Quantitative Analysis of
Redox Metabolism
Ling Liu
A DISSERTATION PRESENTED TO THE FACULTY OF
PRINCETON UNIVERSITY IN CANDIDACY FOR THE DEGREE
OF DOCTOR OF PHILOSOPHY
RECOMMENDED FOR ACCEPTANCE
BY THE DEPARTMENT OF CHEMISTRY
Advisor: Joshua D. Rabinowitz
January 2018
© Copyright by Ling Liu, 2018.
All rights reserved
Abstract
The redox cofactor nicotinamide adenine dinucleotide (NAD) plays a significant role in
metabolism and is a substrate for signaling enzymes including poly-ADP-ribose-polymerases
(PARPs) and sirtuins. NAD concentration falls during aging and in certain diseases, triggering
intense interest in strategies to boost NAD levels, most notably through nicotinamide riboside
(NR) and mononucleotide (NMN). A limitation in understanding NAD metabolism has been
reliance on steady-state concentration measurements. Here, we established methods for NAD
flux quantitation using stable isotope tracers combined with mathematical modeling. Cultured
cells took nicotinamide (NAM) as the predominant NAD source. We showed that mitochondria
directly import NAD and generate NAD from nicotinamide-containing nucleotides, but not from
NAM. In vivo, NAD was made from tryptophan selectively in liver, which then excreted NAM.
NAD fluxes varied widely across tissues, with high flux in small intestine and spleen and low
flux in skeletal muscle. We also showed that intravenous, but not oral administration of NR or
NMN delivered intact molecules to multiple tissues, with skeletal muscle displaying a preference
for NR. In cell lines, newly synthesized NAD was consumed largely by PARPs and sirtuins.
NAD kinase, which accounts for <10% of total NAD production, makes the anabolic and redox
defense cofactor NADP(H). We further developed the quantitative tracing method to measure
NADPH fluxes. While growing cells produce NADPH via the pentose phosphate pathway and
folate metabolism which also make nucleotide precursors, we found that in differentiating
adipocytes, a metabolic cycle involving malic enzyme make both NADPH and two-carbon units
for fat synthesis. This study enables dissection of the production and consumption routes of
redox cofactors across cells under different environmental conditions and murine tissues, and
thus provides a novel window into redox metabolism.
iii
Acknowledgement
First, I would like to sincerely thank my advisor, Prof. Joshua Rabinowitz, for his guidance
throughout my PhD study. He provided constructive insights, expert guidance and direction
when needed; taught me how to conduct experiments, how to communicate with audience during
presentation, and how to write a successful paper; endeavored to send me to meetings, make
connections with peers and extend collaborations; and encouraged me to be entrepreneurial and
explore my ideas. I appreciate his mentorship.
I also want to give thanks to my advisory committee, Prof. Tom Muir, Prof. Mohammad
Seyedsayamdost, Prof. Dorothea Fiedler, and Prof. Joseph Baur, who had given me important
suggestions, especially during my first two years at Princeton.
My thesis work could not have been done without many wonderful collaborators. Prof. Joseph
Baur provided many key insights on the NAD biology and drove forward several projects
efficiently. Dr. David Frederick, Dr. Antonio Davila, Jr and Dr. William J. Quinn III from the
Baur lab collaborated with me on the NAD studies in muscle and mitochondria. Prof. Timothy
Mitchison led me to the NAD world; he provided consistent support since the project’s
conception in 2014. Prof. Eileen White had been supportive for in vivo studies. Dr. Le Zhan
from the White lab helped me apply the NAD tool I developed to their ATG7 model. Prof.
Kathryn Wellen was my first external collaborator and provided insights about adipocyte
biology. I also want to thank Prof. Craig Thompson and Prof. Morris Birnbaum for helpful
discussions in Chapter 4 and Dr. Vihelm A. Bohrfor for providing cells in Chapter 2. I also want
to thank two graduate students – Ying Zhang in the laboratory of Prof. Hildegund Ertl for the T
cell collaboration and Paras Mihas in the laboratory of Prof. Katrin Andreasson for the NADiv
macrophage study. These valuable collaborators have taught me, broadened my knowledge and
inspired me, and I have enjoyed working with every one of them.
I also want to thank my colleagues in the Rabinowitz lab: Dr. Xiaoyang Su, Dr. Junyoung Park,
and Dr. Sheng Hui, who provided their expertise in computation; Dr. Jing Fan, Dr. Xin Teng, Li
Chen, and Zhaoyue Zhang, who collaborated with me on the NADPH projects; and Dr. Wenyun
Lu, who helped me address mass spectrometry challenges. I also want to thank all the other
colleagues in the Rabinowitz lab who I have worked and become friends with: Dr. Gregory
Ducker, Dr. Lifeng Yang, Dr. Lin Wang, Michel Nofal, Dr. Cholsoon Jang, Sisi Zhang, Dr.
Melanie McReynolds, Dr. Raphael Morscher, and Adam Wang.
I thank my parents, my father Yi Liu and mother Yingxiu Wang. For the past 27 years, they have
taken care of me and supported me with their unconditional love. I thank my friends for being
supportive and helping me through tough times.
Lastly, I thank Princeton University. I feel blessed to have come to this prestigious institution. At
Princeton, not only did I receive rigorous training in research, I also have experienced the
transformative power of education and had the opportunity to teach and do volunteer work. I
thank the community here for giving me such a wonderful 5-year experience.
v
Table of Contents
Abstract .......................................................................................................................................... iii
Acknowledgement ......................................................................................................................... iv
Table of Contents ........................................................................................................................... vi
Chapter 1 Introduction .................................................................................................................... 1
1.1. NAD as a cofactor in metabolism ........................................................................................ 1
1.2. Kinetic flux profiling towards the quantitative analysis of NAD ........................................ 3
1.3. NADPH as the energy currency to provide reducing power ................................................ 5
1.4. Structure of the thesis ........................................................................................................... 7
1.5. Reference .............................................................................................................................. 7
Chapter 2 Quantitative analysis of NAD synthesis-breakdown fluxes ......................................... 11
2.1. Abstract .............................................................................................................................. 11
2.2. Introduction ........................................................................................................................ 12
2.3. Results ................................................................................................................................ 15
2.3.1. NAD flux quantification .............................................................................................. 15
2.3.2. NAD consumption routes ............................................................................................ 18
2.3.3. Impact of NAD concentration on fluxes...................................................................... 24
2.3.4. Tissue heterogeneity in NAD synthesis....................................................................... 27
2.3.5. Tracing the fate of NR and NMN ................................................................................ 32
vi
2.4. Discussion .......................................................................................................................... 35
2.5. Methods .............................................................................................................................. 40
2.5.1. Cell culture .................................................................................................................. 40
2.5.2. siRNAs, antibodies, and drugs .................................................................................... 41
2.5.3. Isotope labeling............................................................................................................ 41
2.5.4. Intravenous infusion of wildtype C57BL/6 mice ........................................................ 42
2.5.5. Metabolite measurements in cell lines......................................................................... 43
2.5.6. Metabolite measurements in serum and tissues ........................................................... 44
2.5.7. Quantification in cell lines of NAD synthesis fluxes and of NAD dilution by cell
growth .................................................................................................................................... 44
2.5.8. Quantification of NAD consumption fluxes by NAD kinase, PARPs, Sirtuins, and in
cells with acute DNA damage ............................................................................................... 46
2.5.9. Quantification of NAD fluxes in vivo ......................................................................... 47
2.6. References .......................................................................................................................... 50
Chapter 3 NAD is transported into mammalian mitochondria ..................................................... 58
3.1. Abstract .............................................................................................................................. 58
3.2. Introduction ........................................................................................................................ 59
3.3. Experimental Procedures.................................................................................................... 61
3.3.1. Mitochondrial Isolation from skeletal muscle ............................................................. 61
3.3.2. Mitochondrial Treatments ........................................................................................... 62
vii
3.3.3. NAD-NADH Cycling Assay ....................................................................................... 63
3.3.4. Cell culture .................................................................................................................. 63
3.3.5. Generation of CRISPR cell lines ................................................................................. 64
3.3.6. HPLC analysis of NMN in mitochondria isolated from liver and skeletal muscle ..... 64
3.3.7. Tracer studies ............................................................................................................... 65
3.3.8. Cell culture and isotopic labeling ................................................................................ 66
3.3.9. LC-MS Instrumentation and method development ..................................................... 67
3.3.10. Statistics ..................................................................................................................... 68
3.4. Results ................................................................................................................................ 68
3.4.1. NMN increases NAD levels in isolated mitochondria ................................................ 68
3.4.2. NAD synthesis in isolated mitochondria involves NMNAT, but not Nampt .............. 70
3.4.3. Matrix NAD is not restored by NMN treatment in isolated mitochondria. ................. 71
3.4.4 Cytosolic NMN contributes to mitochondrial NAD..................................................... 74
3.4.5. Cytosolic NAD(H) is imported into the mitochondria ................................................ 78
3.5. Discussion .......................................................................................................................... 83
3.6. References .......................................................................................................................... 87
Chapter 4 Quantitative analysis of adipocyte NADPH pathway usage ........................................ 95
4.1. Abstract .............................................................................................................................. 95
4.2. Introduction ........................................................................................................................ 96
4.3. Results ................................................................................................................................ 98
viii
4.3.1. Quantitative analysis of 3T3-L1 cell NADPH consumption. ...................................... 98
4.3.2. PPP activity and total NADPH generation ................................................................ 100
4.3.3. NADPH contribution of folate metabolism ............................................................... 102
4.3.4. Tracing carbon flux through malic enzyme ............................................................... 105
4.3.5. [2,2,3,3-2H]dimethyl succinate tracer for malic enzyme ........................................... 109
4.3.6. [4-2H]glucose as a malic enzyme tracer .................................................................... 112
4.3.7. Genetic confirmation of ME1’s NADPH contribution.............................................. 113
4.3.8. Impact of hypoxia on adipocyte metabolism ............................................................. 114
4.4. Discussion ........................................................................................................................ 116
4.5. Methods ............................................................................................................................ 120
4.5.1. Cell culture, gene knockdown with siRNA and antibodies. ...................................... 120
4.5.2. Isotopic labeling. ....................................................................................................... 121
4.5.3. Metabolite measurements. ......................................................................................... 122
4.5.4. Quantification of NADPH consumption. .................................................................. 123
4.5.6. CO2 release and oxPPP flux. ..................................................................................... 124
4.5.7. Malic enzyme carbon flux. ........................................................................................ 124
4.5.8. Quantification of fraction NADP2H. ......................................................................... 125
4.5.9. Calculation of ME1-dependent NADP2H flux. ......................................................... 126
4.5.10. Metabolic flux analysis. ........................................................................................... 128
4.6. References ........................................................................................................................ 129
ix
Chapter 5. Discussion ................................................................................................................. 136
Appendix ..................................................................................................................................... 140
Appendix A. Additional Information for Chapter 2 ............................................................... 140
Appendix B. Additional Information for Chapter 3 ............................................................... 152
Appendix C. Additional Information for Chapter 4 ............................................................... 155
x
Chapter 1 Introduction
1.1. NAD as a cofactor in metabolism
Metabolism consists of the chemical transformations that allow growth, reproduction, and
maintenance of homeostasis. To carry out these roles, cells employ fundamental cofactors such
as ATP and NAD. With rapid cycling between the oxidized and reduced forms, NAD is tightly
intertwined with central carbon metabolism (Figure 1.1a). NAD carries high energy electrons
driving oxidative phosphorylation1, and participates in reactions shown as orange arrows (Figure
1.1b).
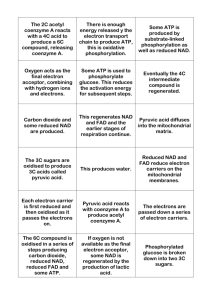
Figure 1.1. NAD in metabolism. (a) With cycling between the oxidized and reduced forms,
NAD intertwines tightly with energy metabolism. (b) NAD serves as a cofactor in reactions in
glycolysis and TCA cycle (orange arrows); NADPH serves as a cofactor in glycolysis, pentose
phosphate pathway and TCA cycle (light orange arrows).
1
NAD metabolism is complex, with multiple production routes and consuming enzymes. In
mammals, NAD is made de novo from tryptophan, via the Preiss-Handler pathway from
nicotinic acid (NA), via the salvage pathway from nicotinamide (NAM), or via the nicotinamide
ribose kinase pathway from nicotinamide riboside (NR)2,3,4. NAD is consumed by NAD kinase,
which makes the anabolic and redox defense cofactor NADPH. Though only with differed by
one phosphate, NADPH serves as a distinct cofactor driving the reactions shown as light orange
arrows (Figure 1.1b). In addition, NAD is consumed by multiple families of signaling enzymes.
Sirtuins (SIRTs) remove acyl marks (most commonly acetylation) on proteins using NAD and
generating O-acyl-ADP-ribose5. ADP-ribosyl-transferases, most famously poly-ADP-ribosepolymerases (PARPs), which play an important role in DNA damage repair, use NAD to modify
proteins with ADP-ribosyl groups6. Cyclic ADP-ribose hydrolases (CD38/CD157) consume
NAD to make the calcium-releasing second messengers, cyclic ADP-ribose and NAADP7.
Not only does NAD have fundamental biological importance, it also ties to human disease and
normal aging. NAD is gradually depleted during aging in multiple tissues, and has been proposed
as a master regulator of age-dependent pathology8. Its depletion induces mitochondrial
dysfunction and nuclear DNA damage by mechanisms that are currently under intense
investigation9,10. Acute NAD depletion has been proposed to promote neurodegeneration, to
drive cardiomyocyte damage during heart attacks, and to potentiate the killing of cancer cells by
chemotherapy11.
2
1.2. Kinetic flux profiling towards the quantitative analysis
of NAD
Due to NAD’s fundamental importance in epigenetics, energy metabolism and aging, it is
essential to measure NAD production and consumption pathways, and how they differ across cell
types, tissues, physiological states, and diseases. In addition, it is important to understand the
impact of drugs and nutraceuticals on NAD metabolism. Analysis of NAD metabolism and
related environmental perturbations has largely relied on the measurement of the concentration
of NAD and its related metabolites. However, estimating NAD synthesis and breakdown flux
based on concentrations is insufficient. Taking the traffic as an example, we want to know how
many cars can pass the road in any given time (synthesis and breakdown fluxes), which is
determined by speed and number of cars on a cross section (concentration).
Figure 1.2a shows that concentration doesn’t necessarily correlate with flux. We cannot
determine which road carries more traffic even though the upper one has a much higher
concentration. In addition, enzyme activities in lysates have been measured4. Yet enzyme
activities in lysates may not reflect cellular regulatory mechanisms. Accordingly, there is an
unmet need to measure NAD production and consumption fluxes in cells and tissues fluxes.
3
Figure 1.2. Kinetic flux profiling provides a solution to the unmet need to dissect NAD
metabolism. (a) Concentration itself (#cars on the cross section) is not sufficient to determine
flux rate (traffic). Photo credit: www.beijinger.com (b) Illustration of the concept of flux
profiling. NAD is generated from its sources and is consumed through pathways like PARP. At
metabolic steady state, we switch the source of NAD from unlabeled form to labeled form
(change the color from black to orange). We then measure the rate of disappearance of the
unlabeled form of NAD when “black” is substituted with “orange”. Since the upper one has a
bigger NAD pool and slower synthesis rate, the disappearance rate will be much smaller
compared to the lower one.
Therefore, flux measurement holds the potential to illuminate the main pathways responsible for
NAD production and consumption, and how they differ across cell types, tissues and disease
states. Figure 1.2b illustrates the basic concept of kinetic flux profiling. At metabolic steady
state, the influx and efflux of NAD pool are both 𝑓𝑖𝑛 . 𝑓𝑖𝑛 can be determined by measuring the
4
rate of NAD labeling and NAD concentration, 𝑓𝑖𝑛 = k · [concentration] · (labeling t1/2)-1. This can
be done through mass spectrometry, with quantitative measurement of both unlabeled and
labeled forms of different NAD-related metabolites12,13.
1.3. NADPH as the energy currency to provide reducing
power
NADP(H) is a close relative of NAD(H) that has distinct roles and is generated from NAD(H)
via NAD kinase. NADPH is a key cofactor and an essential energy carrier involved in
antioxidant defense and reductive biosynthesis, including making DNA, proline and fatty acids14.
It can be produced from NADP in cells by a variety of enzymes including glucose-6-phosphate
dehydrogenase (G6PDH) and 6-phosphogluconate dehydrogenase in the pentose phosphate
pathway (PPP), methylenetetrahydrofolate dehydrogenase (MTHFD) and aldehyde
dehydrogenases (ALDH) in folate metabolism, and isocitrate dehydrogenase (IDH) associated
with the TCA cycle, and malic enzyme (ME). The PPP is localized to the cytosol and NADPHspecific, while different isozymes of MTHFD, ALDH, ME, IDH are found in cytosol and
mitochondria, and may generate NADPH or NADH15,16. Among these different enzymes, the
importance of the PPP in NADPH production is the best established17.
13
C-tracers are well suited and have long been used to follow metabolic activity, due to its stable
incorporation into molecules and minimal kinetic isotope effect. For dissecting redox cofactors
like NADPH, 13C is inadequate when the same carbon transformation can produce either
NADPH or NADH depending on the isozyme involved. To address this limitation, 2H tracer
5
methods have recently been introduced18. Fan et al demonstrated the utility of 3-2H glucose for
tracing oxPPP19, and compartment-specific NADPH hydride 2H-labeling has been traced using
2-hydroxyglutarate as a reporter metabolite18. Both of direct NADPH 2H-labeling measurements
and the 2-hydroxyglutarate reporter approach revealed that the PPP is the largest cytosolic
NADPH source in typical transformed cells in culture, albeit with other pathways collectively
making a roughly comparable contribution20–23. Whether different enzymes play a predominant
role in certain cell types or conditions remains unknown.
The most NADPH-demanding biosynthetic activity in mammals is fat synthesis, which
consumes a majority of cytosolic NADPH in typical transformed cells in culture19. In intact
mammals, fat synthesis is thought to be localized primarily to liver and adipose24. Significant
malic enzyme activity was described in adipose tissue more than 50 years ago25,26. During
adipocyte differentiation, there is coordinate up-regulation of ATP citrate lyase and cytosolic
malic enzyme (ME1), which together with cytosolic malate dehydrogenase and at the expense of
1 ATP, can convert citrate and NADH into acetyl-CoA, NADPH, and pyruvate27. Acetyl-CoA
and NADPH are the two key substrates for fat synthesis, while the resulting pyruvate can be used
to make more citrate. Thus, it is efficient to use malic enzyme to make NADPH in adipose. The
quantitative contribution of different NADPH-producing enzymes in adipose, however, remains
ill defined. Prior quantitative studies suggest a ~60% contribution for the oxPPP and the
remainder from other pathways.
6
1.4. Structure of the thesis
We quantified NAD and NADPH fluxes using stable isotope tracers combined with
mathematical modeling. In Chapter 2, we established methods for measurement of NAD
synthesis and breakdown fluxes in cell lines and mouse tissues. From a more quantitative and
chemical engineering (i.e. flux) perspective than has been done before, we provided answers for
some NAD fundamental questions including the turnover rates and relative contribution between
NAD consumers. In cell lines, NAD was made from nicotinamide and consumed largely by
PARPs and sirtuins. In vivo, NAD fluxes varied widely across tissues, with high flux in small
intestine and spleen and low flux in skeletal muscle. Intravenous, but not oral administration of
nicotinamide riboside or mononucleotide delivered intact molecules to multiple tissues, with
skeletal muscle displaying a preference for NR. In Chapter 3, we focused on mitochondrial NAD
metabolism in mammalian cells, and found out that only intact NAM-contained nucleotides and
NAD, not NAM itself, can be imported into mitochondria directly. In Chapter 4, we dissected the
redox metabolism of NADPH, and studied how cells make NADPH under different
environmental conditions. We showed that most NADPH in differentiating 3T3-L1 adipocytes is
made by malic enzyme. The associated metabolic cycle is disrupted by hypoxia, which switches
the main adipocyte NADPH source to the oxPPP.
1.5. Reference
1.
Pollak, N., Dölle, C. & Ziegler, M. The power to reduce: pyridine nucleotides – small
molecules with a multitude of functions. Biochem. J. 402, 205–218 (2007).
2.
Hassa, P. O., Haenni, S. S., Elser, M. & Hottiger, M. O. Nuclear ADP-ribosylation
7
reactions in mammalian cells: where are we today and where are we going? Microbiol.
Mol. Biol. Rev. 70, 789–829 (2006).
3.
Bogan, K. L. & Brenner, C. Nicotinic acid, nicotinamide, and nicotinamide riboside: a
molecular evaluation of NAD+ precursor vitamins in human nutrition. Annu. Rev. Nutr.
28, 115–130 (2008).
4.
Mori, V. et al. Metabolic profiling of alternative NAD biosynthetic routes in mouse
tissues. PLoS One 9, 1–27 (2014).
5.
Haigis, M. C. & Sinclair, D. a. Mammalian Sirtuins: Biological Insights and Disease
Relevance. Annu. Rev. Pathol. 5, 253–295 (2010).
6.
Rouleau, M., Patel, A., Hendzel, M. J., Kaufmann, S. H. & Poirier, G. G. PARP
inhibition: PARP1 and beyond. Nat. Rev. Cancer 10, 293–301 (2010).
7.
Malavasi, F. et al. Evolution and Function of the ADP Ribosyl Cyclase / CD38 Gene
Family in Physiology and Pathology. Physiol. Rev. 88, 841–886 (2008).
8.
Chini, C., Tarrago, M. & Chini, E. NAD and the aging process: Role in life, death and
everything in between. Mol. Cell. Endocrinol. (2016).
9.
Fang, E. F. et al. Nuclear DNA damage signalling to mitochondria in ageing. Nat. Rev.
Mol. Cell Biol. 17, 308–321 (2016).
10.
van de Ven, R. a. H., Santos, D. & Haigis, M. C. Mitochondrial Sirtuins and Molecular
Mechanisms of Aging. Trends Mol. Med. 23, 320–331 (2017).
11.
Hasmann, M. & Schemainda, I. FK866, a Highly Specific Noncompetitive Inhibitor of
8
Nicotinamide Phosphoribosyltransferase, Represents a Novel Mechanism for Induction of
Tumor Cell Apoptosis. Cancer Res. 63, 7436–7442 (2003).
12.
Trammell, S. A. & Brenner, C. Targeted, LCMS-based Metabolomics for Quantitative
Measurement of NAD(+) Metabolites. Comput. Struct. Biotechnol. J. 4, e201301012
(2013).
13.
Ratajczak, J. et al. NRK1 controls nicotinamide mononucleotide and nicotinamide
riboside metabolism in mammalian cells. Nat. Commun. 7, 13103 (2016).
14.
Voet, D. & Voet, J. Biochemistry. (New york: J. Wiley & Sons, 2004).
15.
Tibbetts, A. S. & Appling, D. R. Compartmentalization of Mammalian folate-mediated
one-carbon metabolism. Annu. Rev. Nutr. 30, 57–81 (2010).
16.
Wise, D. R. et al. Hypoxia promotes isocitrate dehydrogenase-dependent carboxylation of
α-ketoglutarate to citrate to support cell growth and viability. Proc. Natl. Acad. Sci. U. S.
A. 108, 19611–6 (2011).
17.
WHO. Glucose-6-phosphate dehydrogenase deficiency. Bull. World Heal. Organiztion 67,
601–611 (1989).
18.
Lewis, C. a et al. Tracing Compartmentalized NADPH Metabolism in the Cytosol and
Mitochondria of Mammalian Cells. Mol. Cell 55, 253–263 (2014).
19.
Fan, J. et al. Quantitative flux analysis reveals folate-dependent NADPH production.
Nature 510, 298–302 (2014).
20.
Si, Y., Yoon, J. & Lee, K. Flux profile and modularity analysis of time-dependent
9
metabolic changes of de novo adipocyte formation. Am. J. Physiol. Endocrinol. Metab.
292, E1637--46 (2007).
21.
Katz, J. & Rognstad, R. The metabolism of tritiated glucose by rat adipose tissue. J. Biol.
Chem. 241, 3600–10 (1966).
22.
Kather, H., Rivera, M. & Brand, K. Interrelationship and control of glucose metabolism
and lipogenesis in isolated fat-cells. Control of pentose phosphate-cycle activity by
cellular requirement for reduced nicotinamide adenine dinucleotide phosphate. Biochem.
J. 128, 1097–102 (1972).
23.
Flatt, J. P. & Ball, E. G. ARTICLE : Studies on the Metabolism of Adipose Tissue : XV .
AN EVALUATION OF THE MAJOR PATHWAYS OF GLUCOSE CATABOLISM AS
INFLUENCED BY INSULIN AND EPINEPHRINE on the Metabolism of Adipose.
(1964).
24.
Nguyen, P. et al. Liver lipid metabolism. J. Anim. Physiol. Anim. Nutr. (Berl). 92, 272–83
(2008).
25.
Young, J. W., Shargo, E. & Lardy, H. A. Metabolic Control of Enzymes Involved in
Lipogenesis and Gluconeogenesis *. 3, 1687–1692 (1964).
26.
Wise, E. M. & Ball, E. G. Malic enzyme and lipogenesis. Proc. Natl. Acad. Sci. U. S. A.
52, 1255–1263 (1964).
27.
Wise, L. S., Sul, H. S. & Rubin, C. S. Coordinate regulation of the biosynthesis of ATPcitrate lyase and malic enzyme during adipocyte differentiation. Studies on 3T3-L1 cells.
J. Biol. Chem. 259, 4827–32 (1984).
10
Chapter 2 Quantitative analysis of NAD
synthesis-breakdown fluxes
2.1. Abstract
The redox cofactor nicotinamide adenine dinucleotide (NAD) plays a central role in metabolism
and is a substrate for signaling enzymes including poly-ADP-ribose-polymerases and sirtuins.
NAD concentration falls during aging and in certain diseases, which has triggered intense
interest in strategies to boost NAD levels. A limitation in understanding NAD metabolism has
been reliance on steady-state concentration measurements. Here, we present isotope-tracer
methods for NAD flux quantitation. In cell lines, NAD was made from nicotinamide and
consumed largely by PARPs and sirtuins. In vivo, NAD was made from tryptophan selectively in
liver, which then excreted nicotinamide. NAD fluxes varied widely across tissues, with high flux
in small intestine and spleen and low flux in skeletal muscle. Intravenous, but not oral
administration of nicotinamide riboside or mononucleotide delivered intact molecules to multiple
tissues, with skeletal muscle displaying a preference for NR. Thus, fluxes provide a novel
window into NAD biology.
__________________________________________________
Reproduced with permission from Ling Liu, Xiaoyang Su, William Quinn, Sheng Hui, Kristin
Krukenberg, David Frederick, Philip Redpath, Le Zhan, Karthikeyani Chellappa, Eileen White,
Marie Migaud, Timothy Mitchison, Joseph Baur, and Joshua Rabinowitz.
Under review, Cell Metabolism.
11
2.2. Introduction
The redox cofactor NAD (nicotinamide adenine dinucleotide) plays a central role in cellular
energy generation, carrying high energy electrons and driving oxidative phosphorylation1. NAD
is regenerated from NADH by oxidation, with rapid cycling between the oxidized and reduced
forms. The total pool size of NAD(H) depends on the relative rates of synthesis and degradation.
In mammals, NAD is made de novo from tryptophan, via the Preiss-Handler pathway from
nicotinic acid (NA), via the salvage pathway from nicotinamide (NAM, the redox-active ring
alone, without ADP-ribose), or via the nicotinamide ribose kinase pathway from nicotinamide
riboside (NR)2,3,4. NAD is consumed by NAD kinase, which makes the anabolic and redox
defense cofactor NADP(H), as well as multiple families of signaling enzymes. Sirtuins (SIRTs)
remove acyl marks (most commonly acetylation) on proteins using NAD, generating O-acylADP-ribose and NAM5. ADP-ribosyl-transferases, most famously poly-ADP-ribose-polymerases
(PARPs), which play an important role in DNA damage repair, use NAD to modify proteins with
ADP-ribosyl groups6. Cyclic ADP-ribose hydrolases (CD38/CD157) consume NAD to make the
calcium-releasing second messengers, cyclic ADP-ribose and NAADP7. Puzzlingly, the catalytic
domain of CD38 faces the extracellular space under normal conditions, raising questions of how
it accesses NAD8. Thus, NAD metabolism is complex, with multiple production routes and a
myriad of consuming enzymes, many of which primarily function in signaling, rather than
metabolism.
Measuring NAD metabolism is of great interest, due to NAD’s fundamental biological
importance, and ties to human disease and normal aging. NAD is gradually depleted during
aging in multiple tissues, and has been proposed as a master regulator of age-dependent
12
pathology9. Its depletion induces mitochondrial dysfunction and nuclear DNA damage by
mechanisms that are currently under intense investigation10,11. Acute NAD depletion has been
proposed to promote neurodegeneration, to drive cardiomyocyte damage during heart attacks,
and to potentiate the killing of cancer cells by chemotherapy12.
Consistent with the medical importance of NAD metabolism, there has been great interest in its
pharmacological modulation. Small molecule PARP inhibitors promote cell death in certain
cancers by blocking DNA damage repair13, but also spare NAD, which can be beneficial in other
settings14,15. Hyperactivation of PARPs promotes cell death through multiple mechanisms,
including NAD depletion and signaling through PAR-dependent pathways16,17. Inhibitors of the
enzyme NAMPT, which is required for NAD biosynthesis from NAM, are in clinical trials for
cancer treatment, based on their potential to deplete NAD and thereby block cancer growth18.
Certain cancers cannot make NAD from NA, which led to the concept of rescuing normal cells,
but not vulnerable cancer cells, from NAMPT inhibition using NA19. NAMPT activators are
under investigation for treating neurodegeneration by raising NAD20,21. Activators of NADconsuming SIRTs, whose activities are suspected to deleteriously drop when NAD levels are low
in aging and degenerative disease, have also been proposed as therapeutics22. CD38 deletion is
effective in reducing diet-induced obesity and metabolic syndrome in mouse models, and is
thought to act in part by increasing tissue NAD levels23. Finally, there is extensive interest in
NR and NMN, which can be converted into NAD without passing through the gating enzyme for
NAM assimilation, NAMPT, as nutraceuticals to boost NAD levels and prevent the effects of
aging24,25.
13
To date, analysis of NAD metabolism and related drug perturbations has largely relied on
measurement of the concentration of NAD, and occasionally of related metabolites, and on how
these levels change in response to drug perturbation, disease and aging. In addition, enzyme
activities in lysates have been measured4. Estimating NAD synthesis and breakdown rates based
on concentrations or biochemical assays is insufficient: an increased concentration may reflect
increased production or decreased consumption, while enzyme activities in lysates may not
reflect cellular regulatory mechanisms. Accordingly, there is an unmet need to measure NAD
production and consumption rates in cells and tissues (fluxes). Flux measurement holds the
potential to illuminate the main pathways responsible for NAD production and consumption, and
how they differ across cell types, tissues and disease states. Although 14C tracing to estimate
NAD turnover was reported more than 40 years ago26–28,29,30, mass spectrometry now allows
similar experiments to be conducted using stable isotopes, with quantitative measurement of both
unlabeled and labeled forms of different NAD-related metabolites31,32.
Here, we establish methods for measurement of NAD synthesis and breakdown fluxes in cell
lines and mouse tissues using stable isotope tracers combined with mathematical modeling. We
find that NAM is the main NAD source in both cell lines and most murine tissues. Liver actively
makes NAD de novo from tryptophan, releasing NAM into the blood, which supports NAD
biosynthesis in the rest of the body. Mouse tissues vary markedly in NAD fluxes and turnover
rates, with liver, lung, spleen, and small intestine having a turnover half-time faster than any of
the tested cultured cell lines, and skeletal muscle slower. Unlike in cell culture where NR and
NMN are readily incorporated into NAD32,33, oral administration fails to deliver NR or NMN to
tissues without breaking the nicotinamide-ribose bond. Assimilation after IV administration
varies between tissues, with NR being used preferentially over NMN in muscle. Future
14
pharmacological and nutraceutical efforts to boost NAD will need to take into account the
minimal oral bioavailability of NR and NMN and the tissue specific features of NAD
metabolism.
2.3. Results
2.3.1. NAD flux quantification
To quantify NAD metabolism in tissue culture, we substituted [2,4,5,6-2H] NAM into the media
of T47D breast cancer cells. DMEM medium with 10% dialyzed serum was prepared from
scratch with solely isotopic NAM (32 µM, the standard DMEM concentration, which is 15x
normal circulating levels in mice, Appendix Table A1) (Figure 2.1a). Feeding labeled NAM
resulted, at steady-state, in nearly complete NAD labeling. Feeding [U-13C] Trp did not result in
detectable NAD labeling, even after 4 days in NAM-free medium (Appendix Figure A1a and
S1b), consistent with lack of the relevant enzyme expression in T47D cells19,34. There is no
nicotinic acid or nicotinamide riboside in standard cell culture medium. Thus, in these typical
cell culture conditions, essentially all NAD is synthesized from NAM.
Figure 2.1a schematizes NAD synthesis and breakdown fluxes at steady state in growing cells; fin
is the synthetic flux from NAM to NAD, fgrowth accounts for dilution by growth, and fout accounts
for the collective breakdown by NAD kinase, PARPs etc. Color indicates isotope labeling
following transfer into isotope labeled medium. Dynamic labeling studies revealed that labeling
of intracellular NAM (t1/2 20min) was much faster than that of NAD (t1/2 9 h) (Figure 2.1b, for
15
concentration, see Appendix Figure A1c). Thus, NAM equilibration across the membrane is fast
compared to NAD biosynthesis. Although the NAM was M+4, most labeled NAD was M+3, as
expected due to rapid turnover of the redox-active hydrogen at the 4 position (Figure 2.1c). The
rapid exchange of NAD and NADH (which can be estimated from glycolysis rate) resulted in the
indistinguishable labeling kinetics between NAD and NADH (Appendix Figure A1d), and thus
one well mixed pool from the perspective of other NAD-consuming reactions. We also observed
a minor NAD M+2 fraction (Figure 2.1d). The M+2 species could, in theory, arise from
interconversion between NAD and quinolinic acid, or spontaneous H-D exchange. RNAi knockdown of quinolinate phosphoribosyl transferase (QPRT) did not inhibit formation of the M+2
species, suggesting it is generated by spontaneous exchange35 (Appendix Figure A1e and S1f).
We next developed a quantitative analysis of the fluxes underlying the observed labeling
dynamics. After being taken up by cells, NAM forms NAD with flux fin. In the presence of
labeled NAM, the unlabeled fraction of NAD (NADU, Figure 2.1b) accordingly decreases:
dNADU
dt
𝑓
𝑖𝑛
= − [NAD]
NADU (1)
[NAD] is the constant total intracellular concentration of NAD(H) (i.e. the sum of the oxidized
and reduced cofactor concentrations, which is 1880 pmol per million cells, with [NAD] >>
[NADH]; note that the volume of 1 million cells is about 3 µL, so this equates to about 0.6 mM
NAD). Based on the experimental data for isotope incorporation (Figure 2.1b-c), fin is 144 pmol
per million cells per hour, with 95% confidence interval (CI) of 121 to 169 (determined by
bootstrapping). The NAD synthesis flux fin must balance with i) all NAD consumption (i.e., due
to PARPs, SIRTs, CD38, NAD kinase, and other NAD-consumers, with sum of which is fout) and
ii) expansion of the NAD pool due to cell growth (fgrowth). Cell growth was measured separately
16
to determine the growth rate constant (𝑔) with fgrowth = 𝑔 [NAD]. In T47D cells, fgrowth accounts
for ~20% of fin. Therefore, with the NAD concentration of about 0.6 mM and a turnover t1/2 of 9
h, T47D cells breakdown a majority of newly made NAD.
Figure 2.1. Quantitation of NAD turnover in cell culture. (a) Switching the media from
unlabeled to [2,4,5,6-2H] nicotinamide (2H-NAM) results in NAD labeling without otherwise
perturbing cellular pool sizes or fluxes. Fast labeling implies high fluxes relative to poolsize. (b)
Isotopic fractions of intracellular NAM and NAD after switching to 2H-NAM in T47D cells; U,
unlabeled fraction; L, labeled fraction. (c) Labeling schematic. (d) NAD labeling dynamics after
switching to 2H-NAM in T47D cells. Symbols, experimental data (mean ± s.d., n=3); lines are to
guide the eye.
17
2.3.2. NAD consumption routes
NAD is the substrate for essential metabolic processes including NADP synthesis by NAD
kinase and important protein covalent modification reactions (SIRTs, ADP-ribosylation). We
sought to separately quantify the major NAD consuming pathways (Figure 2.2a). To investigate
the contribution of NAD kinase, we measured the dynamics of NADP labeling. Compared to
NAD, NADP labeled detectably more slowly (Figure 2.2b, for concentrations, see Appendix
Figure. A1g). The slower labeling does not reflect a slower intrinsic turnover rate of NADP(H)
relative to NAD(H), but rather the NADP being downstream of NAD, with the time lag in
labeling used to calculate the NAD kinase forward flux (𝑓1 )36 (see Methods). Due to the slower
labeling and 20-fold smaller total pool size of NADP(H) relative to NAD(H), the NAD kinase
flux is only ~ 10% of total NAD consumption, 12 pmol per million cells per hour (CI 11 to 14),
compared to total NAD consumption of 118 pmol per million cells per hour.
Figure 2.2. NAD kinase flux. (a) Approach to calculate NAD consumption by NAD kinase (𝑓1 ,
forward flux). (b) Labeling dynamics; symbols, experimental data (n=3); lines, fit to differential
equations in (a). **p<0.01, paired t-test; dots, experimental data, n=3.
18
To measure NAD consumption by PARP1/2, the major DNA-damage responsive PARPs, we
switched exponentially growing cells simultaneously into 2H-NAM and olaparib (AZD2281), an
FDA-approved PARP1/2 inhibitor drug37. Compared to untreated cells, olaparib-treated cells
accumulated an indistinguishable amount of labeled NAD at early time points(Figure 2.3a, blue
lines), indicating that NAD synthesis from NAM is unaltered. The decay of unlabeled NAD
was, however, slower, and the NAD concentration increased. Thus, PARP inhibition increased
the NAD pool by decreasing its consumption38. Based on the slower rate of unlabeled NAD
decline, we determined the value of fout upon inhibitor treatment (Figure 2.3b-c) to be 79 pmol
per million cells per hour (versus 118 in the absence of PARP inhibition), with the difference
being the PARP contribution of 38 pmol per million cells per hour (CI 28 to 43). Thus, in T47D
cells, approximately one third of NAD consumption is due to basal PARP1/2 activity.
PARP is thought to be the major NAD consumer in cells with DNA damage17,6. In the absence of
DNA damage, basal PARP activity, as measured by the accumulation of protein poly-ADPribosylation in cell lysates with poly(ADP-ribose) glycohydrolase inhibitor added, was recently
reported to vary markedly across cancer cell lines39. We compared PARP-mediated NAD flux in
five human breast cancer cell lines with basal lysate PARylation activities39. We found that the
two cell lines with relatively high PARylation (KPL1 and MCF7) did not exhibit lower NAD
concentration or higher PARP-mediated NAD consumption than the three cell lines with
relatively low PARylation (AU565, SKBR3 and T47D) (Figure 2.3d, Appendix Table A2). This
suggests that cellular PARP1/2 flux is determined by factors distinct from PARP activity as
captured by lysate assays.
19
One potential explanation is that PARP activity is determined mainly by cellular factors, such as
DNA damage, which may not be reliably captured in lysates. Constitutive DNA damage due to
genetic defects in DNA repair has been reported to decrease NAD pools15. We investigated cells
with dysfunction in the DNA repair protein, xeroderma pigmentosum group A (XPA), and a
matched control line that was rescued by XPA transfection15. Compared to XPA-restored cells,
XPA-deficient cells suffer from chronic DNA damage, and exhibit lower steady state NAD
concentration33 (confirmed in Appendix Figure A2a). We observed faster NAD labeling
(Appendix Figure A2b) and an associated larger total NAD consumption flux in the XPAdeficient cells (Figure 2.3e). Moreover, the PARP contribution (as measured by adding olaparib
together with labeled NAM) was larger. Thus, while we do not observe a relationship between
basal lysate PARylation activities and NAD flux, we capture the known link between
compromised DNA repair, PARP, and NAD consumption.
To investigate the effects of acute DNA damage, we treated T47D cells with zeocin to trigger
DNA double strand breaks at the same time as switching into 2H-NAM, and analyzed total and
2
H-NAD after 8 h. Zeocin reduced total NAD to ~60% of control, mainly by accelerating the
loss of unlabeled NAD, and this effect was blocked by olaparib (Figure 2.3f). Quantitative
analysis revealing ~ 2x increase in fout that was reversed by co-treatment with PARP inhibitor
(Figure 2.3g). Thus, PARP consumes about one-third of NAD under basal conditions, and
becomes the dominant consumer in the presence of overt DNA damage (a 4-fold increase in
PARP activity led to a 2-fold increase in total consumption flux). These observations capture the
quantitative change in flux during DNA damage, although harsher damage might lead to a yet
more dramatic change40.
20
To evaluate contributions from other pathways, we monitored the increase in NAD pool size and
labeling pattern in T47D cells treated with sirtinol (a SIRT1/2 inhibitor) and EX527 (a SIRT1
inhibitor) (Figure 2.3h, Appendix Figure. A2c-d). We observed a significant decrease in fout.
Quantitatively SIRT1/2 consume about one-third of NAD under basal conditions (32 pmol per
million cells per hour, CI 24 to 41), similar to consumption by PARP1/2. The effect of dual
PARP1/2 and SIRT1/2 inhibition was roughly additive, confirming that PARP1/2 and SIRT1/2
collectively account for the majority of NAD consumption (Figure 2.3i-j).
We then examined two additional cell lines, the transformed but non-tumorigenic breast cell
MCF7 and differentiating myotubes (C2C12, Appendix Figure A2e-i). Comparison of NAD
labeling to cellular growth rate revealed that most NAD in the MCF7 cells was passed along to
their daughter cells, whereas in the differentiating C2C12 cells, essentially all NAD was
consumed, as expected based on their post-mitotic status (Figure 2.3k). Nevertheless, in both
cases, based on NAM-tracer experiments with olaparib and sirtinol, the relative contributions of
PARP1/2 and SIRT1/2 were similar. For proliferating cells, we did not observe a clear
correlation between growth rate and fgrowth. Thus, across several cell lines, NAD consumption by
PARP1/2 is similar to that by SIRT1/2 (Figure 2.3k-l).
21
Figure 2.3. NAD utilization in cell lines. (a) NAD concentration and labeling in T47D cells
treated with olaparib (10μM, PARP1/2 inhibitor). Olaparib was added simultaneously with
switching cells into 2H-NAM. Symbols, experimental data (mean ± s.d., n=3); lines, fit to
equations corresponding to model in (b) (see Methods). (b) Approach to calculate NAD
consumption by different enzymes, based on assumption of fixed NAD production flux and
decreased consumption flux upon adding inhibitor. (c) Fitted NAD efflux based on NAD
22
concentration, cell growth rate, and isotope labeling in the presence or absence of 10 μM
olaparib as shown in panel (a). Horizontal line within box, best fit; box, interquatile range;
whisker, 95% confidence intervals. (d) Basal lysate PARylation and PARP-mediated NAD
consumption as measured by isotope tracing in the presence and absence of 10 μM olaparib are
not correlated across five breast cell lines. Data are mean ± s.d., n = 3. (e) Total NAD
consumption fluxes in XPA-deficient or XPA-restored cells treated with DMSO or olaparib,
calculated from 2H-NAM labeling in the first 8 h of drug treatment. Results are normalized to
untransfected XPA-deficient cells; data are mean ± s.d., n = 3; * p<0.05, paired t-test. (f) NAD
concentration and labeling in T47D cells incubated simultaneously with 2H-NAM and zeocin
(250μg/ml, to induce DNA double strand break), with or without olaparib, for 8 h. Data are mean
± s.d., n = 3. (g) Increase in total NAD consumption flux based on data in (f) (mean with 95%
confidence interval). (h) NAD concentration and labeling in T47D cells treated with sirtinol (25
μM, Sirtuin 1/2 inhibitor). Sirtinol was added simultaneously with switching cells into 2H-NAM.
Symbols, experimental data (n=3); line, fit to equations. (i) Same as (h) but with dual PARP and
SIRT1/2 inhibition. (j) Decrease in NAD consumption, calculated based on first 4 hours after
drug exposure in T47D cells, for olaparib (10 μM, PARP1/2 inhibitor), sirtinol (25 μM, Sirtuin
1/2 inhibitor), EX527(10 μM, Sirtuin 1/2 inhibitor), and cotreatment of olaparib (10μM) and
sirtinol (25μM) (mean with 95% confidence interval). (k) Fraction of NAD directed toward
supporting growth in different cell lines cell lines, as determined by experimental measurements
of growth rate relative to NAD isotope labeling rate (mean with 95% confidence interval). (l) Pie
graphs indicating NAD fates in differentiated myocytes (C2C12 cells) and proliferating T47D
and MCF7 cells. Consumption routes in C2C12 cells and MCF7 cells were determined as for
T47D cells (see Appendix Figure A2 for data in C2C12 cells and MCF7 cells).
23
2.3.3. Impact of NAD concentration on fluxes
The rate of enzymatic reactions depends on substrate concentration, so we expect an effect of
concentrations on fluxes. To test this for NAD consumption we first treated cells with FK866, an
NAMPT inhibitor in clinical trials41, simultaneously with switching into 2H-NAM. As expected,
FK866 almost completely blocked NAD labeling. We then assessed whether the resulting drop in
NAD concentration altered NAD consumption kinetics. The decline in NAD concentration
following addition of FK866 approximated a single-exponential decay (Figure 2.4a), which
implies that NAD consumption depends linearly on its concentration: fout = k [NAD]. To further
test the relationship between [NAD] and 𝑓𝑜𝑢𝑡 , we reduced the media NAM to 0.1x or 0.01x of
its normal concentration in DMEM (i.e. to roughly 1.5x and 0.15x normal circulating levels),
resulting in a 20% and 70% drop over one week in [NAD] (Figure 2.4b). We then switched to
isotopic NAM at the same concentration and observed that 𝑓𝑜𝑢𝑡 was roughly proportional to
[NAD] (Figure 2.4b-c).
We next probed the effect of increasing NAD on flux by feeding nicotinamide riboside (NR).
Addition of NR at 5x the normal media NAM concentration over 4 days increased [NAD] by
60%. NAD consumption increased proportionally, i.e. we saw no evidence that consumption was
saturated under basal conditions. Thus, both with NAD depletion and increase (via acute
pharmacologic perturbations or long-term nutrient perturbations), , NAD consumption flux was
proportional to its concentration. Because PARP1/2 and SIRT1/2 are major consumption
enzymes, these data suggest that, at least in in T47D cells, their cellular activities are
substantially determined by NAD concentration.
24
Figure 2.4. Relationship between NAD concentration and flux in cell lines. (a) NAD
concentration and labeling in T47D cells treated with FK866 (100nM, NAMPT inhibitor).
FK866 was added simultaneously with switching cells into 2H-NAM. Symbols, experimental
data (mean ± s.d., n=3); line, fit to equations corresponding to the illustrated kinetic scheme,
which assumes that NAMPT fully blocks NAD synthesis and NAD consumption is proportional
to its concentration (“first-order kinetics”). (b) NAD concentration before and after labeling for 5
h. T47D cells were pre-treated with 1x NAM (standard DMEM condition), 0.1x NAM, or 0.01x
NAM for 1 week and labeled with the same concentration of 2H-NAM, or were pre-treated with
5x NR for 4 days and labeled with the same concentration of 2H,13C-NR. Data are mean ± s.d., n
= 4. (c) Correlation between NAD concentration and consumption flux based on data in (b). (d)
Correlation between t1/2 for NAD labeling by 2H-NAM and t1/2 for NAD depletion upon adding
25
FK866 (100nM) across 12 cell lines. Each dot represents one cell line. For data by cell line, see
Appendix Table A3. (e) Across the same 12 cell lines, NAD flux correlates poorly with labeling
t1/2. (f) NAD flux correlates more strongly with intracellular NAD concentration.
To measure NAD breakdown flux, and its dependence on NAD concentration in more cell types,
we measured NAD labeling dynamics in response to FK866 across 12 cell lines (3 other breast
cancer cell lines, 4 gastrointestinal cancer cell lines, 2 melanoma cell lines and differentiated
myocytes and adipocytes). Across these cell lines, the t1/2 for NAD depletion by FK866 was
nearly identical to NAD labeling t1/2 in the absence of drug (slope of 1.03 with R2=0.9246, p <
0.005) (Figure 2.4d, Appendix Table A3). Different cell lines varied in NAD demand for growth
(Figure 2.3k), NAD concentration (from 1 to 7 nmol per million cells) and labeling halftime (5 h
to 14 h). Together [NAD] and labeling t1/2 determine NAD synthesis flux (𝑓𝑖𝑛 = ln2 [NAD]/ labeling t1/2).
Interestingly, [NAD] was more variable than t1/2 and thus exerted greater influence over 𝑓𝑖𝑛 .
Indeed, we found a strong correlation (R2=0.81, p < 0.005) between concentration and fluxes, but
no correlation between t1/2 and fluxes (Figure 2.4e-f). These data are consistent with high
production flux leading to a large NAD pool size, with the consumption rate in cell lines
proportional to [NAD]. One practical implication of this finding is that NAD flux can be
estimated in tissue culture by the kinetics of NAD loss after blocking NAMPT, without the need
for isotope tracer methods.
26
2.3.4. Tissue heterogeneity in NAD synthesis
We next employed isotope tracing to probe whole organism NAD metabolic fluxes within, and
between, mouse tissues. In mammalian serum, tryptophan, NAM and NA are the most abundant
NAD precursors (with concentration >0.1 μM, Figure 2.5a), and accordingly we selected [U-13C]
Trp, [2,4,5,6-2H] NAM, and [U-13C] NA for in vivo tracing studies (Figure 2.5b, for their effects
in vitro, see Appendix Figure A3-4). Infusions were performed on 12-14 week old C57BL/6
mice pre-catheterized on the right jugular vein, aiming to quantify in a tissue-specific manner (i)
biosynthetic flux from tryptophan and NA to NAD, (ii) salvage flux from tissue NAM to NAD,
(iii) exchange flux between tissue NAM and serum NAM, and (iv) NAD kinase flux.
Infusion of [U-13C]-tryptophan (M+11) at a consistent rate of 5 nmol per gram per min rapidly
resulted in approximately 60% serum tryptophan labeling, with accumulation over ~ 24 h of
serum NAM M+6 (six carbon atoms from tryptophan are retained in NAD and NAM) (Appendix
Figure A5a). Tissue sampling at 5 h revealed preferential NAM labeling in liver: Liver NAM
was labeled in excess of circulating NAM, whereas NAM in all other tissues was labeled less
than circulating NAM (Figure 2.5c). A straightforward interpretation is that, like cell lines, most
tissues do not make NAD by de novo synthesis, and instead rely on NAM synthesized and
released from liver. Infusion of [U-13C] NA (M+6) at a consistent rate of 0.02 nmol per gram per
min resulted in 90% serum nicotinic acid labeling. This high extent of labeling indicates that
endogenous NA flux is small. Despite the high extent of circulating NA labeling, the
contribution of NA to serum NAM was low (1% after 5 h, compared to 5% after 5 h from
trptophan infusion, Figure 2.5c). Correcting for the extent of serum NA and tryptophan labeling,
27
this indicates that circulating tryptophan contributes to serum NAM roughly an order of
magnitude more than NA.
Figure 2.5. Contributors to NAD biosynthesis in vivo in mice. (a) Concentration of NAD
contributors (log scale, mean ± s.d., n=4). (b) Schematic of tryptophan (Trp) and NAM tracer
metabolism. 13C-Trp was infused via jugular vein at 5nmol/g/min and 2H-NAM at
0.3nmol/g/min; Tryptophan to NAD flux (f1), NA to NAD flux (f2), NAM uptake from
circulation (f3), and NAMPT flux (f4). (c) Serum and tissue isotope labeling of NAM from 5 h
[U-13C] Trp infusion (left), or from 5 h 13C-NA infusion (right) (mean ± s.d., n=3). (d) Serum
isotope labeling of NAM from 2H-NAM infusion. Symbols, experimental data (mean ± s.d.,
n=3); lines are to guide the eye. (e) NAM labeling from 2H-NAM infusion. (f) Labeled
28
NADP(H) relative to labeled NAD(H) in tissues after 5 h 2H-NAM infusion. (g) NAD(H)
concentration across tissues. (h) Labeled fractions of NAM, NAD and NADPH in tissues after 1
h, 2 h, 5 h of 2H-NAM infusion. For (e) -(h), data are mean ± s.d., n=3.
Infusion of [2,4,5,6-2H] NAM at a consistent rate of 0.2 nmol per gram per min resulted in
approximately 50% serum NAM labeling, with a rapid increase in NAM M+4 and slow
accumulation of NAM M+3, which is formed by assimilation of NAM M+4 into NAD, loss of
the redox-active hydrogen, and subsequent cleavage of NAD to NAM (Figure 2.5d). Tissue
NAM was less labeled than serum NAM, with the extent of labeled NAM assimilation variable
across organs (Figure 2.5e). Thus, in contrast to cell lines where NAM exchange with the media
is fast, in vivo, exchange between the blood stream and tissues is slow and thus potentially an
important site of regulation.
The extent of recycling of assimilated NAM M+4 into NAM M+3 varied by organ, being
greatest in spleen and small intestine and least in skeletal muscle, suggesting rapid NAD
turnover in spleen and small intestine and slow turnover in muscle (Figure 2.5e). Next, we
measured NAM, NAD and NADPH tissue labeling at multiple time points (for concentration, see
Appendix Table A4). NADPH labeled detectably more slowly than NAD, and the relative
labeling of NADP(H) and NAD(H) (Figure 2.5f) allowed us to caculate NAD kinase forward
flux and NADP(H) turnover. Particularly slow NADPH labeling was observed in lung. Like in
cell culture, the NAD kinase forward flux is a modest NAD consumer, accounting for ~25% of
total NAD production flux replenishing NAD-NAM cycle (quantitatively, the sum of f1 +f2 +f3 in
Figure 2.5b). Skeletal muscle showed the greatest lag between NAM and NAD labeling, and the
29
slowest NAD labeling overall, confirming slow NAD turnover, whereas spleen and small
intestine showed the fastest NAD labeling (Figure 2.5e).
To gain a more complete picture of tissue-specific NAD metabolism, we used the NAM-tracing,
Trp-tracing, and NA-tracing data to quantitate NAD fluxes in each tissue (f1 , f2 , f3 , f4 in Figure
2.5b; Appendix Table A5). The flux model assumes metabolic (but not isotopic) steady state
with excretion into serum as the main NAM sink. It does not overtly consider the route of
terminal NAM elimination from the body, although we did observe that methyl-NAM, which
likely plays an important role in NAM elimination, shows indistinguishable labeling across
tissues, indicating rapid sharing of methyl-NAM (unlike NAM itself) throughout the body via the
circulation (Appendix Figure A6). The resulting optimized flux set (Figure 2.6a; Appendix Table
A5) accurately predicted labeling patterns after co-infusion of [U-13C] Trp and [2,4,5,6-2H]
NAM (20:1 ratio, equal to their physiological ratio in serum), and co-infusion of [U-13C]NA and
[2,4,5,6-2H] NAM (1:10 ratio, equal to their ratio in serum) (Appendix Figure A7).
This quantitative analysis confirmed that liver is the main producer of circulating NAM from
tryptophan, with kidney also net excreting NAM from both tryptophan and NA (Figure 2.6a).
Tissue fluxes are reported in units of molarity per time, i.e., are normalized to tissue volumes.
Correcting for the larger volume of liver relative to kidney, the fraction of total NAM production
by liver is > 95%. All other examined tissues were net NAM consumers, but differed
dramatically in their rates of NAD turnover, with small intestine and spleen having a flux more
than 40-fold greater than muscle or fat (Figure 2.6a,b). In contrast to cell lines, where flux
through NAD correlated more strongly with NAD concentration than turnover halftime, in vivo
the reverse was true (Figure 2.6 c,d). This indicates large tissue-specific differences in NAD
30
consumption pathway activities. Notably, while standard tissue culture cell lines showed similar
NAD turnover halftimes irrespective of their tissue of origin, halftimes varied by 50-fold across
tissues in vivo, with the halftime for NAD turnover in small intestine more than 10-fold faster
than in any tested cultured cell line (Figure 2.6e). Based on the striking differences between
cultured cell lines and tissues in vivo, we examined fluxes in freshly isolated primary
hepatocytes. Like liver, and in contrast to HepG2 cells, the freshly isolated hepatocytes produced
NAD from tryptophan and manifested a fast NAD turnover time of ~ 2 h (Figure 2.6f). Thus,
mammalian NAD metabolism involves extensive tissue-specific pathway regulation which is not
replicated in standard cell lines.
Figure 2.6. NAD turnover in tissues. (a) Quantitative NAD fluxes in tissues, based on metabolic
flux analysis informed by LC-MS measurement of metabolite labeling in serum and tissues after
31
separate infusions of 13C-Trp, 13C-NA and 2H-NAM. Values shown are fluxes (unit: μM per
hour) from the best fit flux sets for network in (6b). For complete flux sets, see Table S5. Fluxes
shown for tryptophan and NA reflect net assimilation into NAD. For NAM, there is significant
net export from liver and kidney. For these 2 tissues, we show separately the uptake and
excretion fluxes of NAM, as determined by modeling of the tissue labeling data. For all other
tissues, NAM uptake and excretion are balanced, and we show only a single value corresponding
to the exchange rate between the tissue and circulation. (b) Total NAD production flux (f1 +f2 +f4)
across tissues and relevant NAD enzyme protein expression levels based on antibody staining
from http://www.proteinatlas.org/. (c, d) Across tissues, NAD production flux (panel b)
correlates with inverse labeling half-time but not NAD concentration. (e) NAD labeling halftime across cell lines and corresponding mouse tissues. (f) NAD labeling half-time and Trp
fractional contribution in HepG2 cells, primary hepatocytes, and in vivo liver. Bars are mean
with 95% confidence intervals.
2.3.5. Tracing the fate of NR and NMN
While tryptophan, NA, and NAM are the physiological circulating NAD precursors, NR and
NMN have garnered much attention as potential alternative precursors for use as nutraceuticals
to elevate NAD. These precursors can be incorporated into NAD without breaking the
nicotinamide-ribose linkage, allowing them to bypass the gating NAMPT reaction, which is
subject to feedback inhibition by NAD32,33. NR and NMN boost NAD levels in vitro and in vivo,
and have shown promise in a number of rodent disease models42–44. To probe their metabolism,
we employed versions of NR and NMN that are isotopically labeled on both the nicotinamide
32
and ribose moieties. This allowed us to distinguish NAD made directly from NR or NMN (M+2)
versus NAD made from NAM derived NR or NMN (M+1) (Figure 2.7a). While stable in tissue
culture media, both NR and NMN were quickly degraded to NAM in whole mouse blood (t1/2
3min) (Figure 2.7b, Supplementary Figure A4g). Accordingly, we flash-froze blood specimens
and then later extracted with -80°C methanol (80:20). NR and NMN were administered by
intravenous bolus or oral gavage at a relatively low dose (50 mg/kg). This dose stays close to
normal physiology; the larger boluses (400-1000 mg/kg) used in some studies may be
metabolized differently32. The limit of detection for measurement of NR and NMN were 0.1nM
and 0.2nM. Readily detectable concentrations of intact NR were observed in the blood following
IV injection, but not after oral administration, indicating nearly complete first-pass metabolism
(Figure 2.7d). NMN was barely detectable even after IV administration; its IV dosing did,
however, result in a rise in circulating NR. Irrespective of the route of delivery, the main
circulating product of the administered NR or NMN was NAM, which rose ~20x within 5 min
of IV NR or NMN; oral NR or NMN administration led to a more modest rise in circulating
NAM (Figure 2.7c).
Examination of tissue NAD labeling indicated some direct assimilation of oral NR and NMN
into liver NAD, based on M+2 labeling that made up a minority of the signal, but was
nonetheless readily detectable. The active formation of liver NAD from NR and NMN is
consistent with both compounds being subject to substantial hepatic first pass metabolism. In
contrast, extrahepatic tissues displayed minimal M+2 NAD (Figure 2.7e), suggesting that orally
delivered NR and NMN are converted into NAM before reaching the systemic circulation. IV
injection of NR or NMN, on the other hand, resulted in substantial M+2 NAD in both liver and
kidney. In the brain, we detected only M+1 NAD, indicating a reliance on circulating NAM and
33
suggesting that intact NR and NMN may not cross the blood-brain barrier. Interestingly, NR but
not NMN was efficiently assimilated intact into NAD in muscle. To our knowledge, this is the
first clear example of a differential metabolic effect between these two compounds in vivo. Thus,
tissue-specific utilization of these compounds should be considered in the design of future NADboosting drugs.
Figure 2.7. NR and NMN are effectively delivered to tissues by IV, but not oral administration.
(a) Schematic of 2H,13C-NR and 2H,13C-NMN metabolism in vivo. NAD made directly from NR
or NMN is M+2 labelled. NAD made from NAM derived NR or NMN is M+1 labeled.
Previously made NAD, or NAD made unlabeled NAM is unlabeled (M+0). (b) Stability of NR
34
and NMN standards in PBS, DMEM with 10% DFBS, mouse serum, or mouse blood. Symbols
are experimental data (mean ± s.d., n=3); lines are single exponential fits. (c) Circulating NAM
from tail bleeds at the indicated times after a 50 mg/kg bolus of 2H,13C-NR or 2H,13C-NMN by
oral gavage or by IV injection. (d) Corresponding circulating NR and NMN. (e) Corresponding
tissue NAD labeling. Data are mean ± s.d., n = 3.
2.4. Discussion
NAD plays a central role in epigenetics and energy metabolism. It is accordingly important to
measure NAD production and consumption pathways, and how they differ across cell types,
tissues, physiological states, and diseases, a how they respond to perturbation by drugs and
nutraceuticals. Here we present an isotopic tracing approach to quantify NAD synthesis and
consumption fluxes: introduction of labeled NAM or other NAD-precursors followed by
measurement of NAD labeling. Both NAM and NAD are sufficiently abundant and stable for
facile measurement of their quantitative labeling by LC-MS, rendering the methods well suited
for broad application.
In steadily growing cell lines, NAD labeling follows single-exponential kinetics (Figure 2.1b).
The disappearance rate of unlabeled NAD in the presence of labeled NAM reflects total
consumption pathway activity. By tracing label incorporation into NADP(H) we showed NAD
kinase accounts for 10% of NAD consumption (Figure 2.2). By combining this isotope tracer
measurement with pharmacological modulation of PARP1/2 and SIRT1/2, we were able to
assign each enzyme class a substantial (~ 1/3) role in NAD consumption under basal conditions
35
(Figure 2.3j). As expected, cells defective in DNA repair or suffering acute DNA damage had
faster PARP-mediated NAD consumption, which validated our method, and quantified the effect
of DNA damage on flux through the PARPs for the first time. In contrast, neither PARP
expression levels nor activity in lysate were predictive of the basal PARP-mediated NAD
consumption flux in cell lines. We did not observe substantial NAD consumption by CD38 in
cell culture (based on inhibition with quercetin and apigenin, Appendix Figure A2h), although
genetic evidence suggests that CD38 plays a substantial role in NAD consumption in vivo45,46.
Typical cell culture media contains only two potential NAD precursors, NAM and tryptophan47.
In our hands, primary hepatocytes were the only cell type capable of using tryptophan for NAD
synthesis, indicating that the vast majority of cells depend entirely on NAM. In animals, gene
data indicate expression of the enzymes required for de novo synthesis of NAD from tryptophan
in liver and kidney (Appendix Figure A5d) and the concentration of tryptophan in the diet has
been reported to impact the liver NAD levels48. Consistent with this, quantitative analysis of in
vivo tracing data with labeled NAM and tryptophan indicated de novo NAD synthesis from
tryptophan in kidney and, to a much greater extent, liver. Other tissues, in contrast, relied almost
exclusively on circulating NAM made by the liver. Liver synthesis of NAD and excretion of
NAM occurred even when serum NAM was elevated by co-infusion of tryptophan and NAM;
thus, liver constitutively produces NAM to support NAD synthesis throughout the rest of the
body (Figure 2.6a).
By exploring the response of NAD levels and fluxes to candidate NAD-boosting nutraceuticals,
and measuring NR breakdown during assimilation, we were able to draw new conclusions
potentially relevant to treatment of cancer and age-dependent pathologies. By feeding dual
36
labeled NR we proved that most cultured cell types incorporate NR without breaking the bond
between its nicotinamide and ribose components (Appendix Figure A4d).
To explore the relationship between NAD concentration and fluxes, we changed media levels of
NAM and NR, as well as added FK866, thereby manipulating the intracellular NAD
concentration in cultured cells across an ~ 10-fold range. NAD consumption flux correlated
strongly with NAD concentration; this correlation results in NAD turnover time being relatively
consistent (~ 8 h, substantially longer than the 1-2 h half life previously estimated for
DH98/AH2 cells, which were not included in the present study26,27). The simplest explanation for
the correlation between NAD concentration and flux is that consumption flux is a linear function
of the concentration of NAD, the enzymes’ substrate. According to Michaelis-Menten kinetics,
such a linear relationship is expected only when substrate is sub-saturating. We observed an
average whole cell concentration of NAD ranging from 0.1 – 2 mM, with the T47D cells in
which we conducted the nutrient perturbation experiments having 0.6 mM. While this is similar
to or below the Km of NAD kinase (0.6 - 1 mM)49, it exceeds the reported NAD Km of PARP1
(0.1-0.2 mM) 50, 51, 52 and most of the (quite variable) literature estimates of sirtuin Km values
(0.01 to 0.6 mM). While these biochemical data suggest that PARPs and sirtuins should be
substantially saturated at 0.6 mM NAD, physiological Km values are often higher than those
measured in a test tube, due to active site competition from other metabolites in the cellular
milieu53. In addition, NAD and NADH are often protein bound and the free NAD concentrations
within cytosol and/or mitochondria may be considerably less than the whole-cell averages or the
Km values for consuming enzymes.38 Thus, the simplest biochemical explanation for the
correlation between NAD concentrations and fluxes is a roughly linear dependence of PARP and
sirtuin activity on NAD concentration.
37
In contrast to the variation in NAD concentration in different cell lines, NAD concentrations
were relatively consistent across mouse tissues, while NAD turnover rates varied dramatically
(Figure 2.6e). In several tissues, NAD turnover was substantially faster than in any of the
cultured cell lines that we examined. On the flipside, in skeletal muscle, it was substantially
slower. This variation in NAD turnover rate between tissues in vivo, highlights the importance of
understanding the mechanisms controlling NAD fluxes across tissues. We did not observe strong
correlation across tissues between flux and NAD concentration or the protein levels of known
NAD consuming enzymes (Figure 2.6b-c). Measurements of NMNAT1 lysate activity4 align
well with NMNAT1 protein levels across tissues but do not align particularly closely with the
measured tissue fluxes. This may reflect regulation of these enzymes by other means, such as
partner proteins or subcellular localization, or that other major NAD consumption pathways may
remain to be discovered. For example, one open question is CD38 orientation and regulation.
CD38 is thought to be a major sink of NAD in tissues, especially in older mice, as inferred from
the effects of genetic ablation on NAD levels54,55. However, in its standard ectoenzyme
orientation, where the active site is not exposed to the cytoplasm, CD38 may not be active.
Under some conditions, or in some tissues, it may be expressed in an inverted orientation or on
an intracellular membrane, making it much more active8. This kind of topological regulation
would not be captured in gene expression or lysate biochemical data. Clearly, much remains to
be learned concerning NAD metabolism in tissues, distinct from tissue culture. We note, for
example, that the hepatocellular carcinoma cells line HepG2 exhibits no NAD production from
tryptophan and much slower NAD flux than mouse liver. This kind of differential would be
masked if only steady state NAD concentration was measured, emphasizing the importance of
flux assays.
38
We also explored the metabolism of two NAD precursors that have recently received attention
for their ability to elevate tissue NAD levels, NR and NMN. Interestingly, we found that neither
compound was able to enter the circulation intact in substantial quantities when delivered orally.
While the dose that we used (50 mg/kg) was modest in order to avoid severe metabolic
perturbation, our result is consistent with our previous finding that 200 mg/kg oral NR
contributes directly to NAD synthesis in liver, but not skeletal muscle33. Similarly, in the present
experiment, lack of direct tissue assimilation of orally administered NR or NMN is evident in the
labeling pattern of tissue NAD. Direct assimilation of M+2 NR or NMN would yield M+2 NAD.
Turnover of M+2 NAD within a tissue could in principle produce M+1 NAD after direct NR or
NMN assimilation, but our independent measurements of tissue NAD turnover (Figure 2.5)
revealed that these fluxes are too slow to account for the lack of M+2 tissue NAD. Another
hypothetical possibility is base exchange56,57. Without formally ruling out such a possibility, we
observed that IV administration of either compound results in its detection within the circulation
(albeit to a much greater extent for NR) and a robust M+2 peak in the kidney, proving that the
route of delivery has a profound effect on the ability of these precursors to reach target tissues.
Surprisingly, IV NR was much more effective than NMN for labeling the NAD pool in skeletal
muscle. This is consistent with the proposal that at least some tissues are incapable of taking up
NMN directly32,38. On the other hand, direct transport of NMN would allow its utilization even in
tissues that lack NRK or NAMPT activity. Thus, it will be extremely important to consider
tissue-specific enzyme and transporter expression when using NAD precursors therapeutically.
Overall, by developing broadly applicable NAD tracing methods, we have been able to gather a
substantial body of foundational data regarding NAD metabolism, which collectively provide a
valuable resource for future research. In some cases, such as liver being the main site of NAD de
39
novo synthesis, we are able to validate hypotheses based on expression data. In other cases, such
as NAD consumption by PARP in culture, we find that biochemical data does not predict
metabolic fluxes. Perhaps most importantly, we identify many distinguishing features of the in
vivo context, such as high variability in NAD turnover across tissues, which emphasize the
importance of future in vivo tracing in aging, disease states, and genetically engineered mouse
models. NAD flux tracing should be of great value in aging research and in development of
therapies that boost NAD levels.
2.5. Methods
2.5.1. Cell culture
The cancer cell lines (MCF7, T47D, MDA-MB-231, MDA-MB-468, HepG2, Panc1, 8988T,
HCT116, SK-MEL-2 and SK-MEL-28) were obtained from the American Type Culture
Collection (ATCC, Manassas, VA). XPA-restored and XPA-deficient cell lines were a kind gift
of Dr. Vilhelm A. Bohr’s lab.33 Cancer cells and XPA cells were grown in Dulbecco’s modified
eagle media (DMEM, Cellgro, 10-017) with 10% fetal bovine serum (FBS; Gibco, heatinactivated). 3T3-L1 pre-adipocytes were obtained from ATCC and differentiated as reported47.
C2C12 cell line was obtained from ATCC, maintained in DMEM supplemented with 20% FBS,
and differentiated with DMEM containing 2% donor equine serum (GE Healthcare Life
Sciences) and 1 µM insulin (Sigma). Mouse primary hepatocytes were cultured in William’s
medium E supplemented with ITS (BD Biosciences) and dexamethasone48, and were transferred
into isotopic medium 12 h after implantation. Cell number was determined with an automatic
40
cell counter (Invitrogen). Packed cell volume was determined with PCV tubes (TPP). For
metabolomics experiments, cells were transferred into isotopic medium with 10% dialyzed FBS
at different time (from 0.5 h to 60 h) before being harvested. For labeling > 24 h, isotopic
medium was refreshed daily.
2.5.2. siRNAs, antibodies, and drugs
siRNA of QPRT (sc-62914) and control siRNA were obtaind from Santa Cruz. PA. The
antibodies against the following proteins for western blot were purchased from the indicated
sources: PAR (Trevigen, 4336-BPC-100, 1:1000 dilution), QPRT () and β-actin (Abcam,
ab8229, 1:2000 dilution). The drugs for perturbing NAD synthesis or consumption were
purchased from the indicated sources: FK866 (Cayman Chemical, 13287, 100nM),
olapardaviddavidib (10 µM), sirtinol (Sigma, S7942, 20 µM), EX527 (Sigma, E7034, 10 µM),
zeocin (Invitrogen, 1360033, 250 µg per ml), gallotannin (Sigma, 1643328, 100 µM). PAR in
cellular lysates was detected as described32.
2.5.3. Isotope labeling
[2,4,5,6-2H] NAM and [U-13C] Trp were from Cambridge Isotope Laboratories and [U-13C] NA
was from Sigma. Isotopic NR (nicotinamide 7-13C, ribose 2-2H) was synthesized as described20.
Unlabeled compounds (NAM, NA, Trp, β-Nicotinamide mononucleotide, NAD, NADH, NADP
and NADPH) were purchased from Sigma. DMEM with isotopic NAM was prepared from
scratch following DMEM formula without NAM and supplemented with isotopic form of NAM
41
(32 µM). Isotope-labeled Trptophan medium was prepared from scratch following DMEM
formula without Trptophan (or NAM in Appendix Figure A1a) and supplemented with isotopic
form of Trptophan (80 µM). Isotopic medium was supplemented with 10% dialyzed FBS
(Sigma), for C2C12 only, 2% donor equine serum.
2.5.4. Intravenous infusion of wildtype C57BL/6 mice
Animal studies followed protocols approved by the Princeton University Institutional Animal
Care and Use Committee. In vivo infusion was performed on 12-14 week old C57BL/6 mice precatheterized on the right jugular vein (Charles River Laboratories, Wilmington, MA). The mice
were on normal light cycle (8 AM – 8 PM). The mouse infusion setup (Instech Laboratories,
Plymouth Meeting, PA) included a tether and swivel system so that the animal had free
movement in the cage. Isotope-labeled metabolites were prepared as solutions in normal saline
(100 mM for [U-13C] Trp, 4 mM for [2,4,5,6-2H] NAM, or combined both with same
concentration) and infused via the catheter at a constant rate of 1 µL per 20 g per min. Blood
samples (~20 µl) were collected by tail bleeding, placed on ice in the absence of anticoagulant,
and centrifuged at 16,000g for 5 min at 4oC to isolate serum. At the end of the infusion, the
mouse was euthanized by cervical dislocation and tissues were quickly dissected and snap frozen
in liquid nitrogen with pre-cooled Wollenberger clamp. Serum and tissue samples were kept at 80oC before metabolite extraction for mass spectrometry analysis.
42
2.5.5. Metabolite measurements in cell lines
Cells were grown in 6-well plates (Corning). For steady state labeling of metabolites, labeled
medium was replaced every day, and additionally 2 hours before extracting metabolites.
Metabolism was quenched and metabolites were extracted by aspirating media and immediately
adding 1 mL -80°C 80:20 methanol: water. For intracellular metabolites which are present in
medium (i.e. NAM, Trptophan), cells were washed with 37°C phosphate buffered saline for 3
times before adding -80°C 80:20 methanol: water. After 20 min of incubation on dry ice, the
resulting mixture was scraped, collected into a centrifuge tube, and centrifuged at 10,000 g for 5
min at 4°C. The supernatants were analyzed within 24 h by liquid chromatography coupled to a
mass spectrometer (LC-MS).
The LC–MS method involved hydrophilic interaction chromatography (HILIC) coupled to the Q Exactive
PLUS mass spectrometer (Thermo Scientific). The LC separation was performed on a XBridge BEH
Amide column (150 mm × 2.1 mm, 2.5 μm particle size, Waters, Milford, MA). Solvent A is 95%: 5%
H2O: Acetonitrile with 20 mM Ammonium Bicarbonate, and solvent B is Acetonitrile. The gradient was
0 min, 85% B; 2 min, 85% B; 3 min, 80% B; 5 min, 80% B; 6 min, 75% B; 7 min, 75% B; 8 min, 70% B;
9 min, 70% B; 10 min, 50% B; 12 min, 50% B; 13 min, 25% B; 16 min, 25% B; 18 min, 0% B; 23 min,
0% B; 24 min, 85% B; 30 min, 85% B. Other LC parameters are, flow rate 150 µl/min, column
temperature 25 °C, injection volume 5 μL. The mass spectrometer was operated in positive ion mode for
the detection of NAM and NR, and negative ion mode for other metabolites. Other MS parameters are:
resolution of 140,000 at m/z 200, automatic gain control (AGC) target at 3e6, maximum injection time of
30 ms and scan range of m/z 75-1000.
All isotope labeling patterns were corrected for natural abundance using AccuCor (manuscript
under review). The correction matrices are calculated from the chemical formula and the mass of
43
the metabolite. The labeling pattern vector is solved by taking the inverse of the correction
matrix multiplied by the measure mass distribution vector.
2.5.6. Metabolite measurements in serum and tissues
Serum was thawed on ice before adding -80°C 80:20 methanol: water with a volume of 20 µL
solvent per µL serum, vortexed, incubated on ice for 10 min, and centrifuged at 16,000 g for 10
min, with the supernatant used for LC-MS analysis. Frozen tissues were weighed, ground with a
cryomill (Retsch) at 25 Hz for 30 seconds before adding -20°C tissue extraction solution
(40:40:20 acetonitrile: methanol: water) with a volume of 40 µL solvent per mg tissue, and
incubated on ice for 20 min. Tissue samples were then centrifuged at 16,000 g for 20 min. The
supernants were transferred to new tubes and centrifuged again at 16,000 g for 20 min to remove
any residual debris before analysis. To obtain absolute metabolite concentrations, internal
standards (unlabeled NAD, NADH, NADP, NADPH, NAM) were added directly to the initial
quenching and extraction solvent. Supernatants were analyzed within 24 h by LC-MS.
2.5.7. Quantification in cell lines of NAD synthesis fluxes and of NAD dilution
by cell growth
After switching to medium with labeled NAM, the cellular NAM is almost completely labeled
within the first hour (Figure 2.1b, left). For simplicity, we treat the labeling of cellular NAM as if
it occurred instantaneously at t=0. The unlabeled fraction of NAD (NADU, Figure 2.1b)
decreases as
44
dNADU (𝑡)
dt
=−
𝑓𝑖𝑛
[NAD]
NADU (𝑡)
(1)
where 𝑓𝑖𝑛 is the total NAD synthesis flux and [NAD] is the sum of intracellular NAD and NADH
concentration. The kinetic equation for the unlabeled fraction is given by the solution to Eqn. (1),
i.e.,
𝑓
NADU (𝑡) = 𝑒
𝑖𝑛 ⋅𝑡
−[NAD]
(2)
The best estimation of 𝑓𝑖𝑛 was acquired by minimizing the deviation of model predicted NADU
and the measured values. For example, in the case of Figure 2.1b (T47D cells), this fitting yields
𝑓
𝑖𝑛
a value of 0.077 h-1 for the rate constant [𝑁𝐴𝐷]
(corresponding to a turnover half time 𝑡1/2 ≈ 9
hr ). Since [𝑁𝐴𝐷] in T47D cells is 1880 pmol per million cells, we then obtained 𝑓𝑖𝑛 to be 144
pmol per million cells per hour. 95% CI was determined by Monto Carlo method. All the NADU
were randomly generated according to a t-distribution with measurened mean and variance, with
the central 95% region to be CI.
Due to the exponential growth of the cells, part of this total NAD synthesis flux goes to pool
expansion. The growth demand fgrowth was determined by growth and NAD pool (Eqn.3).
fgrowth = g [NAD]
(3)
where 𝑔 is the growth rate constant, determined by cell number (N) measurement over time
𝑑𝑁
𝑑𝑡
𝑔𝑁. For T47D cells, 𝑔 = 0.015 h-1 (corresponding to a doubling time of 46 hr). Growth rates
were calculated using the software package Origin by fitting to an exponential, as mean ± 95%
confidence interval. We thus get 𝑓𝑔𝑟𝑜𝑤𝑡ℎ = 28± 2 pmol per million cells per hour, which is
45
=
approximately 20% of the total NAD synthesis flux. The gap between 𝑓𝑖𝑛 and fgrowth., 118 pmol
per million cells per hour, is the enzymatic NAD consumption flux.
2.5.8. Quantification of NAD consumption fluxes by NAD kinase, PARPs,
Sirtuins, and in cells with acute DNA damage
To quantify the NAD consumption flux by NAD kinase (𝑓𝑁𝐴𝐷𝐾 ), we note that after switching to
medium with labeled NAM the labeled fraction of NADP (NADPL) follows
dNADPL (t)
dt
𝑓
𝑁𝐴𝐷𝐾
=(NADL (t)-NADPL (t)) [NADP]
(4)
where the kinetics of NADL (t) is given by
dNADL (𝑡)
dt
𝑓
𝑖𝑛
= [NAD]
(1 − NADL (𝑡))
(5)
Eqn (4) can be solved analytically, implying a unique flux solution.29 Best estimation of 𝑓𝑁𝐴𝐷𝐾 is
obtained by minimizing the deviation of the calculated NADPL and the measured values.
NADPL(t) can be calculated from Eqn (4)-(5) with previously determined 𝑓𝑖𝑛 (144 pmol per
million cells per hour), measured [NAD] (constatnt total intracellular NAD and NADH
concentration, 1880 pmol per million cells) and [NADP] (constatnt total intracellular NADP and
NADPH concentration, 27 pmol per million cells). 95% CI was determined by Monto Carlo
method. In each iteration, all the NADPL were randomly generated according to a t-distribution
based on the measured mean and variance. The optimal 𝑓𝑁𝐴𝐷𝐾 was calculated from each iteration
and the central 95% region is the CI.
46
To calculate consumption fluxes by PARPs and Sirtiuns, we blocked the fluxes with their
respective inhibitors while switching to labeled medium, and followed the labeling kinetics. As
the inhibitor does not affect the synthesis flux 𝑓𝑖𝑛 (based on experimental data showing that
accumulation of labeled is unaltered), we model the labeled NAD pool ([NADL ]) and unlabeled
NAD pool ([NADU ]) as
d[NADL ]
dt
[NADL ]
= 𝑓𝑖𝑛 − [NAD
L ]+[NADU ]
⋅ 𝑓𝑜𝑢𝑡 (6)
and
d[NADU ]
dt
[NADU ]
= − [NAD
L ]+[NADU ]
⋅ 𝑓𝑜𝑢𝑡
(7)
Since the initial conditions are known ([NADU](t=0) = [NAD], [NADL](t=0) = 0), with
previously determined 𝑓𝑖𝑛 (144 pmol per million cells per hour), [NADL](t) and [NADU](t) can
be calculated for any assumed value of 𝑓𝑜𝑢𝑡 . The best estimation of 𝑓𝑜𝑢𝑡 is acquired by
minimizing the deviation of model predicted [NADL] and [NADU] and the measured values. 95%
CI was determined by Monto Carlo method. In each iteration, all the [NADL] and [NADU] were
randomly generated according to a t-distribution with measured mean and variance. The 𝑓𝑜𝑢𝑡 was
calculated from each iteration and the central 95% region is the CI.
2.5.9. Quantification of NAD fluxes in vivo
We infused [U-13C] Trp (Trp11, all 11 carbons are labeled), [U-13C] NA (NA6, all 6 carbons are
labeled) and [2,4,5,6-2H] NAM (NAM4, nicotinamide with all hydrogen on the ring labeled)
separately to mice to determine fluxes. Both Trp11 and NA6 resulted in NAD6 (NAD with all
47
carbons on the nicotinamide part labeled) and then NAMTissue,6. NAMTissue,6 was then exchanged
between tissues and circulation (NAM Serum,6) before being taken by tissues to make NAD. NAD3
was made directly from NAM4 (one deuteron of NAM4 becomes the redox-active deuteron of
NAD and thus is quickly lost). Breakdown of NAD3 yields NAM3.
In each organ, as shown in Figure 2.5b, 4 NAD metabolic fluxes are calculated assuming
metabolic steady state in each tissue: 𝑓1 is NAD de novo synthesis flux from tryptophan, 𝑓2 is
NAD synthesis flux from NA, 𝑓3 is NAD synthesis from tissue nicotinamide (NAM), and 𝑓4 is
the flux of NAM being taken up from serum. At metabolic steady state, the NAD and
nicotinamide concentrations in tissue stay constant. Therefore the mass balance suggests the
corresponding breakdown (NAD NAM) and excretion (tissue NAM circulation) fluxes are
fully determined by the production fluxes above, and thus are not included as separate variables
in the model. The following set of differential equations are used to calculate the tissue NAD and
NAM labeling patterns at each time point.
dNAD0
dt
dNAD3
dt
=
dNAD6
dt
dNAMTissue0
dt
dNAMTissue3
dt
[𝑓1 (Trp0 −NAD0 )+ 𝑓2 (NA0 −NAD0 )+𝑓4 (NAMTissue 0 −NAD0 )]
=
cNAD
(−NAD
)+𝑓
(−NAD
)+𝑓
[𝑓1
3
2
3
4 (NAMTissue 3 +NAMTissue 4 −NAD3 )]
cNAD
=
[𝑓1 (Trp11 −NAD6 )+𝑓2 (NA6 −NAD6 )+𝑓4 (NAMTissue 6 −NAD6 )]
=
=
dNAMTissue4
dt
dNAMTissue6
{
dt
=
cNAD
[(𝑓1 +𝑓2 +𝑓4 )(NAD0 −NAMTissue0 )+𝑓3 (NAMSerum 0 −NAMTissue 0 )]
cNAM
[(𝑓1 +𝑓2 +𝑓4 )(NAD3 −NAMTissue3 )+𝑓3 (NAMSerum 3 −NAMTissue 3 )]
=
(8)
cNAM
[(𝑓1 +𝑓2 +𝑓4 )(−NAMTissue4 )+𝑓3 (NAMSerum 4 −NAMTissue 4 )]
cNAM
[(𝑓1 +𝑓2 +𝑓4 )(NAD6 −NAMTissue6 )+𝑓3 (NAMSerum 6 −NAMTissue 6 )]
cNAM
In the equations, NADi represent the labeling fraction of mass isotopomer M+i of tissue NAD.
NAMTissue i and NAMSerum i represent the labeling fraction of tissue NAM and serum NAM M+i,
48
respectively. Trp11 and NA6 represent the labeling fraction of serum tryptophan and serum NA,
respectively. cNAD and cNAM are tissue concentrations of NAD(H) and NAM, respectively (in
nmol/gram tissue weight).
Tryptophan and NA reached steady state in serum within 30 min, therefore Trp11 and NA6 were
treated as constants (60% and 85%, respectively). Serum NAM labeling changes as a function of
time. In our differential equations, we did not simulate the serum NAM labeling. Instead, the
serum NAM labeling was measured experimentally at a few time points, and the empirical
labeling kinetics was obtained through polynomial interpolation. At t=0, NADM+0, NAMM+0 and
NADPHM+0 are 1, while all other fractions are 0. For any given set of the four fluxes, the
dynamic labeling patterns can be calculated from the differential equations. The calculated
values were then compared to the measured labeling patterns (1 h, 2 h, 5 h during [2,4,5,6-2H]
NAM infusion, 5 h after [U-13C] Trp infusion, 5 h after [U-13C] NA infusion). The best estimated
flux set is achieved by minimizing the deviation between the calculated labeling patterns and the
measured ones. The deviation in each labeled fraction is weighted by the reciprocal of the
standard deviation of the replicate experimental labeling measurements. The numerical
simulation of the differential equations were performed in R with the deSolve package and the
optimization was performed with minqa package48. 95% confidence intervals were estimated by
(i) starting from the best-scoring flux distribution, (ii) changing the specific flux, (iii) choosing a
combination of other fluxes which give minimal increase in the Var-SSR, (iv) determining the
increase in the objective function Var-SSR and using an increase of 3.84 as the cutoff for 95%
confidence interval49. The goodness of fit was evaluated by chi-square test (χ20.05(df=15)=25, See
Supplementary Appendix Table A5 for the sum of squared residuals (SSR) value for every
tissue).
49
As a validation of the flux estimation, the optimal set of fluxes determined as above were to
predict the labeling pattern of tissue NAM and NAD upon co-infusion of [U-13C] Trp combined
with [2,4,5,6-2H] NAM, and separately of [U-13C] NA combined with [2,4,5,6-2H] NAM, where
the same doses tracers were used as for the individual tracing experiments (5 nmol per gram per
min for [U-13C] Trp, 0.2 nmol per gram per min for [2,4,5,6-2H] NAM, 0.02 nmol per gram per
min for [U-13C] NA). The predicted labeling data were then compared to the measured values
(see Appendix Figure A7).
2.6. References
1.
Pollak, N., Dölle, C. & Ziegler, M. The power to reduce: pyridine nucleotides – small
molecules with a multitude of functions. Biochem. J. 402, 205–218 (2007).
2.
Hassa, P. O., Haenni, S. S., Elser, M. & Hottiger, M. O. Nuclear ADP-ribosylation
reactions in mammalian cells: where are we today and where are we going? Microbiol.
Mol. Biol. Rev. 70, 789–829 (2006).
3.
Bogan, K. L. & Brenner, C. Nicotinic acid, nicotinamide, and nicotinamide riboside: a
molecular evaluation of NAD+ precursor vitamins in human nutrition. Annu. Rev. Nutr.
28, 115–130 (2008).
4.
Mori, V. et al. Metabolic profiling of alternative NAD biosynthetic routes in mouse
tissues. PLoS One 9, 1–27 (2014).
5.
Haigis, M. C. & Sinclair, D. a. Mammalian Sirtuins: Biological Insights and Disease
Relevance. Annu. Rev. Pathol. 5, 253–295 (2010).
50
6.
Rouleau, M., Patel, A., Hendzel, M. J., Kaufmann, S. H. & Poirier, G. G. PARP
inhibition: PARP1 and beyond. Nat. Rev. Cancer 10, 293–301 (2010).
7.
Malavasi, F. et al. Evolution and Function of the ADP Ribosyl Cyclase / CD38 Gene
Family in Physiology and Pathology. Physiol. Rev. 88, 841–886 (2008).
8.
Zhao, Y. J., Zhu, W. J., Wang, X. W., Zhang, L. H. & Lee, H. C. Determinants of the
membrane orientation of a calcium signaling enzyme CD38. Biochim. Biophys. Acta Mol. Cell Res. 1853, 2095–2103 (2014).
9.
Chini, C., Tarrago, M. & Chini, E. NAD and the aging process: Role in life, death and
everything in between. Mol. Cell. Endocrinol. (2016).
10.
Fang, E. F. et al. Nuclear DNA damage signalling to mitochondria in ageing. Nat. Rev.
Mol. Cell Biol. 17, 308–321 (2016).
11.
van de Ven, R. a. H., Santos, D. & Haigis, M. C. Mitochondrial Sirtuins and Molecular
Mechanisms of Aging. Trends Mol. Med. 23, 320–331 (2017).
12.
Hasmann, M. & Schemainda, I. FK866, a Highly Specific Noncompetitive Inhibitor of
Nicotinamide Phosphoribosyltransferase, Represents a Novel Mechanism for Induction of
Tumor Cell Apoptosis. Cancer Res. 63, 7436–7442 (2003).
13.
Davar, D., Beumer, J. H., Hamieh, L. & Tawbi, H. Role of PARP Inhibitors in Cancer
Biology and Therapy D. Curr Med Chem 19, 3907–39921 (2012).
14.
Pirinen, E. et al. Pharmacological Inhibition of poly(ADP-ribose) polymerases improves
fitness and mitochondrial function in skeletal muscle. Cell Metab. 19, 1034–1041 (2014).
15.
Fang, E. F. et al. Defective mitophagy in XPA via PARP-1 hyperactivation and NAD
51
+/SIRT1 reduction. Cell 157, 882–896 (2014).
16.
Virag, L., Robaszkiewicz, A., Rodriguez-Vargas, J. M. & Oliver, F. J. Poly(ADP-ribose)
signaling in cell death. Mol. Aspects Med. 34, 1153–1167 (2013).
17.
Fouquerel, E. et al. ARTD1/PARP1 negatively regulates glycolysis by inhibiting
hexokinase 1 independent of NAD+ depletion. Cell Rep. 8, 1819–1831 (2014).
18.
Chini, C. C. S. et al. Targeting of NAD metabolism in pancreatic cancer cells: potential
novel therapy for pancreatic tumors. Clin. Cancer Res. 20, 120–30 (2014).
19.
Xiao, Y. et al. Dependence of tumor cell lines and patient-derived tumors on the NAD
salvage pathway renders them sensitive to NAMPT inhibition with GNE-618. Neoplasia
15, 1151–60 (2013).
20.
Wang, J. et al. A local mechanism mediates NAD-dependent protection of axon
degeneration. J. Cell Biol. 170, 349–355 (2005).
21.
Wang, G. et al. P7C3 Neuroprotective Chemicals Function by Activating the Ratelimiting Enzyme in NAD Salvage. Cell 158, 1324–1334 (2014).
22.
Bonkowski, M. s. & Sinclair, D. a. Slowing ageing by design: the rise of NAD+ and
sirtuin-activating compounds. Nat. Rev. Mol. Cell Biol. 17, 679–690 (2016).
23.
Chini, E. N. CD38 as a regulator of cellular NAD: a novel potential pharmacological
target for metabolic conditions. Curr. Pharm. Des. 15, 57–63 (2009).
24.
Ryu, D. et al. NAD+ repletion improves muscle function in muscular dystrophy and
counters global PARylation. Sci. Transl. Med. 8, 1–15 (2016).
25.
Trammell, S. a. J. et al. Nicotinamide riboside is uniquely and orally bioavailable in mice
52
and humans. Nat. Commun. 7, 12948 (2016).
26.
Hillyard, D., Rechsteiner, M. & Olivera, B. Pyridine nucleotide metabolism in mammalian
cells in culture. J. Cell. Physiol. 82, 165–179 (1973).
27.
Rechsteiner, M., Hillyard, D. & Olivera, B. Turnover at nicotinamide adenine dinucleotide
in cultures of human cells. J. Cell. Physiol. 88, 207–217 (1976).
28.
Rechsteiner, M., Hillyard, D. & Olivera, B. Magnitude and significance of NAD turnover
in human cell line D98/AH2. Nature 259, 695–6 (1976).
29.
Hayaishi, O., Ijichi, H. & Ichiyama, A. Studies on the biosynthesis of NAD by a direct
method of tracing metabolism in vivo. Adv. Enzyme Regul. 5, 9–22 (1967).
30.
Ijichi, H., Ichiyama, A. & Hayaishi, O. Studies on the Biosynthesis of Nicotinamide
Adenine Dinucleotide. J. Biol. Chem. 241, 3701–3707 (1966).
31.
Trammell, S. A. & Brenner, C. Targeted, LCMS-based Metabolomics for Quantitative
Measurement of NAD(+) Metabolites. Comput. Struct. Biotechnol. J. 4, e201301012
(2013).
32.
Ratajczak, J. et al. NRK1 controls nicotinamide mononucleotide and nicotinamide
riboside metabolism in mammalian cells. Nat. Commun. 7, 13103 (2016).
33.
Frederick, D. W. et al. Loss of NAD Homeostasis Leads to Progressive and Reversible
Degeneration of Skeletal Muscle. Cell Metab. 24, 269–282 (2016).
34.
Schreiber, V., Dantzer, F., Ame, J.-C. & de Murcia, G. Poly(ADP-ribose): novel functions
for an old molecule. Nat. Rev. Mol. Cell Biol. 7, 517–28 (2006).
35.
Buncel, E. & Lee, C. Isotopes in hydrogen transfer processes. (1976).
53
36.
Yuan, J., Bennett, B. D. & Rabinowitz, J. D. Kinetic flux profiling for quantitation of
cellular metabolic fluxes. Nat. Protoc. 3, 1328–40 (2008).
37.
Menear, K. a. et al. 4-[3-(4-Cyclopropanecarbonylpiperazine-1-carbonyl)-4-fluorobenzyl]
-2H-phthalazin-1-one: A novel bioavailable inhibitor of poly(ADP-ribose) polymerase-1.
J. Med. Chem. 51, 6581–6591 (2008).
38.
Nikiforov, A., Do, C., Niere, M. & Ziegler, M. Pathways and Subcellular
Compartmentation of NAD Biosynthesis in Human Cells FROM ENTRY OF
EXTRACELLULAR PRECURSORS TO MITOCHONDRIAL NAD. J. Biol. Chem. 286,
21767–21778 (2011).
39.
Krukenberg, K. a., Jiang, R., Steen, J. a. & Mitchison, T. J. Basal activity of a PARP1NuA4 complex varies dramatically across cancer cell lines. Cell Rep. 8, 1808–1818
(2014).
40.
Zong, W. X., Ditsworth, D., Bauer, D. E., Wang, Z. Q. & Thompson, C. B. Alkylating
DNA damage stimulates a regulated form of necrotic cell death. Genes Dev. 18, 1272–
1282 (2004).
41.
Zerp, S., Vens, C., Floot, B., Verheij, M. & Triest, B. NAD+ depletion by APO866 in
combination with radiation in a prostate cancer model, results from an in vitro and in vivo
study. Radiother. Oncol. 11, 348–354 (2014).
42.
Canto, C. et al. The NAD + precursor nicotinamide riboside enhances oxidative
metabolism and protects against high-fat diet induced obesity. Cell Metab. 15, 838–847
(2012).
54
43.
Revollo, J. R. et al. Nampt/PBEF/visfatin regulates insulin secretion in β cells as a
systemic NAD biosynthetic enzyme. Cell Metab. 6, 363–375 (2007).
44.
NAD+ metabolism: Bioenergetics, signaling and manipulation for therapy. Biochim.
Biophys. Acta - Proteins Proteomics 1864, 1787–1800 (2016).
45.
Chiang, S. H. et al. Genetic ablation of CD38 protects against Western diet-induced
exercise intolerance and metabolic inflexibility. PLoS One 10, 1–19 (2015).
46.
Sahar, S., Nin, V., Barbosa, M. T., Chini, E. N. & Sassone-Corsi, P. Altered behavioral
and metabolic circadian rhythms in mice with disrupted NAD + oscillation. Aging
(Albany. NY). 3, 794–802 (2011).
47.
Recommended Dietary Allowances: 10th Edition. (1989).
48.
Powanda, M. & Wannemacher, R. Evidence for a linear correlation between the level of
dietary tryptophan and hepatic NAD concentration and for a systematic variation in tissue
NAD concentration in the mouse and the rat. 1471–1478 (1970).
49.
Ohashi, K., Kawai, S. & Murata, K. Identification and characterization of a human
mitochondrial NAD kinase. Nat. Commun. 3, 1248–1249 (2012).
50.
Gibson, B. A. et al. Chemical Genetic Discovery of PARP Targets Reveals a Role for
PARP-1 in Transcription Elongation Bryan. Science (80-. ). 353, 45–50 (2016).
51.
Langelier, M. F., Ruhl, D. D., Planck, J. L., Kraus, W. L. & Pascal, J. M. The Zn3 domain
of human poly(ADP-ribose) polymerase-1 (PARP-1) functions in both DNA-dependent
poly(ADP-ribose) synthesis activity and chromatin compaction. J. Biol. Chem. 285,
18877–18887 (2010).
55
52.
Beneke, S., Alvarez-Gonzalez, R. & Bürkle, a. Comparative characterisation of
poly(ADP-ribose) polymerase-1 from two mammalian species with different life span.
Exp. Gerontol. 35, 989–1002 (2000).
53.
Yuan, J. et al. Metabolomics-driven quantitative analysis of ammonia assimilation in E.
coli. Mol. Syst. Biol. 5, 302 (2009).
54.
Camacho-Pereira, J. et al. CD38 Dictates Age-Related NAD Decline and Mitochondrial
Dysfunction through an SIRT3-Dependent Mechanism. Cell Metab. 23, 1127–1139
(2016).
55.
Chiang, S. H. et al. Genetic ablation of CD38 protects against Western diet-induced
exercise intolerance and metabolic inflexibility. PLoS One 10, 1–19 (2015).
56.
Sauve, A. A., Munshi, C., Lee, H. C. & Schramm, V. L. The Reaction Mechanism for
CD38. A Single Intermediate Is Responsible for Cyclization, Hydrolysis, and BaseExchange Chemistries. Biochemistry 37, 13239–13249 (1998).
57.
Sauve, A. A. & Schramm, V. L. Sir2 Regulation by Nicotinamide Results from Switching
between Base Exchange and Deacetylation Chemistry. Biochemistry 42, 9249–9256
(2003).
58.
Liu, L. et al. Malic enzyme tracers reveal hypoxia-induced switch in adipocyte NADPH
pathway usage. Nat. Chem. Biol. (2016). doi:10.1038/nchembio.2047
59.
He, L., Meng, S., Germain-Lee, E. L., Radovick, S. & Wondisford, F. E. Potential
biomarker of metformin action. J. Endocrinol. 221, 363–369 (2014).
60.
Su, X., Lu, W. & Rabinowitz, J. D. Metabolite Spectral Accuracy on Orbitraps. Anal.
56
Chem. 89, 5940–5948 (2017).
61.
Soetaert, K., Petzoldt, T. & Setzer, R. W. Package deSolve : Solving Initial Value
Differential Equations in R. J. Stat. Softw. 33, 1–25 (2010).
62.
Antoniewicz, M. R., Kelleher, J. K. & Stephanopoulos, G. Determination of confidence
intervals of metabolic fluxes estimated from stable isotope measurements. Metab. Eng. 8,
324–337 (2006).
57
Chapter 3 NAD is transported into mammalian
mitochondria
3.1. Abstract
Mitochondrial NAD levels influence fuel selection, circadian rhythms, and cell survival under
stress. It has alternately been argued that mitochondrial NAD arises from import of cytosolic
nicotinamide (NAM), nicotinamide mononucleotide (NMN), or NAD itself. We report that
isolated mitochondria generate NAD from NMN, but not from NAM. However, newly
synthesized NAD primarily appears outside, rather than inside the organelles. Treating intact
cells with nicotinamide riboside that is isotopically labeled on both the nicotinamide and ribose
moieties results in the appearance of doubly labeled NAD within mitochondria, unequivocally
demonstrating that nicotinamide-containing nucleotides are transported into the organelles.
Under conditions that favor labeling of NAD over NMN in the cytosol, labeling of mitochondrial
nucleotides tracks that of NAD, indicating that intact NAD (or NADH) is transported. Our
results challenge the long-held view that the mitochondrial inner membrane is impermeable to
pyridine nucleotides and suggest the existence of an unrecognized mammalian NAD(H)
transporter.
__________________________________________________
Reproduced with permission from Antonio Davila, Ling Liu, Karthikeyani Chellappa, Philip
Redpath, Eiko Nakamaru-Ogiso, Zhigang Zhang, Marie Migaud, Joshua Rabinowitz, and Joseph
Baur.
Under review, eLife.
58
3.2. Introduction
Nicotinamide adenine dinucleotide (NAD) is an essential reduction-oxidation (redox) cofactor as
well as a cosubstrate for a growing list of enzymes. Within the mitochondria, NAD accepts
electrons from a variety of sources and transfers them to complex I of the electron transport
chain, ultimately resulting in the generation of ATP. In addition, NAD serves as a cosubstrate
for mitochondrial sirtuins and NAD glycohydrolases1. Mitochondrial NAD levels vary in a
circadian fashion and can directly influence fuel selection2, as well as determine cell survival
under stress3. Despite these observations, the mechanisms responsible for generating and
maintaining the mitochondrial NAD pool remain incompletely understood.
NAD can be synthesized de novo from tryptophan or via the Preiss-Handler pathway from
nicotinic acid, but recycling of the nicotinamide generated by continuous enzymatic cleavage of
NAD within the body requires the NAD salvage pathway. This consists of two enzymes:
Nicotinamide phosphoribosyltransferase (NAMPT), which produces nicotinamide
mononucleotide (NMN) in what is considered the rate-limiting step4, and Nicotinamide
mononucleotide adenylyltransferases (NMNATs), which convert NMN to NAD. Three isoforms
of NMNAT have been reported, with NMNAT1 localized to the nucleus, NMNAT2 to the Golgi
apparatus and neuronal axons, and NMNAT3 to the mitochondria, providing the first evidence
that mitochondria contain some of the machinery to maintain their own NAD pool5. Nampt is
primarily nuclear and cytosolic, however, a small portion co-purifies with mitochondria from
live3. Thus, it was suggested that mitochondria contain a complete NAD salvage pathway and
might recycle their own nicotinamide or take it up from the cytosol. Subsequently, Pittelli and
colleagues failed to detect NAMPT in mitochondria purified from HeLa cells and presented
59
immunofluorescence evidence that it was excluded from the mitochondrial matrix6.
Accordingly, it was proposed that cytosolic NMN is taken up into mitochondria and converted to
NAD via NMNAT3 to generate the mitochondrial NAD pool7. However, Felici et al reported
that the full-length transcript for NMNAT3 is not expressed in HEK293 cells, nor in a variety of
mammalian tissues, and that instead the endogenous gene produces two splice variants, one of
which produces a cytosolic protein, and the other of which produces a mitochondrial protein
involved in NAD cleavage rather than synthesis (FKSG76)8. Interestingly, mice lacking
NMNAT3 were reported to have defects primarily in erythrocytes, which lack mitochondria, and
to have normal NAD levels in heart, muscle, and liver and normal mitochondrial NAD content in
multiple tissues 9,10. Felici et al went on to show that providing intact NAD, but not any
metabolic precursor, restores the mitochondrial NAD pool in cells that overexpress FKSG76.
They concluded that mitochondria do not synthesize NAD at all, but rather take it up intact from
the cytosol, which in turn, can take up NAD from the extracellular space. This interpretation is
at odds with recent findings which show that NAD and NMN must first undergo extracellular
degradation to nicotinamide, nicotinic acid, or nicotinamide riboside in order to be taken up into
cells7,11. Moreover, while yeast and plant mitochondria are known to contain NAD transporters,
no mammalian counterparts have been described. Thus, the source of mitochondrial NAD
remains to be firmly established.
Here we present evidence that mitochondria directly import NAD. Consistent with previous
reports of NMNAT activity in mitochondrial lysates, we find that isolated mitochondria can
synthesize NAD from NMN, but not from nicotinamide. However, the majority of this activity
is dependent on NMNAT1, which is not mitochondrial, and results in the production of NAD
outside of the organelles, rather than filling of the matrix. Using intact myotubes, we
60
demonstrate that isotopically labeled nicotinamide riboside, which is converted to NMN by
nicotinamide riboside kinases (NRKs) 12, contributes directly to the mitochondrial NAD pool
without shuttling through an intermediary step as nicotinamide. Substituting labeled nicotinic
acid riboside, which generates NAD via cytosolic NAD synthase, also results in labeling of
mitochondrial NAD, suggesting that fully formed NAD, rather than NMN, is transported.
3.3. Experimental Procedures
3.3.1. Mitochondrial Isolation from skeletal muscle
Male C57BL/6 mice were euthanized by cervical dislocation, and their gastrocnemius and
quadriceps muscles were dissected and placed immediately in ice-cold muscle homogenization
buffer (100mM KCl, 50mM Tris-HCl (pH 7.4), 5mM MgCl2, 1mM EDTA (pH 8.0) and 1.8mM
ATP) at pH 7.2. The entire procedure was performed at 4°C. The fat and connective tissues were
removed and the muscle tissue was chopped into small pieces. The chopped muscle was
incubated for 2 minutes in protease medium (60U of protease from Bacillus lichenformis
(Sigma) per mL of homogenization buffer), washed twice with homogenization buffer, and
transferred to an ice-cold Teflon Potter Elvehjem homogenizer containing homogenization
buffer. The muscle was homogenized using a motor-driven homogenizer for 10 minutes at 150
rpm. A small aliquot of the homogenate was then removed and stored at -80°C for further
analysis. The volume of the remaining homogenate was doubled with homogenization buffer
and centrifuged at 720xg for 5 minutes at 4°C. The pellet was resuspended in homogenization
61
buffer and centrifuged for an additional 5 minutes at 720 x g. The supernatants were combined
and centrifuged at 10,000xg for 20 minutes at 4°C. The supernatant was discarded and the pellet
was resuspended in homogenization buffer and further centrifuged for 10 minutes at 10,000 x g.
The final mitochondrial pellet was resuspended in resuspension buffer (225mM sucrose, 44mM
KH2PO4, 12.5mM Mg-acetate, and 6mM EDTA; pH 7.4) and maintained on ice. Mitochondrial
protein content was quantified using the Micro BCA Protein Assay Kit (Thermo Scientific).
3.3.2. Mitochondrial Treatments
For all experiments, purified mitochondria containing 100ug of total protein were resuspended in
ice-cold or pre-warmed MirO5 respiration buffer (Oroboros) containing the indicated compounds
at a final concentration of 1ug/uL. Pyruvate, Malate, ADP, β-NMN, PRPP, FCCP and
Oligomycin were purchased from Sigma. NAD and NADH were from Roche. Gallotannin was
from Enzo Life Sciences. For timed incubation experiments, the mitochondrial suspensions were
maintained at 37°C in a shaking heat block with the tube caps opened. For NAD and NADH
determination from the mitochondrial suspension, 50ug of mitochondrial protein were
transferred to tubes containing 10% (v/v) of either Perchloric Acid (Sigma) or KOH (Sigma) to
achieve final concentrations of 0.6M or 0.1M, respectively. The mitochondrial lysates were
vortexed vigorously and maintained on ice or stored at -70°C. Prior to storage or analysis, the
KOH lysate were incubated at 55°C for 10 minutes to degrade any residual NAD, then cooled on
ice for 5 minutes.
62
3.3.3. NAD-NADH Cycling Assay
Immediately prior to analysis, mitochondrial lysates were diluted 1:10 in ice-cold phosphate
buffer (pH 8). 5 L of this dilution was then subjected to an enzymatic cycling assay in a 100 μL
total volume as described previously 13. Briefly, NAD standards or diluted mitochondrial extracts
were added to a cycling mixture consisting of 2% ethanol, 100 g/ml alcohol dehydrogenase, 10
g/ml diaphorase, 20 M resazurin, 10 M flavin mononucleotide, 10 mM nicotinamide, 0.1% BSA
in 100 mM phosphate buffer, pH 8.0. The cycling reaction was incubated at room temperature,
and the appearance of resorufin (generated during each oxidation-reduction cycle) was measured
by fluorescence excitation at 544 nm and emission at 590 nm.
3.3.4. Cell culture
C2C12 myoblasts were cultured in Dulbecco’s modified Eagle’s medium (DMEM)
supplemented with 4.5g/L D-Glucose, 2mM Glutamine, 10% FBS and antibiotics. Care was
taken to maintain these cells within the log phase of growth and to avoid allowing them to
become confluent. For differentiation into myotubes, the cells were grown to confluence,
washed once with DPBS (Gibco) and the media was replaced with DMEM containing 2% Horse
serum (Gibco) overnight. Following this, the media was replaced every day for 7 days with
DMEM containing 2% Horse serum and 1µM insulin (modified from prior literature14).
63
3.3.5. Generation of CRISPR cell lines
The CRISPR/Cas9 system was used to target each of the three individual isoforms of NMNAT in
C2C12 cells. For each isoform, two separate guide RNA sequences (gRNA) were targeted
toward the 3’ end of the coding region and were designed using the CRISPR design tool
(http://crispr.mit.edu). A sequence from the ROSA 26 genes (R26) was used as a control. The
gRNA sequences are listed in Appendix Table B1. The gRNAs were cloned into the
LentiCRISPR v2 vector backbone (Addgene, #52961) between Esp3I sites downstream of the
hU6 promoter. Lentivirus was produced by co-transfection of the lentiviral transfer vector with
the pMD2-G envelope and psPAX2 packaging into 293 cells using Fugene 6 transfection reagent
(Promega). The media was changed 24 hours following transfection. The virus-containing
supernatant was collected 48 hours post-transfection and filtered through a 0.22μm syringe filter
to eliminate cells. C2C12 myoblasts were infected with virus in media containing 8μg/mL
hexadinethrine (Sigma) in a dropwise manner with gentle swirling. 24 hours following infection,
the virus was removed and the cells were selected in 1.5μg/mL Puromycin (Gibco).
3.3.6. HPLC analysis of NMN in mitochondria isolated from liver and skeletal
muscle
For determination of NMN, the PCA supernatant was further neutralized with 1 M potassium
carbonate and centrifuged to remove insoluble material. Samples were stored at -80 °C and
subjected to HPLC analysis. Separation of NMN was carried out on an YMC-Pack ODS-A
column (5 um, 4.6 x 250 mm) at 30 °C. Flow rate was set at 0.4 mL/min. The mobile phase was
64
initially 100% of mobile phase A (0.1 M potassium phosphate buffer, pH 6.0) for the first 8 min.
Then, the methanol was lineally increased with mobile phase B (0.1 M potassium phosphate
buffer, pH 6.0, containing 30% methanol) increasing to 50% over 7 minutes. The column was
washed after each separation by increasing mobile phase B to 100% for 3 min. UV absorbance
was monitored at 260 and 340 nm with Shimadzu SPD-M20A. Pertinent peak areas were
integrated by the LabSolution software from Shimadzu, and quantified using standard curves and
normalized to mitochondrial protein content.
3.3.7. Tracer studies
We designed double isotope-labeled nicotinamide riboside (NR) and nicotinic acid riboside
(NAR) tracers, with a single 13C and a single deuterium on the nicotinamide and ribose moieties,
respectively (Fig 4a). Direct incorporation of the intact tracer into NAD yields double-labeled
NAD, whereas breakdown and resynthesis by the salvage pathway of any cell yields singlelabeled NAD (Fig 4 A). The synthesis of the labelled NR was reported previously 15. The
synthesis of the 2H, 13C NAR was accomplished as follows:
13
C-Nicotinamide was hydrolysed
under basic aqueous conditions to generate 13C-nicotinic acid, which following silylation was
coupled to the 2D-tetraacetylated riboside under Vorbruggen conditions to yield the triacetylated
2
H, 13C-NAR. Standard deprotection conditions employing NH3g-MeOH at -20oC for 4 days
were employed to the generate 2H, 13C NAR. 2H, 13C NAR was isolated as a mixture of /
anomers present in a 15:85 ratio, which could not be successfully separated. This /
distribution proves reproducible, and is not observed for the non-labelled NAR (1H NMR, 13C
NMR, MS, HRMS). The 1H NMR spectra of labeled and unlabeled NAR are provided in the
65
supplementary materials (Appendix Figure B1). ESI-MS m/z 258.0926 (M+H); Exact mass
calculated for (12C1213C11H132H1N1O6; M+H) 258.0917; found 258.0926.
3.3.8. Cell culture and isotopic labeling
For the tracer studies, C2C12 myotubes were treated with double-isotope labeled 0.1mM
nicotinamide riboside (NR) or nicotinic acid riboside (NAR) in complete culture medium for 4
hours before extracting metabolites to ensure steady state-labeling. Following the labeling
treatment, the cells were rapidly harvested, were washed once with DPBS and 10% of the
volume was removed and re-pelleted. To this pellet, 200µL of 80:20 methanol:water (supercooled to -80°C) was added, vortexed vigorously and maintained on dry ice until processing as
described below.
Mitochondria were isolated from the remaining 90% of the cells by a method modified from
Trounce et al 16. Briefly, the cells which were pelleted and resuspended in a mitochondrial
isolation buffer (H-buffer) consisting of 210mM mannitol, 70mM sucrose, 1mM EGTA, 5mM
HEPES, 0.5% BSA, pH 7.2. The cells were physically sheared in an ice-cold glass-glass dounce
homgenizer then centrifuged at low-speed (720 x g for 10 minutes, 4°C). The supernatant
(containing the mitochondria was transferred to a separate tube, and pellet underwent a repeated
round of homogenization and centrifugation. The supernatants were combined and further
purified for the removal of cell debris through additional rounds of low speed spins. The
resultant supernatant was subjected to two rounds of high speed centrifugation (10,000 x g for 30
minutes total, 4°C). The resultant pellets of purified mitochondria were dissolved in cold
resuspension buffer (225mM sucrose, 44mM KH2PO4, 12.5mM Mg-acetate, and 6mM EDTA;
66
pH 7.4) and briefly spun (10,000 x g for 2 minutes, 4°C) in order to remove the mannitol from
which interfered with the mass-spectrometry measurement.
Metabolism was quenched and metabolites were extracted by aspirating the wash buffer and
immediately adding 500µL -super-cooled 80% methanol. After 30 min of incubation on dry ice,
the resulting mixture was centrifuged at 10,000 g for 5 min. The alcohol supernatants were
evaporated under nitrogen and resuspended in 200µL water. Metabolite ion counts were
normalized to fraction of the whole. NAM and NMN quantification was performed by adding
standard compounds to the solution.
3.3.9. LC-MS Instrumentation and method development
Nicotinamide, NMN, NR, and NAD+, NAMN, NAR and NAAD+ were analyzed within 24 hours
by reversed-phase ion pairing chromatography coupled with positive-mode electrosprayionization on a Q Exactive hybrid quadrupole-orbitrap mass spectrometer (Thermo); Liquid
chromatography separation was achieved on a Poroshell 120 Bonus-RP column (2.1 mm ×150
mm, 2.7 μm particle size, Agilent). The total run time is 25 min, with a flow rate of 50 μl/min
from 0 min to 12 min and 200μl/min from 12 min to 25 min. Solvent A is 98: 2 water:
acetonitrile with 10 mM amino acetate and 0.1 % acetic acid; solvent B is acetonitrile. The
gradient is 0-70 % B in 12 min 17.
67
3.3.10. Statistics
Results are expressed as mean ± standard error of the mean. Comparison between two groups
was performed using Students t or Mann Whitney test depending on the normality of the data
distribution. All statistical analysis were performed using Prism 6 (GraphPad Software, Inc).
3.4. Results
3.4.1. NMN increases NAD levels in isolated mitochondria
We initially tested whether NAD levels would increase over time in isolated mitochondria
incubated with NAD precursors. In the absence of exogenous metabolizable substrates (state 1 as
defined18,19), warming mitochondria isolated from murine skeletal muscle resulted in a rapid loss
of NAD(H) content (data not shown). With the addition of substrate (pyruvate/malate, state 2)
and ADP (state 3), the rate of NAD loss was progressively slowed, and co-incubation with
NMN, but not nicotinamide or nicotinic acid was found to maintain NAD levels near the starting
value (Figure 3.1a). To discern whether increased NAD content in the presence of NMN truly
reflected new synthesis, rather than slowed degradation, we held mitochondria in state 2 for 30
minutes to establish a reduced NAD content before the addition of ADP to induce state 3 with or
without NMN. Supplementation with NMN restored mitochondrial NAD content in a time and
concentration-dependent manner (Figure 3.1b-d). Synthesis of NAD from NMN also appears to
be at least partially dependent on membrane potential, as addition of the uncoupler FCCP or the
complex I inhibitor rotenone significantly attenuated the rate of NAD appearance (Figure 3.1e).
68
Figure 3.1. Mitochondria synthesize NAD from nicotinamide mononucleotide. (a)
Mitochondria isolated from murine skeletal muscle were maintained for 30 min at 37°C with
shaking in respiratory state 3 (MirO5 respiration buffer containing 10mM Pyruvate, 5uM Malate,
12.5mM ADP) supplemented with 0.5mM NAM, NA, or NMN. (b) Mitochondria initially held
for 30 min in state 2 (MirO5 respiration buffer containing 10mM Pyruvate, 5uM Malate; 37°C
with shaking) were then supplemented with NMN alone or NMN + ADP and incubated for an
additional 30 minutes at 37°C. (c) Time course of mitochondrial NAD levels before and after
addition of NMN or NMN + ADP. (d) Isolated mitochondria were held in state 2 for 30 min
before adding ADP to stimulate state 3 respiration for 60 min in the presence of increasing
amounts of NMN added concomitantly with ADP. (e) Isolated mitochondria were maintained in
state 2 at 37°C with shaking for 30 min and then transitioned to state 3 in the absence or presence
of NMN (0.5mM), FCCP (4uM), or rotenone (ROT; 0.5uM) and incubating for an additional 60
69
min at 37°C with shaking. The data shown are means ± SEM from biological duplicates of
multiple experiments. (*, P < 0.05; **, P < 0.001; ***, P < 0.0001; 2-tailed, unpaired Student’s ttest)
3.4.2. NAD synthesis in isolated mitochondria involves NMNAT, but not
Nampt
In contrast to incubation with NMN, incubation of NAD-deficient mitochondria with
nicotinamide did not affect NAD concentration (Figure 3.2a). This was true whether or not
exogenous phosphoribosyl- pyrophosphate (PRPP, the second substrate for the Nampt reaction)
was supplied. Because the localization of Nampt to mitochondria was described in organelles
derived from the liver, we also repeated this experiment with liver-derived mitochondria.
Similar to muscle-derived mitochondria, liver-derived organelles synthesized NAD readily from
NMN, but were incapable of utilizing nicotinamide to a measureable degree, whether or not
PRPP was provided (Figure 3.2b). To further investigate the involvement of NAD salvage
enzymes, we employed specific inhibitors of Nampt (FK866) and NMNAT (Gallotannin). As
expected, Gallotannin strongly reduced NAD synthesis from NMN (Figure 3.2c). However,
addition of FK866 had no effect, arguing against the possibility that NMN breaks down to
nicotinamide prior to incorporation into NAD.
70
Figure 3.2. NAD contents of mitochondria isolated from murine skeletal muscle or liver
(nmol/mg mitochondrial protein ± SEM). (a) Mitochondria isolated from murine skeletal muscle
were held in respiratory state 2 for 30 minutes at 37°C with shaking before adding ADP (state 3)
and incubating for 60 min in the absence or presence of 0.5mM of the precursors NMN, NAM,
PRPP, or NAM and PRPP. (b) Mitochondria isolated from murine liver were held in state 2 at
37°C for 30 minutes with shaking before the addition of ADP (state 3) in the presence or absence
of 0.5mM NMN, NAM or NAM and PRPP. (c) Muscle mitochondria were maintained in state 2
for 30 minutes before the addition of ADP (state 3) and further incubated at 37°C for 60 minutes
in the presence or absence of NMN and inhibitors Gallotannin (100uM) or FK866 (10nM). The
data shown are means ± SEM from biological duplicates of multiple experiments. (*, P < 0.05;
**, P < 0.005; ***, P < 0.0001; unpaired Student’s t-test)
3.4.3. Matrix NAD is not restored by NMN treatment in isolated
mitochondria.
Given that a decline in matrix NAD content will eventually limit respiratory capacity, we next
tested whether NMN treatment could restore the respiratory capacity of mitochondria that had
been held in state 2 for an extended period. Despite increasing NAD, NMN treatment did not
71
lead to recovery of state 3 respiration in isolated mitochondria (Figure 3.3a). This suggested two
possible interpretations: 1) that another form of mitochondrial damage unrelated to NAD content
limited respiration, or 2) that the newly synthesized NAD was not localized in the matrix where
it would be able to participate in mitochondrial metabolism. To test the latter possibility, we
pelleted mitochondria after NMN treatment and compared the NAD contents of the pellet and
supernatant to the whole mixture. Surprisingly, the increase in NAD was almost exclusively
outside of the organelles, with no rescue of matrix NAD content after NMN treatment (Figure
3.3b). We next considered the possibility that mitochondria are sparingly permeable to NAD
directly. While low concentrations of NAD failed to have a major impact on matrix NAD
content, high (5-10 mM) external NAD led to an appreciable increase. Notably, this
concentration is far in excess of whole cell or tissue NAD concentration (~300-1000 μM), but is
only slightly above our estimates for NAD concentration in the mitochondrial matrix (3-4 mM,
based on the approximation that 1 mg of mitochondrial protein corresponds to ~1µL of matrix
volume21). Thus, high external concentrations may be required to create a gradient that favors
import. Consistent with these findings, 10 mM external NAD prevented the loss of matrix NAD
content over time in mitochondria held in state 2, and significantly slowed the decline in
respiratory capacity (Figure 3.3 c-d).
72
Figure 3.3 Effect of NMN treatment in isolated mitochondria. (a) State 3 coupled mitochondrial
oxygen consumption. Isolated skeletal muscle mitochondria were measured directly from ice or
maintained in respiratory state 2 (MirO5 respiration buffer containing 10mM Pyruvate, 5µM
Malate) at 37°C with shaking for 60 minutes before adding 12.5mM ADP (state 3) with or
without 0.5mM NMN and incubated an additional 30 minutes at 37°C before being measured.
(b) Isolated skeletal muscle mitochondria were maintained in state 2 at 37°C with shaking for 30
minutes before adding ADP (state 3) with or without NMN and incubated an additional 60
minutes. The mitochondrial suspension was then either lysed directly in 0.6M perchloric acid
(final concentration) or centrifuged at 10,000xg for 2 minutes at 4°C to collect the supernatant
and subsequent washed pellet which were then treated with perchloric acid. (c, d) Isolated
skeletal muscle mitochondria were maintained in state 2 at 37°C with shaking for 30 minutes
73
before adding ADP (state 3) with or without 10mM NAD and returned to the incubation
conditions. At the indicated timepoints, aliquots were removed from the pooled mitochondrial
suspension and processed for NAD analysis of direct lysis, pellet and supernatant as previously
described, or analyzed for state 3 respiratory capacity using high-resolution respirometry.
Results are expressed as mean ± SEM. The data are representative of multiple experiments. (*, P
< 0.05; **, P < 0.005; ***, P < 0.0001; unpaired Student’s t-test)
3.4.4 Cytosolic NMN contributes to mitochondrial NAD
To test the behavior of mitochondria in intact cells with physiologically relevant cytosolic
concentrations of NAD and NMN, we next employed an isotopic labeling approach.
Nicotinamide riboside (NR) is taken up by cells and converted to NMN by nicotinamide riboside
kinases (NRKs)11,12. We treated intact C2C12 myotubes with NR that had been isotopically
labeled on both the nicotinamide ring and the ribose moiety, such that its incorporation into
NMN and subsequent conversion to NAD would result in retention of both heavy isotopes,
whereas degradation of NR by polynucleotide phosphorylase or enzymatic consumption of NAD
to generate nicotinamide would separate the labels (Figure 3.4a). We detected a high proportion
of doubly labeled NMN and NAD in mitochondria isolated from the myotubes, unequivocally
demonstrating that cytosolic NMN contributes to mitochondrial NAD without an intermediated
step involving degradation to nicotinamide (Figure 3.4b-c). The slightly more rapid appearance
of doubly-labeled NAD in intact whole cell lysates as compared to isolated mitochondria is
suggestive that at least some NAD synthesis is occurring outside of the organelles. Since NRK is
not present in mitochondria, NMN must be produced in the cytosol, but these data do not allow
74
us to distinguish whether mitochondrial NAD arises from conversion of imported NMN or from
direct uptake of cytosolic NAD.
Figure 3.4. Nicotinamide riboside is incorporated intact into mitochondrial NAD. (a)
Isotopically-labeled nicotinamide riboside (NR) was synthesized to contain a C-13 on the
pyridine carboxyl group and a deuterium on the ribose moiety. (b) Fractional labeling of NAD in
C2C12 whole cell lysate (WC) and isolated mitochondria (mito) following 4 hours of incubation
with double-labeled NR with or without gallotannin (Gallo; 100 μM). (c) Fractional labeling of
NMN found in C2C12 whole cell lysate (WC) and isolated mitochondria (mito) following 4
hours of incubation with double-labeled NR with or without gallotannin (Gallo; 100 μM). Data
shown are means ± SEM.
75
To discern whether mitochondria has the ability to directly import intact NAD, rather than
relying on synthesis from imported NMN, we repeated the isotopic labeling experiments using
nicotinic acid riboside (NAR). The processing of NAR to NAD requires the cytosolic enzyme
NAD synthase (NADS), which catalyzes the final step by amidating nicotinic acid adenine
dinucleotide (NaAD). Thus, NAD synthesis from this precursor should proceed via NAMN and
be strictly cytosolic. When NAD was labeled via NAR, we again observed nearly equivalent
labeling of the total and mitochondrial pools of both NAD and NMN (Figure 3.5 a-b), which was
puzzling, given that NMN is not an intermediate of NAD synthesis from NAR. Thus, we
considered several possibilities to explain the observed NMN labeling: 1) The labeled NAR
could have been contaminated with labeled NR, resulting in direct production of both NAMN
and NMN, 2) Given the much higher concentration of NAD in cells, non-enzymatic degradation
of a small amount of labeled NAD during extraction could account for a substantial portion of
the NMN signal, and 3) NMN could be generated from NAD through enzymatic processes such
as reverse flux through NMNATs or degradation of NADH by the Nudix hydrolase Nudt13 and
oxidation of the resulting NMNH 22,23. To be sure the parent NAR compound contained no
detectable NR contamination we tested it against mixtures of the two; a spike of as little as
0.01nM NR into 1µM M NAR was robustly detected, whereas no signal was present in the NAR
alone, thereby excluding the first possibility that labeled NMN arose from contaminating NR
(Figure 3.5c). Notably, our data also suggest that nicotinic acid-containing nucleotides are not
able to enter the mitochondria at all. While NAR was almost undetected by our techniques, we
observed a dramatic exclusion of NAMN and NaAD from the mitochondrial fractions (Figure
3.5d). This provides a second layer of specificity since both the enzyme and the substrate for the
NAD synthase reaction appear to be cytosolic.
76
Figure 3.5. Nicotinic acid riboside is incorporated intact into mitochondrial NAD. (a) Fractional
labeling of NAD in C2C12 whole cell lysates and isolated mitochondria following 4 hours of
incubation with doubly-labeled NAR. (b) Fractional labeling of NMN in C2C12 whole cell
lysates and isolated mitochondria following 4 hours of incubation with doubly-labeled NAR. (c)
Confirmation of the lack of NR contamination in NAR. 1uM NAR was combined with
increasing concentrations of NR (0-100nM) to demonstrate that NR is absent in the NAR and
readily detected by this methodology. (d) Total ion counts for NAAD and NAMN in whole cell
lysates and mitochondrial isolates from differentiated C2C12 cells treated with isotopicallylabeled NR or NAR tracers for 4 hours. Results expressed as means ± SEM.
77
3.4.5. Cytosolic NAD(H) is imported into the mitochondria
To distinguish between second and third possibilities (nonenzymatic and enzymatic generation
of NMN, respectively), and to obtain differential labeling of NMN and NAD that would allow us
to distinguish which species was taken up by mitochondria, we next employed a CRISPR-based
system to target each of the three NMNAT isoforms with two independent guide RNAs in
C2C12 myoblasts. All cell lines differentiated into myotubes with no apparent differences in size
or structure at the end of the week-long differentiation protocol. Loss of NMNAT1 protein
expression was verified by western blot, while we were unable to reliably detect NMNAT2 or
NMNAT3 using available antibodies. However, reduction of mRNA expression and loss of wild
type DNA sequence at the target sites were observed in the cell lines (Figure 3.6h). Myotube
NAD content was significantly reduced in the two lines targeting NMNAT1, as compared to
controls or lines targeting the other isoforms (Figure 3.6a). There were no significant differences
in mitochondrial NAD content in freshly isolated organelles (Figure 3.6b, ice). However,
organelles from the NMNAT1-targeted lines showed increased susceptibility to NAD depletion
by holding in state 2, and limited ability to synthesize NAD from NMN (Figure 3.6b), supporting
the model that the majority of NMNAT activity in mitochondrial preps arises from
contaminating NMNAT1, rather than matrix-localized NMNAT3.
Myotubes with NMNAT1 targeted had reduced NAD content and dramatically increased NMN
content in whole-cell lysates, consistent with a major role for this isoform in NAD synthesis
from NMN (Figure 3.6c). NMNAT2 or NMNAT3 targeting did not lead to obvious changes in
pyridine nucleotide distribution compared to control cells (Figure 3.6d). Intriguingly, treatment
of NMNAT1 targeted cells with NAR led to a large discrepancy in the fractional labeling of the
78
total NMN and NAD pools (Figure 3.6e). Since the fractional labeling of mitochondrial pyridine
nucleotide pools after addition of labeled NAR approached that of total NAD and far exceeded
that of total NMN (Figure 3.6f), our results indicate that NAD is taken up directly by
mitochondria under these conditions, unless NMN is compartmentalized such that a large pool of
unlabeled molecules is trapped within the myotubes but unavailable to the mitochondria. NAR
treatment was replicated in triplicate to confirm that the mitochondrial NAD and NMN pools are
significantly more enriched for double label than is the total NMN pool in NMNAT1-targeted
cells, supporting the model that mitochondrial pyridine nucleotides originate from imported
NAD (or NADH), rather than import of cytosolic NMN (Figure 3.6g-h).
Figure 3.6 Labeling of mitochondrial NAD tracks that of total NAD, but not of total NMN. For
all panel figures, data representing whole cells are depicted as solid bars, whereas data from
79
isolated mitochondria are shown with a stippled pattern. (a) Differentiated C2C12 parental and
LentiCRISPR transgenic myotubes were lysed and analyzed for NAD content from three
biological replicates. The cells are as follows: ctrl- parental line with no vector; R26- vector
control; 1a and 1b- two separate guide RNAs targeting NMNAT1; 2a and 2b- two separate guide
RNAs targeting NMNAT2; 3a and 3b- two separate guide RNAs targeting NMNAT3. (b)
Mitochondria isolated from differentiated C2C12 cells were held in state 2 (MirO5 respiration
buffer containing 10mM Pyruvate, 5uM Malate) at 37°C with shaking for 30 min. They were
then collected and lysed in perchloric acid immediately, or transitioned into state 3 by adding
ADP (12.5mM, final concentration) with or without supplementation with NMN (0.5mM, final
concentration) and maintained for 60 min at 37°C with shaking before collection. *, P < 0.05; **,
P < 0.001; 2-tailed, unpaired Student’s t-test versus R26. (c-d) Total ion counts of NAD and
NMN in extracts from C2C12 LentiCRISPR whole cells (c) and isolated mitochondria (d)
following a 4-hour incubation with isotopically-labeled NR or NAR tracer. (e-f) Fractional
labeling of metabolites (NAD and NMN) measured in C2C12 LentiCRISPR whole cells (e) and
isolated mitochondria (f) after a 4-hour incubation with isotopically-labeled NR or NAR tracer.
(g) Fractions of double-labeled NAD and NMN measured in C2C12 LentiCRISPR whole cell
and mitochondrial lysates following 4-hour incubation with isotope-labeled NAR (means ±
SEM). (h) Immunoblot confirming NMNAT1 knockout in CRISPR C2C12 cell line.
Although these data strongly support the conclusion that mitochondria take up NAD, they are
consistent with two interpretations concerning the source of labeled NMN. The lower fractional
labeling of NMN in the NMNAT1 targeted cells treated with NAR could be due to the
80
prevention of reverse flux through NMNAT1, or could reflect dilution of labeled NMN that is
generated non-enzymatically (during extraction) into the larger pool of unlabeled NMN that is
present in these cells. By varying the extraction conditions, we were able to confirm that
spontaneous hydrolysis of NAD to NMN does occur to some degree using our standard
extraction method for metabolomics studies (Figure 3.7a). However, by injecting methanolic
extracts directly into the LC-MS without a drying/concentration step, we were able to completely
avoid this artifact (Figure 3.7b). Repeating the NAR treatment using this method revealed very
low NMN levels in the whole cell lysates with almost no detectable labeling, whereas the
fractional labeling of NAD was consistent with that in previous experiments (Figure 3.7c).
Mitochondria isolated from these cells contained labeled NAD, confirming that they import fully
synthesized NAD from the cytosol. NMN in mitochondria was also labeled, and we speculate
that this reflects degradation of a small proportion NAD during the isolation process. While it
remains technically possible that cytosolic NADH could be converted to NMNH by Nudix
hydrolase activity, then rapidly imported and converted to mitochondrial NADH without
equilibrating with NMN, we were unable to detect labeling of NMNH in NAR-treated myotubes,
and thus view this as a remote possibility.
81
Figure 3.7. Direct injection of methanolic extracts reveals preferential labeling and
mitochondrial uptake of NAD over NMN. (a) Incubation of NAD at 37°C in water, but not 80%
methanol results in substantial degradation to NMN. Blue bars show unlabeled NMN resulting
from NAD degradation; Red bars indicate labeled NMN from spiked-in standard (1uM, dual
labeled). (b) NAD total ion count measured in parallel from same samples in (a). (c) NMN
concentration and labeling in differentiated C2C12 cells extracted with -80°C 80:20
methanol:water, analyzed either by hydrophilic interaction chromatography (no drying step), or
dried under N2, re-suspended in water and analyzed by reversed-phase ion-pairing
chromatography (with drying step). Blue bars show unlabeled NMN resulting from intracellular
NMN + NAD degradation after the drying step; Red bars indicate labeled NMN from spiked-in
standard (1uM, dual labeled). (d) NAD total ion count measured in parallel from same samples
in (a). (e) NAD and NMN labeling in differentiated C2C12 cells treated with dual labeled NAR
82
for 4 hours (whole cell vs. isolated mitochondria). Data are compiled from three biological
replicates and are displayed as means ± s.d.
3.5. Discussion
Mammalian mitochondria lack obvious homologues of the NAD transporters found in yeast and
plant mitochondria, raising the question of how they are able to obtain the cofactor. Evidence has
been presented in support of direct NAD uptake 8,24, or intramitochondrial synthesis from
nicotinamide or NMN 3,7,25. Our current results support the model that that direct uptake of intact
NAD contributes to the mitochondrial NAD pool. However, we note that we cannot exclude
further contributions from intramitochondrial NAD synthesis.
Yang et al. showed that a portion of Nampt co-purifies with mitochondria from liver, suggesting
the model that mitochondria contain an intact NAD salvage pathway, and take up nicotinamide,
rather than NMN or NAD 3. This proposal is consistent with earlier work by Grunicke and
coworkers showing that 14C-labeled nicotinamide incubated with isolated mitochondria is
incorporated into both NMN and NAD25. However, it is possible that an exchange reaction
catalyzed by NAD glycohydrolases (or sirtuins), rather than net biosynthesis could have been
responsible for the labeling observed in these experiments26. Moreover, we were not able to
observe net NAD synthesis when isolated mitochondria were supplied with nicotinamide, with or
without exogenous PRPP. Importantly, we cannot exclude that PRPP might need to be generated
within the mitochondrial matrix, or that mitochondrial. Nampt activity might be present in
certain cell types or under certain stresses. However, the present data do not support the ability
of mitochondria to synthesize NAD autonomously from nicotinamide, and we note that neither
83
Nampt nor PRPP synthetase has been reported as a mitochondrial protein in the recently updated
MitoCarta2.0 database27.
The mitochondrial localization of NMNAT3 strongly suggests that the organelles might be
capable of taking up and using NMN from the cytosol when required. In agreement with
previous studies detecting NMNAT activity in mitochondrial lysates5, 28-30, we demonstrate that
isolated mitochondria synthesize NAD from NMN. However, the use of intact organelles in our
experiments allowed us to discern that the vast majority of, if not all NAD generated from NMN
by isolated mitochondria ends up outside the matrix. Moreover, the bulk of this activity is lost
when mitochondria are isolated from myotubes lacking the nuclear isoform NMNAT1,
suggesting that it arises from small amounts of contamination in the mitochondrial preparations.
It is tempting to speculate that this might also account for the observation of Felici et al. that
their mitochondrial lysates contained NMNAT activity that was not attributable to any transcript
of the Nmnat3 gene8. Therefore, our data on isolated mitochondria do not provide direct evidence
for the ability of NMN import to contribute to mitochondrial NAD.
While mammalian mitochondria are generally considered to be impermeable to pyridine
nucleotides31,32, at least two studies have previously reported evidence for uptake of NAD.
Rustin et al. reported that direct addition of NAD restored mitochondrial NAD levels and
respiration rate in digitonin-permeabilized human cells that had reduced NAD content due to
extended culture without medium changes24, although it is not clear that a rapid breakdown and
resynthesis could be completely excluded in these experiments. Felici et al. reported evidence
that in HEK293 cells, brain, skeletal muscle, and kidney, the full-length transcript described for
NMNAT3 does not exist, and that instead, two splice variants are detectable, encoding a
84
cytosolic protein and the mitochondrial protein FKSG76, neither of which is translated at
detectable levels8. This observation is underscored by the lack of obvious phenotypes in most
tissues of mice lacking the NMNAT3 gene, with the exception of erythrocytes, which have
cytosolic NMNAT3 and no mitochondria9. Interestingly, overexpression of FKSG76
dramatically increases NMNAT activity in cell lysates, yet depletes NAD from the mitochondria
of intact cells. These depleted mitochondrial NAD levels can be rescued by exogenous NAD,
but not by any precursor, leading the authors to propose that intact NAD crosses the plasma
membrane and subsequently enters the mitochondria directly. Notably, the NAD precursors
provided by Felici et al. should all be incorporated into the nucleocytosolic pool of NAD, and
thus would be available to replenish mitochondrial NAD via direct transport. The lack of rescue
of FKSG76-depleted mitochondrial NAD levels after precursor treatment therefore implies that
either import of precursors or NAD synthesis from them is too slow to compete with the
degradation mechanism, whereas direct NAD influx is rapid, or that other aspects of NAD
synthesis are impaired in these cells. In addition, it has been reported by Nikiforov et al. that
pyridine nucleotides are not transported across cell membranes efficiently and are instead broken
down to the corresponding nucleosides or further before being taken up7. This model is distinctly
at odds with the finding of Felici et al. that extracellular NAD but not nicotinamide riboside is
able to restore mitochondrial NAD in cells overexpressing FKSG76.
Our studies using isotopically labeled NR and NAR unequivocally demonstrate that the
mitochondrial NAD pool can be established through direct import of NAD (or NADH). Using
doubly labeled NR resulted in nearly equivalent labeling of NMN and NAD in whole cell lysates
or mitochondria. The existence of doubly labeled NAD within the mitochondria in this
experiment proves that mitochondrial NAD synthesis does not require nicotinamide import (as
85
this would only carry a single label), but does not distinguish whether NMN or NAD was
transported. To accomplish this, we differentially labeled NAD and NMN by providing doubly
labeled NAR. NAR is converted to NAD in the cytosol via NAMN and NAAD, and therefore
should not label the NMN pool. Our initial experiment was compromised by hydrolysis of a
minority of the NAD to NMN during extraction, but when this technical hurdle was overcome,
either by CRISPR targeting of NMNAT1 to enlarge the NMN pool or by directly injecting
methanolic extracts into the LC-MS to avoid hydrolysis, the expected pattern of NAD labeling
without NMN labeling was obtained. Under these conditions, the mitochondrial pool of NAD
was also labeled, demonstrating that it originated from imported cytosolic NAD, rather than
NMN.
Our results indicate that mammalian mitochondria contain an NAD or NADH transporter. While
we are not the first to suggest that mitochondria can take up NAD(H), the identity of the putative
transporter in mammalian mitochondria has never been elucidated and its existence continues to
be debated. A number of proteins have been identified that allow NAD to cross membranes33,34,
but none of these have been shown to act in mitochondria35-37. The known member of the
mitochondrial solute carrier family that transports NAD, SLC25A17, has been localized
exclusively to peroxisomes, where it functions to exchange NAD, FAD and free CoA for
adenosine 3′,5′-diphosphate, FMN and AMP35,38. In yeast and plants, nucleoside
deoxyribosyltransferases transport NAD across the mitochondrial inner membrane from the
cytosol by exchanging AMP and GMP or more slowly by uniport35,39. However, candidate
mammalian NAD transporters identified based on sequence homology have proven to have
alternative targets (e.g., the mitochondrial folate carrier)3,36,40. Recently, the plant mitochondrial
NAD transporter, AtNDT2, was targeted and expressed in the mitochondrial membrane of
86
human HEK293 cells, which resulted in the redistribution of cellular NAD into mitochondria28.
Surprisingly, this led to a slower proliferation, a significant reduction oxidative respiration and a
dramatic loss of cellular ATP, which was attributed to a metabolic shift from oxidative
phosphorylation to glycolysis28. These results were interpreted to suggest that a mitochondrial
NAD transporter is unlikely to exist in human cells. Nonetheless, our findings support the ability
of mammalian mitochondria to import NAD and suggest that the toxicity of AtNDT2 may be
more related to its specific kinetics or regulation than to a generalizable effect of NAD transport.
Importantly, our findings do not exclude the possibility that NMN import and synthesis via
NMNAT3 also contribute to the mitochondrial NAD pool. Indeed, Cambronne et al. recently
employed a fluorescent biosensor to demonstrate that mitochondrial NAD levels are sensitive to
depletion of either NMNAT3 (mitochondrial) or NMNAT2 (Golgi/cytosolic), implying that both
NMN and NAD import contribute to the mitochondrial NAD pool41. This observation suggests
that a mitochondrial transporter for NMN may also await discovery. Alternatively, it is possible
that NMNAT3 could function primarily to reverse NAD(H) hydrolysis or could work in
combination with enzymes such as Nudt13 that generate NMN(H)22.
In summary, we show that mammalian mitochondria are capable of directly importing NAD (or
NADH). This finding strongly suggests the existence of an undiscovered transporter in
mammalian mitochondria.
3.6. References
87
1. Dolle, C., Rack, J. G., and Ziegler, M. (2013) NAD and ADP-ribose metabolism in
mitochondria. FEBS J 280, 3530-3541
2. Peek, C. B., Affinati, A. H., Ramsey, K. M., Kuo, H. Y., Yu, W., Sena, L. A., Ilkayeva, O.,
Marcheva, B., Kobayashi, Y., Omura, C., Levine, D. C., Bacsik, D. J., Gius, D., Newgard, C.
B., Goetzman, E., Chandel, N. S., Denu, J. M., Mrksich, M., and Bass, J. (2013) Circadian
clock NAD+ cycle drives mitochondrial oxidative metabolism in mice. Science 342, 1243417
3. Yang, H., Yang, T., Baur, J. A., Perez, E., Matsui, T., Carmona, J. J., Lamming, D. W.,
Souza-Pinto, N. C., Bohr, V. A., Rosenzweig, A., de Cabo, R., Sauve, A. A., and Sinclair, D.
A. (2007) Nutrient-sensitive mitochondrial NAD+ levels dictate cell survival. Cell 130,
1095-1107
4. Revollo, J. R., Grimm, A. A., and Imai, S. (2004) The NAD biosynthesis pathway mediated
by nicotinamide phosphoribosyltransferase regulates Sir2 activity in mammalian cells. J Biol
Chem 279, 50754-50763
5. Berger, F., Lau, C., Dahlmann, M., and Ziegler, M. (2005) Subcellular compartmentation and
differential catalytic properties of the three human nicotinamide mononucleotide
adenylyltransferase isoforms. J Biol Chem 280, 36334-36341
6. Pittelli, M., Formentini, L., Faraco, G., Lapucci, A., Rapizzi, E., Cialdai, F., Romano, G.,
Moneti, G., Moroni, F., and Chiarugi, A. (2010) Inhibition of nicotinamide
88
phosphoribosyltransferase: cellular bioenergetics reveals a mitochondrial insensitive NAD
pool. J Biol Chem 285, 34106-34114
7. Nikiforov, A., Dolle, C., Niere, M., and Ziegler, M. (2011) Pathways and subcellular
compartmentation of NAD biosynthesis in human cells: from entry of extracellular
precursors to mitochondrial NAD generation. J Biol Chem 286, 21767-21778
8. Felici, R., Lapucci, A., Ramazzotti, M., and Chiarugi, A. (2013) Insight into molecular and
functional properties of NMNAT3 reveals new hints of NAD homeostasis within human
mitochondria. PLoS One 8, e76938
9. Hikosaka, K., Ikutani, M., Shito, M., Kazuma, K., Gulshan, M., Nagai, Y., Takatsu, K.,
Konno, K., Tobe, K., Kanno, H., and Nakagawa, T. (2014) Deficiency of nicotinamide
mononucleotide adenylyltransferase 3 (nmnat3) causes hemolytic anemia by altering the
glycolytic flow in mature erythrocytes. J Biol Chem 289, 14796-14811
10. Yamamoto, M., Hikosaka, K., Mahmood, A., Tobe, K., Shojaku, H., Inohara, H., and
Nakagawa, T. (2016) Nmnat3 Is Dispensable in Mitochondrial NAD Level Maintenance In
Vivo. PLoS One 11, e0147037
11. Ratajczak J, Joffraud M, Trammell SAJ, Ras R, Canela N, Boutant M, Kulkarni SS,
Rodrigues M, Redpath P, Migaud M, Auwerx J, Yanes O, Brenner C, Canto C. 2016. NRK1
controls nicotinamide mononucleotide and nicotinamide riboside metabolism in mammalian
cells. Nature Communications. 7:13103
89
12. Bieganowski, P., and Brenner, C. (2004) Discoveries of nicotinamide riboside as a nutrient
and conserved NRK genes establish a Preiss-Handler independent route to NAD+ in fungi
and humans. Cell 117, 495-502
13. Frederick, D. W., Davis, J. G., Davila, A., Jr., Agarwal, B., Michan, S., Puchowicz, M. A.,
Nakamaru-Ogiso, E., and Baur, J. A. (2015) Increasing NAD synthesis in muscle via
nicotinamide phosphoribosyltransferase is not sufficient to promote oxidative metabolism. J
Biol Chem 290, 1546-1558
14. Yaffe D, Saxel O. (1977) Serial passaging and differentiation of myogenic cells isolated from
dystrophic mouse muscle. Nature. 270(5639): 725-7
15. Frederick DW, Loro E, Liu L, Davila A Jr, Chellappa K, Silverman IM, Quinn WJ 3rd, Gosai
SJ, Tichy ED, Davis JG, Mourkioti F, Gregory BD, Dellinger RW, Redpath P, Migaud ME,
Nakamaru-Ogiso E, Rabinowitz JD, Khurana TS, Baur JA. (2016) Loss of NAD homeostasis
leads to progressive and reversible degeneration of skelatal muscle. Cell Metabolism.
24(2):269-282
16. Trounce IA, Kim YL, Jun AS, Wallace DC. Assessment of mitochondrial oxidative
phosphorylation in patient muscle biopsies, lymphoblasts, and transmitochondrial cell lines.
Methods in Enzymology. 264:484-509
90
17. Lu, W. et al. Metabolomic analysis via reversed-phase ion-pairing liquid chromatography
coupled to a stand alone orbitrap mass spectrometer. Analytical Chemistry. 82, 3212–21
(2010).
18. Chance B, Wiliams GR. (1956) The respiratory chain and oxidative phosphorylation. Adv
Enzymol Relat Subj Biochem. 17:65-134
19. Nicholls DG, Ferguson SJ. (1992) Bioenergetics 2. Academic Press, London. 288 pp.
20. Formentini L, Moroni F & Chiarugi A (2009) Detection and pharmacological modulation of
nicotinamide mononucleotide (NMN) in vitro and in vivo. Biochem Pharmacol 77, 1612–
1620.
21. Das M, Parker JE, Halestrap AP. (2003) Matrix volume measurements challenge the
existence of diazoxide/glibencamide-sensitive KATP channels in rat mitochondria. J. Physiol.
547.3: 893-902
22. Abdelraheim SR, Spiller DG, McLennan AG. (2017) Mouse Nudt13 is a mitochondrial
Nudix hydrolase with NAD(P)H pyrophosphohydrolase activity. The Protein
Journal. https://doi.org/10.1007/s10930-017-9734-x
23. Long A, Klimova N, Kristian. (2017) Mitochondrial NUDIX hydrolases: A metabolic link
between NAD and catabolism, GTP and mitochondrial dynamics. Neurochemistry
International. https://doi.org/10.1016/j.neuint.2017.03.009
91
24. Rustin P, Parfait B, Chretien D, Bourgeron T, Djouadi F, Bastin J, Rotig A, Munnich A.
(1996) Fluxes of nicotinamide adenine dinucleotide through mitochondrial membranes in
human cultured cells. J. Biological Chemistry. 271(25):14785-14790
25. Kun, E., Zimber, P. H., Chang, A. C., Puschendorf, B., and Grunicke, H. (1975)
Macromolecular enzymatic product of NAD+ in liver mitochondria. Proc Natl Acad Sci U S
A 72, 1436-1440
26. Behr, A., Taguchi, H., and Gholson, R. K. (1981) Apparent pyridine nucleotide synthesis in
mitochondria: an artifact of NMN and NAD glycohydrolase activity? Biochem Biophys Res
Commun 101, 767-774
27. Calvo, S.E., Klauser, C.R., Mootha, V.K. MitoCarta2.0: an updated inventory of mammalian
mitochondrial proteins (2016). Nucleic Acids Research. 44(D1):D1251-7
28. VanLinden MR, Dolle C, Petterson IKN, Kulikova VA, Niere M, Agrimi G, Dyrstad SE,
Palmieri F, Nikiforov AA, Tronstad KJ, Zielgler M. (2015) Subcellular distribution of NAD+
between cytosol and mitochondria determines the metabolic profile of human cells. J.
Biological Chemistry. 290, 27644-27659.
29. Yahata N, Yuasa S, Araki T. (2009) Nicotinamide mononucleotide adenlytransferase
expression in mitochondrial matrix delays wallerian degeneration. The Journal of
Neuroscience. 29(19):6276-6284
92
30. Barile M, Passarella S, Danese G & Quagliariello E. (1996) Rat liver mitochondria can
synthesize nicotinamide adenine dinucleotide from nicotinamide mononucleotide and ATP
via a putative matrix nicotinamide mononucleotide adenylyltransferase. Biochem Mol Biol
Int. 38, 297–306.
31. Stein LR & Imai S (2012) The dynamic regulation of NAD metabolism in mitochondria.
Trends Endocrinol Metab. 23, 420–428.
32. Chappell JB. (1968) Systems used fort he transport of substratesinto mitochondria. British
Medical Bulletin. 24(2):150-157
33. Bruzzone S, Guida L, Zocchi E, Franco L, De Flora A. (2001) Connexin 43 hemi channels
mediate Ca2+-regulated transmembrane NAD+ fluxes in intact cells. FASEB J. 15:10–12
34. Verderio C, Bruzzone S, Zocchi E, Fedele E, Schenk U, De Flora A, Matteoli M. (2001)
Evidence of a role for cyclic ADP-ribose in calcium signalling and neurotransmitter release
in cultured astrocytes. J. Neurochem. 78:646–657
35. Palmieri F. (2013) The mitochondrial transporter family SLC25: Identification, properties
and physiopathology. Molecular Aspects of Medicine. 34:465–484
36. Haitina, T., Lindblom, J., Renstrom, T., and Fredriksson, R. (2006) Fourteen novel human
members of mitochondrial solute carrier family 25 (SLC25) widely expressed in the central
nervous system. Genomics. 88: 779-790
93
37. Haferkamp, I., Schmitz-Esser, S., Linka, N., Urbany, C., Collingro, A., Wagner, M., Horn,
M., and Neuhaus, H. E. (2004) A candidate NAD+ transporter in an intracellular bacterial
symbiont related to Chlamydiae. Nature. 432(7017):622-5
38. Agrimi G, Russo A, Scarcia P, Palmieri F. (2012) The human gene SLC25A17 encodes a
peroxisomal transporter of coenzyme A, FAD and NAD+. Biochem J. 443(1):241-7
39. Todisco S, Agrimi G, Castegna A, Palmieri F. (2006) Identification of Mitochondrial NAD
transporter in Saccharomyces cerevisiae. J. Biological Chemistry. 281(3); 1524-1531
40. Di Noia, M. A., Todisco, S., Cirigliano, A., Rinaldi, T., Agrimi, G., Iacobazzi, V., and
Palmieri, F. (2014) The human SLC25A33 and SLC25A36 genes of solute carrier family 25
encode two mitochondrial pyrimidine nucleotide transporters. J. Biological Chemistry. 289,
33137-33148
41. Cambronne XA, Stewart ML, Kim DH, Jones-Brunette AM, Morgan RK, Farrens DL, Cohen
MS, Goodman RH. (2016) Biosensor reveals multiple sources for mitochondrial NAD+.
Science. 352(6292): 1474-1477
94
Chapter 4 Quantitative analysis of adipocyte
NADPH pathway usage
4.1. Abstract
The critical cellular hydride donor NADPH can be produced by a variety of routes, including the
oxidative pentose phosphate pathway (oxPPP), folate metabolism, and malic enzyme. In growing
cells, it is efficient to produce NADPH via the oxPPP and folate metabolism, which also make
nucleotide precursors. In non-proliferating adipocytes, a metabolic cycle involving malic enzyme
holds the potential to make both NADPH and two-carbon units for fat synthesis. Recently
developed deuterium (2H) tracer methods make possible direct measurement of NADPH
production by the oxPPP and folate metabolism. Here we enable tracking of NADPH production
by malic enzyme with [2,2,3,3-2H]dimethyl-succinate and [4-2H]glucose. Using these tracers, we
show that most NADPH in differentiating 3T3-L1 adipocytes is made by malic enzyme. The
associated metabolic cycle is disrupted by hypoxia, which switches the main adipocyte NADPH
source to the oxPPP. Thus, 2H-tracers enable dissection of NADPH production routes across cell
types and environmental conditions.
_______________________________________________
Reproduced with permission from Ling Liu, Supriya Shah, Jing Fan, Junyoung Park, Kathryn
Wellen, and Joshua Rabinowitz.
Nature Chemical Biology, 2016,12(5):345-52
95
4.2. Introduction
NADPH is a key cofactor involved in antioxidant defense and reductive biosynthesis1. It can be
produced in cells by a variety of enzymes including glucose-6-phosphate dehydrogenase
(G6PDH) and 6-phosphogluconate dehydrogenase in the pentose phosphate pathway (PPP),
methylenetetrahydrofolate dehydrogenase (MTHFD) and aldehyde dehydrogenases (ALDH) in
folate metabolism, and isocitrate dehydrogenase (IDH) and malic enzyme (ME) associated with
the TCA cycle2,3. Among these different enzymes, the importance of the PPP in NADPH
production is the best established4.
13
C-tracers have long been used to follow metabolic activity, but they provide only indirect
information on the sources of redox cofactors like NADPH. They are inadequate when the same
carbon transformation can produce either NADPH or NADH depending on the isozyme
involved. To address this limitation, hydride transfer from 2H-glucose or 2H-serine into NADPH
in cells has recently been tracked directly using mass spectrometry5. In related work,
compartment-specific NADPH hydride 2H-labeling has been traced using 2-hydroxyglutarate as
a reporter metabolite.6 2-hydroxyglutarate is made by NADPH-driven α-ketoglutarate (α-KG)
reduction by mutant IDH, with IDH1 localized into the cytosol and IDH2 to mitochondria. Both
of direct NADPH 2H-labeling measurements and the 2-hydroxyglutarate reporter approach
revealed that the PPP is the largest cytosolic NADPH source in typical transformed cells in
culture, albeit with other pathways collectively making a roughly comparable contribution.
Whether different enzymes play a predominant role in certain cell types or conditions remains
unknown.
96
The most NADPH-demanding biosynthetic activity in mammals is fat synthesis, which
consumes a majority of cytosolic NADPH in typical transformed cells in culture5. In intact
mammals, fat synthesis is thought to be localized primarily to liver and adipose7. Significant
malic enzyme activity was described in adipose tissue more than 50 years ago8,9. During
adipocyte differentiation, there is coordinate up-regulation of ATP citrate lyase and cytosolic
malic enzyme (ME1), which together with cytosolic malate dehydrogenase and at the expense of
1 ATP, can convert citrate and NADH into acetyl-CoA, NADPH, and pyruvate10. Acetyl-CoA
and NADPH are the two key substrates for fat synthesis, while the resulting pyruvate can be used
to make more citrate. Thus, it is efficient to use malic enzyme to make NADPH in adipose. The
quantitative contribution of different NADPH-producing enzymes in adipose, however, remains
ill defined. Prior quantitative studies suggest a ~60% contribution for the oxPPP and the
remainder from other pathways11–14.
Here we employ 2H-tracing to quantitatively analyze NADPH metabolism in the common tissue
culture model of adipose, 3T3-L1 adipocytes. While 2H tracers for the oxPPP and folate
metabolism were recently established5,6, suitable tracers for malic enzyme were lacking. We
demonstrate the utility of both [2,2,3,3-2H]dimethyl-succinate and [4-2H]glucose for tracing
hydride flux from malate to NADPH and subsequently into fat. Combining this approach with
13
C-labeling studies shows that malic enzyme is the main NADPH source in normoxic 3T3-L1
adipocytes with total NADPH production more than double the PPP. While adipocyte
differentiation and associated fat synthesis continue in hypoxia, the mode of NADPH production
dramatically changes, with malic enzyme’s contribution minimal and the oxPPP predominant.
97
4.3. Results
4.3.1. Quantitative analysis of 3T3-L1 cell NADPH consumption.
3T3-L1 pre-adipocytes cells grow in standard tissue culture media and can be induced to
differentiate into adipocytes by addition of a hormone cocktail15,16. We monitored cell
proliferation, cell volume expansion and associated lipid accumulation during the differentiation
process (Figure 5.1a-b). Fastest lipid accumulation occurred between days 4 and 7, and
accordingly we focused on day 5 in subsequent analysis of metabolic activity in differentiating
adipocytes.
NADPH is used to drive the synthesis of deoxyribonucleotides, proline, and fatty acids. We
investigated NADPH biosynthetic consumption fluxes in proliferating and differentiating (day 5)
3T3-L1 cells. To determine the amount of NADPH consumed by deoxyribonucleotide synthesis,
we measured the rate of change in cell number and assumed a constant amount of DNA per cell,
with 1.25 NADPH per DNA base (2 for thymidine and 1 for the other bases). For proline, we
measured the rate of protein accumulation and corrected for the average frequency of proline,
with 1.5 NADPH per proline5. The NADPH consumption by DNA and proline synthesis, was, as
expected, greater in the proliferating than differentiating cells.
For lipid synthesis, we corrected the observed rate of total cellular fatty acid accumulation for the
fraction of fatty acid synthesized de novo, which was determined by feeding [U-13C]glucose and
[U-13C]glutamine and measuring the extent of fatty acid labeling by mass spectrometry
(Supplementary Results, Appendix Figure C1). In the proliferating 3T3-L1 cells, fatty acids were
98
assimilated to support growth, but 13C-labeling was minimal, indicating fatty acid acquisition
primarily by uptake from media. In contrast, upon differentiation, fatty acid content per cell
increased and was driven by de novo synthesis. In the proliferating and differentiating cells, the
incorporation rate of two-carbon units into fatty acids was 0.011 and 0.120 μmol per day per
million cells, respectively, with 2 NADPH required per two-carbon unit. The fat synthesis rate of
the differentiating adipocytes was similar to that observed previously in transformed and cancer
cells5. Thus, total biosynthetic NADPH consumption in proliferating pre-adipocytes is relatively
low and devoted substantially to deoxyribonucleotide and proline synthesis, whereas in
differentiating adipocytes it is higher (similar to growing transformed cells) and devoted almost
solely to fat synthesis (Figure 4.1c).
Figure 4.1. NADPH consumption during adipogenesis. (a) Cell number and packed cell volume
(PCV) in normoxic 3T3-L1 cells upon initiation of differentiation. (b) Total saponified fatty
acids from cells in (a). (c) NADPH biosynthetic consumption fluxes in proliferating and
differentiating (day 5) 3T3-L1 cells. Data are mean ± s.d., n=3.
99
4.3.2. PPP activity and total NADPH generation
We used two complimentary methods to measure PPP activity. First, we cultured cells in the
presence of [1-14C]glucose versus [6-14C]glucose and detected the released 14CO2. The oxPPP
releases C1 of glucose as CO2. The [6-14C]glucose corrects for release of C1 by other pathways,
because C1 and C6 are rendered identical by the triose phosphate isomerase step in glycolysis
(Figure 4.2a). We determined an oxPPP flux of 0.017 and 0.020 μmol per day per million cells
in the proliferating and differentiating cells respectively (Figure 4.2b), and confirmed the rate in
differentiating cells also using [1,2-13C]glucose tracer (Appendix Figure C2a-c); these rates are
substantially below that previously reported in transformed growing cells5. Next, we fed [12
H]glucose and [3-2H]glucose, which label NADPH in the first step (G6PDH) and third step (6-
phosphogluconate dehydrogenase) of the oxPPP, respectively.5 In the proliferating cells, M+1
NADPH exceeded M+1 NADP+ by ~13% (Figure 4.2c). Similar NADPH labeling was also
observed in several transformed growing cell lines5,6. In contrast, in the differentiating
adipocytes, there was much less NADPH labeling from [1-2H]glucose. Thus, in contrast to
growing cells, differentiating 3T3-L1 cells get a substantially lower fraction of their NADPH
from the oxPPP.
The 2H-glucose labelling results can be used to quantitate the fractional contribution of the PPP
to total cytosolic NADPH production. The inferred fractional contribution of the PPP to NADPH
production can be used to deduce the total cytosolic NADPH production rate, which is equal to
the absolute oxidative PPP flux divided by the fractional contribution of the PPP to NADPH
production (Eqn. 1, 2)5.
𝑓 NADPH from oxPPP = 2 * ( 𝑓 CO2 from glucose C1 - 𝑓 CO2 from glucose C6)
100
(1)
NADP 2 H
𝑓 NADPH from oxPPP= 2 ∗ NADPH
total
∗
G6Ptotal
2H−G6P
∗ 𝑓 NADPH from all cytosolic sources ∗ CKIE (2)
In Eqn. 1, 𝑓CO2 from glucose C1 is based on the measured release rates of 14C-CO2 corrected for
the fractional radioactive labeling of glucose (and similarly for C6, see Methods) and multiplied
by two to account for the oxPPP stoichiometry of 2 NADPH per glucose. In Eqn. 2, the
measured fractional 2H-labeling of NADPH is corrected for the 2H-labeling of glucose-6phosphate (Appendix Figure C2d) and for the deuterium kinetic isotope effect (CKIE)17 and
multiplied by two as only one of the two hydrogens that are transferred to NADPH via the
oxPPP is labeled. Combining Eqn. 1 and 2, the measured absolute oxPPP NADPH production
(0.034 and 0.040 μmol per day per million cells) divided by the fractional contribution of the
oxPPP (46% and 16%) gave a total cytosolic NADPH production flux of approximately 0.074
and 0.250 μmol per day per million cells, in the proliferating and differentiating cells
respectively. This total NADPH production flux was nearly identical to the independently
measured biosynthetic NADPH consumption flux (Figure 4.2d). Thus, most NADPH both in
proliferating and in differentiating cultured cells is consumed for biosynthesis, with fat synthesis
dominant in the differentiating cells.
101
Figure 4.2. NADPH production by the oxidative pentose phosphate pathway. Data are from
normoxic proliferating or differentiating (day 5) 3T3-L1 cells. (a) Oxidative pentose phosphate
pathway schematic. G6PDH, glucose-6-phosphate dehydrogenase; 6PGD, 6-phosphogluconate
dehydrogenase. (b) 14CO2 release from [1-14C]glucose or [6-14C]glucose. The difference reflects
the oxPPP flux. (c) NADP(H) 2H-labeling in cells fed [1-2H]glucose for 2 h. (d) Comparison of
NADPH production with biosynthetic NADPH consumption. Total NADPH consumption was
calculated from absolute oxPPP flux (Panel b) divided by NADP2H fraction measured by
NADPH labeling (Panel c). Data are mean ± s.d., n=3 (***, p<0.001 by T-test).
4.3.3. NADPH contribution of folate metabolism
The folate metabolic enzymes MTHFD and ALDH have NADPH-producing dehydrogenase
activity. MTHFD is required for oxidizing methylene-THF into the key one-carbon donor
formyl-tetrahydrofolate (formyl-THF). In contrast, ALDH does not produce a useful one-carbon
donor, but instead oxidizes formyl-THF into THF, CO2, and NADPH (Figure 4.3a).
102
Cytosolic formyl-THF, which is required by proliferating cells for purine synthesis, can be
produced from methylene-THF by the cytosolic methylene-THF dehydrogenase MTHFD1 with
concomitant cytosolic NADPH production. Alternatively, it can be made from formate exported
by mitochondria, in which case methylene-THF oxidation occurs in the mitochondria with
associated production by MTHFD2 of mitochondrial NADH and (to a lesser extent)
NADPH18,19. To determine where one-carbon units are made in proliferating 3T3-L1 cells, we
fed [2,3,3-2H]serine and looked for production of 2H-labeled thymidine triphosphate (TTP). The
cytosolic pathway produces doubly labeled TTP, whereas one deuterium is lost in the
mitochondrial pathway resulting in single TTP labeling (Appendix Figure C2e). We observed
only M+1 TTP, indicating minimal cytosolic MTHFD1 flux in the direction of NADPH
production (Appendix Figure C2f).
Therefore, we focused on the complete oxidation of one-carbon units by the combined action of
MTHFD and ALDH, which can be traced based on release of CO2 from [3-14C]serine and [214
C]glycine. We observed substantial release of serine C3 as CO2, indicating that the complete
one-carbon oxidation pathway is actively producing NADPH (Figure 4.3b). The absolute
magnitude, however, was smaller than the oxPPP flux. Consistent with the methylene-THF
oxidation pathway resulting in a modest contribution to total NADPH production, feeding of
[2,3,3-2H]serine, the main pathway substrate, resulted in ~ 3% labeling of NADPH at its redox
active hydride (Appendix Figure C2g). Thus, in differentiating 3T3-L1 adipocytes, folate
metabolism contributes modestly to NADPH production.
We recognized one possibility for deficient NADPH labeling is H-D exchange. We measured the
extent of labeling in cells placed in media containing D2O, and observed NADP+ getting
103
deuterium incorporation at C-4 position and dideuterium NADPH. Correction of the directly
measured 2H labeling fractions for NADPH H-D exchange20 revealed half of NADPH redox
active hydrogen coming from water in differentiating 3T3-L1 cells. The re-evaluation of oxPPP,
in light of such H-D exchange, showed the contribution to total NADPH to be ~40%.20
Figure 4.3. NADPH production by folate metabolism. Data are from normoxic proliferating or
differentiating (day 5) 3T3-L1 cells. (a) Folate pathway schematic. THF, tetrahydrofolate;
MTHFD, methylenetetrahydrofolate dehydrogenase; ALDH, aldehyde dehydrogenase. (b) 14CO2
release from [1-14C]glycine, [2-14C]glycine, or [3-14C]serine. (c) Fractional NADPH contribution
of oxPPP, folate pathway, and other sources before correcting the H-D exchange. The estimate
of NADPH made by folate metabolism assumes that MTHFD2 produces NADH. Data are mean
± s.d., n=3.
104
4.3.4. Tracing carbon flux through malic enzyme
The above analysis implies that a majority of (>50%) NADPH in differentiating adipocytes
comes from source(s) other than the oxPPP and folate metabolism (Figure 4.3c). We accordingly
considered malic enzyme. To evaluate total malic enzyme flux, we fed [U-13C]glutamine, whose
metabolism through the citric acid cycle and malic enzyme labels pyruvate (see Methods,
Appendix Figure C3). Assuming that pyruvate and malate are labeled similarly in both
mitochondria and cytosol,
𝑓𝑀𝐸
𝑓𝐺𝑙𝑦𝑐𝑜𝑙𝑦𝑠𝑖𝑠
Pyr[M+3]
= Pyr
[M+0]
∗
Maltotal
(3)
Mal[M+4] + 0.5∗Mal[M+3]
This assay measures gross flux from malate to pyruvate, which will exceed the net malic enzyme
flux when alternative pathways between malate and pyruvate are active (e.g. gluconeogenesis,
reverse pyruvate carboxylase, or reverse malic enzyme9,21,22). It also does not account for
pyruvate and malate compartmentation or identify whether malic enzyme is making NADH or
NADPH.
Similar to many transformed cell lines, proliferating 3T3-L1 cells showed only trace pyruvate
labeling from glutamine23 (Figure 4.4a). Upon differentiation, however, there was extensive
labeling, with malate to pyruvate flux producing ~ 15% of the pyruvate pool (Figure 4.4b). Due
to the speed of glycolysis (glucose uptake rate of 6.4 μmol per day per million cells), total gross
flux from malate to pyruvate on day 5 is 2.4 μmol per day per million cells, approximately 10times the measured total NADPH consumption and production rates.
To evaluate whether gluconeogenic flux involving the combined action of malate
dehydrogenase, phosphoenolpyruvate carboxykinase (PEPCK), and pyruvate kinase contributes
105
to the observed pyruvate labeling, we monitored the labeling of phosphoenolpyruvate (PEP), the
direct product of PEPCK, and the more abundant phosphoglycerate (adjacent in glycoylsis), by
[U-13C]glutamine. Only trace labeling was observed, thereby ruling out a major contribution of
the gluconeogenic pathway (Figure 4.4c).
We next explored whether quantitative metabolic flux analysis (MFA) of 13C-labeling data for
the full set of measurable central carbon metabolites would be sufficient to determine net malic
enzyme flux and its compartmentation. Specifically, we developed a carbon- and redox-balanced
flux model of central metabolism and searched computationally for fluxes that fit experimental
data for nutrient uptake, waste excretion, and metabolite 13C-labeling in cells fed [U-13C]glucose
or [U-13C]glutamine (Figure 4.4d, Appendix Table C1). For simplicity, we allowed only forward
flux through pyruvate carboxylase and malic enzyme. A minimal reaction network with only
cytosolic malic enzyme (ME1) fit the data less well than the network including also
mitochondrial malic enzyme or pyruvate carboxylase reversibility (Appendix Table C2,
Appendix Figure C4). In the case with ME1 only (blue numbers in Figure 4.4d), the malic
enzyme flux was around 2.9 μmol per day per million cells. Inclusion of mitochondrial malic
enzyme (red numbers in Figure 4.4d) did not significantly change the total malic enzyme flux,
but rendered the ME1 flux indeterminant (confidence interval 0.2 to 2.0 μmol per day per million
cells) (Appendix Table C2). Thus, 13C-tracers were insufficient to determine cytosolic malic
enzyme activity and associated NADPH production.
106
Figure 4.4. Carbon flux through malic enzyme. Data are from normoxic proliferating or
differentiating (day 5) 3T3-L1 cells. (a) Production of malate [M+4] and pyruvate [M+3] from
[U-13C]glutamine (12 h labeling duration). (b) Relative abundance of pyruvate [M+3] versus
malate [M+4]. (c) Associated production in differentiating 3T3-L1 adipocytes of M+3 labeled
3PG, 3-phosphoglycerate; PEP, phosphoenolpyruvate; Pyr, pyruvate; Lac, lactate. Data are mean
± s.d., n=3 (***, p<0.001 by T-test). (d) Central carbon metabolic fluxes in differentiating 3T3L1 adipocytes based on metabolic flux analysis informed by nutrient uptake, waste excretion,
and biomass production fluxes, as well as LC-MS analysis of intracellular metabolite labeling in
cells fed [U-13C]glucose or [U-13C]glutamine. Values shown are relative fluxes (normalized to
glucose uptake) from the best fitting flux sets for 3 different conditions: (top values, blue) a
simplified network with cytosolic (ME1) but not mitochondrial (ME2 or ME3) malic enzyme;
107
(middle values, red) with inclusion of mitochondrial malic enzyme (ME2 or ME3); (bottom
values, purple) constraint of the ME1 flux also using 2H-labeling data from Figure 4.5. Red and
purple fluxes values are only shown when they are more than 10% different from the blue value.
Confidence intervals for malic enzyme and pyruvate carboxylase fluxes are shown in the inset.
For complete flux distributions and confidence intervals, see Appendix Table C1. GAP,
glyceraldehyde-3-phosphate; Glyc, glycerol; OAA, oxaloacetate; αKG, α-ketoglutarate; Cit,
citrate.
108
4.3.5. [2,2,3,3-2H]dimethyl succinate tracer for malic enzyme
We therefore sought to track hydride transfer mediated by malic enzyme. Previous efforts to
trace such activity using [2,3,3,4,4-2H]glutamine had been unsuccessful5, and were also
unsuccessful here because loss of the 2H-label throughout the intervening citric acid cycle
reactions (Appendix Figure C5a). As an alternative, we fed the membrane permeable succinate
analog [2,2,3,3-2H]dimethyl succinate (Appendix Figure C5a,b). Tracer addition increased the
cellular concentration of succinate without markedly perturbing other metabolite concentrations
or fluxes (Appendix Figure C6). We followed labeling from [2,2,3,3-2H]dimethyl succinate
through the C2 hydride of malate to NADPH and finally to newly synthesized fatty acids (Figure
4.5a). NADPH labeling at its redox active hydride was analyzed by comparing the M+1 fraction
of NADPH to NADP+. In the absence of [2,2,3,3-2H]dimethyl succinate, the NADP+ and
NADPH labeling patterns were identical (Appendix Figure C5b). Addition of tracer resulted in
increased labeling of NADPH but not NADP+ selectively in differentiating but not proliferating
3T3-L1 cells, with 3.4% ± 0.3% of the total adipocyte NADPH labeled (Figure 4.5b). Analysis
of fatty acids, which reflects specifically cytosolic NADPH and thus ME1, similarly revealed
selective 2H-labeling in the differentiating adipocytes (Figure 4.5c). Quantitative analysis of the
mass isotope distribution of a set of abundant fatty acids (omitting pre-existing fatty acids and
those acquired by uptake from media, as determined by 13C-labeling data) revealed an average
hydride 2H-labeling fraction of 2.87% ± 0.31% (Appendix Figure C7). Adjustment for the kinetic
isotope effect in hydride transfer from NADPH to fat (~1.1 )24 yields an associated cytosolic
NADPH labeling fraction of 3.2% ± 0.5%, in excellent agreement with the directly measured
whole cell NADPH labeling.
109
Converting the NADPH labeling fraction from [2,2,3,3-2H]dimethyl succinate into the fractional
NADPH contribution of malic enzyme requires two important corrections: (i) fractional 2Hlabeling of cytosolic malate’s C2 hydride and (ii) the malic enzyme deuterium kinetic isotope
effect (~ 1.5, see Methods).
𝑓𝑁𝐴𝐷𝑃𝐻 𝑓𝑟𝑜𝑚 𝑀𝐸1 =
NADP2 H
NADPH
∗
Mal
MalC2−deuteron
∗ 𝑓𝑁𝐴𝐷𝑃𝐻 𝑓𝑟𝑜𝑚 𝑎𝑙𝑙 𝑠𝑜𝑢𝑟𝑐𝑒𝑠 ∗ CKIE
(4)
Forward flux from [2,2,3,3-2H]succinate results in [2,3-2H]malate, i.e., M+2 malate (Appendix
Figure C8a). The observed fraction of M+2 malate was, however, only 1.5%. The larger peak
was M+1 malate (Appendix Figure C8b). Reverse flux through malate dehydrogenase can
produce M+1 malate labeled at the C3 hydride ([3-2H]malate). As fumarate is symmetric,
fumarase will interconvert [3-2H] and [2-2H]malate (Appendix Figure C8a). Because malic
enzyme will produce NADP2H selectively from malate labeled at the C2 hydride, it was critical
to determine the relative abundance of [2-2H] versus [3-2H]malate. [3-2H]malate (and also [2,32
H]malate) yields M+1 oxaloacetate and aspartate, whereas [2-2H]malate yields unlabeled.
Hence, subtracting the fraction of M+1 aspartate from that of M+1 plus M+2 malate gives the
fraction of [2-2H]malate, which was ~ 6.4%. Summing [2-2H]malate and [2,3-2H]malate, the
fraction of malate which is capable of making NADP2H was 7.9% (Figure 4.5d, see Methods).
Thus, while [2,2,3,3-2H]dimethyl succinate labeled only ~ 3.2% of NADPH, the fraction of
NADPH generated via malic enzyme is ~ 60%.
110
Figure 4.5. Tracing hydride flux through malic enzyme. Data are from normoxic proliferating or
differentiating (day 5) 3T3-L1 cells. (a) Schematic of [2,2,3,3-2H]dimethyl succinate
metabolism. (b) NADP(H) 2H-labeling in cells fed [2,2,3,3-2H]dimethyl succinate for 24 h. (c)
Palmitate 2H-labeling in cells fed [2,2,3,3-2H]dimethyl succinate for 5 days. (d) Extent of 2Hlabeling of the redox-active hydrogen of malate, whole cell NADPH, and cytosolic NADPH
(inferred from fatty acid labeling) in differentiating 3T3-L1 adipocytes fed [2,2,3,3-2H]dimethyl
succinate (labeling duration 24 h except for the fatty acids). (e) Schematic of [4-2H]glucose
metabolism. (f) NADP(H) 2H-labeling in cells fed [4-2H]glucose for 24 h. (g) Palmitate 2Hlabeling in cells fed [4-2H]glucose for 5 days. (h) Extent of 2H-labeling of the redox-active
hydrogen of malate, whole cell NADPH, and cytosolic NADPH (inferred from fatty acid
labeling) in differentiating 3T3-L1 adipocytes fed [4-2H]glucose. (i) Western blot to verify
knockdown of NADPH-producing enzymes in differentiating 3T3-L1 adipocytes. The full gel
images can be found at Appendix Figure C13. (j) Impact of knockdown of NADPH-producing
111
enzymes on total cellular palmitate abundance (free + saponified from lipids). (k) Impact
NADPH-producing enzyme knockdown on palmitate 2H-labeling from [2,2,3,3-2H]dimethyl
succinate. Results are normalized to siCTRL cells (100%). Data are mean ± s.d., n=3 (**,
p<0.01 by T-test).
4.3.6. [4-2H]glucose as a malic enzyme tracer
Dimethyl succinate is not a typical circulating nutrient. In addition, conversion of [2,2,3,32
H]dimethyl succinate to [2-2H]malate requires oxidation of succinate to fumarate by succinate
dehydrogenase (Complex II) in the inner mitochondrial membrane and the resulting labeled
malate must traffic to the cytosol to feed ME1. Incomplete mixing between the mitochondria and
cytosol could result in overestimation of cytosolic malate labeling and thereby underestimation
of ME1’s contribution to NADPH. We accordingly sought an alternative tracer strategy
involving only standard nutrients where labeled malate would be made directly in the cytosol.
One way to generate cytosolic [2-2H]malate is via malate dehydrogenase-catalyzed reduction of
oxaloacetate by NAD2H. [4-2H]glucose can label cytosolic NADH via glyceraldehyde-3phosphate dehydrogenase6 (Figure 4.5e). Compared to the dimethyl succinate tracer, [42
H]glucose resulted in a similar extent of [2-2H]malate labeling (Appendix Figure C8c). While a
small amount of labeling of NAD(P)H itself by [4-2H]glucose was observed in the proliferating
cells, labeling in NADP+ and NADPH was equivalent, indicating incorporation of 2H-labeled
ribose into newly synthesized NADP+ without redox active hydride labeling (Figure 4.5f). In
contrast, preferential labeling of NADPH relative to NADP+ was observed in the differentiating
adipocytes, indicating flux into NADPH’s redox-active hydride via malic enzyme. Consistent
112
with this, [4-2H]glucose labeled fatty acids selectively in the differentiating cells (Figure 4.5g).
Quantitatively, the extent of redox active NADPH hydride labeling was identical within error for
both the [4-2H]glucose and the dimethyl succinate (Figure 4.5h).
Integration of the ME1 flux constraint from the 2H-tracers with the nutrient uptake, waste
excretion, and 13C-tracer data via quantitative metabolic flux analysis of the network including
cytosolic and mitochondrial malic enzyme resulted in a coherent set of whole cell fluxes (purple
numbers in Figure 4.4d). In the absence of pyruvate carboxylase or malic enzyme reversibility,
all fluxes were well-defined. Inclusion of such reversibility rendered mitochondrial fluxes
indeterminant without affecting the fit or impacting ME1 flux (Appendix Table C2). The
confidence interval for NADPH production rate was 0.4% to 0.8% of the glucose uptake rate for
the oxPPP and 2.7% to 3.5% for ME1 (Appendix Table C1).
4.3.7. Genetic confirmation of ME1’s NADPH contribution
Both ME1 and ME2 (NADH-producing mitochondrial malic enzyme) have been previously
shown based on shRNA knockdown to be required for adipocyte differentiation25. Here we
observed that ME1 protein, but not ME2 or ME3 protein, increased dramatically during
adipocyte differentiation (Appendix Figure C9a). To evaluate the functional significance of ME1
relative to other cytosolic NADPH-producing enzymes, we knocked down, on differentiation day
2, G6PDH (the committed enzyme of the oxPPP), MTHFD1 (required for cytosolic one-carbon
unit oxidation), IDH1 (the cytosolic NADPH-generating isocitrate dehydrogenase), and ME1
(Figure 4.5i, Appendix Figure C9b). Silencing ME1, but not the other enzymes, decreased fatty
acid accumulation in the differentiating adipocytes (Figure 4.5j). Moreover, ME1 knockdown
113
decreased carbon flux from malic acid to pyruvate (Appendix Figure C9c-e) and fatty acid
labeling from [2,2,3,3-2H]dimethyl succinate (Figure 4.5k). Thus, ME1 is the main source of
NADPH to drive fatty acid synthesis in adipocytes and is required for effective lipogenesis.
4.3.8. Impact of hypoxia on adipocyte metabolism
The quantitative flux analysis in the differentiating adipocytes revealed a metabolic cycle in
which pyruvate is generated by malic enzyme and consumed by pyruvate carboxylase26 and
pyruvate dehydrogenase. This cycle is efficient in terms of minimizing the transport of substrates
between the cytosol and mitochondrion (Appendix Figure C9f). We were curious if malic
enzyme would continue to be the predominant NADPH source under conditions where the cycle
is disrupted, such as by inhibition of pyruvate dehydrogenase activity in hypoxia27,28.
Understanding the impact of hypoxia on differentiating adipocyte metabolism is also of potential
medical relevance as obesity has been proposed to result in hypoxia in adipose tissue29,30.
We began by determining whether differentiation would proceed in 1% oxygen. Though
attenuated, fatty acid synthesis, associated lipid accumulation, and adipocyte markers were
induced by differentiation in hypoxia (Appendix Figure C10a-e). The source of the fatty acid
carbon changed from mainly glucose to mainly glutamine, as occurs also in hypoxic cancer
cells31,32, with increased glucose uptake and lactate excretion (Appendix Figure C10f, g). To
evaluate NADPH production routes in hypoxic differentiating adipocytes, we traced hydride
labeling into fat from both [1-2H]glucose and [3-2H]glucose to probe the oxPPP and both
[2,2,3,3-2H]dimethyl succinate and [4-2H]glucose to probe malic enzyme. Hypoxia resulted in
markedly increased labeling from both oxPPP tracers (Figure 4.6a, Appendix Figure C11a-e) and
114
nearly completed elimination of labeling from both malic enzyme tracers (Figure 4.6b, Appendix
Figure C11f). Associated quantitation, correcting for substrate labeling and the deuterium kinetic
isotope effect17,33,34, revealed that the contribution of the oxPPP increased from 21% ± 4% in
normoxia to 55% ± 5% in hypoxia, whereas the contribution of malic enzyme decreased from
60% ± 5% to 3% ± 2% (mean ± s.d., n = 3). Thus, in response to hypoxia, the main lipogenic
NADPH source switches from malic enzyme to the oxPPP (Figure 4.6c, d). We also compared
the impact of differentiation (starting at day 0) in hypoxia versus switch into hypoxia midway
through the differentiation process (starting at day 3). This later switch produces an intermediate
phenotype in terms of NADPH production routes (Appendix Figure C12). To investigate the
mechanism by which NADPH production was being controlled, protein levels of ME1 and the
NADPH-producing oxPPP enzyme (G6PDH) were measured. While the oxPPP protein level did
not change markedly in response to hypoxia, ME1 decreased (Appendix Figure C10e). Together,
these data reveal that differentiation in hypoxia, in part by suppressing ME1 enzyme abundance,
shifts the main 3T3-L1 adipocyte NADPH production route to the oxPPP.
Figure 4.6. Hypoxia increases adipocyte NADPH production by the oxidative pentose phosphate
pathway and blocks that by malic enzyme. (a) Labeling of palmitate in 3T3-L1 adipocytes fed
[1-2H]glucose to trace cytosolic NADPH production by the oxPPP. (b) Labeling of palmitate in
115
3T3-L1 adipocytes fed [4-2H]glucose or [2,2,3,3-2H]dimethyl succinate to trace cytosolic
NADPH production by malic enzyme. Cells were cultured throughout the 5-day differentiation
period in the presence of tracer and either ambient oxygen or 1% O2. (c) Summary of metabolic
activity in differentiating normoxic or hypoxic adipocytes, showing disruption of the citratepyruvate cycle in hypoxia and its replacement by reductive carboxylation, with concomitant shift
away from NADPH production by malic enzyme. (d) Quantitative comparison of NADPH
production routes in differentiating normoxic or hypoxic adipocytes. Data are mean ± s.d., n=3.
4.4. Discussion
Cells employ two fundamental energy currencies: high-energy phosphate bonds and high-energy
electrons. High-energy phosphate bonds in the form of ATP are produced in significant
quantities by only two routes, glycolysis and oxidative phosphorylation, with glycolysis a
significant ATP source specifically when oxygen is limited. High-energy electrons in the form of
NADPH, in contrast, can be produced by a variety of pathways. The physiological rationale for
use of one pathway over another remains an open question.
In recent work, we and others used 2H-tracers to examine quantitatively NADPH production
pathways in transformed growing cells5,6. This analysis led to two major conclusions: (i) most
cytosolic NADPH in growing cells is used for reductive biosynthesis, not antioxidant defense,
and (ii) the largest NADPH contributor is the oxPPP with folate metabolism also playing a role.
Growing cells have a high demand for nucleotide synthesis, which requires precursors generated
by the PPP and folate metabolism. The observed oxPPP and folate fluxes in growing cells are
necessary for meeting ribose phosphate and 10-formyl-THF demand, and in so doing also
116
provide most of the required NADPH5. Thus, in growing cells, there is physiologic efficiency in
using the oxPPP and folate metabolism for NADPH production.
Here we examine NADPH metabolism in adipocytes (3T3-L1 cells), which upon differentiation
stop growing but remain biosynthetically active. We show that both total biosynthetic NADPH
demand and NADPH production increase upon differentiation, to a level comparable to typical
transformed cells. The overall metabolic requirements of differentiating adipocytes are, however,
distinct. Differentiating adipocytes do not engage in significant nucleotide synthesis and thus
have minimal need for ribose phosphate and 10-formyl-THF. The fractional NADPH
contribution of these pathways drops. Instead, in normoxic differentiating adipocytes, most
NADPH is made by malic enzyme. We prove this using a combination of classical 13C-glutamine
tracing into pyruvate augmented by more global flux analysis and a newly developed method for
directly tracing 2H-NADPH production by malic enzyme.
Despite significant interest in malic enzyme’s role in cancer13 and obesity35,36,37, previous
methods could not directly follow NADPH production from malic enzyme in cells. Carbon
isotope tracer studies, while valuable23,26 , cannot directly differentiate NADH and NADPHdependent malic enzyme. Although recent work observed NADH and NADPH labeling from [42
H]glucose, the NADPH labeling was attributed to an unknown mechanism rather than malic
enzyme. The two tracers that we provide here, [2,2,3,3-2H]dimethyl succinate or [4-2H]glucose,
both produce [2-2H]malate which in turn makes NADP2H and 2H-labeled fatty acids. Production
of labeled malate by [2,2,3,3-2H]dimethyl succinate is more direct, but relies on a nonphysiologic uptake mechanism and transfer of malate from mitochondrion to cytosol.
Accordingly, [4-2H]glucose may be more generally applicable, as it uses a physiological uptake
117
mechanism and sequence of cytosolic reactions to label malate, and is better suited to potential
future in vivo application.
An important virtue of having two tracers is that any one method may be subject to non-random
error (e.g. due to unaccounted for H-D exchange, compartmentation, or factors impacting the
kinetic isotope effect). Some such errors may be common to both tracers, which each feed
through [2-2H]malate. Moreover, each tracer labels metabolites in addition to malate, which can
potentially result in 2H labeling of NADPH or fatty acids through other routes. For example,
turning of the TCA cycle converts [3-2H]malate into 2H-isocitrate labeled at the hydride
transferred to NADPH by IDH1/2. While we did not observe significant (iso)citrate labeling
from these tracers in adipocytes, we do in some other cell types. These observations highlight the
need for careful consideration of all possible means of gaining or losing 2H labeling when such
tracers employed, especially as even minor fluxes can impact quantitative analysis. That said, our
main findings appear to be robust. Both tracers gave quantitatively indistinguishable results: a
malic enzyme contribution to cytosolic NADPH of roughly 60% in normoxia and 3% in hypoxia.
Among the multitude of possible NADPH production routes, why do normoxic adipocytes rely
on malic enzyme? And why does this change in hypoxia? Fatty acid synthesis requires cytosolic
acetyl-CoA. Pyruvate is converted to acetyl-CoA selectively in the mitochondrion. This acetylCoA is carried into the cytosol as citrate, which is then re-converted into oxaloacetate and acetylCoA in the cytosol by ATP-citrate lyase38. Reduction of oxaloacetate by cytosolic malate
dehydrogenase yields cytosolic malate. Conversion of this malate into pyruvate and NADPH by
malic enzyme regenerates pyruvate. This cycle39 serves dual purposes in adipocytes: (i)
118
production of cytosolic acetyl-CoA and (ii) generation of NADPH from reducing equivalents
originally derived from glycolysis as NADH (Appendix Figure C9f).
This pyruvate-citrate cycle requires mitochondrial acetyl-CoA made by pyruvate decarboxylase,
an enzyme which is inactivated by multiple mechanisms in hypoxia. Thus, disruption of the
pyruvate-citrate cycle, and the associated switch from glucose to glutamine carbon being used
for lipogenesis, is a logical consequence of cultivation in low oxygen. Both glucose-driven and
glutamine-driven production of cytosolic acetyl-CoA require ATP-citrate lyase and thus produce
oxaloacetate, which can undergo NADH-driven reduction to malate. Therefore, use of malic
enzyme to make NADPH in hypoxia should be feasible. This makes the dramatic shift away
from malic enzyme towards the oxPPP yet more interesting. Elucidation of the underlying
regulatory mechanisms is an important objective of future research.
In summary, in both growing and differentiating normoxic adipocytes, NADPH production is
carried out by pathways that also serve other important physiological roles. In growing cells,
these are pathways coupled to nucleotide synthesis (oxPPP, folate); in differentiating adipocytes,
they are pathways coupled to generation of cytosolic acetyl-CoA. Hypoxia switches the primary
NADPH production route in differentiating adipocytes back to the oxPPP. Much as malic
enzyme plays a particularly important role in making NADPH in normoxic differentiating
adipocytes, we hypothesize that other NADPH producing enzymes, such as IDH37, will play a
predominant role in certain yet-to-be-discovered cell types and settings. Accordingly, the variety
of feasible NADPH production pathways can be rationalized as allowing metabolic efficiency
across diverse cell types and conditions with distinct total metabolic requirements.
119
4.5. Methods
4.5.1. Cell culture, gene knockdown with siRNA and antibodies.
3T3-L1 pre-adipocytes were obtained from American Type Culture Collection and confirmed to
be mycoplasma free by MycoAlert Mycoplasma Detection Kit (Lonza, LT07-218). 3T3-L1 preadipocytes were grown in Dulbecco’s modified eagle media (DMEM, Cellgro, 10-017) with 10%
FBS (Gibco, heat-inactivated). Adipogenesis was induced in 3T3-L1 pre-adipocytes with a
cocktail containing 5 µg/ml insulin, 0.5 mM isobutylmethylxanthine, 1 µM dexamethasone and 5
µM troglitazone (Sigma). After 2 days, new medium was added and cells were maintained in 5
µg/ml insulin. Cell number was determined with an automatic cell counter (Invitrogen). Packed
cell volume was determined with PCV tubes (TPP). All siRNAs were all obtained from Santa
Cruz Biotechonlogy. siRNA targeting G6PDH (sc-60668), MTHFD1(sc-61083), IDH1(sc60830), ME1 (sc-149342) was transfected into 3T3-L1 adipocytes on day 2 post-differentiation
using Lipofectamine RNAiMAX (Invitrogen) and an Amaxa Nucleofector for electroporation.
Timeline of knockdown experiments can be found at Appendix Figure C9b, c. The antibodies
against the following proteins were purchased from the indicated sources: ME1 (Abcam,
ab97445, 1:1000 dilution), ME2 (Abcam, ab139686, 1:1000 dilution), ME3 (Abcam, ab172972,
1:2000 dilution), G6PDH (Abcam, ab993, 1:1000 dilution), β-actin (Abcam, ab8229, 1:2000
dilution), MTHDF1 (Abgent, abin785327, 1:1000 dilution); IDH1 (Proteintech, 12332-1-AP,
1:2000 dilution), PPAR-γ (Santa Cruz, sc7196, 1:1000 dilution) and tubulin (Sigma, T6199,
1:1000 dilution). Quantitative PCR was performed on purified cDNA samples. Gene expression
data was normalized to 18S rRNA. Primers used are SLC2A1(Glut1)-FWD,
120
CCCAGAAGGTTATTGAGGAG; SLC2A1(Glut1)-REV, AGAAGGAACCAATCATGCC;
SLC2A4(Glut4)-FWD, GCCCGAAAGAGTCTAAAGC; SLC2A4(Glut4)-REV,
CTTCCGTTTCTCATCCTTCAG; PPARγ-FWD, TGGCATCTCTGTGTCAACCATG; PPARγREV, GCATGGTGCCTTCGCTGA; RETN-FWD, CTGTCCAGTCTATCCTTGCACAC;
RETN-REV, CAGAAGGCACAGCAGTCTTGA; FABP4-FWD,
ACAAAATGTGTGATGCCTTTGTGGGAAC; and FABP4-REV,
TCCGACTGACTATTGTAGTGTTTGATGCAA.
4.5.2. Isotopic labeling.
The following isotopic tracers were purchased from the indicated sources: [2,3,3-2H]serine, [12
H]glucose, [3-2H]glucose, [U-13C]glutamine, [U-13C]glucose (Cambridge Isotope Laboratories);
[2,2,3,3-2H]dimethyl succinate (Sigma). Isotope-labeled glucose and glutamine medium was
prepared from phenol red-, glucose-, glutamine-, sodium pyruvate-, sodium bicarbonate-free
DMEM powder (Cellgro) supplemented with 3.7g/L sodium bicarbonate, 25 mM glucose and 4
mM glutamine. Isotope-labeled serine medium was prepared from scratch following the standard
DMEM formula, by mixing together stock solutions containing vitamins, amino acids without
serine, inorganic salts, and glucose, and thereafter supplemented with 42 mg/L [2,3,3-2H]serine.
Isotope-labeled succinate medium was prepared from DMEM powder, 25 mM glucose, 4 mM
glutamine supplemented with 2 mM [2,2,3,3-2H]dimethyl succinate. In HEK293T cells (but not
the 3T3-L1 cells studied here) we find that decreasing the glucose and glutamine levels in
DMEM to 10 mM and 1 mM respectively, increases fractional malate labeling from the tracer
121
and thereby facilitates malic enzyme flux measurement. Isotopic medium was supplemented with
10% dialyzed fetal bovine serum (Sigma) and, for differentiating cells only, 5 µg/ml insulin.
4.5.3. Metabolite measurements.
Cells were grown in 6 cm tissue culture dishes, and the labeled medium was replaced every day,
and additionally 2 hours before extracting metabolites. Because labeling of glycolytic and oxPPP
intermediates and the redox active hydride of NADPH reaches steady state over ~ 5 min, where
for TCA intermediates can take several hours40, to ensure steady-state labeling, oxPPP tracing
with [1-2H]glucose and [1,2-13C]glucose was performed for a minimum of 30 min and other
labeling experiments for a minimum of 12 h. Metabolism was quenched and metabolites were
extracted by aspirating media and immediately adding 2 mL -80°C 80:20 methanol: water. After
20 min of incubation on dry ice, the resulting mixture was scraped, collected into a centrifuge
tube, and centrifuged at 10000 g for 5 min. Insoluble pellets were re-extracted with 1 mL -80°C
80:20 methanol: water on dry ice. The supernatants from two rounds of extraction were
combined, dried under N2, resuspended in 1 mL water, and analyzed within 6 h by reversedphase ion-pairing chromatography coupled with negative-mode electrospray-ionization highresolution MS on a stand-alone orbitrap (Thermo)41. For lipid extraction, cells were quenched
with 2 mL -20°C 0.1M HCl in 50:50 methanol:water solution, incubated on ice for 20 min. The
resulting supernatant was extracted with 1 mL chloroform. The chloroform extract was dried
under N2, saponified with 1 mL 0.3 M KOH in 9:1 methanol:water solution at 80°C for 1 h, and
acidified by formic acid. Fatty acids were then extracted using 1 mL hexane twice. The hexane
from two rounds of extraction was combined, dried under nitrogen, resuspended in 1 mL 1:1:0.3
122
chloroform:methanol:water, and analysed by reversed-phase ion-pairing chromatography
coupled with negative-mode electrospray ionization high-resolution MS on a quadrupole timeof-flight mass spectrometer (Agilent Technologies model 6550)42. All isotope labeling patterns
were corrected for natural 13C-abundance.
4.5.4. Quantification of NADPH consumption.
NADPH consumption by reductive biosynthesis in the proliferating cells was assessed as
described previously5. Briefly, we determined experimentally the biomass fraction (normalized
to cell number) of DNA (DNA assay kit, Life Technologies), total protein (DC protein assay kit,
Bio-Rad), proline (LC-MS), and fatty acids (LC-MS). Then, for each component, we measured
the relative contribution of different acquisition routes (e.g. biosynthesis versus uptake). The
resulting total NADPH consumption is given by:
𝑃𝑟𝑜𝑑𝑢𝑐𝑡 𝑖
NADPH consumption =∑𝑖 (
𝑃𝐶𝑉
𝑁𝐴𝐷𝑃𝐻 𝑐𝑜𝑛𝑠𝑢𝑚𝑒𝑑
)∗(
𝑃𝑟𝑜𝑑𝑢𝑐𝑡 𝑖
) ∗Growth rate
(5)
For the differentiating cells, because growth rate is not well-defined and biomass composition is
changing, we instead inferred DNA synthesis based on rate of increase in cell number (which
was negligible by day 5) and measured directly the rate of increase in protein and fat:
𝑁𝑒𝑤𝑙𝑦 𝑆𝑦𝑛𝑡ℎ𝑒𝑠𝑖𝑧𝑒𝑑 𝑃𝑟𝑜𝑑𝑢𝑐𝑡 𝑖
NADPH consumption =∑𝑖 (
𝑃𝐶𝑉
𝑁𝐴𝐷𝑃𝐻 𝑐𝑜𝑛𝑠𝑢𝑚𝑒𝑑
)∗(
𝑃𝑟𝑜𝑑𝑢𝑐𝑡 𝑖
)
(6)
Taking NADPH consumed by fatty acid biosynthesis for example, we corrected for newly
synthesized fatty acid based on 13C-enrichment from [U-13C]glucose and [U-13C]glutamine. For
each fatty acid species, its unlabeled fraction comes either from pre-existing fat (synthesized or
taken up before the labeling began) or fat taken up directly from serum in the medium; neither of
these consume NADPH. Since only the fraction of fatty acid newly synthesized from 2C units
123
during the labeling interval uses NADPH, the amount of a newly synthesized fatty acid
species(palmitate for example) where labeling fractions are [M+0], [M+1], etc. is given by:
𝑁𝑒𝑤𝑙𝑦 𝑠𝑦𝑛𝑡ℎ𝑒𝑠𝑖𝑧𝑒𝑑 𝑝𝑎𝑙𝑚𝑖𝑡𝑎𝑡𝑒 = 𝑃𝑎𝑙𝑚𝑖𝑡𝑎𝑡𝑒 𝑎𝑚𝑜𝑢𝑛𝑡 ∗ ∑16
𝑖=1
[𝑀+𝑖]∗𝑖
16
(7)
4.5.6. CO2 release and oxPPP flux.
14
CO2 fluxes were quantified as previously described5. Briefly, cells were grown in 12.5 cm2
tissue culture flasks with DMEM with low bicarbonate (0.74g/L) and additional HEPES (6 g/L,
pH 7.4). 14C tracer was added to the media and the flask was sealed with a stopper with a center
well (Kimble Chase) containing thick pieces of filter paper saturated with 200 µL 10 M KOH.
Cells were incubated for 24 h. Thereafter, 1 mL 3 M acetic acid was added to the culture medium
to quench metabolism. Filter paper (and any associated residue) in the center well was collected
into liquid scintillation cocktail (PerkinElmer). The signal was corrected for intracellular
substrate labelling according to percentage of radioactive tracer in the media, and fraction of
particular intracellular metabolite from media uptake, which was measured by 13C-tracer. The
14
C flux (per cell number per time) after correction is given by:
14
𝐶14 𝑠𝑖𝑔𝑛𝑎𝑙
CO2=𝐿𝑎𝑏𝑒𝑙𝑖𝑛𝑔 𝑡𝑖𝑚𝑒∗𝐶𝑒𝑙𝑙 𝑛𝑢𝑚𝑏𝑒𝑟 ∗
𝐶12 𝑠𝑢𝑏𝑠𝑡𝑟𝑎𝑡𝑒
𝐶14 𝑡𝑟𝑎𝑐𝑒𝑟
𝐹𝑟𝑎𝑐𝑡𝑖𝑜𝑛 𝑚𝑒𝑑𝑖𝑢𝑚 𝑛𝑢𝑡𝑟𝑖𝑒𝑛𝑡 𝐶13 𝑙𝑎𝑏𝑒𝑙𝑒𝑑
∗ 𝐹𝑟𝑎𝑐𝑡𝑖𝑜𝑛 𝑖𝑛𝑡𝑟𝑎𝑐𝑒𝑙𝑙𝑢𝑙𝑎𝑟 𝑠𝑢𝑏𝑠𝑡𝑟𝑎𝑡𝑒 𝐶13 𝑙𝑎𝑏𝑒𝑙𝑒𝑑
(9)
4.5.7. Malic enzyme carbon flux.
Gross carbon flux from malate to pyruvate, ignoring compartmentation, was quantified based on
pyruvate labeling from [U-13C]glutamine. Since the observed fraction of M+1 and M+2 pyruvate
were small (sum of both is less than 0.5%) relative to M+3 pyruvate (3%, Appendix Figure C2),
124
the analysis is based solely on the observed M+3 pyruvate signal corrected for the fraction of
malate which is capable of making M+3 pyruvate. Forward flux from [U-13C]glutamine results in
M+4 malate [1,2,3,4-13C] (fractional abundance ~ 20%). Reductive carboxylation of glutamine
coupled to citrate lyase can produce M+3 malate (total fractional abundance ~ 8%) in the form
[2,3,4-13C], which produces M+2 not M+3 pyruvate. Malate M+3 exists also as [1,2,3-13C],
which produces M+3 pyruvate. Assuming rapid exchange between malate and fumarate (which
is symmetric), the abundances of [1,2,3-13C] and [2,3,4-13C]malate will be equal; incomplete
exchange will result in less [1,2,3-13C].
𝑓𝑀𝐸
𝑓𝐺𝑙𝑦𝑐𝑜𝑙𝑦𝑠𝑖𝑠
Pyr[M+3]
= Pyr
unlabeled
∗
Mal𝑡𝑜𝑡𝑎𝑙
Mal[M+4] + 𝑎∗Mal[M+3]
(𝑎 =
Mal[1,2,3−13 C]
Mal[1,2,3−13 C] + Mal[2,3,4−13 C]
≈ 0.5)
(8)
Eqn. 8 applies when malic enzyme flux is much less than glycolytic flux; otherwise, it is
necessary to include a term to account for unlabeled pyruvate made via malic enzyme.
4.5.8. Quantification of fraction NADP2H.
The whole-cell fraction of NADPH redox active hydride labeled, (𝑥), was determined from the
labeling pattern of NADP+ and NADPH from the same sample incubated with 2H-precusors. Let
a0 be the unlabeled fraction of NADP+, a1 be its [M+1] fraction, etc. We obtained 𝑥 to best fit the
mass isotope distributions vectors (𝑁𝐴𝐷𝑃+ , 𝑁𝐴𝐷𝑃𝐻) by least square fitting in MATLAB:
𝑎0
+
𝑁𝐴𝐷𝑃 = [𝑎1 ]
𝑎2
𝑎0 (1 − 𝑥)
𝑎 (1 − 𝑥) + 𝑎0 𝑥
𝑁𝐴𝐷𝑃𝐻 = [ 1
]
𝑎2 (1 − 𝑥) + 𝑎1 𝑥
𝑎2 𝑥
125
(10)
4.5.9. Calculation of ME1-dependent NADP2H flux.
Converting the whole-cell NADPH labeling fraction from [2,2,3,3-2H]dimethyl succinate into
the fractional NADPH contribution of malic enzyme requires two corrections: (i) 2H-labeling of
malate’s C2 hydride (Eqn. 11), (ii) deuterium’s kinetic isotope effect of ME1.
MalC2−deuteron
Mal
=
[2−2 H]Mal
Mal
+
[2,3−2 H]Mal
Mal
Mal[M+1] +Mal[M+2]
=(
Mal
)−(
Asp[M+1]
Asp
−
Mal[M+2]
Mal
)
(11)
Correction for isotope effect was as previously described5:
𝐹𝐷
𝐹𝐻
=
𝑥
𝑣
∗ 𝐷
(1−𝑥) 𝑣
(12)
𝐻
where FD is flux producing NADP2H, FH is flux producing unlabeled NADPH, x is the fraction
of [2-2H]malate (7.9% calculated from Eqn. 9), and 𝑣𝐷 /𝑣𝐻 is the kinetic isotope effect for the
isolated enzyme, 1.47 ± 0.0243. Error estimates for the calculated NADPH production fluxes
include propagation of the experimental error in the substrate labeling fractions.
Determination of the cytosolic NADPH labeling fraction based on fatty acid 2H-labeling requires
correction for (i) the fraction of the individual fatty acids species that is imported rather than
synthesized de novo and (ii) any 2H-labeling that can enter fatty acids via their acetyl-groups. In
the proliferating condition, cells were maintained at ≤ 80% confluency (ambient oxygen) with no
differentiation reagents . In the differentiating condition, both differentiation cocktail and tracer
were added starting on day 0. To correct for the import of fatty acids, the mass isotope
distribution vectors for combined [U-13C]glucose and [U-13C]glutamine labeling and separately
for [2,2,3,3-2H]dimethyl succinate labeling were corrected for natural 13C-abundance. Then, the
126
observed M+0 fraction from the combined [U-13C]glucose and [U-13C]glutamine labeling
experiment was subtracted from the M+0 fraction from the [2,2,3,3-2H]dimethyl succinate
labeling experiment, as this fraction of fatty acids was not made during the duration of the
labeling experiment. Because fatty acids can potentially become 2H-labeled via passage of 2H to
the acetyl group of acetyl-CoA, in addition to via NADPH, we measured acetyl group labeling
(M+1) from [2,2,3,3-2H]dimethyl succinate based on LC-MS analysis of acetylated compounds
(e.g. N-acetyl-aspartate) relative to their unacetylated precursors (e.g. aspartate), with the
average labeling fraction 0.3%. Eight acetyl groups are required to produce one palmitate
molecule and the probability that an acetyl-CoA deuterated at C1 will pass that deuterium to the
fatty acid chain is at most two-thirds (at least one of three C1 hydrogen atoms is lost during the
fatty acyl chain extension reaction; more may be lost by H-D exchange 44). Thus, the resulting
palmitate labeling follows a binomial distribution with n=8, p=0.002:
𝑀0
𝑀
fatty acid 2H-labeling from acetyl groups [ 1 ] =
𝑀2
⋮
0.9841
0.0158
[
]
0.0001
⋮
(13)
Let a0 be the unlabeled fraction of fatty acid from NADPH, a1 be [M+1] fraction where NADPH
𝑛
put one 2H atom on, etc., then 𝑎𝑘 = (𝑘 ) 𝐴𝑘 (1 − 𝐴)𝑛−𝑘 where A is the NADP2H fraction (for
palmitate, n=14; for additional fatty acid species, see Appendix Figure C7).
𝑀0 ∗ 𝑎0
𝑀0 ∗ 𝑎1 + 𝑀1 ∗ 𝑎0
The experimentally observed fatty acid labeling = [
]
𝑀0 ∗ 𝑎2 + 𝑀1 ∗ 𝑎1 + 𝑀2 ∗ 𝑎0
⋮
(14)
We obtained the A by least square fitting to a binomial function in Matlab to best match the
experimentally observed fatty acid 2H-labeling pattern.
127
4.5.10. Metabolic flux analysis.
Fluxes were computed based on the network shown in Figure 4.4d with, in addition, both
cytosolic and mitochondrial aspartate and alanine transamination reactions and a protein
degradation reaction that produces unlabeled amino acids in balanced amounts based on their
naturally occurring frequency in whole cell protein. Measurements that were used to constrain
the model were glucose, glutamine, and oxygen uptake, with the latter used to constrain total
NADH production and thus TCA turning; lactate, glycerol, and non-essential amino acid
secretion (Supplementary Table 1); total NADPH consumption; lipid and protein synthesis rate;
oxPPP flux as measured by 14C-CO2 release; 13C-labeling of cellular metabolites (glucose-6phosphate, 3-phosphoglycerate, phosphoenolpyruvate, pyruvate, lactate, alanine, citrate, αketoglutarate, malate and aspartate) from experiments feeding [U-13C]glucose or feeding [U13
C]glutamine (Appendix Figure C3); saponified fatty acid measurements from [U-13C]glucose
and [U-13C]glutamine labeling experiments which were used to compute the cytosolic labeling
fractions of acetyl-CoA. When indicated, the model was also constrained with the ME1 flux as
measured using 2H tracers.
A cumulated isotopomer (cumomer)45 balance model was generated using the carbon mapping
network of central carbon metabolism and 13CFLUX2 software (www.13cflux.net)46. Using this
model, each flux distribution simulated for both the [U-13C]glucose and [U-13C]glutamine
conditions, and fluxes were optimized by minimizing the variance-weighted sum of squared
residuals (Var-SSR) between the simulated and measured labeling fractions and uptake/secretion
rates using the interior-point algorithm47 in Matlab. To avoid overfitting of labeling fractions that
were associated (due to unusually low random variation in the individual measurements) with an
128
atypically small standard deviation, the standard deviation of each individual fractional labeling
measurement was floored to 0.8%, which is the mean standard deviation across all such data
(excluding fractional labeling < 1%). As malate measurement represented the mixture of
cytosolic and mitochondrial pools, a linear combination of two malate pools was fitted to the
measured fractions. The non-convex optimization was solved starting from different initial flux
distributions to account for the presence of local minima. Confidence intervals were estimated
for a single reaction at a time by (i) starting from the best-scoring flux distribution, (ii) iteratively
increasing or decreasing the flux through that reaction, (iii) optimizing all of the other fluxes, (iv)
determining the increase in the objective function Var-SSR, (v) defining the upper and lower
bounds of the confidence interval as the flux where Var-SSR increased by 3.84 (χ2 cutoff for
p<0.05 with 1 degree of freedom)48. The code used for metabolic flux analysis is available on a
Github public repository: https://github.com/PrincetonUniversity/adipocytes
4.6. References
1.
Voet, D. & Voet, J. Biochemistry. (New york: J. Wiley & Sons, 2004).
2.
Tibbetts, A. S. & Appling, D. R. Compartmentalization of Mammalian folate-mediated
one-carbon metabolism. Annu. Rev. Nutr. 30, 57–81 (2010).
3.
Wise, D. R. et al. Hypoxia promotes isocitrate dehydrogenase-dependent carboxylation of
α-ketoglutarate to citrate to support cell growth and viability. Proc. Natl. Acad. Sci. U. S.
A. 108, 19611–6 (2011).
129
4.
WHO. Glucose-6-phosphate dehydrogenase deficiency. Bull. World Heal. Organiztion 67,
601–611 (1989).
5.
Fan, J. et al. Quantitative flux analysis reveals folate-dependent NADPH production.
Nature 510, 298–302 (2014).
6.
Lewis, C. a et al. Tracing Compartmentalized NADPH Metabolism in the Cytosol and
Mitochondria of Mammalian Cells. Mol. Cell 55, 253–263 (2014).
7.
Nguyen, P. et al. Liver lipid metabolism. J. Anim. Physiol. Anim. Nutr. (Berl). 92, 272–83
(2008).
8.
Young, J. W., Shargo, E. & Lardy, H. A. Metabolic Control of Enzymes Involved in
Lipogenesis and Gluconeogenesis *. 3, 1687–1692 (1964).
9.
Wise, E. M. & Ball, E. G. Malic enzyme and lipogenesis. Proc. Natl. Acad. Sci. U. S. A.
52, 1255–1263 (1964).
10.
Wise, L. S., Sul, H. S. & Rubin, C. S. Coordinate regulation of the biosynthesis of ATPcitrate lyase and malic enzyme during adipocyte differentiation. Studies on 3T3-L1 cells.
J. Biol. Chem. 259, 4827–32 (1984).
11.
Si, Y., Yoon, J. & Lee, K. Flux profile and modularity analysis of time-dependent
metabolic changes of de novo adipocyte formation. Am. J. Physiol. Endocrinol. Metab.
292, E1637–46 (2007).
130
12.
Katz, J. & Rognstad, R. The metabolism of tritiated glucose by rat adipose tissue. J. Biol.
Chem. 241, 3600–10 (1966).
13.
Kather, H., Rivera, M. & Brand, K. Interrelationship and control of glucose metabolism
and lipogenesis in isolated fat-cells. Control of pentose phosphate-cycle activity by
cellular requirement for reduced nicotinamide adenine dinucleotide phosphate. Biochem.
J. 128, 1097–102 (1972).
14.
Flatt, J. P. & Ball, E. G. ARTICLE : Studies on the Metabolism of Adipose Tissue : XV .
AN EVALUATION OF THE MAJOR PATHWAYS OF GLUCOSE CATABOLISM AS
INFLUENCED BY INSULIN AND EPINEPHRINE on the Metabolism of Adipose.
(1964).
15.
Green, H. & Meuth, M. An established pre-adipose cell line and its differentiation in
culture. Cell 3, 127–33 (1974).
16.
Rosen, E. D. & MacDougald, O. a. Adipocyte differentiation from the inside out. Nat.
Rev. Mol. Cell Biol. 7, 885–96 (2006).
17.
Shreves, D. S. & Levy, H. R. Kinetic mechanism of glucose-6-phosphate dehydrogenase
from the lactating Rat Mammary Gland. Jbc 255, 2670–2677 (1980).
18.
Yang, X. M. & MacKenzie, R. E. NAD-dependent methylenetetrahydrofolate
dehydrogenase-methenyltetrahydrofolate cyclohydrolase is the mammalian homolog of
the mitochondrial enzyme encoded by the yeast MIS1 gene. Biochemistry 32, 11118–
11123 (1993).
131
19.
Tibbetts, A. S. & Appling, D. R. Compartmentalization of Mammalian folate-mediated
one-carbon metabolism. Annu. Rev. Nutr. 30, 57–81 (2010).
20.
Zhang, Z., Chen, L., Liu, L., Su, X., Rabinowitz, J. D. Chemical basis for deuteruim
labeling of fat and NADPH. J. Am, Chem. Soc.139 (41), 14368-14371(2017).
21.
Jitrapakdee, S. et al. Structure, Mechanism and Regulation of Pyruvate Carboxylase.
Biochem. J 413, 369–387 (2008).
22.
Rutter, W. J. & Lardy, H. a. Purification and properties of pigeon liver malic enzyme. J.
Biol. Chem. 233, 374–382 (1958).
23.
DeBerardinis, R. J. et al. Beyond aerobic glycolysis: transformed cells can engage in
glutamine metabolism that exceeds the requirement for protein and nucleotide synthesis.
Proc. Natl. Acad. Sci. U. S. A. 104, 19345–50 (2007).
24.
Yuan, Z. & Hammes, G. Elementary Steps in the Reaction Mechanism of Chicken Liver
Fatty Acid Synthase. 259, 6748–6751 (1984).
25.
Jiang, P., Du, W., Mancuso, A., Wellen, K. E. & Yang, X. Reciprocal regulation of p53
and malic enzymes modulates metabolism and senescence. Nature 493, 689–93 (2013).
26.
Yaguang Si, Hai Shi, and K. L. Impact of Perturbed Pyruvate Metabolism on Adipocyte
Triglyceride Accumulation. Metab Eng 11, 382–390 (2009).
132
27.
Kim, J. W., Tchernyshyov, I., Semenza, G. L. & Dang, C. V. HIF-1-mediated expression
of pyruvate dehydrogenase kinase: A metabolic switch required for cellular adaptation to
hypoxia. Cell Metab. 3, 177–185 (2006).
28.
Lu, C. W., Lin, S. C., Chen, K. F., Lai, Y. Y. & Tsai, S. J. Induction of pyruvate
dehydrogenase kinase-3 by hypoxia-inducible factor-1 promotes metabolic switch and
drug resistance. J. Biol. Chem. 283, 28106–28114 (2008).
29.
Hosogai, N. et al. Adipose tissue hypoxia in obesity and its impact on adipocytokine
dysregulation. Diabetes 56, 901–911 (2007).
30.
Trayhurn, P. Hypoxia and adipose tissue function and dysfunction in obesity. Physiol.
Rev. 93, 1–21 (2013).
31.
Mullen, A. R. et al. Reductive carboxylation supports growth in tumour cells with
defective mitochondria. Nature 481, 385–388 (2011).
32.
Kamphorst, J. J., Chung, M. K., Fan, J. & Rabinowitz, J. D. Quantitative analysis of
acetyl-CoA production in hypoxic cancer cells reveals substantial contribution from
acetate. Cancer Metab. 2, 1–8 (2014).
33.
Price, N. E. & Cook, P. F. Kinetic and Chemical Mechanisms of the Sheep Liver. Arch.
Biochem. Biophys. 336, 215–223 (1996).
34.
Hermes, J. D., Roeske, C. a, O’Leary, M. H. & Cleland, W. W. Use of multiple isotope
effects to determine enzyme mechanisms and intrinsic isotope effects. Malic enzyme and
glucose 6-phosphate dehydrogenase. Biochemistry 21, 5106–5114 (1982).
133
35.
Al-Dwairi, A., Pabona, J. M. P., Simmen, R. C. M. & Simmen, F. a. Cytosolic malic
enzyme 1 (ME1) mediates high fat diet-induced adiposity, endocrine profile, and
gastrointestinal tract proliferation-associated biomarkers in male mice. PLoS One 7,
e46716 (2012).
36.
Lee, C. Y., Lee, S. M., Lewis, S. & Johnson, F. M. Identification and biochemical analysis
of mouse mutants deficient in cytoplasmic malic enzyme. Biochemistry 19, 5098–103
(1980).
37.
Koh, H.-J. et al. Cytosolic NADP+-dependent isocitrate dehydrogenase plays a key role in
lipid metabolism. J. Biol. Chem. 279, 39968–39974 (2004).
38.
Wellen, K. E. et al. ATP-citrate lyase links cellular metabolism to histone acetylation.
Science 324, 1076–80 (2009).
39.
Boucher, A. et al. Biochemical mechanism of lipid-induced impairment of glucosestimulated insulin secretion and reversal with a malate analogue. J. Biol. Chem. 279,
27263–71 (2004).
40.
Munger, J. et al. Systems-level metabolic flux profiling identifies fatty acid synthesis as a
target for antiviral therapy. Nat. Biotechnol. 26, 1179–1186 (2008).
41.
Lu, W. et al. Metabolomic analysis via reversed-phase ion-pairing liquid chromatography
coupled to a stand alone orbitrap mass spectrometer. Anal. Chem. 82, 3212–21 (2010).
42.
Sutterlin, H. a, Zhang, S. & Silhavy, T. J. Accumulation of phosphatidic acid increases
vancomycin resistance in Escherichia coli. J. Bacteriol. (2014). doi:10.1128/JB.01876-14
134
43.
Edens, W. a, Urbauer, J. L. & Cleland, W. W. Determination of the chemical mechanism
of malic enzyme by isotope effects. Biochemistry 36, 1141–7 (1997).
44.
Seyama, Y. et al. Identification of sources of hydrogen atoms in fatty acids synthesized
using deuterated water and stereospecifically deuterium labelled NADPH by gas
chromatographic mass spectrometric analysis. Biomed. Mass Spectrom. 5, 357–361
(1978).
45.
Wiechert, W., Möllney, M., Isermann, N., Wurzel, M. & De Graaf, A. a. Bidirectional
reaction steps in metabolic networks: III. Explicit solution and analysis of isotopomer
labeling systems. Biotechnol. Bioeng. 66, 69–85 (1999).
46.
Weitzel, M. et al. 13CFLUX2 - High-performance software suite for 13C-metabolic flux
analysis. Bioinformatics 29, 143–145 (2013).
47.
Waltz, R. a., Morales, J. L., Nocedal, J. & Orban, D. An interior algorithm for nonlinear
optimization that combines line search and trust region steps. Math. Program. 107, 391–
408 (2006).
48.
Antoniewicz, M. R., Kelleher, J. K. & Stephanopoulos, G. Determination of confidence
intervals of metabolic fluxes estimated from stable isotope measurements. Metab. Eng. 8,
324–337 (2006).
135
Chapter 5. Discussion
NAD(H) and NADP(H) are two essential redox cofactors with different physiological functions.
NAD(H) plays an essential role in epigenetics and energy metabolism, while NADP(H) drives
antioxidant defense and reductive biosynthesis. It is accordingly important to measure NAD(H)
and NADP(H) metabolism, and how they differ across cell types, tissues, physiological states
and diseases, and how they respond to perturbation by drugs and nutraceuticals. There are two
fundamental questions in understanding the metabolism of these coenzymes- 1) how the
dinucleotide backbone is synthesized and consumed, and 2) how the hydride is transferred on
and off from the backbone. The metabolism of NAD backbone is complex, with multiple
production routes and a myriad of consuming enzymes including the one making NADP. For the
hydride transfer, however, the role of NAD-NADH cycling has been well established
(glycolysis, TCA and beta-oxidation), while the rational for use of one pathway over another to
make NADPH from NADP remains an open question. Therefore, this thesis aims to dissect
redox metabolism through 1) quantifying the synthesis and consumption of NAD backbone, and
2) investigating NADPH hydride transfer.
In Chapter 2, we quantified NAD synthesis and consumption fluxes through introducing labeled
NAM, Trp, NA and NAM-contained nucleotides followed by measuring NAD labeling using
mass spectrometry. We later applied this approach to investigate how NAD is synthesized in
mitochondria in Chapter 3. By developing broadly applicable NAD tracing methods, we have
been able to gather a substantial body of foundational data regarding NAD metabolism, which
collectively provide a valuable resource for future research. NAD flux tracing should be of
excellent value in the following three aspects:
136
First, tracing genetically engineered mouse models would unravel the link between metabolic
signal and protein expression. From an autophagy-deficient mouse model (ATG7flox/flox), we
applied the isotopic tracing technique to measure NAD flux and found a significant decrease in
NAD de novo synthesis in liver. This has led to the preliminary result identifying the decreased
protein expression of HAAO, catalyzing one of the multiple steps in NAD de novo synthesis
(data not shown in this thesis). This kind of regulation would not be captured without metabolic
tracing technique.
Second, tracing NAD synthesis and consumption in vivo helps understand the role of NAD
during aging and disease states. By combining this isotope tracer measurement with
pharmacological modulation of PARP1/2 and SIRT1/2, and inhibitors for CD38, we assigned
each enzyme the contribution in cultured cells. We also quantified the effect of DNA damage
through faster PARP-mediated consumption in cultured cells. Clearly, much remains to be
learned concerning NAD metabolism in tissues, distinct from cultured cells. One remaining
question is the contributions of each enzyme in murine tissues, and how they change under nonbasal conditions. Tissues other than liver relied almost exclusively on circulating NAM to make
NAD. Therefore, the question can be approached through 1) manipulate NAM availability in
circulation, 2) measure how NAD concentration in each tissue changes under different NAM
availability, and 3) quantify the consumption fluxes. This would help discover the mechanism of
decreasing NAD in aging and disease states.
Third, dissecting NAD metabolism in vivo helps develop therapies that boost NAD levels. By
exploring the response of NAD levels and fluxes to candidate NAD-boosting nutraceuticals, and
measuring NR breakdown during assimilation, we were able to draw new conclusions potentially
137
relevant to treatment of cancer and age-dependent pathologies. We found that neither NR or
NMN was able to enter the circulation intact in substantial quantities when delivered orally. One
remaining challenge is to protect the bond between its nicotinamide and ribose component, to
elongate degradation half-lives. We observed that IV administration of either compound results
in direct incorporation into NAD, proving that the route of delivery has a profound effect on the
ability of these nutraceuticals to reach target tissues. Thus, it will be extremely important to
optimize the route of delivery, the molecular structure and formulation to elevate tissue NAD
levels.
In Chapter 4 we examined quantitatively NADPH production pathways. In transformed growing
cells, there is physiologic efficiency in using the oxPPP and folate metabolism for NADPH
production and for nucleotide synthesis. We examined NADPH metabolism in adipocytes (3T3L1 cells), which upon differentiation do not engage in significant nucleotide synthesis but remain
biosynthetically active. This led to the distinct metabolic requirements. We proved the leading
role of malic enzyme, using a combination of classical 13C-glutamine tracing augmented by flux
analysis and a newly developed method for directly tracing 2H-NADPH production by malic
enzyme. The malic enzyme utilization serves dual purposes in adipocytes: (i) production of
cytosolic acetyl-CoA and (ii) generation of NADPH from reducing equivalents originally
derived from glycolysis as NADH.
The two tracers that we provided in Chapter 4, [2,2,3,3-2H]dimethyl succinate or [4-2H]glucose,
both produce [2-2H]malate which in turn makes NADP2H. Production of NADP2H by [2,2,3,32
H] dimethyl succinate is more direct, but relies on a non-physiologic uptake mechanism and
transfer of malate from mitochondrion to cytosol. Therefore, further modification is required to
138
make this tracer more suited to potential in vivo application. Accordingly, [4-2H]glucose may be
more generally applicable, as it uses a physiological uptake mechanism and sequence of
cytosolic reactions to label malate. It is essential for future work to apply these 2H-tracers in vivo,
to examine quantitatively NADPH production pathways in murine tissues under normal and
disease states.
Together, this thesis broadly described the metabolism of redox cofactors NAD(H) and
NADP(H) from a more quantitative and chemical engineering perspective than has been done
before. Main findings included the NAD(P) synthesis-breakdown in cultured cells, and the
difference in the backbone metabolism across cell lines and murine tissues. By dissecting the
redox cofactor metabolism, this study enhanced depth and novelty to the NAD(P) biology, and
provided fundamental tools for future research on redox metabolism.
139
Appendix
Appendix A. Additional Information for Chapter 2
Appendix Figure A1. In T47D cells, there is not de novo NAD synthesis from tryptophan and
NAD M+2 does not arise due to activity of the de novo pathway enzyme QPRT. (a) In cells
grown in [U-13C]Trp in normal DMEM (1x NAM) or NAM-free DMEM (0x NAM) for 4 days,
intracellular tryptophan is essentially fully labeled. (b) NAD is not detectably labeled. Absolute
signal intensity for Trp and NAD are normalized to the signal in standard DMEM. (c) NAD
concentration in cells fed 2H-NAM. (d) Indistinguishable labeling of NAD and NADH (left) and
NADP and NADPH (right) in cells fed 2H-NAM. (e) Knockdown of QPRT does not alter the
ratio between NAD [M+2] and NAD [M+3] following 6 h or 12 h of 2H-NAM labeling. (f)
Western blot for QPRT knockdown. (g) Concentrations of NAD, NADH, NADP and NADPH.
Data are mean ± s.d., n = 3.
140
Appendix Figure A2. Role of growth, PARP, sirtuins, and CD38 in NAD turnover in selected
cell types. (a) NAD concentration in XPA-deficient or XPA-restored cells (relative to restored
cells). (b) NAD concentration and labeling in XPA-deficient and XPA-restored cells treated with
DMSO (negative control) or olaparib (10 μM, PARP1/2 inhibitor) for 6 h. Olaparib was added
simultaneously with switching cells into 2H-NAM. (c) Stability of 50 μM sirtinol in DMEM
supplemented with 10% DFBS (37°C). (d) NAD concentration and labeling in T47D cells
treated with DMSO (negative control), 25 μM sirtinol (+), 50 μM sirtinol (++), or 100 μM
sirtinol (+++), for 8 h. Sirtinol was added simultaneously with switching cells into 2H-NAM. (e)
Growth rate of MCF7, T47D and differentiating C2C12 cells. Lines are single exponential fits.
(f) Measurement of NAD consumption by PARPs and sirtuins in MCF7 cells. NAD
concentration and labeling was measured in cells treated with DMSO, olaparib (10 μM), or
141
sirtinol (25 μM) for 4 h or 9 h. Drug was added simultaneously with switching cells into 2HNAM. (g) Measurement of NAD consumption by NAD kinase in MCF7 cells. Cells were fed 2HNAM starting at t = 0 and NAD and NADP labeling were measured. NAD labeling significantly
exceeded NADP labeling at early time points (**p<0.01, * p<0.05, paired t-test). (h, i) Same as
(f, g) but in C2C12 cells. For panel a-i, data are mean ± s.d., n = 3. (j) CD38 does not consume
substantial NAD in T47D cells. Consumption rates were calculated based on 4 h incubation with
2
H-NAM and quercetin (50μM, CD38 inhibitor) or apigenin (25μM, CD38 inhibitor). Bars are
mean ± 95% confidence interval of fout. (k) Across the same 12 cell lines as Figure 4, NAD usage
for growth correlates with growth rate (p=0.01).
Appendix Figure A3. Contributors to NAD biosynthesis in cell lines. (a) NAD biosynthesis and
consumption schematic. Trp, Tryptophan; NA, nicotinic acid; NR, nicotinamide riboside; NAM,
142
nicotinamide; NMN, nicotinamide ribotide; QA, quinolinic acid; NAAD, nicotinic acid adenine
dinucleotide. (b) Fraction of NAD in T47D cells coming from the indicated supplemented
substrate based on isotope tracing for 24 h. Compound concentrations are reported relative to
nicotinamide in commercial DMEM (32 μM NAM = 1x). (c) NAD concentration in T47D cells
fed DMEM supplemented with additional precursors for 48 h. (d) Labeling fraction of NAD in
cells fed [U-13C]Trp (5x) or [U-13C]NA (1x) in DMEM for 48 h. Data are mean ± s.d., n = 3. (e)
Across cell lines, the traction of NAD coming from NA (data from panel d) correlates with
NaPRT1 mRNA expression (data from https://portals.broadinstitute.org/ccle/).
143
Appendix Figure A4. Metabolic impact and assimilation routes of NR, NMN, and NAD.
Related to Figure 5 and Figure 7. (a) Heat map of metabolite concentration changes in T47D
cells in response to NR, NMN, NAD (5x the concentration of NAM, individually in the presence
of NAM) after 24 h. Each column represents one sample. Data were normalized to cell number.
All individual samples were then normalized to the average of the control (DMEM) samples. (b)
Schematic illustrating (i) the intracellular steps at which of gallotannin (Gallo, NMNAT
inhibitor) and FK866 (NAMPT inhibitor) target NAD metabolism, (ii) the extracellular step at
144
which Ap4A blocks the degradation of NAD to NMN, and (iii) the extracellular steps at which
PPADS and CMP are expected based on literature to act (grey38) or were detected to act in this
study (green). (c) Experimental design to test pathway steps required for assimilation of NR and
NAD. Cells were fed 2H-NAM for 48 h, after which unlabeled precursors (NAD or NR, 1x) and
inhibitors (100 nM FK866, 100 µM gallotannin, 25 µM PPADS, 1 mM Ap4A or 2 mM CMP)
were simultaneously added for 12 h. (d) NAD concentration and labeling in T47D cells with 12
h FK866 or gallotnanin treatment. Newly added NR bypassed FK866 but was blocked by
gallotannin, while newly added NAD was taken intact partially and thus bypassed both steps. (e)
NAD concentration and labeling in T47D cells treated for 12 h with PPADS, Ap4A ,or CMP.
Blockade of NAD degradation by these inhibitors (as verified in panel f) partially but not fully
blocked assimilation of extracellular NAD into intracellular NAD, suggesting that extracellular
NAD can contribute to the intracellular NAD pool both by direct uptake and by extracellular
degradation to NR followed by cellular NR uptake and metabolism. (f) Degradation of NAD
(300 µM) into NMN and NR in fresh DMEM supplemented with 10% dialyzed FBS at 37°C,
and its inhibition by PPADS, Ap4A or CMP (at the above concentrations). Unexpectedly, CMP
prevented degradation of NAD to NMN, rather than exclusively blocking NMN to NR, and
PPADS was only modestly blocked degradation to NMN, despite preventing the appearance of
NR. (g) Degradation of NR and NMN into NAM in blood at 37°C. NAM concentrations were
normalized to the added NR and NMN concentration (100 µM). (h) Stability of 100 μM NR,
NMN and NAD in DMEM supplemented with 10% DFBS (37°C). Concentrations were
normalized to 0 h. (i) NAD concentration in T47D cells fed 2H,13C-NR (5x, 32μM=1x) for 12 h.
Medium was either refleshed every 2 h, or remained unchanged. Data are mean ± s.d., n = 3.
Lines are to guide the eye.
145
Appendix Figure A5. De novo NAD synthesis. (a) De novo pathway with labeling states of
intermediates from [U-13C] Trp indicated. (b) Isotopic fractions of tryptophan and NAM in
serum. 13C-Trp was infused via jugular vein at 5 nmol/g/min. Lines are to guide the eye. (c)
Labeled fractions of tryptophan and NAD in tissues after 5 h [U-13C] Trp infusion. Note that
NAD labeling is greatest in liver. Data are mean ± s.d., n=3. (d) Liver and kidney have the
complete set of NAD de novo synthesis enzymes. Data are from the Human Protein Atlas.
146
Appendix Figure A6. NAM and N-methylnicotinamide (MeNAM) labeling in serum and
tissues. MeNAM displayed indistinguishable labeling across tissues, indicating rapid sharing of
MeNAM (unlike NAM itself) throughout the body via the circulation. Mice were either infused
with 2H-NAM for 2 h (a), or co-infused with 2H-NAM and 13C-Trp for 24 h (b). Data are mean ±
s.d., n=2.
147
Appendix Figure A7. Measured and model-predicted NAD and NAM labeling fractions in
tissues. (a) For co-infusion of [U-13C] Trp and [2,4,5,6-2H] NAM (20:1 ratio, equal to their
physiological ratio in serum) for 5 h. Correlation coefficient is 0.993. (b) For co-infusion of [U13
C]NA and [2,4,5,6-2H] NAM (1:10 ratio, equal to their ratio in serum) for 5 h. Correlation
coefficient is 0.997. Measured data are mean ± s.d., n=3.
148
Appendix Table A1. NAD precursor availability in DMEM, mouse chow, the serum of mice,
and circulatory turnover fluxes (Fcirc). DMEM and chow data are from the manufacturer. Serum
data are LC-MS measurements made here (mean ± s.d., n = 3). Turnover fluxes were calculated
from infusion rate and steady state labeling percentage (mean ± s.d., n = 3) (Method as
described, Hui et al, Nature, 2017).
Concentrations
Mouse chow Mouse serum
13.7 mM
46±4 µM
Trp
DMEM
80 µM
NAM
32 µM
-
NA
NMN
NAD
NR
-
0.98 mM
-
2.1±0.2 µM
0.22±0.07
µM
1nM
< 1nM
7.0±2.3 nM
Turnover fluxes
Fcirc
2.8±0.4 nmol/g/min
0.55±0.04 nmol/g/min
2.0±0.9 pmol/g/min
-
Appendix Table A2. NAD fluxes and protein PARrylation across five human breast cancer cell
lines. Data for lysate PARylation (detected as described27) are mean ± s.d., n = 6. Data for NAD
concentration are mean ± s.d., n = 3. Data for labeling t1/2 and PARP-mediated consumption are
mean ± 95% confidence interval (L.B. lower boundary, U.B. upper boundary).
Lysate PARylation (µg PAR
per mg protein)
NAD pool (nmol per million
cells)
NAD labeling t1/2 (h)
NAD consumption by Best
PARP (pmol per
L.B.
million cells per h)
U.B.
KPL1
MCF7
AU565
T47D
SKBR3
61±10
39±8
2.9±0.7
2.1±0.6
1.4±0.5
2.1±0.3
4.0±0.2
4.3±0.2
1.9±0.2
2.6±0.4
12.2±0.7
13.5±0.4
9.7±0.5
8.6±0.3
9.9±0.5
17
53
56
38
48
14
46
44
28
38
25
55
60
43
55
149
Appendix Table A3. Half-time for NAD labeling by 2H-NAM and for NAD depletion upon
adding FK866 (100 nM) in different cell lines. Data are mean ± 95% confidence interval.
Breast Cancer
hour
NAD
labeling
halflife
Time to
deplete
half NAD
GI Cancer
Melanoma
Differentiation
MDAMB231
MDAMB468
MCF7
T47D
HCT1
16
HepG
2
Panc1
8988T
SKMEL2
SKMEL28
C2C1
2
3T3L1
7.1
±1.2
5.6
±0.4
13.2
±0.3
8.5
±0.6
6.6
±0.6
8.1
±0.3
12.3
±2.5
10.2
±0.4
12.9
±0.5
7.3
±0.8
8.3
±1.2
5.1
±0.3
7.3
±0.3
4.9
±0.3
13.2
±0.9
6.4
±0.2
7.1
±0.9
7.3
±0.7
11.9
±1.0
7.4
±0.6
11.2
±1.0
7.9
±1.4
8.3
±0.8
5.9
±0.6
Appendix Table A4. Concentrations of NAM, NAD(H), and NADP(H) in murine tissues. Data
are mean ± s.d., n = 4.
Small
White
µM
Brain
Heart
Kideny
Liver
Pancrea
Skeletal
s
Muscle
Lung
Adipose
Intestin
Spleen
e
NAM
8±3
46±13
60±22
58±12
44±18
51±24
40±17
47±13
90±13
64±10
NAD(H)
35±9
258±53
459±47
518±42
690±48
146±21
467±59
219±53
241±43
255±35
NADP(H)
2.5±0.2
55±21
32±5
90±33
97±20
63±31
24±8
101±40
53±26
49±19
150
Appendix Table A5. Metabolic flux distributions (normalized to weight) with confidence
intervals and SSR in tissues. Fluxes are normalized to weight. Each flux is shown with 95%
confidence intervals of NAD labeling half-lives (L.B. lower boundary, U.B. upper boundary).
Tissue
White
Adipose
Brain
Heart
Kidney
Lung
Skeletal
Muscle
Pancreas
Small
Intestine
Spleen
Liver
Best
L.B.
U.B.
Flux
L.B.
U.B.
Flux
L.B.
U.B.
Flux
L.B.
U.B.
Flux
L.B.
U.B.
Flux
L.B.
U.B.
Flux
L.B.
U.B.
Flux
L.B.
U.B.
Flux
L.B.
U.B.
Flux
L.B.
U.B.
f1
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.1
6.3
6.1
6.6
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
0.0
55.0
54.2
55.7
Flux (µM / h)
f2
f3
0.1
2.3
0.1
2.3
0.1
2.2
0.1
17.1
0.1
17.0
0.1
17.0
1.0
21.0
1.0
20.7
1.1
20.7
5.4
55.7
5.2
55.9
5.5
54.8
0.8
37.4
0.7
39.2
0.8
35.7
0.0
9.4
0.0
8.4
0.0
10.1
3.5
52.1
3.3
49.4
3.7
54.1
1.2
73.6
1.1
76.1
1.2
71.0
1.1
69.4
1.0
71.7
1.1
67.0
0.9
54.0
0.8
54.5
1.0
52.1
151
f4
10.7
8.1
14.9
46.0
37.4
57.4
120.5
90.5
169.5
124.0
105.0
148.0
41.9
36.9
47.7
10.4
6.5
14.7
38.1
32.5
44.3
581.6
435.6
859.6
409.2
325.2
547.2
176.4
140.4
228.4
Halflife (h)
2.3
3.0
1.6
3.9
4.8
3.1
2.6
3.5
1.9
2.6
3.1
2.2
2.4
2.7
2.1
14.6
23.2
10.3
7.8
9.1
6.8
0.3
0.4
0.2
0.4
0.5
0.3
2.1
2.4
1.7
SSR
38.2
20.6
21.6
23.4
153.0
19.8
66.2
99.3
53.5
16.1
Appendix B. Additional Information for Chapter 3
Appendix Figure B1. NMR spectra confirmation of NAR synthesis product. Red NMR trace
represents unlabeled β–NAR. Blue NMR trace represents double-labelled NAR (~15% ɑ-NAR
based on integration), with deuterium labeled on sugar and C13 on the nicotinic acid (structure
shown at the bottom).
152
Appendix Figure B2. Confirmation of CRISPR knockout efficiency using RT-PCR. Total RNA
was extracted from differentiated cells in duplicate using Trizol according to manufacturer
instructions (Invitrogen). Subsequently, cDNA was synthesized with the High capacity cDNA
reverse transcription kit (ABI). RT-PCR were performed using Power SYBR Green PCR master
mix (ABI) on the Quantstudio 7 Flex RT-PCR system (ABI). For all assays, the plots show gene
expression values relative LC ROSA26 (plasmid control”, the reference sample, and are
normalized to the gene 36B4. For each NMNAT isoform, two distinct gRNA were generated (a
and b) near the 5’ end which are separated by a short sequence (~40bp). The primer sequences for
each are listed in Appendix Table B2 (5’ to 3’):
153
Appendix Table B1. gRNA sequences cloned into LentiCRISPR v2 vector backbone.
name
Sequence- FOR 5’--> 3’
REV 5’--> 3’
LC-R26
CACCGAAGATGGGCGGGA
AAACAGAAGACTCCCGCCCA
GTCTTCT
TCTTC
NMNAT 1 LC – 1a
CACCGTTCTTGTACGCATC
AAACGTCGGTGATGCGTACA
– gRNA 1
ACCGAC
AGAAC
NMNAT 1 LC – 1b
CACCGGTTCTGCCATGATG
AAACCCGAATCATCATGGCA
– gRNA 2
ATTCGG
GAACC
NMNAT 2 LC – 2a
CACCGGCAGGCCAGCAGG
AAACACGTTATCCTGCTGGC
– gRNA 1
ATAACGT
CTGCC
NMNAT 2 LC – 2b
CACCGTCCAGAATTCCGAC AAACGATCCAGTCGGAATTC
– gRNA 2
TGGATC
NMNAT 3 LC – 3a
CACCGCGCAGGTGCATATT AAACATCACGAATATGCACC
– gRNA 1
CGTGAT
TGCGC
NMNAT 3 LC – 3b
CACCGGCCATGGCCACTC
AAACATCACCGAGTGGCCAT
– gRNA 2
GGTGAT
GGCC
CRISPR
target
CRISPR
Ctrl
(ROSA26)
TGGAC
154
Appendix C. Additional Information for Chapter 4
Appendix Figure C1. Quantification of carbon flux into fatty acids in normoxia. (a)
Concentration of intracellular saponified palmitate on different days post differentiation. (b)
Labeling of saponified palmitate in 3T3-L1 cells after feeding either [U-13C]glucose or [U13
C]glutamine for differentiation days 0 to 5. (c) 13C-incorporation into different fatty acids after
feeding either [U-13C]glucose or [U-13C]glutamine for differentiation days 0 to 5. (d) 13Cincorporation into different fatty acids in proliferating 3T3-L1 cells after feeding simultaneously
both [U-13C]glucose and [U-13C]glutamine for 2 days. Data are mean ± s.d., n=3.
155
Appendix Figure C2. Tracing oxPPP and MTHFD flux. (a) Schematic of metabolism of the
oxPPP tracer [1,2-13C]glucose. Production of M+1 trioses is indicative of oxPPP flux in excess
of demand for ribose-5-phosphate for nucleotide synthesis. (b) M+1 and M+2 percentages of 3phosphoglycerate and pyruvate in differentiating 3T3-L1 cells (day 5) fed [1,2-13C]glucose for
12 h. (c) Comparison of ratio of oxPPP flux determined by 14CO2 release from [1-14C]glucose
and [6-14C]glucose (see main text Figure 4.2) to that determined by M+1/M+2 triose labeling
from [1,2-13C]glucose. (d) Glucose-6-phosphate 2H-labeling in cells fed [1-2H]glucose for 2 h.
156
(e) Schematic of metabolism of [2,3,3-2H]serine into methylene-THF via the cytosol (SHMT1)
or mitochondria (SHMT2, MTHFD2, MTHFD1L, and then eventually re-incorporation in the
cytosol via THFD1). (f) dTTP labeling in proliferating 3T3-L1 cells fed [2,3,3-2H]serine for 12
h. M+2 thymidine reflects cytosolic flux; M+1 reflects mitochondrial flux. (g) Direct
measurement of NADPH labeling from [2,3,3-2H]serine, indicative of folate-dependent NADPH
production. The fraction M+1 NADP(H) was measured in differentiating cells fed [2,3,32
H]serine for 12 h. Data are mean ± s.d., n=3 (**, p<0.01 by T-test).
157
Appendix Figure C3. [U-13C]glucose and [U-13C]glutamine labeling of TCA cycle-related
compounds. Differentiating normoxic 3T3-L1 cells (day 5) were fed [U-13C]glucose or [UC]glutamine for 24 h. 3PG, 3-phosphoglycerate; Pyr, pyruvate; Lac, lactate; Mal, malate; αKG,
13
α-ketoglutarate; Cit, citrate. Data are mean ± s.d., n=3.
158
Appendix Figure C4. Measured and model-fitted metabolite isotope labeling fractions from the
metabolic flux analysis. (a) For normoxic differentiating 3T3-L1 cells (day 5) fed [U13
C]glucose for 24 h. (b) As per (a) except with [U-13C]glutamine. Data are mean ± s.d., n=3.
159
Appendix Figure C5. [2,2,3,3-2H]dimethyl succinate but not [2,3,3,4,4-2H]glutamine is an
effective malic enzyme tracer. (a) Malate labeling in 3T3-L1 adipocytes (day 5) fed [2,3,3,4,42
H]glutamine or [2,2,3,3-2H]dimethyl succinate for 24 h. (b) NADP(H) labeling in 3T3-L1
adipocytes (day 0 or day 5) fed [2,2,3,3-2H]dimethyl succinate or unlabeled medium for 24 h.
Data are mean ± s.d., n=3 (**, p<0.01 by T-test).
160
Appendix Figure C6. Effect of dimethylsuccinate on metabolism of normoxic differentiating
3T3-L1 adipocytes (day 5). (a) Heat map of metabolite concentration changes in response to 2
mM 2H-dimethyl succinate (DMS) after 24 h treatment. Each column represents one sample.
Data were normalized to cell number. All individual samples were then normalized to the
average of the control (no DMS) samples. (b, c) Metabolite labeling from [U-13C]glutamine and
[U-13C]glucose with or without addition of 2 mM unlabeled dimethylsuccinate.
Dimethylsuccinate’s uptake rate (0.32 μmol per day per million cells) is ~25% of the glutamine
uptake rate and ~ 5% of the glucose uptake rate. Data are mean ± s.d., n=3.
161
Appendix Figure C7. Fatty acid labeling in 3T3L1 adipocytes fed [2,2,3,3-2H]dimethyl
succinate. (a) NADPH-mediated 2H-labeling of different abundant fatty acids. The raw fatty acid
mass spectra were corrected for natural 13C abundance. They were then further corrected for the
fractional de novo synthesis of each fatty acid and the extent of fatty acid 2H-labeling coming
from 2H-acetyl groups (as opposed to from NADP2H). (b) The number of NADPH molecules
required for making each fatty acid molecule44. (c) Cytosolic NADP2H percentages calculated
from each fatty acid’s labeling pattern. (d) Fatty acid labeling without correcting for the extent of
de novo synthesis and acetyl group labeling. Data are mean ± s.d., n=3.
162
Appendix Figure C8. Determining fractional 2H-labeling of cytosolic malate’s C2 hydride. (a)
Differential fate of 2H at malate position 2 versus 3, and potential for exchange between the two
positions due to symmetry of fumarate. MDH, malate dehydrogenase; GOT, glutamateoxaloacetate transaminase; Suc, succinate; Mal, malate; Asp, aspartate. (b) Extent of 2H-labeling
of malate and aspartate in differentiating 3T3-L1 adipocytes fed [2,2,3,3-2H]dimethyl succinate
(labeling duration 24 h). (c) Extent of 2H-labeling of malate and aspartate in differentiating 3T3L1 adipocytes fed [4-2H]glucose (labeling duration 24 h).
163
Appendix Figure C9. Genetic manipulation of ME1 with siRNA. (a) Confirmation by western
blot that ME1 is induced during 3T3-differentiation. (b) Timeline of knockdown experiments
shown in main text Figure 4.5i, j and k. (c) Timeline for alternative knockdown approach of
electroporation used in panels d, e of this figure. (d) Western blot analysis of ME1 in 3T3-L1
adipocytes electroporated as per panel c. (e) Knockdown of ME1 decreases carbon flux from
malate to pyruvate. Normoxic differentiating 3T3-L1 adipocytes (day 5) were fed [U13
C]glutamine for 24 h. (f) Schematic of pyruvate-citrate cycle driven by ME1 to promote fatty
acid synthesis. Data are mean ± s.d., n=3 (**, p<0.01 by T-test).
164
Appendix Figure C10. Adipocyte differentiation proceeds in hypoxia, with increased acetylCoA production from glutamine. (a) Fold-increase in the concentrations of common fatty acids
in 3T3-L1 cells differentiating for 5 days in either ambient O2 or 1% O2. Data are normalized to
proliferating 3T3-L1 cells (ambient oxygen). (b) 13C-incorporation into different fatty acids after
feeding simultaneously both [U-13C]glucose and [U-13C]glutamine for 2 days. In the
differentiating condition, tracers were added starting on day 3. (c) Cell number in 3T3-L1 cells
differentiating in either ambient oxygen or 1% O2. (d) Gene expression of differentiating 3T3-L1
cells in either ambient oxygen or 1% O2. Data are normalized to pre-adipocytes (ambient
oxygen). (e) Western blot analysis of G6PDH, ME1 and PPAR-γ from pre-adipocytes (ambient
165
O2), normoxic differentiating, hypoxic differentiating, or switch into hypoxia midway (cultured
in ambient O2 until day 3 before switching into 1% O2 for 2 days) 3T3-L1 cells (for timeline, see
Appendix Figure C11a). (f) Labeling of palmitate in 3T3-L1 adipocytes fed [U-13C]glutamine in
the conditions as per (a). (g) Relative glucose uptake rate and lactate excretion rate. Data are
normalized to normoxic differentiating 3T3-L1 cells. Data are mean ± s.d., n=4 for panel a; n=3
for panel b-c, f-g; n=5 for panel d.
Appendix Figure C11. [3-2H]glucose as a complementary oxPPP hydride tracer. Data are from
normoxic differentiating (day 5) or hypoxic differentiating (1% O2, day 5) 3T3-L1 cells. (a)
Schematic of [1-2H]glucose and [3-2H]glucose metabolism. (b) Oxidative pentose phosphate
pathway schematic. G6PDH, glucose-6-phosphate dehydrogenase; 6PGD, 6-phosphogluconate
dehydrogenase. (c) Production of M+1 labeled glucose-6-phosphate, 3-phosphoglycerate,
pyruvate, and citrate from [1-2H]glucose or [3-2H]glucose (2 h labeling duration). (d) Labeling
166
of palmitate in 3T3-L1 adipocytes fed [1-2H]glucose or [3-2H]glucose for differentiation days 3
to 5. (e) Fractional NADPH contribution of oxPPP. (f) Labeling of malate and aspartate in 3T3L1 adipocytes fed [4-2H]glucose for 12 h (for fatty acid labeling, see Figure 4.6b). Data are mean
± s.d., n=3.
Appendix Figure C12. Tracing oxPPP and ME flux in adipocytes switched into hypoxia
midway through differentiation. (a) Timeline of 2H-tracing experiments in normoxic
differentiating (day 5), hypoxic differentiating (day 5), or switch into hypoxia midway (cultured
in ambient O2 until day 3 before switching into 1% O2 for 2 days) 3T3-L1 cells. (b) Labeling of
167
palmitate in 3T3-L1 adipocytes fed [1-2H]glucose for differentiation days 3 to 5. (c) Fractional
NADPH contribution of oxPPP. (d) Labeling of palmitate in 3T3-L1 adipocytes fed [42
H]glucose for differentiation days 3 to 5. (e) Fractional NADPH contribution of ME1. Data are
mean ± s.d., n=3.
Appendix Figure C13. Gel images of western blot analysis. (a) Gel images of knockdown
experiments shown in main text Figure 4.5i. (b) Gel images of western blot analysis in 3T3-L1
adipocytes shown in Appendix Figure C8a. (c) Gel images of western blot analysis in 3T3-L1
adipocytes shown in Appendix Figure C8d. (d) Gel images of western blot analysis 3T3-L1 cells
shown in Appendix Figure C9e.
168
Appendix Table C1. Metabolic flux distributions with confidence intervals in normoxic
differentiating (day 5) 3T3-L1 cells.
Fluxes are normalized to glucose uptake rate. Each flux is shown with 95% confidence intervals
(L.B. lower boundary, U.B. upper boundary). Measured uptake and excretion rates are shown as
average ± 2*s.d..
169
Appendix Table C2. Metabolic flux analysis scores for different network topologies with and
without ME1 flux constrained based on 2H-labeling data.
Scores = average variance-weighted squared residual between optimal solutions and measured
labeling fractions and uptake and excretion rates. Fluxes are in absolute units normalized to cell
number.
Lower scores indicate a closer match between the measured data and the model output.
“Forward” indicates that only the forward reaction was included in the network. “Reversible”
indicates that both forward and backward flux were allowed through the reaction. “Constrained”
indicates that the ME1 flux was constrained based on the 2Hlabeling data. “-“ indicates that the
reaction was omitted from the network. ME1 fluxes are in absolute units normalized to cell
number.
170