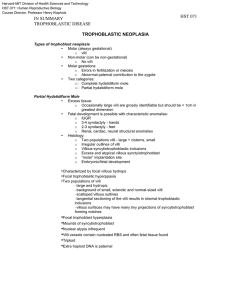
GESTATIONAL TROPHOBLASTIC DISEASES Presenter: Dr. Macharia (MBChB). For: Dr. Juma (Senior Consultant, OBGYN) • OUTLINE 1. Definition 2. Classification 3. Pathology and pathogenesis 4. Clinical features 5. Investigations and treatment options 6. Prognosis and the future introduction • Gestational trophoblastic disease refers to a spectrum of pregnancy-related trophoblastic proliferative abnormalities. • Zygote…morula….blastocyst……inner cell mass, outer cell mass (Trophoblast) syncitiotrophoblast... Cytotrophoblast classification 1.Pathological 2.Clinical classification Pathological 1. Hydatiform moles............................90% 2. Invasive mole....................................5% 3. Choriocarcinoma.............................2-3% 4. Placenta site trophoblastic disease....1% 5. Epitheloid trophoblastic tumour.......1% classification Clinical BENIGN 1. Hydatiform moles............................90% MALIGNANT 1. Invasive mole....................................5% 2. Choriocarcinoma.............................2-3% 3. Placenta site trophoblastic disease....1% 4. Epitheloid trophoblastic tumour.......1% • All these tumours arise from the trophoblastic cells • Exception PSTD arise from intermediate trophoblastic cells • Retain properties of the placenta • They all secrete Beta HCG important for diagnosis n follow up Hydatidiform mole • A pregnancy characterised by vesicular swelling of placenta villi and usually the absence of an intact fetus • Also called molar pregnancy • Etiology unclear...appears to result from abnormal gametogenesis and fertilisation • Can be complete or partial H. mole • Prevalence • Hydatidiform Mole is the commonest of these diseases. • 10* more in the east 1:5000 ppn • In Taiwan the incidence is 1:125 deliveries • USA 1:1500 deliveries • Kenya 1:370 deliveries. Home deliveries • The incidence of choriocarcinoma in Kenya is 1: 847 H mole... Risk factors. • Age <16 N >40yrs. • History of molar pregnancy • Certain HLA types, • A +O ....AB POOR PROGNOSIS. • Nutrional deficiencies: proteins, FolicAcid, Vitamin A • Multiparity • Low SES H mole TYPES • Complete . No embryo. Anucleate ovum. • Partial....discernible fetal parts ..usually triploid (69 chromosomes) • ASSIGNMENT list 5 differences between a partial and a complete mole Pathology • multiple grapelike vesicles filling and distending the uterus • There is edema of the villi stroma, avascular villi,nests of proliferating synciotrophoblast and cytotrophoblast elements surrounding the villi. • The likely hood of malignant transformation depends on degree of proliferation and anaplasia Molar pregnancy Clinical features • A period of amenorrhoea • 90% present with pv bleeding • 80% present with passage of vesicles • 14.3% present with hyperemesis • PET 10-12% • Hyperthyroidism 10% • Multiple ovarian cysts 15-30% • FH>DATES, absent Fetal parts on palpation Molar pregnancy Diagnostic tests • PDT. Positive in high dilution. • Beta HCG*10 of what is expected for gestation • FBC, LFTs,ESR • Radiography....honey comb appearance • CXR • Ultra sound: snow storm appearance H mole: management • Suction evacuation of the uterus under high dose syntocinon. 80% are curable after D&C • Hysterectomy if uncontrollable hemorrhage • GXM at the ready!!!!!!! • Follow up with serum b HCG 2/52 for 3/12 • Then monthly for 9 months. Some – 3 months for 1 more year. • GIVE OC…no AUBs H mole SEQUELAE • 25% invasive mole • 3-5% chorioca • 70% no change • COMPLICATIONS Haemorrhage, PET,HG CHORIOCARCINOMA • • • • highly malignant metastasises rapidly 50% follow Hmole 25% follow abotions 25% follow term pregnancy • BIOPSY IS Contraindicated. a) Highly vascularised b) Highly metastatic clinical features dx • As above POA • IN additional metastasis hemoptysis, icp, haemorhagic diasthesis, pv bleeding • Dx as above • RX M MAC, EMACO • Radiation • Combination • Surgery..hysterectomy if desired family size Invasive mole • A histological diagnosis.. after hysterectomy • Rx as chorioca PSTD • • • • • • 1% of GTDS From IT. Human placenta lactogen for diagnosis Metastasis. Less aggressive POOR response to chemo Definitive rx surgery summary GTDs are proliferative diseases of the trophoblasts With good Hx PE and Ix.. Clinicians can easily pick GTDs GTDs are very treatable upon establishing diagnosis Thank listening you for