14). A blood sample was collected after a fasting period of 8 and 12 hours, and the glucose concentration was determined using automated technique. Insulinemia was measured by radioimmunoassay - RIA (Coat-a-Count insulin, Siemens Healthcare Diagnostics, Los Angeles, CA USA). HOMA-IR (Homeostatic Model Assessment) was calculated by the following formula: [Fasting Glucose (mmol / L) x Insulin fasting (µU / mL)] / [22.5], with a normal value lower than 2.71, and served to quantify resistance to insulin (15). The status of the periodontium was evaluated by the Community Periodontal Index (CPI) (16). A single examiner conducted the evaluations. The mouth was divided into sextants and six sites of each of the following teeth were evaluated: 17, 16, 11, 26, 27, 47, 46, 31, 36, 37. The highest code will be registered according to the following criteria: 0 (healthy), 1 (gingival bleeding after probing), 2 (presence of sub or supragingival calculus), 3 (periodontal pocket with 4-5 mm) and 4 (periodontal pocket with at least 6 mm). The study participants were classified as: healthy periodontium (PCI = 0), gingivitis (PCI = 1 or 2) or periodontitis (PCI = 3 or 4). Complementarily, all participants underwent a direct analysis of bioelectrical impedance (Z), with eight electrodes (tetrapolar) and two different frequencies (20kHz, 100kHz, InBody®120) in order to obtain a parameter representative of the amount of intra-abdominal fat (Visceral Fat percentage - VF%) and Total Body Fat percentage (TF%) (17,18). The normality of the data was verified using the Shapiro-Wilk test. The PCI, the periodontal condition of the sextants, the HOMAIR index, the age and the BMI were analyzed using the Kruskal-Wallis test, followed by the Dunn test for multiple comparisons. TF%, VF%, VF% / TF% ratio, !4 W/H ratio and WC were analyzed using the Variance Analysis, followed by the Tukey test for multiple comparisons. The Spearman correlation test was used to analyze the correlation between the CPI score and the following parameters: BMI, TF%, VF%, VF% / TF% ratio, HOMA-IR and W/H ratio. The level of significance was 5%. RESULTS No difference was observed in age. The BMI, WC, TF%, VF% and WC were significantly higher (p <0.05) in the groups GFOb and VOb compared to the control group (Table 1). There was also no difference in the VF% / TF% ratio among the groups. The VOb group had a significantly higher WC in relation to the GFOb group (p<0.05). The W/H ratio was significantly lower (p <0.05) in the control and GFOb groups when compared to the VOb group, but there was no difference between control and GFOb group in this parameter. There was no difference between BMI, TF% and VF% between the GFOb and VOb groups (Table 1). Table 1. Age, BMI, TF%, VF%, VF% / TF% ratio, W/H ratio and WC. Variáveis Controle GFOb VOb Age (years) 26.43 + 2.66 26.10 + 2.13 28.18 + 2.41 BMI (Kg/m²) 22.04 + 0.47 33.95 + 1.33 * 34.56 + 1.24 * TF% 33.44 + 1.53 47.57 + 1.29 * 44.81 + 1.40 * VF% 16.66 + 0.74 22.24 + 0.58 * 22.03 + 0.58 * VF% / TF% 0.49 + 0.01 0.46 + 0.01 0.49 + 0.01 W/H 0.73 + 0.03 0.79 + 0.01 0.95 + 0.01 *# WC (cm) 68.64 + 2.20 93.00 + 3.40 * 110.10 + 2.68*# * p <0.05 compared to the control group; #p <0.05 compared to the GFOb group The VOb group had a significantly higher HOMA-IR index (p = 0.0002) than the CG group. No difference was observed in the HOMA-IR index of the GFOb group in relation to the other groups (Figure 1). !5 ! Figure 1. Evaluation of the HOMA-IR index. Values are presented as average ± mean standard error. * p <0.05 compared to the control group. Patients in the VOb group had a significantly lower number (p = 0.0174) of healthy sextants compared to CG. A significantly higher number (p = 0.0162) of sextants with gingival bleeding in the ObV group was also observed in relation to the CG. The GFOb group showed no difference in these variables in relation to the other groups. There was no difference in the number of sextants with presence of dental calculus or periodontal pocket between groups (Table 2). Table 2. Mean number of sextants per patient according to the periodontal status assessed by the Community Periodontal Index. Periodontal Condition Control GFOb VOb Health Gingive 5.00 + 0.36 4.07 + 0.46 3.43 + 0.39 * Probing Bleeding 0.57 + 0.29 0.79 + 0.28 1.57 + 0.29 * Dental Calculus 0.43 + 0.20 1.14 + 0.33 0.79 + 0.24 Periodontal Pocket (4-5mm) 0.07 + 0.07 0.07 + 0.07 0.43 + 0.20 *p<0.05 compared to control group; values are shown as average ± mean standard error The mean PCI score was significantly higher (p = 0.0045) in the VOb group than in the control group. There was no difference in the GFOb group when compared to the other groups (Figure 2). !6 ! Figure 2. Evaluation of the periodontal condition by IPC. Values are presented as average ± mean standard error. * p <0.05 compared to the control group. There was a significant positive correlation between the PCI score and the VF% (p = 0.0300), HOMA-IR (p = 0.0173), W/H (p = 0.0004) and WC (p = 0.0082) (Table 3). Table 3. Analysis of the correlation between the CPI score and the BMI,TF%, vVF%, VF%/TF%, HOMA-IR, W/H and WC. Spearman Correlation Test (r) p-value BMI 0.26 0.15 % de total fat 0.22 0.23 % visceral fat 0.39 0.03* % de total fat / % de visceral fat 0.28 0.13 HOMA-IR 0.43 0.02* W/H 0.59 0.0004* WC 0.54 0.01* Variables *p<0,05 DISCUSSION The study showed that obese women, with predominance of intra-abdominal fat, have a higher PCI score compared to women of normal weight (C). Otherwise, the !7 obese women with gluteofemoral fat region did not present a significantly different score of PCI when compared to VOb women or to the control group.These results suggest that women afflicted with visceral obesity may have a worse oral health compared to lean women, belonging to the same age group and with similar living habits and socioeconomic conditions, since they come from the same community. Obese women, as a whole (GFOb and VOb), had the anthropometric measurements, BMI, WC and W/H, and two parameters extracted from bioimpedance (%TF and %VF), significantly different from those generated from the group of women with normal weight, demonstrating the greater corporal adiposity of these women in relation to the lean ones. There was no difference between the groups when analyzed by the biometric impedance parameter %VF / %TF ratio, representative of the proportion of visceral fat in relation to the amount of total body fat. It will be expected that these visceral obese individuals, presented this parameter increased when compared to individuals with normal weight or their peers with predominance of subcutaneous fat. However the real bioelectrical impedance acuracy to determine the amount of the visceral adipose tissue (VAT) has not yet been well established among different populations and ethnics groups. Browning and collaborators founded that the bioelectrical impedance analysis estimates were more highly correlated with total abdominal fat than VAT. (19). Some studies showed that it analyses better, or equivalently estimates, VAT amount compared to tape-measured waist circumference (20,21), but other studies found the opposite (22). Anyway WC is an index of central obesity recommended by the National Institutes of Health, World Healthy Organization, the American Heart Association, and the International Diabetes Foundation for screening for risk of metabolic and cardiovascular disease, due its value as a criterion for visceral obese definition (23). Large-population, multiethnic studies are needed to demonstrate whether abdominal bioelectrical impedance analysis is consistently superior to waist circumference to estimate VAT across populations. The VOb patients showed a higher HOMA-IR value than lean women, pointing to the presence of insulin resistance (IR) in women with visceral obesity. HOMA-IR has been used as an !8 important laboratory method to identify and quantify IR in several studies because of its positive and highly significant correlation with the clamp (24), the gold standard method for IR diagnosis (25). Although no statistically significant difference was observed between the two subgroups of obese women (VOb versus GFOb), the mean HOMA-IR value of the GFOb group did not differ from that of the control group, suggesting that there is a lower magnitude of IR in these women with subcutaneous obesity. Regarding the periodontal evaluation, we observed that the VOb patients presented a lower number of sextants with healthy gingiva and a greater number of sextants with bleeding at the probe. This finding suggests the existence of a negative influence of the degree of adiposity on periodontal health. There was also a significant difference between the VOb group and the control group regarding PCI, corroborating to the greater severity of PD in women with greater accumulation of fat than in women with normal weight. Likewise, no statistically significant difference was found between the two subgroups of obese women regarding this parameter, but the GFOb patients did not show a worse periodontal condition in relation to the control group and there was a tendency for PD condition to be less severe in women with GFOb compared to VOb women, reinforcing the hypothesis that the visceral fat accumulation may be more negatively associated to PD than the subcutaneous fat accumulation. Excessive production of inflammatory cytokines by visceral adipocytes, and by immune cells infiltrated into fatty tissue, may accentuate periodontitis (7,8). On the other hand it is known that the subcutaneous fat does not constitute a source producing proinflammatory cytokines. In fact, one of its secretory products is adiponectin, a hormone with anti-inflammatory actions and beneficial metabolic effects (26). The design of the present study does not allow to establish a causal relationship between the two diseases, much less if PD could aggravate the obesity and the IR. However, theoretically, because the inflamed periodontium is also a source of cytokines, the PD may accentuate the typical alterations of the Metabolic Syndrome (27), considering that these proinflammatory products reach all organs through the systemic circulation. TNF-α seems to play a central role in this !9 scenario. In addition to reducing the cellular response to insulin, directly limiting the metabolic effects of this hormone, this cytokine interferes with adipogenesis, decreasing expression of the transcription factor PPARγ (Peroxisome ProliferatorActivated Receptor Gamma) and protein C/EBPα (CCAAT/enhancer- binding protein alpha), essential elements for the recruitment of immature adipocytes and their differentiation into cells capable of storing lipids. The limitation of the storage capacity of adipose tissue favors the ectopic deposition of fat mainly in the liver, heart and pancreas, accentuating the metabolic alterations in Visceral Obesity (28,29,30). Vivekananda and collaborators conducted a study evaluating 60 obese subjects with a W/H ratio > 0.90 who underwent a weight reduction program, were able to observe a decrease in serum levels of TNF-α and an increase in adiponectin levels associated with a concomitant improvement in the clinical PD parameters (31). Prospectives interventions studies are needed to better clarify the pathophysiological aspects involved in the two diseases. When all the patients were analyzed together, the PCI was positively correlated with the percentage of visceral fat, HOMA-IR, W/H and waist circumference, strengthening the association of PD with anthropometric and laboratory parameters indicative of accumulation of visceral fat. There was no significant correlation of PD with BMI. Indeed, this parameter does not reflect the appropriate size of metabolic burden of fat in our body. In contrast, WC would mirror the metabolic burden of fat better than BMI (32), because it is a clinical marker of visceral fat accumulation. Few longitudinal studies have examined the interrelation of visceral obesity and PD. Three prospective observational studies found a temporal association between obesity and the subsequent development of PD. One of these studies considered body fat distribution rather than BMI as exposure, demonstrating that the 1% increase in W/ H ratio was associated with a 3% increase in the risk of developing periodontal ligament loss, alveolar bone loss, and probing pocket depth progression throughout the follow-up (33). Two intervention studies found that the response to noninvasive periodontal treatment was better among lean than obese, whereas three other studies did not find significant differences (34,35). Nevertheless, such studies !10 are heterogeneous, since different definitions and parameters are used by the authors, as well as periodontal evaluations, as those used to define the distribution of body fat. These issues are clinically extremely relevant since they deal with two diseases of high prevalence and socioeconomic impact. Health professionals should be attentive to this association and approach them concomitantly, reinforcing the necessity of the multiprofessional work in the evaluation and treatment of these individuals. In conclusion, the present study reforce previous data from the literature associating Obesity with PD, suggesting that such association may not occur in all obese, but mainly in those with accumulation of intra-abdominal fat. REFERENCES 1. D’Aiuto F, Sabbah W, Netuveli G et al. Association of the metabolic syndrome with severe periodontitis in a large U.S. population-based survey. J Clin Endocrinol Metab 2008 93: 3989–3994. 2.Fukui N, Shimazaki Y, Shinagawa T et al. Periodontal status and metabolic syndrome in middle-aged Japanese. J Periodontol 2012 83: 1363–1371. 3.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA 2013;309(1):71-82. 4.Centers for Disease Control and Prevention. Periodontal dis- ease. Available from: Available from http://www.cdc.gov/oral- health/periodontal_disease/. 5.Marcenes W, Kassebaum NJ, Bernabe E et al. Global burden of oral conditions in 1990-2010: a systematic analysis. J Dent Res 2013 92: 592–597. 6.Obesity: Preventing and managing the global epidemic. Report of a WHO consultation (WHO technical report series 894). Geneva, Switzerland: World Health Organization; 2000 7.Marchetti E, Monaco A, Procaccini L et al. Periodontal disease: the influence of metabolic syndrome. Nutr Metab (Lond) 2012 9: 88. 8.Bullon P, Morillo JM, Ramirez-Tortosa MC et al. Metabolic syndrome and periodontitis: is oxidative stress a common link? J Dent Res 2009 88: 503–518 9.Després JP, Lemieux I, Bergeron J, Pibarot P, Mathieu P, Larose E, Rodés-Cabau J, Bertrand OF, Poirier P. Abdominal obesity and the metabolic syndrome: contribution to global cardiometabolic risk. Arterioscler Thromb Vasc Biol 2008;28:1039-49. !11 10.Karolina J, Michal H, Marek B. Visceral fat and insulin resistance – what we know? Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2018; 162:XX. 11.Manolopoulos KN, Karpe F, Frayn KN. Gluteofemoral body fat as a determinant of metabolic health. Int J Obes (Lond). 2010; 34(6):949-59. 12.Lamster IB, Pagan M. Periodontal disease and the metabolic syndrome. Int Dent J. 2017; 67(2):67-77. 13.Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900.000 adults: collaborative analyses of 57 prospective studies. Prospective Study Collaboration. Lancet 2009;373(9669):1083-1096. 14.World Health Organization (WHO) Expert Committee. Physical status: the use and interpretation of anthropometry. Technical Report Series no. 854. WHO: Geneva, 1995. 15.Geloneze B, Rodovalho-Geloneze S, Parisi C, Pícolo M, Repetto EM Tambascia MA. Standardization of insulin tolerance test in Brazilian population. Diabetes Res Clin Pract. 2000;50(Suppl 1):S102. 16.Ministério da Saúde. Projeto SB2000 - Condições de Saúde Bucal da População Brasileira no ano 2000. A Doença Periodontal pg. 34-38. 17.Rodrigues MN, Silva SC, Monteiro WD, Farinatti PV. Estimativa da gordura corporal medinate equipamentos de bioimpedância, dobras cutâneas e pesagem hidrostática. Rev Bras Med Esporte 2001; 7(4):125-131. 18.Eickembrg M, Oliveira CC, Roriz AKC, Sampaio LR. Bioimpedância elétrica e sua aplicação em avaliação nutricional. Rev Nutr Campinas 2011; 24(6):883-893. 19.Browning LM, Mugridge O, Chatfield MD, et al. Validity of a new abdominal bioelectrical impedance device to measure abdominal and visceral fat: comparison with MRI. Obesity 2010; 18:2385 – 2391. 20.Park KS, Lee DH, Lee J, et al. Comparison between two methods of bioelectrical impedance analyses for accuracy in measuring abdominal visceral fat area. J Diabetes Complicat 2016; 30:343 – 349. 21.Berker D, Koparal S, Isik S, et al. Compatibility of different methods for the measurement of visceral fat in different body mass index strata. Diagn Interv Radiol 2010; 16:99 – 105. 22.Gomez-Ambrosi J, Gonzalez-Crespo I, Catalan V, et al. Clinical usefulness of abdominal bioimpedance (ViScan) in the determination of visceral fat and its application in the diagnosis and management of obesity and its comorbidities. Clin Nutr 2018; 37:580 – 589. 23.The IDF consensus worldwide definition of the Metabolic Syndrome. Internacional Diabetes Federation 2006. 24.Geloneze B, Tambascia M. Laboratory and diagnostic evaluation of insulin resistance. Atheros 2002; 13 (2): 42-49. 25.DeFronzo R, Tobin J, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol, 1979; 237: E214 E223. 26.Krause MP, Milne KJ, Hawke TJ. Adiponectin-Consideration for its Role in Skeletal Muscle Health. Int J Mol Sci. 2019 Mar 27;20(7). pii: E1528. !12 27.Koo HS, Hong SM. Prevalence and Risk Factors for Periodontitis Among Patients with Metabolic Syndrome. Metab Syndr Relat Disord. 2018; 16(7):375-38. 28.Byrne CD, Targher G. Ectopic fat, insulin resistance, and nonalcoholic fatty liver disease: implications for cardiovascular disease. Arterioscler Thromb Vasc Biol. 2014 Jun; 34(6):1155-61. 29.Lefterova MI, Lazar MA. New developments in adipogenesis. Trends Endocrinol Metab 2009; 20(3): 107–114. 30.Xu H, Sethi JK, Hotamisligil GS. Transmembrane tumor necrosis factor (TNF)-α inhibits adipocyte differentiation by selectively activating TNF receptor 1. J Biol Chem 1999; 274(37): 26287–26295. 31.Vivekananda L, Faizuddin M. Effect of Weight Reduction on the Serum Adiponectin and Tumor Necrosis Factor-α Levels and the Clinical Parameters of Obese Patients with and without Periodontal Disease. J Int Soc Prev Community Dent. 2019; 9(2): 166-171. 32.Rhee EJ. Being Metabolically Healthy, the Most Responsible Factor for Vascular Health Diabetes Metab J. 2018 Feb;42(1):19-25. 33.Gorman A, Kaye EK, Apovian C, Fung TT, Nunn M, Garcia RI. Overweight and obesity predict time to periodontal disease progression in men. J Clin Periodontol 2012; 39:107-114. 34.Lakkis D, Bissada NF, Saber A, et al. Response to periodontal therapy in patients who had weight loss after bariatric surgery and obese counterparts: a pilot study. J Periodontol 2012; 83:684-689. 35.Suvan J, Petrie A, Moles DR, et al. Body mass index as a predictive factor of periodontal therapy outcomes. J Dent Res 2014; 93:49-54. !13