BMB-303 HUMAN NUTRITION YEARUL KABIR SIR.
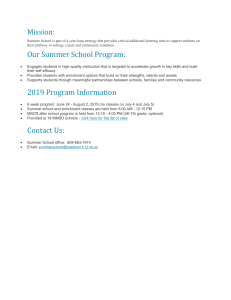
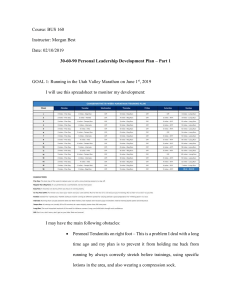
advertisement

Overview of Nutrition BMB 303 – HUMAN NUTRITION Yearul Kabir (Handout # 1) 1/29/2019 1 Human Nutrition • The action, interaction, and balance of the nutrients and other substances in food in relation to health and disease, and the process by which the body ingests, digests, absorbs, transports, utilizes, and excretes food substances. • The processes by which the body as a whole obtains and uses necessary substances from foods (nutrients) to maintain structural and functional integrity. It is rare for a food to contain just one nutrient. Meat is not just protein, bread solely carbohydrate. Foods contain mixtures of nutrients, although in most cases protein, fat or carbohydrate dominates. 1/29/2019 F.R.SIDDIQUEE 2 2 Nutrients • Chemical substances obtained from food and used in the body to promote growth, maintain, and repair tissues. • Macronutrients: carbohydrates, lipids (fat), proteins relatively large molecules. • Micronutrients: vitamins, minerals - small molecules. • People eat food, not nutrients; however, it is the combination and amounts of nutrients in consumed foods that determine health. • In studying nutrition, we focus on the function of nutrients in the body so that we can see why they are important in the diet. 1/29/2019 F.R.SIDDIQUEE 3 3 Nutrients …. • A nutrient is a chemical whose absence from the diet for a long enough time results in a specific change in health; we say that a person has a deficiency of the nutrient e.g., lack of vitamin C lead to scurvy; iron deficiency causes anemia. • Nonnutrients • Nutrients are not only chemicals in food. Other substances add flavor and color, some contribute to texture and others, like caffeine, have physiological effects on the body. • Fiber have important health benefits but do not fit the classical defination of a nutrient. • Also phytochemicals are not nutrients, they have important health functions, such as antioxidant activity, which may reduce risk of heart disease and cancer. • May be beneficial, neutral or harmful to the body. 1/29/2019 F.R.SIDDIQUEE 4 Introducing the Nutrients • Six Classes of Nutrients • Carbohydrates, lipids, proteins, vitamins, minerals & water. • Composition of the Body • The human body is made of compounds similar to those found in foods – mostly water (60%) and some fat (13-21% men, 23-31% women), with carbohydrate, protein, vitamins, minerals, and other minor constituents. • Nutrients serve 3 general functions • Provide energy • Regulate body processes • Contribute to body structures • In other words, nutrients are substances that the body uses for growth, maintenance and repair of its tissues. • Such as entire lining of digestive tract is renewed every 3 days; RBC replaced by new cells every120 days, skin cells by every 7 years. 1/29/2019 F.R.SIDDIQUEE 5 1/29/2019 F.R.SIDDIQUEE 6 6 Introducing the Nutrients…. • Macronutrients and Micronutrients • Macronutrients: Relatively large molecules. & body needs large quantities. • Micronutrients: small molecules & body needs comparatively small quantities. • Organic and Inorganic Nutrients • Nutrients that contains carbon are organic nutrients such as carbohydrates, lipids, proteins and vitamins. Minerals and water are inorganic nutrients. • Energy-yielding Nutrients • Nutrients which gives energy in the body such as carbohydrates, lipids and proteins. Alcohols also provide energy, but it is not a nutrient. 1/29/2019 F.R.SIDDIQUEE 7 Introducing Nutrients • Minerals - the simplest of the nutrients, each a chemical element, all atoms are alike; identity never changes e.g., iron in cooked food; in eaten food; as part of red blood cell; broken down cell, iron lost in the body excretion. • Water - consists of two elements - hydrogen and oxygen. Water and minerals are inorganic nutrients because they contain no carbon. • Carbohydrates - carbon, hydrogen, and oxygen. • Lipids - carbon, hydrogen, oxygen. • Proteins - carbon, hydrogen, oxygen, and nitrogen (sulphur). • Vitamins - carbon, hydrogen, oxygen (nitrogen, minerals). • Carbohydrates, lipids, proteins, and vitamins are called organic compounds because they contain carbon. 1/29/2019 F.R.SIDDIQUEE 8 8 Introducing the Nutrients…. • Vitamins • Organic compounds, do not provide energy but facilitate the release of energy from the energy nutrients. • 13 different vitamins, each with a different function, e.g., vision, sex hormones, bleeding, skin repair, replacement of red blood cells, lining of the digestive tract. • Vulnerable to destruction by heat, light, and chemicals. • Minerals • Found in body structures such as bones and teeth. Also in body fluids. 16 essential minerals in human nutrition. • Can be bound by substances and become unavailable for absorption by the body. • Cannot be destroyed during cooking (because they are inorganic). Can be lost through food refining or leaching through water used for cooking, but not cooking. 1/29/2019 F.R.SIDDIQUEE 9 9 Introducing the Nutrients…. • • • • • Water Most abundant nutrient Provide environment for all body’s activities Participates in many metabolic reactions A medium for transport of vital materials to cell and waste products away from cells. 1/29/2019 F.R.SIDDIQUEE 10 10 Introducing the Nutrients…. • Essential Nutrients • Nutrients that the body cannot make at all, or in sufficient quantities. These nutrients must therefore be supplied from foods (needed from outside). • Meaning that if you do not ingest them, you will develop deficiencies; the body cannot make these nutrients for itself. • The body can make some nutrients, but it cannot make all of them, and it makes some in insufficient quantities to meets its need. It must obtain these nutrients from foods. • Essential nutrients are found in all six classes of nutrients. Water, a form of carbohydrate, some lipids, some parts of proteins, all vitamins and minerals. 1/29/2019 F.R.SIDDIQUEE 11 Nutrients and Energy • One of the main reasons we eat food, and the nutrients it contains, is for energy. Every cellular reaction, every muscle movement, every nerve impulse requires energy. • When we speak of the energy in foods, we are talking about the potential energy that food contain. Energy is not a food component. • Energy is available from foods because foods contain carbohydrates, fats and proteins. These nutrients can be broken down completely (metabolized) to yield energy in a form that cells can use. • Practically all foods contain mixture of all 3 energy-yielding nutrients, as well as water, vitamins, minerals and other substances. • Although they are sometimes classed by the predominant nutrient. It is inaccurate to describe a food as its predominant nutrient : meat as protein or bread as carbohydrate. 1/29/2019 F.R.SIDDIQUEE 12 Energy from Foods • Carbohydrates • Protein • Fat 4 kcal/g 4 kcal/g 9 kcal/g • Fat, therefore, has a greater energy density than either carbohydrate or protein. • Alcohol is not a nutrient because it interferes with the growth, maintenance, and repair of the body even though it provides 7 kcal/g energy in the body. • The chemical bonds between the atoms of the energy–yielding nutrients break down and release energy which is then used to do various activities in the body. • If the body does not use the released energy, it rearranges the energy into new compounds for storage (e.g., fat). 1/29/2019 F.R.SIDDIQUEE 13 13 Measurement of Energy The energy released from the energy nutrients is measured in calories : units by which energy is measured. Calorie, tiny units of energy so small that a single apple provides tens of thousands of them. • Food energy is measured in kilocalories (1000 calories equal 1 kilocalorie), abbreviated kcalories or kcal. A capitalized version is also sometimes used: Calories. • Definition : One kcal is the amount of heat necessary to raise the temperature of 1 kg of water 1oC. 1/29/2019 F.R.SIDDIQUEE 14 14 Balanced Diet • A balanced diet may be defined as one which contains the various groups of food stuffs such as energy yielding foods, body building foods and protective foods, in the correct proportions so that an individual is assured of obtaining the minimum requirements of all the nutrients. • The components of a balanced diet will differ according to age, sex, physical activity, economic status and the physiological state. • A balanced diet gives daily nutrients in the proper amounts and proportion required by the body. • Your diet is balanced if the amount of energy you take in through what you eat equals the amount of energy you expend in daily activities and exercise. 1/29/2019 F.R.SIDDIQUEE 15 Role of Carbohydrates in Human Nutrition BMB 408 – HUMAN NUTRITION Yearul Kabir (Handout # 2) 1/29/2019 F.R.SIDDIQUEE 16 Major Dietary Carbohydrates • Carbohydrates are polyhydroxy aldehydes, ketones, alcohols, acids, their simple derivatives and their polymers having linkages of the acetal type. • They may be classified according to their degree of polymerization and may be divided initially into three principal groups, namely sugars, oligosaccharides and polysaccharides. • Class (DP*) • Sugars (1-2) Sub-Group Components Monosaccharides Glucose, galactose, fructose • Disaccharides Sucrose, lactose • Polyols Sorbitol, mannitol • Oligosaccharides (3-9) Malto-oligosaccharides Maltodextrins Other Oligosaccharides • • Polysaccharides (>9) Raffinose, Stachyose Starch Amylose, amylopectin Non-Starch polysaccharides Cellulose, hemicellulose, • 1/29/2019 F.R.SIDDIQUEE pectins 17 Different forms of carbohydrates in food • The term carbohydrate covers a large number of diferent compounds, all composed of carbon, hydrogen, and oxygen atoms. • Classification of Carbohydrates: • Simple Carbohydrates: Monosaccharides and Disaccharides • Monosaccharides: Hexose (glucose, fructose, and galactose) • Disaccharides: Sucrose, Lactose, Maltose, Mannose • Complex Carbohydrates: Polysaccharides • Starch • Glycogen • Dextrin • Cellulose Polysaccharides are further designated as digestible (starches) or indigestible (fibers). 1/29/2019 F.R.SIDDIQUEE 18 Carbohydrate as a Dietary Essential • You need some carbohydrate daily as a source of glucose. How much carbohydrate is enough? • Requirements for Carbohydrate • The amount of carbohydrate required to avoid ketosis is very small (about 50 g/day). • Intakes of less than 50 g of carbohydrate/day are associated with adverse health effects. These symptoms are similar to those that develop in starvation. • In addition to providing easily available energy for oxidative metabolism, carbohydrate-containing foods are vehicles for important micronutrients and phytochemicals. • There is an unexplained loss of large amounts of both sodium and water, which explains the rapid loss of body weight found in people eating a carbohydratefree diet. The loss of sodium is followed by a loss of potassium, which usually leads to weakness. • At the same time, protein of the body (muscles) begins to break down, which leads to muscle wastage, further weakness, and further weight loss. 1/29/2019 F.R.SIDDIQUEE 19 Carbohydrate as a Dietary Essential….. • Even more seriously, when carbohydrate is absent, the use of fat to provide energy becomes hindered in the final series of chemical steps normally involved in oxidizing the fat. • This leads to the accumulation of chemical intermediates of fat oxidation, known as ketones. • This state, known as ketosis, is associated with mild disturbances of cellular function and is an early indication of insufficient carbohydrate availability in the body. • As the ketones build up, they begin to be found as abnormal components of blood and urine. Also, because they change the hydrogen ion balance (or acid-base balance) of tissues, the ketones begin to interfere with the normal functioning of various body processes. 1/29/2019 F.R.SIDDIQUEE 20 Carbohydrate as a Dietary Essential….. • People reaching this stage are said to be suffering from ketosis, which usually produces symptoms of fatigue and dehydration and a loss of stamina. • All these undesirable effects of a carbohydrate-free diet are soon corrected by the return of carbohydrate to the diet – a clear indication that carbohydrate really is a dietary essential. • Carbohydrates are also used in the synthesis of various metabolically active complexes. Glycoproteins are important components of cellular membranes. Glycolipids, such as sphingolipids and gangliosides, have roles at receptor sites on cells and in synaptic transmission. • Mucopolysaccharides have important water-holding or binding properties in many sites of the body; they occur in basement membranes and in intercellular cement and form an integral part of cartilage, tendon, skin and synovial fluid. 1/29/2019 F.R.SIDDIQUEE 21 Recommended Carbohydrates Intake • Intake of available carbohydrate (starch and sugar) that might be ideal to support long-term health: 55 to 60 percent of total Kcal. Further, added sugar be used in moderation (< 10% of Kcal), more should come from complex carbohydrates and naturally occurring sugars in foods. • A person consuming 2000 kcal diet a day should therefore have 1100 to 1200 kcal energy from carbohydrate, or about 275 to 300 grams. • Most of this would be starch, with its accompanying fiber, some would be the naturally occurring sugars of fruits, vegetables, and milk. • Estimates of the minimum amount of carbohydrate needed by an adult are in the range of 150-180 g carbohydrate per day. 1/29/2019 F.R.SIDDIQUEE 22 Trends in Carbohydrates Use • Because most diets contain at least 200 g of carbohydrate/day, a lack of carbohydrate is unlikely to reach the level where it causes serious problems. • Also, because carbohydrate-rich foods are the cheapest source of energy they tend to be used in amounts that ensure al least a minimum intake, especially among those with low incomes. • There is a big difference, however, between eating at least the minimal amount of carbohydrate and eating the optimal amount. • Fiber is not counted in computing energy from carbohydrate; we do not know enough yet about its energy contributions, but they are probably not large in comparison with those from starch and sugar. 1/29/2019 F.R.SIDDIQUEE 23 Fiber • Fiber is an indigestible carbohydrate. It is taken in as part of many foods, but most of it simply passes through the digestive tract because we do not possess the enzymes needed to break it down into a form that can be absorbed into the blood. • However, some bacteria in the large intestine can degrade some components of fiber, releasing products that can be absorbed into the body and used as an energy source. • Two categories of fiber are found in food: • crude fiber and • dietary fiber. • The major component of crude fiber is the polysaccharide called cellulose. 1/29/2019 F.R.SIDDIQUEE 24 Fiber… • Several other carbohydrates and related compounds called pectins, hemicelluloses, and lignins are found in plant foods and are also resistant to digestion in the human digestive tract. These, together with cellulose, are known collectively as dietary fiber. • This is a general term that describes any material in food that remains undigested in the intestine. The cellulose that is called crude fiber is just a part of dietary fiber as whole. • Dietary fiber can also be classified into soluble and insoluble fiber, depending on how it reacts with water. • Fiber Intake: With all the uncertainties, it is probably true to say that about 20 – 30 g of dietary fiber daily is a desirable intake. 1/29/2019 F.R.SIDDIQUEE 25 Soluble Fiber • Soluble fiber is found in fruits, some legumes, and such grains as oats, rye, and barely. It dissolves in water to form a gel. This gel forms within the digestive tract and serves to slow the rate at which food passes through the small intestine. This in turn increases the rate of absorption of nutrients from the food. • Which is why home remedies for diarrhea often included eating fruits rich in the soluble fiber pectin, such as apples and pears. • Pharmaceutical manufacturers also add pectin to antidiarrhea medications. • Anyone who has made marmalade, jam, or jelly has probably used the soluble fiber pectin as a thickening agent. 1/29/2019 F.R.SIDDIQUEE 26 Insoluble Fiber • Insoluble fiber: composed of cellulose, hemicellulose, and lignins – is found in vegetables and wheat bran. It tends to absorb water and increase in bulk, greatly contributing to the volume of stools or feces. The associated water softens the stools. • This causes insoluble fiber to increase gastrointestinal motility, or in other words speed the movement of material through in GI tract, especially the colon. Bacteria will not digest insoluble fiber. • In other words, insoluble fiber (like cellulose) is valued for its ability to prevent or relieve constipation. 1/29/2019 F.R.SIDDIQUEE 27 Health Benefit of Fiber • Soluble fiber is known to have cholesterol lowering effects because of its promotion of increased fecal excretion of bile acids, slower cholesterol and lipid absorption, and increased production of shortchain fatty acids by fermentation in the large intestine. • Insoluble fiber softens the stool and increases bulk, and thus effectively prevents constipation, which appears to play a role in the development of colon cancer and diverticulitis. • Theoretically, the longer potentially carcinogenic substances contained in feces remain in the colon, the more opportunity they have to damage the intestinal lining. 1/29/2019 F.R.SIDDIQUEE 28 Health Benefit of Fiber…. • How do dietary fibers help to reduce the incidence of colon cancer and diverticulosis? • The link between a lack of dietary fiber and the onset of colon cancer has been attributed to various effects of fiber – namely: • • • • • Changes in the populations of microorganisms in the GI tract The decreased binding of intestinal bile acids The increased time for which food residue remains in the colon Decreased stool weight and volume and Decreased frequency of defecation • Scientists postulate that the microorganisms encouraged by a diet low in dietary fiber enhance the formation of cancer-causing substances (carcinogens). These microorganisms may also prevent or at least limit the breakdown of carcinogens that are normally destroyed by the microorganisms that thrive when there is more dietary fiber in the diet. 1/29/2019 F.R.SIDDIQUEE 29 Health Benefit of Fiber…. • The main alternative theory suggests that the beneficial effect of dietary fiber results from its speeding of the passage of feces through the large intestine. • The logic behind this idea is that faster passage means less time for any carcinogens present to be in contact with the intestinal wall. Also, the bulk and water of the feces may dilute the carcinogens to a nontoxic level. • Some fibers bind bile and carry it out of the body; this is also thought to reduce cancer risk. • Diverticulosis is a condition in which the muscles of the colon weaken, forming small pouches that can become painfully inflamed (diverticulitis) if food residue gets trapped within them. It often occurs in people who are chronically constipated. 1/29/2019 F.R.SIDDIQUEE 30 Health Benefit of Fiber…. • Diverticulosis is associated with a weakening of the intestinal wall caused by the pressure from hard stools. The weakened intestinal wall then develops small outpouchings in which fecal material becomes trapped. Diverticulitis is an inflammation of the intestinal wall that develops when these outpouchings become irritated or infected. • Different Fibers, Different Effects • Not all the fibers have similar effects. For example, wheat bran, which is composed mostly of cellulose, has no cholesterol lowering effect, whereas oat bran and the fiber of apple (pectin) do lower blood cholesterol. • Fibers that form gels in water (pectin and guar) prolong the time of transit of materials through the intestine, whereas insoluble fibers (cellulose) tend to reduce the time. 1/29/2019 F.R.SIDDIQUEE 31 Hazards of Too Much Fiber • There is now concern that some people may be consuming too much fiber, which can lead to a condition known as irritable bowel syndrome. • It is also possible that too much fiber may cause decreased absorption of some mineral elements (magnesium, calcium, zinc, and iron), either by binding to them or by simply speeding the passage of food through the intestinal tract and reducing the opportunity for the mineral elements to be absorbed. • At present it is thought that 20 to 30 g of dietary fiber per day maximizes the benefits of fiber while minimizing the possible adverse effects of either excessive or insufficient fiber consumption. 1/29/2019 F.R.SIDDIQUEE 32 Classification of Starch according to Digestibility • Rapidly digestible starch: digested within 20 minutes • Slowly digestible starch: digested between 20 and 120 minutes • Resistant starch: not digested • Rapidly digestible starch (RDS) is readily available to digestive enzymes and digested rapidly and completely in the small intestine. Example: freshly cooked starchy food. • Slowly digestible starch (SDS) digested completely in the small intestine, but slowly. They have a specific internal structure that delays digestion and conversion into glucose. Example: mostly raw cereals. • Resistant starch is the name given to the components of dietary starch that are resistant to the normal enzymatic digestion process in the small intestine. 1/29/2019 F.R.SIDDIQUEE 33 Starch according to Digestibility….. • There are three type of resistant starch: • Physically inaccessible (RS1) • Resistant granules (RS2) • Retrograded (RS3) • They originated in three possible ways: • The physical structure of the food may prevent access to digestive enzymes if the starch is surrounded by fat. • The nature of the cell walls around the starch granules may impede digestion. • Where the starch has become retrograded by heating and cooling, the enzymes are no longer able to break the bonds. • It must be remembered, however, that digestibility is variable and probably dependent on the composition of the meal. 1/29/2019 F.R.SIDDIQUEE 34 Resistant Starch • Resistance starches that escape digestion in the small intestine become available for fermentation in the colon by the bacterial flora. • The result of this process is an increase in fecal mass owing to the multiplication of the bacteria, production of short-chain fatty aids (acetic, propionic and butyric acids) and a decrease in colonic pH. • In addition, CO2, H2 and some CH4 are produced. These contribute to a sensation of bloating and flatulence. • It has been estimated that between 20 and 30% of the potential energy contained in the resistant starch becomes available to the body in the form of short-chain fatty acids absorbed from the colon. 1/29/2019 F.R.SIDDIQUEE 35 Which class of starch is nutritionally the most desirable form and why? • SDS is the most desirable form of starch, as it digested slowly thus keep the body’s blood glucose levels relatively steady throughout the day. • The delayed release of glucose into the blood stream from foods containing SDS helps to prevent the rapid rise in blood glucose levels that can occur after a meal high in simple sugars or rapidly digested carbohydrate. • A slower rise in blood glucose level support the more efficient movement of glucose into cell and may prevent elevated blood insulin levels, which can contribute to the development of diabetes. • SDS has been recognized to provide control energy release, more prolonged glucose release and helps in the management of diabetes. 1/29/2019 F.R.SIDDIQUEE 36 Non-Starch Polysaccharides • Constituents of NSP • Cellulose • Non-cellulosic polysaccharides: Hemicelluloses, pectins, beta-glucans, gums and mucilages • In the mouth, high-fiber foods generally require more chewing. This slows down the process of eating and stimulates an increased flow of saliva. The saliva contributes to the volume of the swallowed food bolus. • Once in the stomach, the fiber-rich food tends to absorb water and the soluble component starts to become viscous. Both of these changes delay stomach emptying. In the small intestine, the soluble fiber travels slowly because of increased viscosity; this prolongs the period of time available for the absorption of nutrients. 1/29/2019 F.R.SIDDIQUEE 37 Non-starch Polysaccharides…. • The fiber may also bind some divalent ions in the small intestine, making them unavailable for absorption at this point. • Once in the large intestine, the soluble fiber becomes a food source for the growth and multiplication of the bacteria flora. The consequences of this are exactly the same as described above for resistant starch. • Thus, both resistant starch and soluble NSPs contribute to increasing bulk in the large intestine, and the production of fatty acids and gases. • Insoluble fiber, which has reached the colon largely unchanged, swells by water holding, and adds further to the volume of the colonic contents. The feces, therefore, are both bulkier and softer because of the increased water content. 1/29/2019 F.R.SIDDIQUEE 38 Carbohydrate and Microflora • Carbohydrate which is fermented stimulates the growth of bacteria in the large gut. • This is a generalized effect which leads to an increase in the total number of bacteria or biomass. • When bacterial growth occurs, the microflora synthesize protein actively from preformed amino acids and peptides as well as some de-novo synthesis using ammonia as the source of nitrogen. • The additional biomass is excreted in feces and is one of the mechanisms whereby carbohydrate influences bowel habit. 1/29/2019 F.R.SIDDIQUEE 39 Carbohydrate and Microflora …. • One of the more significant developments in recent years with regard to the gut microflora has been the demonstration that specific dietary carbohydrates selectively stimulate the growth of individual groups or species of bacteria. • An example of this is the effect of fructo-oligosaccharides on the growth of bifidobacteria. • The importance of bifidobacteria is that they may be one of the major contributors to colonization resistance in the colon, thereby protecting the host from invasion by pathogenic species. • Foods which selectively stimulate the growth of gut bacteria are known as prebiotics. 1/29/2019 F.R.SIDDIQUEE 40 Carbohydrate and Microflora …. • One of the more significant developments in recent years with regard to the gut microflora has been the demonstration that specific dietary carbohydrates selectively stimulate the growth of individual groups or species of bacteria. • An example of this is the effect of fructo-oligosaccharides on the growth of bifidobacteria. • The importance of bifidobacteria is that they may be one of the major contributors to colonization resistance in the colon, thereby protecting the host from invasion by pathogenic species. • Foods which selectively stimulate the growth of gut bacteria are known as prebiotics. 1/29/2019 F.R.SIDDIQUEE 41 What happens if I do not have enough blood glucose? • Because both too little and too much glucose are harmful, blood levels are maintained within a narrow range through the opposing action of the hormones insulin and glucagon. • When blood glucose levels are high, insulin helps the cells absorb glucose, thereby lowering the blood glucose level. • When blood glucose levels fall beneath the acceptable limit (hypoglycemia), the pancreas releases glucagon, which stimulates degradation of liver glycogen to glucose. • If the fuel crisis persists and the glycogen supply has been depleted, the body will begin to form glucose from protein and glycerol by gluconeogenesis. 1/29/2019 F.R.SIDDIQUEE 42 Hypoglycemia • If the blood glucose level falls much too low, to about 60 mg/dl, a condition called hypoglycemia (too little glucose in the blood) results. • Hypoglycemia is not a disease, but a symptom by which various diseases can be diagnosed (just as hyperglycemia is a symptom of diabetes). • In extreme cases both hypoglycemia and hyperglycemia can cause people to fall into a coma and die. • Reactive Hypoglycemia: A mild form of hypoglycemia, sometimes called reactive hypoglycemia, occurs from time to time in almost everyone. Sometimes this is simple because a person has waited too long between meals. People who get up and get going without eating breakfast are running on an empty fuel tank. Not surprisingly, they report a high incidence of reactive hypoglycemia, as a result of insufficient food. 1/29/2019 F.R.SIDDIQUEE 43 Spontaneous Hypoglycemia • In rare instances people develop a serious condition known as spontaneous or fasting hypoglycemia, characterized by chronically low blood glucose levels. This condition results from an underlying disease state, such as stimulation of excessive insulin production by a pancreatic tumor. No matter how much people with spontaneous hypoglycemia eat, their blood sugar remains too low. • If they go for a long period without food, their blood sugar may drop so low that their energy-starved brain loses consciousness. • Clearly this is a life-threatening condition that requires immediate medical treatment. 1/29/2019 F.R.SIDDIQUEE 44 What happens if I have high blood glucose? • Hyperglycemia: If the blood glucose level rises too high, above 200 mg/dl, a condition called hyperglycemia (too much glucose in the blood) results. • In people suffering from diabetes mellitus, hyperglycemia can occur. • How can diabetes be controlled through diet? • The key to treating diabetes is to keep blood glucose at a constant and moderate level using a carefully planned diet and, if necessary, medication. • A diet rich in complex carbohydrates and containing non-starch polysaccharides is recommended in the management of diabetes. 1/29/2019 F.R.SIDDIQUEE 45 How can diabetes be controlled through diet? • Using a menu planning guide known as the Diabetic Exchange Lists, dietitians help clients with diabetes develop a meal plan that specifies how much of which types of food (exchanges) can be eaten at each meal and snack. • A diet rich in complex carbohydrates but with small amounts of sugar is the key to controlling blood glucose levels. • Diabetic Exchange Lists separate individual foods into six lists: milk, vegetable, fruit, bread, meat, and fat. The milk, starch, and meat lists are further divided to identify high-, medium-, and low-fat food choices. The reason for dividing foods into these lists is that food items vary with respect to their carbohydrate, protein, fat, and kcalorie content. 1/29/2019 F.R.SIDDIQUEE 46 How can diabetes be controlled through diet? • The foods in each Exchange List have roughly the same amounts of nutrients and kcalories, which makes it easy to exchange one food for another within a given list. • For example, one slice of bread and ½ cup of cooked rice are considered to be nutritionally equivalent (contains 15 g carbohydrate, 3 g protein, trace fat and 80 kcal). • Because each Exchange List contains a wide variety of foods, people with diabetes have considerable freeway in developing their own menus. 1/29/2019 F.R.SIDDIQUEE 47 Glycemic Effect of Foods • The glycemic effect of a food is the effect that food has on a person’s blood glucose and insulin response – how fast and how high the blood glucose rises, and how quickly the body responds by bringing it back to normal. • The concept of glycemic index is a measure of the ability of a carbohydrate to contribute to the concentration of blood glucose. • High glycemic index means that the dietary carbohydrate elevates blood glucose faster and to a higher level than a carbohydrate of lower glycemic index. • A food’s ranking depends on a number of factors working together, and the effect is not always one might expect. For example, ice cream, is a high-sugar food, but it ranks lower than baked potatoes, a high-starch food. • Diets with a low glycemic index have been shown to have various health benefits, including reduction of blood lipids and improved blood glucose control in diabetic subjects. 1/29/2019 F.R.SIDDIQUEE 48 What is Glycemic Index (GI)? A scale that ranks carbohydrates by how much they raise blood glucose levels compared to a reference food. Glycemic Index (GI): Ranking Low Moderate High 0 – 55 56 – 69 70 or more The glycemic index is defined as the incremental area under the blood glucose response curve of a 50g carbohydrate portion of a test food expressed as a percent of the response to the same amount of carbohydrate from a standard food such as glucose or white bread taken by the same subject. Glycemic Index (GI): Sample Graphs Determination of Glycemic Index • Comparison of the areas under the two glucose curves obtained produces a “glycemic index”. The glycemic index for white bread is 100. Area for test meal • • Glycemic Index = ---------------------------------------- X 100 Area for glucose standard • • Incremental area under the curve • A number of different methods have been used to calculate the area under the curve. For most glycemic index data, the area under the curve has been calculated as the incremental area under the blood glucose response curve (IAUC), ignoring the area beneath the fasting concentration (below the baseline). • This can be calculated geometrically by applying the trapezoid rule. 1/29/2019 F.R.SIDDIQUEE 51 Determination of Glycemic Index …. • Sample data are shown in Table. The data for Standard #1 are used in the diagram in Figure to illustrate the details of the actual calculation. • Table: Sample blood glucose responses to the ingestion of 50g carbohydrate • Minutes 0 15 30 45 60 90 120 IAUC • Standard #1 4.3 6.3 7.9 5.3 4.1 4.6 4.9 114 • Standard #2 4.0 6.0 6.7 5.5 5.3 5.0 4.2 155 • Standard #3 4.1 5.8 8.0 6.5 5.9 4.8 3.9 179 • Test Food 4.0 5.0 5.8 5.4 4.8 4.2 4.4 1/29/2019 F.R.SIDDIQUEE 93 52 Determination of Glycemic Index …. • Sample calculations of incremental area under the curve (IAUC) • The IAUC for the data illustrated above (Standard #1, Table) equals the sum of the areas of the triangles and trapezoids: A+B+C+D+F • The area of triangle A = 2.0 × 15/2 = 15.0 The area of trapezoid B = (2.0 + 3.6) × 15/2 = 42.0 The area of trapezoid C = (3.6 + 1.0) × 15/2 = 34.5 The area of triangle D = 1.0 × 12.5/2 = 6.25 • The area of triangle E = 0.3 × 18/2 = 2.7 • The area of trapezoid F = (0.3 + 0.6) × 30/2 = 13.5 Therefore, IAUC = 15.0 + 42.0 + 34.5 + 6.25 + 2.7 +13.5 = 114 mmol.min/L. • Area of Triangle = ½ b (time) x h (conc. of glucose) • Area of Trapezoid = (sum of parallel sides) x ½ (distance between them) 1/29/2019 F.R.SIDDIQUEE 53 Glycemic Index …. • 50g carbohydrate portion • The portion of food tested should contain 50g of glycemic (available) carbohydrate. • In practice, glycemic carbohydrate is often measured as total carbohydrate minus dietary fiber, as determined by the AOAC method. • Since this method does not include RS1 and RS2 when they are present, they will be mistakenly included as glycemic carbohydrate. • Standard food • Either white bread or glucose can be used as the standard food. • The GI values obtained if white bread is used are about 1.4 times those obtained if glucose is the standard food. 1/29/2019 F.R.SIDDIQUEE 54 Glycemic Index …. • Same subject • Blood glucose responses vary considerably from day-to-day within subjects. • Thus, to obtain a representative mean response to the standard food, it is recommended that the standard food be repeated at least three times in each subject. • This is illustrated by the data in Table, which is typical for normal subjects. • The standard food was repeated three times giving IAUCs of: 114, 155 and 179. • The mean ± SD IAUC is 149 ± 33 and the coefficient of variation (100 × SD/mean) is 22%. • For this subject, the GI of the test food = 100 × 93/149 = 62. 1/29/2019 F.R.SIDDIQUEE 55 low glucose response (low GI) high glucose response (high GI) Plasma glucose response (mmol/L) from a high vs. low GI food. The change in blood glucose concentration over time is expressed and calculated as the area under the curve (AUC) Plasma glucose (mmol/l) Evaluation of the incremental rise of blood glucose (area under curve) after ingestion of a food that contains 50g of carbohydrates, as a percentage of the same amount of carbohydrate from a reference food (white bread or glucose) and absorbed by the same person 8 6 4 0 1/29/2019 0.5 1 1.5 2 F.R.SIDDIQUEE 2.5 Time (h) 57 Glycemic Index …. • Calculation of glycemic index of meals or diets • The GI can be applied in a detailed fashion to mixed meals or whole diets by calculating the weighted GI value of the meal or diet. • For example, the way to calculate the GI of a meal containing bread, cereal, sucrose, milk and orange juice is shown in Table. • Food g Glycemic Proportion of total • Carbohydrate • Bread 25 0.342 100 • Cereal 25 0.342 72 Food Glycemic Meal Glycemic Glycemic Carbohydrate Index Index * 34.2 24.6 • Milk 6 0.082 39 3.2 • Sucrose 5 0.068 87 5.9 • Orange juice 12 0.164 74 12.1 • TOTAL 73 80.0 • * Values for each food equal the proportion of total glycemic carbohydrate multiplied by the food GI. The sum of these values is the meal GI. • Using this type of calculation, there is a good correlation between meal GI and the observed glycemic responses of meals of equal nutrient composition. 1/29/2019 F.R.SIDDIQUEE 58 Glycemic Load (GL): What does it mean? Glycemic load measures the degree of glycemic response and insulin demand produced by a specific amount of a specific food. Glycemic load reflects both the quality and the quantity of dietary carbohydrates. GL = GI/100 x CHO (grams) per serving Example: GL of an apple = 40/100 x 15g = 6g Glycemic Load (GL): What does it mean? The concept of glycemic load offers an accounting of both a food’s glycemic index and its carbohydrate content. Take carrots, for example. In laboratory tests, 50 grams of carbohydrate from boiled carrots ranks in the middle of the glycemic index scale, indicating a moderate capacity for elevating blood glucose. However, the glycemic index fails to reveal that a typical half-cup serving of carrots presents the body with only 8 g of absorbable carbohydrate – to receive a test portion of 50 g requires eating more than 3 cups of boiled carrots at a sitting. Therefore, the glycemic load of a serving of carrots is low, a point often overlooked. Glycemic Load (GL): Ranking Individual food portion: Low 0-10 Moderate 11-19 High 20+ Whole day: Low Moderate High < 80 100 > 120 GI vs. GL Glycemic Index: ranks carbohydrates based on their immediate blood glucose response. GI = glycemic quality Glycemic Load: helps predict blood glucose response to specific amount of specific carbohydrate food. quality GL = glycemic quantity Effects of Low GI Foods satiety hungry voluntary food intake 1/29/2019 F.R.SIDDIQUEE 63 Benefits of Low GI Diet Are there any documented benefits to lowering the GI of one’s diet? YES! type 2 DM risk BG levels cholesterol levels heart disease risk weight Pictures of Low/High GI Meals & Snacks GI = 60 GL = 48 GI = 42 GL = 31 Pictures of Low/High GI Meals & Snacks GI = 85 GL = 48 GI = 39 GL = 22 Pictures of Low/High GI Meals & Snacks GI = 83 GL = 19 GI = 14 GL = 1 Pictures of Low/High GI Meals & Snacks GI = 80 GL = 32 GI = 61 GL = 12 Pictures of Low/High GI Meals & Snacks GI = 57 GL = 31 GI = 32 GL = 16 Glycemic Index of Common Foods and Sugars 1/29/2019 Food GI Maltose 105 Glucose 100 Rice (low amylose) eg white rice88 Cornflakes 84 Honey 73 White Bread 70 Mashed Potatoes 70 Wholemeal bread 69 Soft drink 68 Ice cream 61 Sucrose 65 Rice (high amylose) eg Basmati 59 Papaya 58 Rice vermicelli 58 Boiled potato 56 Sweet corn 55 Mango 55 Potato crisps 54 Banana 53 Chocolate 49 Green Peas 48 F.R.SIDDIQUEE47 Instant noodles 70 Blood glucose • A blood glucose level of about 90 mg/dl is referred to as the fasting glucose level because it is the level that is maintained during fasting. • Glucose is the main source of energy for the central nervous system (CNS), which used about 140 g (9 Tbsp) of glucose per day. Red blood cells need about 40 g (3 Tbsp) of glucose per day. • Carbohydrate Effect on Brain Function • Prolonged hypoglycemia in brain results in histologically demonstrable and functionally irreversible damage to brain tissue. • Recent research has indicated that the kind and amount of carbohydrate in the diet can influence brain function and behavior. 1/29/2019 F.R.SIDDIQUEE 71 Carbohydrate Effect on Brain Function…. • When carbohydrate intake is high, comprising 70% to 80% of total kcal, the brain produces more serotonin. • When produced in excess, serotonin causes a carving for carbohydrate and therefore increased consumption of carbohydrate, which in turn stimulates the production of yet more excess serotonin. • This make a person sleepy and sluggish. 1/29/2019 F.R.SIDDIQUEE 72 Some Aspects of the Role of Carbohydrate • • • • • • Protein Sparing Action of Carbohydrates The Need for Carbohydrates for the Oxidation of Fats Carbohydrates as a Source of Energy for Muscular Work Special Functions of Carbohydrates in Liver Synthesis of Ribose from Glucose Carbohydrate and Dental Health 1/29/2019 F.R.SIDDIQUEE 73 Protein Sparing Action of Carbohydrates • The body uses mainly carbohydrates as a source of energy when they are adequately supplied in the diet, thus sparing protein for tissue building, since meeting the energy needs of the body takes priority over other functions like growth. • If the diet does not supply adequate calories, the dietary protein is oxidized as a source of energy. There is also breakdown of tissue proteins to a greater extent. • This function of carbohydrates serving as a source of energy and preventing dietary protein from being oxidized and preventing excess tissue protein breakdown in calorie deficiency in called “protein sparing action of carbohydrates”. • For example, the daily urinary N excretion of 135 mg in an adult rat during fasting is reduced to 93 mg when 12 g of glucose is fed to the rat. Glucose has spared about 33% of the body protein broken down in the fasted rat. 1/29/2019 F.R.SIDDIQUEE 74 The Need for Carbohydrates for the Oxidation of Fats • In the oxidation of fats, the acetyl CoA formed from the oxidation of fatty acids reacts with oxaloacetic acid (formed from carbohydrate breakdown product – pyruvic acid or formed from the aspartic acid) to form citric acid which is oxidized through the TCA cycle back to oxaloacetic acid through a series of reactions. • If adequate amounts of oxaloacetic acid are not available, acetyl CoA is formed in large amounts from the oxidation of fatty acids and a part of it is converted into ketone bodies (acetoacetic acid and βhydroxy butyric acid) which accumulate in blood and tissues and produce ketosis. 1/29/2019 F.R.SIDDIQUEE 75 Carbohydrates as a Source of Energy for Muscular Work • Carbohydrates are the major source of energy for muscular work. During muscular contraction glycogen is broken down to lactic acid. The process is known as glycolysis. • During the recovery period lactic acid is first oxidized to pyruvic acid and then to acetyl CoA, which in turn is oxidized through TCA cycle to CO2 and H2O thus producing energy for muscular work. • As a source of energy, carbohydrates are more important during moderate or severe muscular work as in athletics. 1/29/2019 F.R.SIDDIQUEE 76 Special Functions of Carbohydrates in Liver • These include detoxifying action and a regulating influence on protein and fat metabolism. The liver of well-fed animals is rich in glycogen. Such a liver is more resistant to certain poisons such as carbon-tetrachloride, alcohol or arsenic and toxins of bacteria than the livers of under-fed animals with low glycogen reserves. • Synthesis of Ribose from Glucose • The pentose-ribose is present in RNA and many nucleotides. It is formed in the body from glucose by the pentose pathway and is incorporated in RNA and nucleotides. 1/29/2019 F.R.SIDDIQUEE 77 Carbohydrate and Dental Caries • Dietary carbohydrate is implicated as a major cause of dental caries, or tooth decay. • High intake of dietary sugars Multiplication of oral bacteria Production of acid Low oral pH Demineralization of teeth Dental Caries. • Carbohydrate as Glycoproteins • Carbohydrates are found in the form of polysaccharide chains attached to proteins such as glycoproteins. As such they are important constituents of tissue antigens (in the cell membrane) and secreted proteins. 1/29/2019 F.R.SIDDIQUEE 78 Individual Sugars • Glucose: Glucose (also known as dextrose, blood sugar, and grape sugar) found naturally in fruits, vegetables, and honey. These foods, however, provide us with an average of only 18 g of glucose per day, which is only a small fraction of the glucose used daily in the body. • The rest is provided by the breakdown of more complex carbohydrates, by the conversion of other monosaccharides, or by the metabolism of certain amino acid. • Sorbitol: a derivative of glucose that is formed when glucose is chemically “reduced” by the addition of one hydrogen atom. • Sorbitol occurs naturally in such fruits as apples, pears, and peaches and also in several vegetables. 1/29/2019 F.R.SIDDIQUEE 79 Sorbitol • It is not actively absorbed from the gastrointestinal tract and is absorbed at about one third the rate of glucose absorption. • This means that eating food rich in sorbitol allows blood glucose levels to remain above the fasting level for a longer time than does eating food correspondingly rich in glucose. Thus eating sorbitol may delay the onset of hunger. • For this reason, sorbitol is an ingredient in some foods designed for use in weight-reducing diets and has been used clinically as a noninsulin-stimulating carbohydrate. • Unfortunately, sorbitol also causes flatulence and diarrhea in some people, which considerably reduces its acceptability. • Sorbitol is also widely used as a sweetener in chewing gums because it is less likely to promote the formation of dental cavities than is sucrose. 1/29/2019 F.R.SIDDIQUEE 80 Fructose • Fructose (also known as levulose or fruit sugar) occurs in many different fruits. It also makes up one third of the sugar in honey. • Insulin is not needed to allow fructose to be transported into cells; so fructose does not cause problems of high blood sugar levels in persons with diabetes. This has led to the idea that diets high in fructose might be a suitable way for those with diabetes to get their supplies of carbohydrate. • Fructose is less likely to be cariogenic (tending to cause tooth decay) than other sugar-based sweeteners. Tooth decay, technically known as caries, is produced when bacteria in the mouth act on carbohydrate to produce acid. • The level of acid production depends on what carbohydrates are available in the mouth, with fructose resulting in a relatively low level. 1/29/2019 F.R.SIDDIQUEE 81 Galactose • Galactose, the third main monosaccharides of nutritional relevance, occurs only as a result of the breakdown during digestion of the disaccharide lactose. • Studies using laboratory animals have linked excessive galactose consumption with the development of cataracts. • The levels used, however, indicated that this was unlikely to present any problem to humans apart from the few people with a genetic defect of metabolism known as galactosemia. • Galactosemia: is an inborn error of metabolism and occurs in newborn infants. They have an inability to convert galactose to glucose due to deficiency of the enzyme galactose-1-phosphate uridyl transferase. • Galactose accumulates in blood and tissues and is excreted in urine. 1/29/2019 F.R.SIDDIQUEE 82 Galactosemia • In galactosemia, the concentration of galactose-1-phosphate uridyl transferase is very low. Carbohydrate intake must be controlled when such enzyme deficiencies occur. If milk is withheld from the infants’ diet and substituted by lactose-free food, the condition is alleviated. • If the intake of galactose is not restricted, mental retardation results. • In the absence of normal metabolism of galactose, some of it is converted to its alcohol form – galactitol – by reduction. This is mainly responsible for cataract production. 1/29/2019 F.R.SIDDIQUEE 83 Sucrose • Sucrose is the most common disaccharide. The familiar white crystals or powder of sucrose is simply known as “sugar”, which is 100% sucrose. • Brown sugar, with its more distinctive flavor, is 97% sucrose and is made by partially refining sucrose or by adding some molasses to white refined sugar. 1/29/2019 F.R.SIDDIQUEE 84 Lactose • Lactase convert lactose into glucose and galactose. • Milk, our only source of lactose, is also our most dependable source of calcium. • In most mammals, intestinal lactase activity is high at birth, declines to low levels during childhood, and remains low in adulthood. • Lactase deficiency may also arise as a secondary condition, resulting from damage to the intestinal mucosa by some other disease process, such as malnutrition, HIV infection and parasitic infestations. • The low levels of lactase in the intestine (lactase insufficiency) are associated with intolerance to milk and other milk products containing lactose (lactose intolerance). • People with lactose intolerance experience a lot of discomfort if they eat large amounts of lactose-containing dairy products. 1/29/2019 F.R.SIDDIQUEE 85 Lactose • They can eat fermented dairy products, such as cheese and yogurt, prepared by fermentation because the fermentative microorganisms convert the original lactose into lactic acid. • Most infants, including those who become lactase insufficient in later life, do have the appropriate levels of enzymes to thrive solely on milk without any problems. The intolerance to lactose in people with lactase insufficiency develops later, in early childhood. • The availability of the enzyme lactase, purified from yeasts and molds, has made it possible for lactose-intolerant people to drink milk or milk products without concern. • The enzyme, which is available in tablet or powder form, is taken before or with lactose-containing foods or is mixed with the food before it is consumed. 1/29/2019 F.R.SIDDIQUEE 86 How does Processing Affect Carbohydrates? • Processing tends to reduce the nutrient density of carbohydrate-rich foods. • Sugar is extracted from sugarcane and sugar beets through a process that purifies the sucrose molecule. This is accomplished by removing all of the starch, fiber, minerals, and vitamins. Not surprisingly, the resulting refined sugar is considered ‘empty calories’. • Like sugar and starch, whole grains are refined to make white flour. This process, which removes the fiber-rich bran and the vitamin-rich germ, leaves mainly the powdery, white starch of the endosperm. • Law in USA requires the manufacturers of any flour or flour product to add back three of the B-complex vitamins (thiamin, riboflavin and niacin) plus the minerals iron at the same levels in which they were present before refining. 1/29/2019 F.R.SIDDIQUEE 87 How does Processing Affect Carbohydrates? • Not replaced, however, are fiber and many other vitamins and minerals. The result is a major source of kcalories that is much lower in nutrient density than the whole grain from which it was derived. • If animals store glucose in their tissues as glycogen, why are not meats a good source of dietary carbohydrate? • First of all, the amount of glycogen that animals, or for that matter humans, can store is relatively small. The entire body contains only a couple of hours’ worth of energy in the form of glycogen. • Second, any glycogen that was present in an animal’s tissues is depleted when the animal is fasted or frightened before slaughter. 1/29/2019 F.R.SIDDIQUEE 88 Changes in Carbohydrate during Cooking • The effects of heating on carbohydrates are predominantly beneficial in that it break down the cell walls, solubilizes starch and makes it more easily digested. • The heat during cooking cause the starch within the cells to swell. This bursts the cell walls, and the starch and other nutrients within become accessible to digestive enzymes. 1/29/2019 F.R.SIDDIQUEE 89 Total Carbohydrate • Although the individual components of dietary carbohydrate are readily identifiable, there is some confusion as to what comprises total carbohydrate as reported in food tables. • Two principal measures of total carbohydrate are used, firstly, that derived by "difference" and secondly the direct measurement of the individual components which are then combined to give a total. • Calculating carbohydrates by "difference" has been used since the turn of the century. • The protein, fat, ash and moisture content of a food are determined, subtracted from the total weight of the food and the remainder, or "difference", is considered to be carbohydrate. 1/29/2019 F.R.SIDDIQUEE 90 Total Carbohydrate …. • There are, however, a number of problems with this approach to total carbohydrate analysis in that the "by difference" figure includes a number of noncarbohydrate components such as lignin, organic acids, tannins, waxes, and some Maillard products. • In addition to this error, it combines all of the analytical errors from the other analyses. • Finally, a single global figure for carbohydrates in food is uninformative because it fails to identify the many types of carbohydrates in a food and thus to allow some understanding of the potential physiological properties of those carbohydrates. 1/29/2019 F.R.SIDDIQUEE 91 Total Carbohydrate …. • There are, however, a number of problems with this approach to total carbohydrate analysis in that the "by difference" figure includes a number of noncarbohydrate components such as lignin, organic acids, tannins, waxes, and some Maillard products. • In addition to this error, it combines all of the analytical errors from the other analyses. • Finally, a single global figure for carbohydrates in food is uninformative because it fails to identify the many types of carbohydrates in a food and thus to allow some understanding of the potential physiological properties of those carbohydrates. 1/29/2019 F.R.SIDDIQUEE 92 Digestion and Absorption of Carbohydrate • Before carbohydrate can fulfill its role in the body, it must be converted into monosaccharide units that can be absorbed by the intestinal mucosal cells and transported to the blood. • The required changes are brought about by the action of certain enzymes found in the mouth and the intestine and by the acidity of the stomach contents. • In the mouth, salivary α-amylase, or ptyalin, which is present in saliva, partially breaks down starch. It catalyzes the hydrolysis of most α(1-4) linkages but not the final or “terminal” α(1-4) linkages of starch chains, the α(1-4) linkages next to branching points, or the α(1-6) linkages responsible for branching. 1/29/2019 F.R.SIDDIQUEE 93 Digestion and Absorption of Carbohydrate…. • The eventual end products of α-amylase digestion (salivary and pancreatic) are maltose, maltotriose, and α-limited dextrins (branched polymers containing an average of eight glucose units). • In stomach, the food particles mixed with gastric secretions (contain no specific enzyme for the breakdown of carbohydrates), but the HCl in stomach stops the action of salivary amylase. The action of αamylase is inhibited because the optimal pH value of the enzyme is 6.7. • Before the food mixed compltely with the gastric acid secretion, as much as 20% to 30% of the starch may have changed to maltose. • In the small intestine the conditions change from acidic to alkaline, and another potent α-amylase released from the pancreas acts to continue the digestion of starch and dextrins. 1/29/2019 F.R.SIDDIQUEE 94 Digestion and Absorption of Carbohydrate…. • Finally enzymes of small intestine containing α-limited dextrinase, glucoamylase, maltase, lactase, and sucrase, which are able to split α-limited dextrins, maltotriose, maltose, lactose, and sucrose into their respective monosaccharide units. • The monosaccharides glucose, galactose, and fructose produced by this process of digestion are rapidly absorbed across the intestinal wall to the blood in the capillaries that drain into the portal vein. The portal vein carries the monosccharides and other absorbed nutrients to the liver. • When absorbed, monosccharides reach the liver, and fructose and galactose are converted into glucose, which is then carried in the blood to the rest of the body. 1/29/2019 F.R.SIDDIQUEE 95 Summary of Carbohydrate digestion, absorption, and circulation • Source • Mouth • (Salivary glands) Enzyme Products Salivary α-amylase Hydrolyzes α(1-4) linkages, (alkaline pH) producing α-limited dextrins, maltotriose and maltose • Stomach: Hydrochloric acid (acid pH) • Small Intestine Pancreatic α-amylase • (Pancreas) (alkaline pH) • • • • • • Hydrolyzes α(1-4) linkages, producing α-limited dextrins, maltotriose and maltose Intestinal Wall Maltase, Sucrase,Hydrolyzes maltose & (intestinal mucosa) Lactase maltotriose to glucose α-limited dextrinase Sucrose to glucose & fructose (alkaline pH) Lactose to galactose & glucose Sugars enters to blood after absorption Starch to glucose then to the liver Glucose Systemic circulation 1/29/2019 F.R.SIDDIQUEE 96 Class Work - 1 • Calculation of Energy Available from Food • Two slices of bread with one tablespoon of butter on it contains 25 grams carbohydrate, 8 grams protein, and 10 grams fat, calculate the total energy provided by the above food ? • To calculate the energy available from a food, multiply the number of grams of carbohydrate, protein, and fat by 4, 4, and 9, respectively. Then add the results together to find out the total energy from that particular food. • Therefore, • 25 g carbohydrate X 4 kcal/g = 100 kcal • 8 g protein X 4 kcal/g = 32 kcal • 10 g fat X 9 kcal/g = 90 kcal • Total = 222 kcal. • From this information, we can calculate the percentage of kcalories each of the energy nutrients contributes to the total. 97 1/29/2019 F.R.SIDDIQUEE 97 Percentage of Calories from Nutrients • To determine the percentage of kcal from fat, for example, divide 90 fat kcal by the total 222 kcal. • 90 fat kcal ÷ 222 total kcal = 0.405 (rounded to 0.41) • Then multiply by 100 to get the percentage: • 0.41X 100 = 41% • Health recommendations that urge people to limit fat intake to 30% of kcal to the day's total energy intake. i.e., daily recommended fat intake should be 30% of total energy intake. • If the proportion of fat in each food choice throughout a day exceeds 30% of kcal, then the day's total surely will, too. • Knowing that this snack provides 41% of its kcal from fat alerts a person to choose a low-fat selections of food at other times of the day. • Q. What percentage of the energy comes from carbohydrate and protein ? 1/29/2019 F.R.SIDDIQUEE 98 98 More Calculation Q 1. How many kcalories one would derive by eating 250 g of bread containing 11.5 g of protein, 4.2 g of fat and 32 g of carbohydrates? Also calculate what percentage of the energy in bread comes from each energy yielding nutrients? Ans. Kcalories from energy nutrients in bread : • 11.5 g protein x 4 kcal/g = 46 kcal from protein • 4.2 g fat x 9 kcal/g = 37.8 kcal from fat 32 g Carbohydrate x 4 kcal/g = 128 kcal from carbohydrate • Total = 211.8 kcal • Percentage of energy from each energy nutrients : • (46 kcal ÷ 211.8 kcal) x 100 = 21.8% kcal (protein) • (37.8 kcal ÷ 211.8 kcal) x 100 = 17.8% kcal (fat) • (128 kcal ÷ 211.8 kcal) x 100 = 60.4% kcal (carbohydrate) • Total = 100% 99 1/29/2019 F.R.SIDDIQUEE 99 • Q 2. Calculate how many of the 213 kcalories provided by a 340 ml beer come from alcohol, if the beer contains 2 g protein, and 18 g carbohydrates. How many grams of alcohol does this represent? • Ans to Q 2. • Kcalories from energy nutrients of beer : • 2 g protein = 8 kcal from protein • 18 g carbohydrate = 72 kcal from carbohydrate • 213 total kcal – 80 kcal(protein + carbohydrate) = 133 kcal from alcohol. • 133 kcal alcohol ÷ 7g/kcal = 19 g alcohol 1/29/2019 F.R.SIDDIQUEE 100 100 • Q 3. A food label says that this particular food gives only 18 kcal per 100 g and the chemical composition says that it contains 5 g of protein, 1 g of fat per 100 g of food. • Is this label misleading ? Why or why not ? • Ans to Q 3. • Yes, the label is misleading. • Because having 5 g protein and 1 g fat contains • ( 5 g protein x 4 kcal/g) = 20 kcal and • (1 g fat x 9 kcal/g) = 9 kcal • Total = 29 kcal energy. • Therefore gives 18 kcal per 100 g can not be true. 1/29/2019 F.R.SIDDIQUEE 101 101 • Q 4. Suppose your energy intake for the day is 1500 kcalories (kcal). What percentage of the Daily Value (DV) or daily requirement for energy does your intake represent ? (Use the Daily Value of 2000 kcal as the standard). • Ans. • 1500 kcal (energy intake) ÷ 200 kcal (DV) = 0.75 • Therefore, 0.75 x 100 = 75% of the Daily Value. • The energy intake represent 75% of daily requirement. 1/29/2019 F.R.SIDDIQUEE 102 102 • Q1. Calculate how much energy come from alcohol of the 172 kcalories provided by a snack (containing 8 grams carbohydrate, 3 grams protein and 4 grams fat) and a 15-ounce can of beer, if the beer contains 1 gram protein and 14 grams carbohydrate. • (Hint : The remaining kcalories derive from alcohol). How many grams of alcohol does this represent ? • Ans. to Q.1. • 8 g carbohydrate from snack and 14 g from beer = 22 g carbohydrate • • 22 g carbohydrate x 4 kcal/g = 88 kcal from carbohydrate • Similarly, 3 g + 1 g = 4 g protein x 4 kcal/g = 16 kcal from protein • 4 g fat (only from snack) x 9 kcal/g = 36 kcal from fat • ------• Total energy from energy nutrients = 140 kcal • 172 total kcal – 140 kcal (carbohydrate + protein + fat) • = 32 kcal from alcohol. • Therefore, 32 kcal alcohol ÷ 7 g/kcal = 4.57 g alcohol • Ans. 32 kcal energy come from alcohol and it represent 4.57 g alcohol 1/29/2019 F.R.SIDDIQUEE 103 Key to Quiz 1….. • Q2. Consider an advertisement of a new "health food" product that claims that the product provides 17 grams protein and 12 kcal per dose. Is it possible ? If not then why not ? • Ans. to Q2. • No, it is not possible. • Having 17 g protein contains (17 g protein x 4 kcal/g) 68 kcal energy. • Therefore, containing 12 kcal can not be true. • Q3. A diet provides a total of 2200 kcalories of which 40% of the energy is from fat and 20% from protein. How many grams of carbohydrate are contained in the diet? • a. 220 • b. 285 • c. 440 • d. 880 • 40% energy from fat + 20% from protein, so rest 40% from carbohydrate. • Total 2200 kcal, so 40% of that (2200 X 0.40) = 880 kcal from carbohydrate and as 1 g carbohydrate gives 4 kcal energy, 880 kcal is given by (880 kcal/4) = 220 g carbohydrate 1/29/2019 F.R.SIDDIQUEE 104 Key to Quiz 1….. • Q4. What is the kcalorie value of a meal supplying 110 g of carbohydrates, 25 g of protein, 20 g of fat, and 5 g of alcohol? • a. 160 • b. 345 • c. 560 • d. 755 • • • • • • • Ans. 110 g carbohydrate X 4 kcal/g = 440 kcal 25 g protein X 4 kcal/g = 100 kcal 20 g fat X 9 kcal/g = 180 kcal 5 g alcohol X 7 kcal/g = 35 kcal ------------755 kcal 1/29/2019 F.R.SIDDIQUEE 105 Key to Quiz 1….. • Q 5a: • Suppose one kg of body fat equals to about 7,800 kilocalories. Therefore, losing 1 kg requires a 7,800 kilocalories deficit. The opposite is true for weight gain. • If you added 520 kilocalories from an extra sandwich, fruit salad, or a bag of chips to your normal eating plan every day – without boosting your activity level --- how long it will take to gain 1 kg ? • Ans. • • • 1/29/2019 7,800 kcal = 1 kg of body fat 7,800 kcal ÷ 520 kcal per day = 15 days. Therefore, 15 days will need to gain 1 kg. F.R.SIDDIQUEE 106 More Calculation • Q 5b: • Suppose one kg of body fat equals to about 7,800 kilocalories. Therefore, losing 1 kg requires a 7,800 kilocalories deficit. The opposite is true for weight gain. • (b) If you burned 260 extra kilocalories per day by walking about 30 minutes – 5 days a week without increasing your calorie intake – how long it will take to lose that 1 kg from body fat and from where it would come? • Ans. • 260 kcal per day X 5 days = 1300 kcal per week • Therefore, 1 kcal in (1 ÷ 1300) week • To burned 7800 kcal then required • [(1 ÷ 1300) X 7800] week = 6 weeks. • 7800 kcal = 1 kg body fat • Therefore, 4 weeks will be needed and it will come from body fat. 1/29/2019 F.R.SIDDIQUEE 107 1/29/2019 F.R.SIDDIQUEE 108 108 Book References • Human Nutrition by Helen A. Guthrie and Mary F. Picciano, McGraw Hill Publisher, 1995. • Understanding Nutrition. By Ellie Whitney and Sharon Rady Rolfes. 3rd Edition, Thomson Wadsworth, USA, 2005. • Nutrition: Concepts and Controversies. By Frances Sizer and Ellie Whitney. 10th Edition, Thomson Wadsworth, USA, 2005. • Discovering Nutrition. By Paul Insel, R. Elaine Turner and Don Ross. 2nd Edition, American Dietetic Association, Jones and Bartlett Publishers, Inc. USA, 2006. 1/29/2019 F.R.SIDDIQUEE 109 Role of Proteins in Human Nutrition BMB 408 – HUMAN NUTRITION Yearul Kabir (Handout # 3) 1/29/2019 F.R.SIDDIQUEE 110 Protein • Protein has been recognized as a dietary essential for well over a century. Proteins perform many different functions in the body: • Structural components of body tissues (especially in muscles, cartilage, and bone); e.g., collagen. • Enzymes, hormones, components of the immune system (antibodies) • Transporters of other substances; e.g., hemoglobin. • Membrane-bound carriers e.g., Retinol binding protein (RBP) • Blood clotting • Regulators of many biochemical processes (Regulators of fluid balance, acidbase regulators) and • Source of energy and glucose • Protein is a source of the amino acids and nitrogen needed for the synthesis of the proteins of the body. The primary role of dietary protein is to supply amino acids for biosynthesis, but it can also be used as a source of energy. 1/29/2019 F.R.SIDDIQUEE 111 Chemical Composition of Protein • All proteins are synthesized from amino acid molecules and 20 different amino acids are used in protein synthesis, although a protein can contain many hundreds of amino acid units (or residues) overall. • All amino acids contain an amino group, a carboxyl group, and a hydrogen atom attached to a central carbon atom, which is also bonded to the side chain or side group of the amino acid. The side chain is the only part of the structure that varies. • The fact that all amino acids contain nitrogen is important in the chemical analysis of foods because it distinguishes proteins from carbohydrates and lipids, which contain no nitrogen. 1/29/2019 F.R.SIDDIQUEE 112 Protein Proteins contain Carbon (C), Hydrogen (H), Oxygen (O) atoms as in carbohydrates and lipids, but in addition contain Nitrogen (N), and sometimes Sulphur (S). Basic units ➞ Amino Acids. Amino Acids: All have the same basic structure 1. A central carbon atom (C) with a hydrogen (H) 2. An amino group (NH2) 3. An acid group (COOH) 4. A variable side group (R) All amino acids are identical in structure except the side group, R, which differs in different amino acids. 1/29/2019 F.R.SIDDIQUEE 113 Nutritional Classification of Amino Acids • From a nutritional point of view, amino acids are classified into two groups: • Essential (indispensable) and • Non-essential (dispensable). • Essential amino acids are ones that cannot be synthesized by the body at a rate sufficient to meet the needs for growth and maintenance. It is essential that these amino acids are provided in the diet. • Nonessential amino acids are ones that the body can make in adequate amounts from other compounds if necessary. The label nonessential does not mean that the body does not need these amino acids – it does. They are “nonessential” only in the sense that they are not essential components of the diet. 1/29/2019 F.R.SIDDIQUEE 114 Nutritional Classification of Amino Acids…. • There are 9 essential amino acids that cannot be made by the body and, therefore, have to be supplied in the diet. • They are leucine, isoleucine, valine, lysine, tryptophan, threonine, methionine, phenylalanine, and histidine. • Histidine is the most recent addition to the list because it was only recently recognized that adults are unable to synthesize enough histidine to meet their needs over a long period. • If sufficient nitrogen is available in the diet, the body can synthesize adequate supplies of the other 11 amino acids. The cells of the body are able to synthesize the carbon skeleton and add the sidechains of 11 of the 20 amino acids, using amino groups from other amino acids. 1/29/2019 F.R.SIDDIQUEE 115 Amino Acids • Conditionally essential amino acids: sometimes a nonessential amino acid becomes essential under special circumstances, when the need for it exceeds the body’s ability to produce it. • Example: the body normally uses the essential amino acid phenylalanine to make tyrosine (a nonessential amino acid). • But if the diet fails to supply enough phenylalanine, or if the body cannot make the conversion for some reason (happens in the inherited disease phenylketonuria), then tyrosine becomes conditionally essential. • Some amino acids may become indispensable in certain circumstances such as: arginine in case of urea cycle disorders. 1/29/2019 F.R.SIDDIQUEE 116 1/29/2019 F.R.SIDDIQUEE 117 Amino acid sequences • Proteins are made up of about 20 common amino acids. • Amino acids link end-to-end in a variety of sequences to form thousands of different polypeptide chains and many proteins (all enzymes, hormones are proteins). • A peptide bond unites each amino acid to the next. • Protein denaturation • ►Heat, acid, or other conditions disturb the stability of proteins. • ► Proteins uncoil and lose their shape and ability to function. • ►The proteins is said to undergo denaturation, e.g., • hardening of egg when cooked • curdling of milk when acid is added. • Past a certain point, denaturation is irreversible. 1/29/2019 F.R.SIDDIQUEE 118 Nitrogen Balance • Nitrogen balance reflects whether a person is gaining or losing protein. • In healthy adults, protein synthesis balances with degradation, and protein intake from food balances with nitrogen excretion in the urine, feces, and sweat. • A pregnant woman is adding protein, so she has a positive nitrogen balance. • A healthy person who is neither gaining nor losing protein is in nitrogen equilibrium (zero balance). • A person who is severely ill and losing protein has a negative nitrogen balance. 1/29/2019 F.R.SIDDIQUEE 119 Nitrogen Balance…. • The amount of nitrogen consumed (N in) compared with the amount of nitrogen excreted (N out) in a given period of time. • • N in = N out ► Nitrogen equilibrium (zero nitrogen balance). N in > N out ► Positive N balance. Growing infants, children, pregnant women, people recovering from protein deficiency or illness. • N in < N out ► Negative N balance. Starving, severe stress such as burns, injuries, infections, and fever. • About 10-15 g nitrogen are excreted each day in the urine of a healthy adult, mostly in the form of urea, with smaller contributions from ammonia, uric acid, creatinine and some free amino acids. Urea: 12.9 g Nitrogen/24 h 1/29/2019 F.R.SIDDIQUEE 120 1/29/2019 F.R.SIDDIQUEE 121 Protein Metabolism • Protein Turnover and the Amino Acid Pool • Proteins are constantly made and broken down within each cell of the body. The degradation and synthesis of protein is called protein turnover. • Breakdown of protein frees amino acids which join the general circulation, or mix with amino acids from food protein to form an “amino acid pool” within the cells and circulating blood. • The rate of protein degradation and the amount of protein intake may vary, but the pattern of amino acids within the pool remains fairly constant. 1/29/2019 F.R.SIDDIQUEE 122 Protein Metabolism…. • Using Amino Acids to Make Proteins or Nonessential Amino Acids • If a particular nonessential amino acid is not readily available, cells can make it from another amino acid. • If an essential amino acid is missing, the body may break down some of its own proteins to obtain it. • Using Amino Acids to Make Other Compounds • The amino acid tyrosine is used to make the neurotransmitters norepinephrine and epinephrine. • Tryptophan serves as a precursor for the vitamin niacin and neurotransmitter serotonin. 1/29/2019 F.R.SIDDIQUEE 123 Protein Metabolism…. • Using Amino Acids for Energy and Glucose • When glucose or fatty acids are limited, the cells are forced to use amino acids for energy and glucose. • The body dismantles its tissue proteins and uses them for energy. • Deaminating Amino Acids • Amino acids are first deaminated before they are broken down for energy. • Deamination strips off the nitrogen-containing amino groups and produces ammonia which is released into the blood stream. • The liver picks up the ammonia, and converts it into urea, and returns the urea to the blood. • The kidneys filter urea out of the blood, and amino nitrogen ends up in the urine. 1/29/2019 F.R.SIDDIQUEE 124 Protein Metabolism…. • Using Amino Acids to Make Fat • If protein is eaten in excess of the body’s need, the amino acids are deaminated and nitrogen is excreted. • The remaining carbon fragments are converted to fat and stored for later use. • In this way, protein-rich foods can contribute to obesity. • Protein Synthesis • For protein synthesis to occur, all the essential amino acids should be present and in sufficient quantity in the food eaten. This determines the protein quality of the food. 1/29/2019 F.R.SIDDIQUEE 125 Protein Quality • The quality of a dietary protein is determined by the kind of amino acids it contains and the proportions in which they are present. • Good quality proteins contain all of the essential amino acids in proportions capable of promoting growth when they are the only proteins in the diet. • Such proteins are known as complete proteins and proteins of high biological value. • Essential amino acids normally compose about one third of the amino acids in such protein. • All animal proteins, except gelatin (which has limited amounts of tryptophan and lysine), are complete proteins. 1/29/2019 F.R.SIDDIQUEE 126 Protein Quality…. • High-Quality (Complete) Proteins • Dietary proteins containing all the essential amino acids in relatively the same amounts that human beings require. They may also contain nonessential amino acids. • Contain all the essential amino acids and are highly digestible. e.g., fish, meat, poultry, cheese, eggs, milk proteins. • Plant proteins (vegetables, grains, legumes) may be limiting in one or more essential amino acids. • ► Soy protein is complete, corn protein incomplete. • Reference protein: a standard against which to measure the quality of other proteins. e.g., egg protein, assigned the value of 100. 1/29/2019 F.R.SIDDIQUEE 127 Protein Quality…. • Poor quality proteins, described as incomplete proteins or proteins of low biological value, are those that lack or have limited amounts of one or more essential amino acids. • Protein quality is influenced by two factors: protein’s digestibility and amino acid composition. • • Protein Digestibility • A measure of the amount of amino acids absorbed from a given protein intake. • Animal proteins ► high digestibility (90 -99%). • Plant proteins ► low digestibility (70 - 90%). [Soy and legumes > 90%]. 1/29/2019 F.R.SIDDIQUEE 128 Protein Quality…. • Amino Acid Composition • Protein synthesis will be limited if the diet contains too little of any of the 9 essential amino acids. • An essential amino acid supplied in less than the amount needed for protein synthesis is called a limiting amino acid. • The absence of a limiting amino acid from the diet will limit protein synthesis. • Four most limiting amino acids: Lysine, Methionine, Threonine, Tryptophan. 1/29/2019 F.R.SIDDIQUEE 129 Protein Quality…. • Some proteins that contain all the essential amino acids but a relatively small amount of one of them have sufficient amino acids to promote the repair of body tissues but not enough to promote growth. • In such proteins the amino acid present in the smallest amount, relative to the amount required for growth, is called the limiting amino acid of the protein. • Methionine is the limiting amino acid in legumes, and lysine is the limiting amino acid in cereal protein. • Vegetable sources of proteins such as soybeans contain some of all the essential amino acids, but they do not have enough of one or more of them to be effective in meeting the needs for growth. 1/29/2019 F.R.SIDDIQUEE 130 Protein Quality…. • If a protein is to be useful to the body, it should supply all of the indispensable amino acids in appropriate amounts. • If this is not the case, any synthesis that is required can only take place by breaking down existing proteins. • Alternatively, limited synthesis may take place until all of the amino acid present in least amounts has been used up. • The body cannot synthesize incomplete proteins, therefore, synthesis is limited by this amino acid. Such as amino acid is termed “limiting” and the protein from which it comes would described as having low quality. 1/29/2019 F.R.SIDDIQUEE 131 Complement Protein • By combining two proteins that are limiting in different amino acids, it is possible to make a complete good quality protein. In this way, vegetarian diets can be as adequate in protein as diets containing both animal and vegetable proteins. • For example, wheat has ample methionine but lacks lysine, and soybeans have ample lysine but are limited in methionine, so a combination of wheat and soybeans provides a mixture of amino acids capable of promoting growth. • It is possible to complement protein foods of plant origin with foods derived from animals to compensate for the limiting amino acid. • In particular, milk and its products provide good complementary protein to partner the plant foods. 1/29/2019 F.R.SIDDIQUEE 132 Complementary Proteins • Two or more proteins whose amino acids complement each other in such a way that the essential amino acids missing from one are supplied by the other. e.g., • Legumes (+Isoleucine, +Lysine; -Methionine, -Tryptophan). • Grains (-Isoleucine, -Lysine; +Methionine, +Tryptophan) 1/29/2019 F.R.SIDDIQUEE 133 Complement Protein…. • Populations have naturally been doing this type of protein combination (or complementation) for generations; there is nothing new about it and many traditional dishes reflect this. • Examples of such traditional mixtures includes: • • • • Bread and cheese Macaroni cheese Rice pudding Cereal and milk Why do the proteins of animal sources have better nutritional quality than proteins of plant sources? 1/29/2019 F.R.SIDDIQUEE 134 Complement Protein…. 1/29/2019 F.R.SIDDIQUEE 135 1/29/2019 F.R.SIDDIQUEE 136 1/29/2019 F.R.SIDDIQUEE 137 How the Protein Quality can be Quantified? • A Measure of Protein Quality • Several biological and chemical methods for evaluating the quality of food proteins and identifying high-quality proteins have been developed. The most commonly used methods are: • Protein digestibility–corrected amino acid score (PDCAAS) • A measure of protein quality assessed by comparing the amino acid score of a food protein with the amino acid requirements of preschool-age children and then correcting for the true digestibility of the protein; recommended by the FAO/WHO. • First the protein’s amino acid composition is determine, and then it is compared against the amino acid requirements of preschool-age children. This comparison reveals the most limiting amino acid – the one that falls shortest compared with the reference. 1/29/2019 F.R.SIDDIQUEE 138 Measuring Protein Quality…. • To determine how well the food protein meets human needs, we need to calculate the ratio by dividing the amino acid profile of food protein by the amino acid reference pattern (for example, 30÷18 = 1.67). The amino acid with the lowest ratio is the most limiting amino acid – in this case, methionine. Its ratio is the amino acid score for the protein – in this case 0.84. • If a food protein’s limiting amino acid is 70 percent of the amount found in the reference protein, it receives a score of 70. • Essential AA AA profile(mg/g prot.) AA ref. prot. (mg/g) A.A. Score • Histidine 30.0 18 1.67 • Isoleucine 42.5 25 1.70 • Methionine 21.1 25 0.84 • Lysine 1/29/2019 69.0 51 F.R.SIDDIQUEE 1.35 139 Measuring Protein Quality…. • The amino acid score alone, however, does not account for digestibility. Protein digestibility, as determined by rat studies, yields a value of 79% for pinto beans. • The amino acid score multiplied by the food’s protein digestibility percentage gives the PDCAAS value. • PDCAAS = protein digestibility X amino acid score • PDCAAS for pinto beans = 0.79 x 0.84 = 0.66 • PDCAAS Values of Selected Foods: Casein – 1.00; Egg white – 1.00; Beef – 0.92; Pinto beans – 0.66. • Egg proteins have traditionally been used as the “reference proteins” as their amino acid pattern most nearly conforms to that of total body protein. Most recently, the amino acid pattern in human milk has been set as the standard against which all other proteins can be judged for their efficiency of meeting human needs. 1/29/2019 F.R.SIDDIQUEE 140 Measuring Protein Quality…. • Amino Acid Scoring • A measure of protein quality assessed by comparing a protein’s amino acid pattern with that of a reference protein; sometimes called chemical scoring. • Advantages: Simple and inexpensive, it easily identifies the limiting amino acid. • Disadvantages: Fails to estimate the digestibility of a protein, which may strongly affect the protein’s quality. • It relies on a chemical procedure in which certain amino acids may be destroyed, making the pattern that is analyzed inaccurate. 1/29/2019 F.R.SIDDIQUEE 141 • A Reference Pattern for Amino Acid Scoring of Protein (whole egg) • For every 3210 units of essential amino acids, 145 must be histidine, 340 must be isoleucine, 540 must be leucine, and so on. 1/29/2019 F.R.SIDDIQUEE 142 Measuring Protein Quality…. • To compare a text protein with the reference protein, the chemical analysis of the test protein’s amino acids was done. • Then, taking 3210 units of the amino acids, we need to compares the amount of each amino acid to the amount found in 3210 units of essential amino acid in egg protein. • For example, suppose the test protein contained (per 3210 units) 360 units of isoleucine; 500 units of leucine; 350 of lysine; and for each of the other amino acids, more units then egg protein contains. • The two amino acids that are low are leucine (500 as compared with 540 in egg) and lysine (350 versus 440 in egg). 1/29/2019 F.R.SIDDIQUEE 143 Measuring Protein Quality…. • The ratio, amino acid in the test protein divided by amino acid in egg, is 500/540 (or about 0.93) for leucine and 350/440 (or about 0.80) for lysine. • Lysine is the limiting amino acid (the one that falls shortest compared with egg). If the protein’s limiting amino acid is 80 percent of the amount found in the reference protein, it receives a score of 80. 1/29/2019 F.R.SIDDIQUEE 144 Measuring Protein Quality…. • Biological Value • The BV of a protein is measured as the percentage of absorbed nitrogen that is retained (that is, not excreted) for use in growth or maintenance. This indicator is based on the assumption that more nitrogen is retained when the essential amino acids are present in sufficient amounts to meet the needs for growth. • In a test of BV, two nitrogen balance studies are done. • In the first, no protein is fed, and nitrogen (N) excretions in the urine and feces are measured. • It is assumed that under these conditions, N lost in the urine is the amount the body always necessarily loses by filtration into the urine each day, regardless of what protein is fed (endogenous N). 1/29/2019 F.R.SIDDIQUEE 145 Measuring Protein Quality…. • The N lost in the feces (called metabolic N) is the amount the body invariably loses into the intestine each day, whether or not food protein is fed. • Endogenous N is “urinary N on a zero-protein diet”. • Metabolic N is “fecal N on a zero-protein diet”. • In the second study, an amount of protein slightly below the requirement is fed. Intake and losses are measured; then the BV is derived using this formula: • BV = (Nitrogen retained/Nitrogen absorbed) x 100 • Egg protein has a BV of 100, indicating that 100% of the N absorbed is retained. • A food or diet with a BV of 70 or more (meaning that 70% of the absorbed nitrogen is retained) is considered capable of supporting growth, assuming that the diet provides sufficient energy. 1/29/2019 F.R.SIDDIQUEE 146 Measuring Protein Quality…. • Advantages: Being based on experiments with human beings and of measuring actual nitrogen retention. • Disadvantages: • Involves controlled animal feeding studies, which makes it a cumbersome, costly and time consuming procedure. • It is based on several assumptions that may not be valid. For example, the physiology, normal environment, or typical food intake of the subjects used for testing may not be similar to those for whom the test protein may ultimately be used. • For another example, the retention of protein in the body does not necessarily mean that it is being well utilized. 1/29/2019 F.R.SIDDIQUEE 147 Measuring Protein Quality…. • Net Protein Utilization • Like BV, NPU measures how efficient a protein is used by the body and involves two balance studies. • NPU is the percentage of ingested nitrogen that is retained. • NPU = (Nitrogen retained / Nitrogen intake) x 100 • Advantages: Similar as BV. Used more frequently animals as test subjects. • Disadvantages: Because it does not take into account differences in the digestibility of proteins, it gives a poorly digested but good quality protein a false low value. i.e., it does not distinguish between two possible caused: a poor amino acid composition of the test protein or poor digestibility. 1/29/2019 F.R.SIDDIQUEE 148 Measuring Protein Quality…. • Protein Efficiency Ratio • Measures the weight gain of a growing animal and compares it to the animal’s protein intake. Until recently, the PER was generally accepted in the USA and Canada as the official method for assessing protein quality, and it is still used to evaluate proteins for infants. • Young rats are fed a measured amount of protein and weighed periodically as they grow. The PER is expressed as: • PER = weight gain (g)/protein intake (g). • Advantages: Less costly and simple . • Disadvantages: Time consuming; the amino acid needs of rats are not the same as those of human beings; and the amino acid needs for growth are not the same as for the maintenance of adult animals (e.g., growing animals need more lysine). 1/29/2019 F.R.SIDDIQUEE 149 Health Effects of Protein • Insufficient protein intake is a problem for many people of the world, especially the poor in many countries. • Protein-Energy Malnutrition (PEM) • A condition that arises from deficiency of protein, energy, or both. • Mostly affects children during early childhood. • Children who are thin for their height may be suffering from acute PEM (recent severe food deprivation), whereas children who are short for their age have experienced chronic PEM (long-term food deprivation). • Poor growth due to PEM is easy to overlook because a small child may look quite normal. • Afflicting 500 million children. Most of the 33,000 children who die each day are due to PEM. 1/29/2019 F.R.SIDDIQUEE 150 Protein deficiency • Children are most likely to suffer from protein deficiency in a complex picture of protein-energy malnutrition (PEM). • Classically, the two main forms of PEM are marasmus and kwashiorkor; there is considerable debate as to whether these are separate conditions or two ends of the spectrum of the same conditions. • They have been seen to occur in the same village and even in the same child at different times, suggesting a common cause. 1/29/2019 F.R.SIDDIQUEE 151 Classification of PEM • Two forms: Marasmus: Characterized by extreme wasting: just skin and bones. • A severe deprivation of food over a long time (chronic PEM). • ► inadequate intake of energy, protein, essential fatty acids, vitamins and minerals. • ► occurs mostly in children 6 to 18 months old. • Marasmic children look like little old people. Little or no fat under the skin. • Compared with healthy people, marasmic individuals are more susceptible to infection, and more likely to suffer death or disability from infection. The extreme loss of muscle • and fat characteristic of • marasmus is apparent in • this child’s “matchstick” • arms. 1/29/2019 F.R.SIDDIQUEE 152 Effects of Marasmus • • • • impairs brain development and learning ability. slow metabolism and lower body temperature. growth cessation (short height for age: stunting) inability to digest food. 1/29/2019 F.R.SIDDIQUEE 153 1/29/2019 F.R.SIDDIQUEE 154 Marasmus 1/29/2019 F.R.SIDDIQUEE 155 Classifying PEM…. • Kwashiorkor: A sudden and recent severe deprivation of food (acute PEM). • ► inadequate intake of protein or (measles). Thinness for height (wasting) • ► occurs mostly in children between months and 2 years. • The edema and enlarged liver characteristic of apparent in this child’s swollen • Malnourished children commonly have an abdomen from parasites as well. 1/29/2019 F.R.SIDDIQUEE infections 18 belly. kwashiorkor are enlarged 156 Effects of Kwashiorkor • Loss of weight and body fat. • Inability to maintain body fluid balance, leakage of fluid into interstitial spaces. • The child’s limbs and face become swollen with edema, a distinguishing feature of kwashiorkor. • Fatty liver ➞bulging belly (no protein carriers to transport fat out of the liver). • Hair color loss. 1/29/2019 F.R.SIDDIQUEE 157 1/29/2019 F.R.SIDDIQUEE 158 1/29/2019 F.R.SIDDIQUEE 159 Marasmus-Kwashiorkor Mix • The combination of marasmus and kwashiorkor is characterized by the edema of kwashiorkor with the wasting of marasmus. • Most often, the child is suffering the effects of both malnutrition and infections. • Some researchers believe that kwashiorkor and marasmus are two stages of the same disease. • They point out that kwashiorkor and marasmus often exist side by side in the same community. 1/29/2019 F.R.SIDDIQUEE 160 Health Effects of Protein Excess Protein • Over consumption of proteins offer no benefits and may pose health risks. • In developed countries, excess protein and energy are a greater problem than protein deficiency. • Obesity: Excessive protein intakes often lead to dietary imbalance, increasing fat consumption while crowding fruits, vegetables, and grains out of the diet. • Heart Disease: Diets rich in animal protein often associated with high intakes of saturated fat and cholesterol. • Osteoporosis: Excess calcium excretion may occur with high protein and low calcium intakes. • Cancer: Diets high in red meat have been linked to colon and prostate cancers. 1/29/2019 F.R.SIDDIQUEE 161 Recommended Protein Intake • The safe level of protein intake was established by FAO/WHO/UNU as 0.75 g/kg body weight per day. • 10 to 15% of daily energy intake. • In a 2000 kcal diet, that represents 200 to 300 kcal, or 50 to 75 g. • RDA for adults: 0.8 g /kg body weight /day. • ► Higher requirements for: • larger people, infants, children, pregnant women, athletes ➞ requirement increases when replacing worn-out tissue, building new tissue during growth etc. • Daily Value • 50 g protein • 10% of a 2000 kcal diet 1/29/2019 F.R.SIDDIQUEE 162 How to Calculate Protein RDA • The RDA is 0.8 g protein per kg healthy body weight. • Examples: • Male, 19+ years old, 70 kg • 70 kg X 0.8 g/kg = 56 g protein per day • Female, 19+ years old, 57 kg • 57 kg X 0.8 g/kg = 46 g protein per day 1/29/2019 F.R.SIDDIQUEE 163 How to Calculate Amount of Protein • The characteristic element in protein is nitrogen, which constitutes about 16% of its weight. • That is, on average, amino acid weight about 6.25 times as much as the nitrogen. • 100 ÷ 16 = 6.25 • Therefore, scientist estimate the amount of protein in a sample of food, body tissue, or other material by multiplying the weight of nitrogen in it by 6.25. 1/29/2019 F.R.SIDDIQUEE 164 Recommended Books • Understanding Nutrition. By Ellie Whitney and Sharon Rady Rolfes. 3rd Edition, Thomson Wadsworth, USA, 2005. • Nutrition: Concepts and Controversies. By Frances Sizer and Ellie Whitney. 10th Edition, Thomson Wadsworth, USA, 2005. • Discovering Nutrition. By Paul Insel, R. Elaine Turner and Don Ross. 2nd Edition, American Dietetic Association, Jones and Bartlett Publishers, Inc. USA, 2006. 1/29/2019 F.R.SIDDIQUEE 165 Protein Digestion • Goal: To supply the amino acids from which the body makes its own proteins. • When a person eats foods containing protein, enzyme break • long polypeptides ➞ shorter polypeptides ➞ tripeptides, dipeptides ➞ amino acids. • Mouth • Chewing and crushing moisten protein-rich foods and mix them with saliva to be swallowed. 1/29/2019 F.R.SIDDIQUEE 166 Protein Digestion….. • Stomach • Major event ➞Partial hydrolysis of proteins. • ► Hydrochloric acid (HCl) uncoils (denatures) proteins so digestive enzymes can attack the peptide bonds. • ► HCl also converts pepsinogen (inactive) to pepsin (active). • ► Pepsin break down large polypeptides into smaller polypeptides and some amino acids. • Small Intestine • ► Proteases (pancreatic & intestinal) hydrolyze polypeptides into short peptide chains (oligopeptides), tripeptides, dipeptides, and amino acids. • ► Peptidase enzymes then split the dipeptides and tripeptides into single amino acids. 1/29/2019 F.R.SIDDIQUEE 167 1/29/2019 F.R.SIDDIQUEE 168 Protein Absorption • ► Carriers transport the amino acids (and some dipeptides and tripeptides) into the intestinal cells. • ► Here, amino acids may be used for energy or used to synthesize other needed compounds. • ► If not used, they are transported back to the liver. 1/29/2019 F.R.SIDDIQUEE 169 Fats and Oils in Human Nutrition BMB 408: Human Nutrition Yearul Kabir, Ph.D. Handout # 4 Lipids: Triglycerides, Phospholipids & Sterols • The bonding of atoms are different in lipids than in carbohydrates. • In carbohydrates, the carbon atoms are bonded to oxygen; in lipids the carbon atoms are usually bonded to hydrogen. • Fats are solid at room temperature whereas oils are liquid. • There is more energy in the C-H bond of lipids than in the C-O bonds of carbohydrates. • Therefore, lipids supply more energy calories than carbohydrates and proteins. • Classification • Simple lipids: These are esters of fatty acids and glycerol. • Compound lipids: Phospholipids (e.g., Lecithin and cephalin) • Glycolipids- containing carbohydrates in combination with fatty acids and glycerol (e.g., cerebrosides) 1/29/2019 F.R.SIDDIQUEE 171 Classification of Lipids • Simple lipids: These are esters of fatty acids and glycerol. • Compound lipids: In addition to fatty acids and glycerol, lipids contain some other organic compounds. • Phospholipids: contain phosphoric acid and a nitrogenous base in addition to fatty acids and glycerol (e.g., Lecithin and cephalin) • Glycolipids: containing carbohydrates in combination with fatty acids and glycerol (e.g., cerebrosides) • Waxes: These are esters of fatty acids and long chain aliphatic alcohols. • Derived lipids: These include sterols and fatty acids. 1/29/2019 F.R.SIDDIQUEE 172 Roles of Dietary Fat • In general, the functions of lipids are classified as structural, metabolic, regulatory, nutritional and storage. • Serves as a structural component of cell membranes. Lipids in the form of cholesterol and phospholipids of cell membranes modulate various cellular functions. • Endogenously synthesized lipid modulators like prostaglandins, leukotrienes, lipoxins, diacylglycerol and inositol triphosphates mediate the regulatory or physiological functions. • Increases the flavor and palatability of foods • Provides a concentrated source of energy • Carries the essential fatty acids, the fat-soluble vitamins, and certain phytochemicals such as carotenoids 1/29/2019 F.R.SIDDIQUEE 173 Chemistry of Lipids • • • • • • • • • • • Two basic components: Glycerol and Fatty Acids The glycerol has a backbone that can hold up to 3 fatty acids. 1 fatty acid on the glycerol = Monoglyceride 2 fatty acids on the glycerol = Diglyceride 3 fatty acids on glycerol = Triglyceride Most lipids in foods (95%) are triglycerides composed of three fatty acids attached to one molecule of glycerol. Of the lipids stored in the body, 99% are triglycerides. Roles of Tryglycerides (Triacylglycerol) Fuel for the body Insulate the body Helps the body to use carbohydrates and proteins efficiently Fat helps spare proteins for other important tasks. 1/29/2019 F.R.SIDDIQUEE 174 1/29/2019 F.R.SIDDIQUEE 175 Fatty Acids • An organic acid containing carbon atoms with hydrogen atoms attached. It has a methyl group (CH3) at one end and an acid group (COOH) at the other end. • The carbon chain: only even numbers of carbons - up to 24. 18carbon fatty acids commonly found in foods, e.g., Stearic acid. • 12C - 24C common in meats and fish • 6C – 10C or less than 6C present in dairy products 1/29/2019 F.R.SIDDIQUEE 176 Degree of unsaturation • A. Saturated Fatty Acids: fatty acids that are fully loaded with hydrogen atoms and contain only single bonds between the carbon atoms (C-C) e.g. stearic acid. The fatty acid is saturated with hydrogen. • A saturated fat is composed of triglycerides in which all the fatty acids are saturated. • Sources: meat, poultry, milk, butter, egg yolk, lard, chocolate, coconut, coconut oil, vegetable shortening. • B. Unsaturated Fatty Acids: Fatty acids that contain one or more double bonds (C=C) between adjacent carbon atoms. Each pair of double bonded carbon pair is bonded to only 2 hydrogen atoms (1 each). The fatty acid is not saturated with hydrogen. 1/29/2019 F.R.SIDDIQUEE 177 Degree of unsaturation…. • If an unsaturated fatty acid contains only one C=C double bond, it is called a monounsaturated fatty acid, e.g, Oleic acid: 18C, abundant in olive oil. • Sources: avocado, peanuts, peanut butter, olives, olive oil. • If it contains two or more C=C double bonds, it is called polyunsaturated fatty acid, • e.g., Linoleic acid: 18C, 2 double bonds. • Linolenic acid: 18C, 3 double bonds. • Sources: vegetable oils (corn, safflower, soybean, canola etc.), margarine, mayonnaise, almonds, pecans, walnuts, fish. 1/29/2019 F.R.SIDDIQUEE 178 An impossible chemical structure Oleic acid – 18-carbon, monounsaturated Linoleic acid – 18-carbon, polyunsaturated 1/29/2019 F.R.SIDDIQUEE 179 Location of double bonds • The position of the first double bond nearest the methyl (CH3) end in a polyunsaturated fatty acid is used to classify fatty acids using an omega number. • Omega-3 fatty acid: 3 carbons away from CH3 • Omega-6 fatty acid: 6 carbons away from CH3 • Nomenclature • α-Linolenic: C18:3 ω-3 • Linoleic: C18:2 ω-6 1/29/2019 F.R.SIDDIQUEE 180 18-Carbon Fatty Acids • Name Number of Number of Carbon Atoms Double Bonds Saturation • Stearic acid 18 • Oleic acid 0 18 • Linoleic acid 18 • Linolenic acid 1/29/2019 Saturated 1 2 18 Polyunsaturated 3 F.R.SIDDIQUEE Monounsaturated Polyunsaturated 181 Effects of the Degree of Fatty Acid Unsaturation and Chain Length on Fat Properties • Firmness: At room temperature, polyunsaturated vegetable oils liquids • saturated animal fats solid. • Butter more saturated than margarine butter harder than margarine. • Not all vegetable oils are polyunsaturated: cocoa butter, palm oil, coconut oil saturated. Even though they are of vegetable origin, they are firmer than most vegetable oils but softer than most animal fat at room temperature. Because of short carbon chain. 1/29/2019 F.R.SIDDIQUEE 182 1/29/2019 F.R.SIDDIQUEE 183 Fat Properties…. • Stability: polyunsaturated fats spoil most readily due to ease of oxidation of double bonds rancidity. • Saturated fats more resistant to oxidation, less likely to become rancid. • Rancidity in Fats • The development of off-flavours in fats is known as rancidity. There are two main types of rancidity: Hydrolytic and Oxidative • Hydrolytic rancidity: When fat is hydrolysed by lipase, free fatty acids are formed. The odours of low molecular weight fatty acids contribute to the rancidity. 1/29/2019 F.R.SIDDIQUEE 184 Fat Properties…. • Oxidative rancidity: the oxidation takes place at the unsaturated linkage (double bond). The addition of oxygen to the unsaturated linkage results in the formation of peroxide which on decomposition, yields aldehydes and ketones having pronounced off-odour. • For Protection against rancidity: • Air tight seal container to exclude oxygen and use refrigerated storage. • Use of permitted antioxidants BHA (butylated hydroxy anisole), BHT (butylated hydroxy toluene), vitamins C and E. • Hydrogenation (saturate some points of unsaturation) 1/29/2019 F.R.SIDDIQUEE 185 Hydrogenation • A chemical process in which hydrogen molecules are added to unsaturated fats to reduce the number of double bonds. • Advantages: • 1. Protects against oxidation prolong shelf-life. • 2. Alters texture of foods by making liquid vegetable oils more solid. e.g., partially hydrogenated vegetable oils become spreadable margarine. • Disadvantages: • 1. health advantage of PUFA are lost • 2. Some left over unsaturated fatty acids after hydrogenation change from cis to trans form. • These trans-fatty acids behave more like saturated fatty acids and affect health adversely. 1/29/2019 F.R.SIDDIQUEE 186 1/29/2019 F.R.SIDDIQUEE 187 1/29/2019 F.R.SIDDIQUEE 188 Phospholipids • It is similar to a triglyceride but having a phosphate group (phosphorus-containing) and alcohol (nitrogen-containing) in place of one of the fatty acids. • Fatty acids make phospholipids soluble in fats, but phosphate allows them to dissolve in water. • Phospholipids are part of our cell membrane. • Found naturally in foods. The best known phospholipid is lecithin. • Eggs, liver, soybeans, wheat germ and nuts (almond) are rich sources of lecithin. 1/29/2019 F.R.SIDDIQUEE 189 Phospholipid (Lecithin) 1/29/2019 F.R.SIDDIQUEE 190 Phospholipids Phospholipids possess one hydrophilic polar “head” group and usually two hydrophobic nonpolar “tails”. For this reason phospholipids are amphiphathic. 1/29/2019 Lipid Bilayer F.R.SIDDIQUEE 191 Role of Phospholipids • used in food industry as emulsifiers. • As a part of cell membranes, allows vitamins and hormones to pass thru. • Also keep fats suspended in blood and body fluids. • Lecithin protects against fatty liver development. • But large dosages cause GI distress, sweating, salivation and loss of appetite. • Liver makes enough of lecithin as required. 1/29/2019 F.R.SIDDIQUEE 192 Classification of Phospholipids Classified into 3 groups: – Phosphoglycerides (Glycerophospholipid) – Phosphoinositides – Phosphosphingosides Phosphoglycerides: Glycerol, 2 fatty acids, phosphate + another group. In most phosphoglycerides, Pi is in turn esterified to OH of a polar head group (X): e.g., serine, choline, ethanolamine, glycerol, or inositol. Glycerol Fatty Acid O O R1 Fatty Acid C H2C O O CH H2C C R2 O O P O X O Phosphate 1/29/2019 X glycerophospholipid The 2 fatty acids tend to be non-identical. They may differ in length and/or the F.R.SIDDIQUEE presence/absence of double bonds. 193 Phosphoglycerides (Glycerophospholipid)… 1. Lecithin (Phosphatidyl Choline): nitrogenous base is choline Partial hydrolysis of lecithins by lecithinase ( (active principle found in snake venoms) cause removal of one fatty acid and yield lysolecithins (lysophosphatidylcholine). Result of snake bite, lysolecithins cause rapid rupture (hemolysis) of RBC. 2. Cephalin: Two types: • Phosphatidyl ethanolamine: nitogenous base is ethanolamine • Phosphatidyl serine: nitogenous base is serine. 1/29/2019 F.R.SIDDIQUEE 194 Classification of Phospholipids…. • 3. Plasmalogens (Phosphoglyceracetats): Position one FA of TG is replaced by ether or vinyl ether. • Constitute about 10% of the PL of brain and muscle • Phosphoinositides (Phosphatidyl inositols) • With inositol as polar head group. • Monophosphoinositide • Diphosphoinositide • Triphosphoinositide O O R1 C H2C O O CH H2C C R2 O O P O O H OH OH H OH phosphatidylinositol 1/29/2019 F.R.SIDDIQUEE OH H H H H OH 195 Classification of Phospholipids…. • Phosphosphingosides (Sphingomyelins) • Has a phosphocholine or phosphethanolamine head group. • Commonly found in nerve tissue especially in the myelin sheath of the nerve. • Sphingomyelins are common constituent of plasma membranes CH3 H3C + N O H2 C H2 C O CH3 P O phosphocholine H2C sphingosine Sphingomyelin 1/29/2019 O OH H2C OH H C CH NH CH O C fatty acid R OH H C CH H3N+ CH HC HC (CH2 )12 (CH2 )12 sphingosine CH3 CH3 F.R.SIDDIQUEE 196 Classification of Phospholipids…. Glycolipids (Cerebrosides): contain carbohydrates. The amino group of sphingosine can form an amide bond with a fatty acid carboxyl, to yield a ceramide. In the more complex sphingolipids, a polar “head group" is esterified to the terminal hydroxyl of the sphingosine moiety of the ceramide called Cerebrosides (a monosaccharide such as glucose or galactose attached to the C1 -OH of ceramide. OH H2C CH2OH OH H C NH O OH H OH CH CH H H H O C OH O H H2C OH ceramide 1/29/2019 CH NH CH HC O R H C (CH2 )12 CH3 cerebroside with -galactose head group F.R.SIDDIQUEE C R HC (CH2 )12 CH3 197 Classification of Phospholipids…. Gangliosides: a type of glycolipid A ganglioside is a ceramide with a polar head group that is a complex oligosaccharide, including the acidic sugar derivative sialic acid. Gangliosides have an oligosaccharide attached to the C1 -OH of ceramide. • More than 15 different gangliosides have been characterised and their structures determined. • Cerebrosides and gangliosides are found in the brain and nervous tissue. Cerebrosides and gangliosides, collectively called glycosphingolipids, are commonly found in the outer leaflet of the plasma membrane bilayer, with their sugar chains extending out from the cell surface. 1/29/2019 F.R.SIDDIQUEE 198 Niemann-Pick Disease • Accumulation (stored) of large quantities of sphingomyelins in the brain caused a syndrome called Niemann-Pick disease. Niemann-Pick disease is a rare genetic disorder, inherited as an autosomal recessive condition. The disease is caused by deficiency of sphingomyelinase, which cleaves ceramide-phosphocholine bond of sphingomyelin. 1/29/2019 F.R.SIDDIQUEE 199 Gaucher Disease • Gaucher disease is inherited (passed from parent to child). • Both parents must be either carriers or have the disease for the disease to present in a child. Hereditary syndrome, not so rare. • Disease due to deficiency of enzyme glucosyl ceramide hydrolase (glucocerebrosidase). • Body cannot process glucocerebroside, thus accumulates in the body. • In Gaucher disease, the glucocerebrosides appear in relatively large amount in the liver and spleen. • More common than Tay-Sachs. 1/29/2019 F.R.SIDDIQUEE 200 Tay-Sachs Disease • The classical form of Tay-Sachs disease (TSD) is a fatal, recessive genetic disorder in children that causes progressive destruction of the central nervous system. • Oldest medically describe lipid storage genetic disease due to deficiency of enzyme N-acetylgalactosaminidase, which cleaves a specific bond ( β14) between an N-acetyl-D-galactosamine and a D-galactose residue in GM2 ganglioside. • In effect, GM2 is not degraded to GM1. • With the result, GM2, which is also called as Tay-Sachs gangliosides, is accumulated in large amounts in brain cells causing degeneration of the nervous system. • 100-300 times the normal GM2 content. 1/29/2019 F.R.SIDDIQUEE 201 Lipid Storage Diseases 1/29/2019 F.R.SIDDIQUEE 202 Sterols • Sterols: compounds with multiple-ring structure. The most important sterol is cholesterol. • Many important body compounds are sterols e.g., bile acids, sex hormones (such as testosterone), adrenal hormones (such as cortisol), and vitamin D, as well as cholesterol itself. 1/29/2019 F.R.SIDDIQUEE 203 Cholesterol • Only foods derived from animals have cholesterol in it, e.g., meats, eggs, fish, poultry, and dairy products. • Foods of plant origin don’t contain cholesterol but only plant sterols e.g., phytosterols. • More than 90% of all the body’s cholesterol resides in the cells. • Liver makes about 800 to 1500 mg of cholesterol per day. • If cholesterol deposits in the artery walls, these deposits lead to a disease known as atherosclerosis, which causes heart attacks and stroke. • Daily, the GI tract receives 50 to 100 g triglycerides, 4 to 8 g of phospholipids and 300 to 450 mg of cholesterol. 1/29/2019 F.R.SIDDIQUEE 204 Lipid Transport • The transport vehicle for fats are known as lipoproteins. • Lipoproteins move the fatty materials through the watery blood stream. • The body makes four main types of lipoproteins, they are clusters of lipids and proteins, and are distinguished by size, density, and amounts of proteins and lipids • more lipids lower density • more proteins higher density • Lipoproteins • Chylomicrons • VLDL = very-low-density lipoproteins • LDL = low-density lipoproteins • HDL = high-density lipoproteins 1/29/2019 F.R.SIDDIQUEE 205 Lipid Transport…. • • • • Chylomicrons: largest and least dense of lipoproteins. They transport diet-derived lipids (mostly TG) from the intestine to the rest of the body. Very Low Density Lipoprotein (VLDL): the type of lipoproteins made primarily by liver cells to transport lipids to other parts (various tissues) of the body, contains mainly triglycerides. Low-Density Lipoprotein (LDL): cholesterol-rich lipoprotein, derived from VLDL as cells remove TG from them, thus leaving behind mainly the cholesterol. Known as bad cholesterol. Carries cholesterol from the liver to body tissues. High-Density Lipoprotein (HDL): the liver makes HDL to carries cholesterol from the cells (tissues) back to the liver for recycling or disposal, known as good cholesterol. 1/29/2019 F.R.SIDDIQUEE 206 Health Implications • The blood cholesterol linked to heart disease is LDL cholesterol. HDL also carry cholesterol, but elevated HDL represent cholesterol returning from the rest of the body to the liver for breakdown and excretion. • Point to remember: • High LDL cholesterol is associated with a high risk of heart attack (less healthy), whereas high HDL cholesterol seems to have a protective effect (healthy). • Keep in mind that the cholesterol itself is the same, and that the differences between LDL and HDL reflect the proportions and types of lipids and proteins within them – not the type of cholesterol. 1/29/2019 F.R.SIDDIQUEE 207 Factors that lower LDL or raise HDL • Weight control • Monounsaturated or polyunsaturated, instead of saturated, fat in the diet • Soluble fibers • Phytochemicals • Moderate alcohol consumption • Physical activity 1/29/2019 F.R.SIDDIQUEE 208 Essential Fatty Acids (EFAs) • Fatty acids that are essential to human health but cannot be made by the body. They must therefore be supplied by the diet. • Out of all the fatty acids, only two are not made by the body. • All EFAs are unsaturated and must be provided from external food sources, e.g., fish, vegetable oils, seeds, nuts. • EFAs should make up at least 3% of energy intake per day and most diets meet this minimum requirement adequately. • Linoleic Acid: 18 carbons, two double bonds, Omega-6 fatty acids vegetable oils (corn, sunflower, safflower, soybean, cotton seed), poultry meat. • Linolenic Acid: 18 carbons, three double bonds, Omega-3 fatty acids - Oils (flax seed, walnut, soybean, canola, wheat germ), nuts and seeds (butternuts, walnuts, soybean kernels), vegetables (soybeans). 1/29/2019 F.R.SIDDIQUEE 209 Essential Fatty Acids 1/29/2019 F.R.SIDDIQUEE 210 Lipid Metabolism • Storing fat as fat: Fat provides more than twice the energy of carbohydrate and protein. It is an efficient storage form of energy. • The fat cells of the adipose tissue has unlimited capacity to store fat by capturing triglycerides from lipoproteins as they pass by after meals. • An enzyme – lipoprotein lipase (LPL) - hydrolyzes the triglycerides to glycerol, fatty acids and monoglycerides, and pass them on to the cells. In the cells, other enzymes reassemble the pieces into triglycerides again for storage. • Making fat from carbohydrate or Protein: Glucose can be converted to fat but requires more energy. • Enzymes break down glucose into 2-carbon fragments which are then combined to make long-chain fatty acids. • Some amino acids can also be converted to fat. 1/29/2019 F.R.SIDDIQUEE 211 Lipid Metabolism…. • Making fat from fat: Little energy is required to convert fat from diet into fat for storage than to make fat from carbohydrates and proteins. • The body therefore prefers to make fat from dietary fat. • Therefore food fat is the source of most of the fat stored in the body. • Using fat for energy: • An enzyme (hormone-sensitive lipase) in the cells of the adipose tissue dismantle stored triglycerides to release glycerol and fatty acids directly into the blood. • Other cells in the body that require energy then capture the glycerol and fatty acids and break them down to yield energy, carbon dioxide, water. 1/29/2019 F.R.SIDDIQUEE and 212 Blood Lipid Profile • Hearing a physician say, “Your blood lipid profile looks fine”, is reassuring. • Reveals the concentration of various lipids in the blood, notably triglycerides and cholesterol, and their lipoprotein carriers (VLDL, LDL, and HDL). • This information alerts people to their disease risks and their need to change eating habits. • Desirable blood lipid profile: • Total cholesterol: <200 mg/dl • LDL cholesterol: <100 mg/dl • HDL cholesterol: ≥60 mg/dl • Triglycerides: <150 mg/dl 1/29/2019 F.R.SIDDIQUEE 213 Health Effects of Lipids • Heart Disease • Elevated blood cholesterol is major risk factor for cardiovascular disease. • It deposits in arteries, raising blood pressure and thus reducing supply of blood to heart and other tissues. • Higher the cholesterol, the earlier and more likely the tragedy. • What most people don’t realize that food cholesterol does not raise blood cholesterol as dramatically as saturated fat does. 1/29/2019 F.R.SIDDIQUEE 214 Health Effects of Lipids…. • Risks from Saturated fat • Fats rich in lauric, myristic, and palmitic fatty acids raise LDL cholesterol. • Stearic acid does not raise LDL cholesterol but increases the risk of heart diseases. • Sources red meats, high-fat milk products, and chocolate. • Risks from trans fats • trans fats increase blood LDL just like saturated fats and lower HDL. • Sources animal origin foods, hydrogenated shortenings, deepfried foods. 1/29/2019 F.R.SIDDIQUEE 215 Health Effects of Lipids…. • Risks from Cholesterol • Dietary cholesterol (egg, milk products, meat, poultry, shellfish) has also been implicated in raising blood cholesterol and increasing the risk of heart disease, although its effect is not as strong as that of saturated fat or trans fat. • Limiting saturated fat is more effective than limiting cholesterol intake. • Benefits from Monounsaturated and Polyunsaturated Fats • MUFA (olive oil and canola oil) and PUFA (vegetable oils: safflower, soy, corn, sunflower, etc.) decreases the risk for heart disease. 1/29/2019 F.R.SIDDIQUEE 216 Health Effects of Lipids…. • A diet that uses olive oil instead of other cooking fats, especially butter, stick margarine, and meat fats, may offer numerous health benefits. Olive oil helps to protect against heart disease by: • Lowering total and LDL cholesterol and not lowering HDL cholesterol or raising triglycerides. • Lowering LDL cholesterol susceptibility to oxidation. • Lowering blood clotting factors. • Providing phytochemicals that act as antioxidants. • Lowering blood pressure. Olive oil is not a magic portion; like other fats they delivers 9 kcal, which can contribute to weight gain in people who fail to balance their energy intake with their energy output. Its role in a healthy diet is to replace the saturated fats. Other vegetable oils, such as canola or safflower oil are also generally low in saturated fats and high in unsaturated fats. 1/29/2019 F.R.SIDDIQUEE 217 Health Effects of Lipids…. • Benefits from Omega-3 Polyunsaturated Fats • Lowers blood cholesterol and heart disease. • Fish and marine foods are good sources of eicosapentaenoic acid (EPA C20:5, omega-3 family) and docosahexaenoic acid (DHA C22:5,omega-3 family) fatty acids. • People who eat once a week can lower their blood cholesterol and their risk of heart disease and stroke. • Diets low in both fat and saturated fat, combined with fish consumption improves person’s lipid profile, prevents blood clots, lower blood pressure. • The native peoples of Alaska, northern Canada, and Greenland, who eat a diet rich in omega-3 fatty acids, notably EPA and DHA, have a remarkably low rate of heart disease even though their diets are relatively high in fat. 1/29/2019 F.R.SIDDIQUEE 218 Health Effects of Lipids…. • Cancer • Total fat intake and risk of type of cancer are related e.g., prostate cancer and fat intake. • The association between cancer and fat appears to be due primarily to saturated fats or dietary fat from meats. • Dietary fat seems not to initiate cancer development but to promote cancer once it has arisen. • Obesity • Higher fat intake contributes to obesity. • Other risk factors for cancer include smoking, alcohol, and environmental contaminants. 1/29/2019 F.R.SIDDIQUEE 219 Fats give foods their flavor, texture and palatability, in addition to carrying fatsoluble vitamins, so some fat in the diet is essential for good health, but too much fat, especially saturated fat, increases risks for chronic diseases. 1/29/2019 F.R.SIDDIQUEE 220 Recommended Intakes of Fat • No RDA or upper limit has been set for fat. • Reduce total fat (saturated fat, trans fat, and cholesterol) to 20 to 35% of daily energy intake. • Part of this fat should be from essential fatty acids; • Linoleic acid: 5-10% and linolenic acid: 0.6-1.2% of daily energy intake. • Reduce saturated fat and trans fat to less than 10% of energy intake. • Reduce cholesterol intake to less than 300 mg daily. An egg contains 200 mg of cholesterol, all of it in the yolk. • Balance omega-3 and omega-6 intakes (1:6). Omega-3: 0.55 g per 1000 kcal, Omega-6: 3.3 g per 1000 kcal. So eat more fish and less red meat. 1/29/2019 F.R.SIDDIQUEE 221 Recommended Intakes of Fat…. • • • • • • • • • • DRI for fat: 20 to 35% of energy intake. Linoleic acid AI: 5 to 10% of energy intake. Linolenic acid AI: 0.6 to 1.2% of energy intake. Daily Values: 65 g fat (based on 30% of 2000 kcal diet). 20 g saturated fat (based on 10% of 2000 kcal diet. 300 mg cholesterol 1/29/2019 F.R.SIDDIQUEE 222 Other Recommendation Use lean meat and nonfat milk. Eat plenty of vegetables, fruits, and grains Use fat and oils sparingly. Look for invisible fat. Invisible fat in meats, chips, fries, cookies, crackers, biscuits, cakes, chocolates. Keep invisible fat in mind when making selection of food. • Choose your food wisely. • Always read food labels • • • • 1/29/2019 F.R.SIDDIQUEE 223 Some Brain Storming Question/Answer Q1. What dietary factors have the greatest impact on blood cholesterol? Ans: Many factors—including genetic inheritance, body weight, and baseline blood lipids—influence the extent to which plasma cholesterol levels respond to dietary changes. Thus, the relationship between diet and blood lipids is highly individual. • In general, research demonstrates that dietary saturated fat and trans-fat have the greatest impact on the lipid profile. • Saturated fat intake increases total- and LDL-cholesterol levels. Saturated fat intake raises serum cholesterol levels substantially, dietary cholesterol has only a limited effect. • Intake of trans-fat appears particularly harmful since it raises LDL-cholesterol while lowering HDL-cholesterol levels 1. • Studies shows that a 50 mg change in dietary cholesterol was associated with a 1 mg/dl change in both plasma total and LDL cholesterol levels, they indicated that replacing just 1% of calories from saturated fats with polyunsaturated fats would be expected to decrease plasma total and LDL-cholesterol levels by 3.0 mg/dl and 2.2 mg/dl, respectively • Therefore, limiting dietary saturated fat and trans-fat appears more effective in improving lipid profiles than reducing dietary cholesterol. 1/29/2019 F.R.SIDDIQUEE 224 Question/Answer… Q2. What is the influence of dietary cholesterol on plasma cholesterol levels? Ans: Dietary cholesterol, once thought to play a primary role in determining plasma cholesterol levels, is now understood to have a negligible effect on blood lipids in most healthy people. • On average, increasing one’s intake of dietary cholesterol by 100 mg/day results in a 2.3 mg/dl increase in total cholesterol, a 1.9 mg/dl increase in LDL-cholesterol, and a 0.4 mg/dl increase in HDL cholesterol. • Because HDL cholesterol increases with dietary cholesterol intake, the LDL:HDL ratio remains virtually unchanged. Q3. What role does genetic inheritance play in regulating blood cholesterol? Ans: Physiological responses to changes in dietary cholesterol are heavily influenced by genetic predisposition. • For example, individuals with certain genetic variants of apolipoprotein E tend to have a heightened sensitivity to dietary cholesterol (meaning that their blood cholesterol levels are prone to rise more than average in response to cholesterol in the diet. An estimated 15-20 percent of the population falls into this category.) • Even in these cholesterol-sensitive (hyper-responsive) individuals, the effect of cholesterol intake is minimal. • On average, cholesterol sensitive individuals exhibit a 3.9 mg/dl change in plasma total cholesterol in response to an increase or decrease of 100 mg of cholesterol/day, while those with normal sensitivity experience an average change of 1.4 mg/dl. 1/29/2019 F.R.SIDDIQUEE 225 Question/Answer… Q4. What is the impact of egg intake on plasma lipids? Ans: Many cholesterol-containing foods are also naturally high in saturated fat. Eggs are one of the rare exceptions. While they are high in cholesterol, eggs contain very little saturated fat (one Large egg contains only 1.5 grams) and are low in calories (only 75 calories per Large egg). • Egg consumption has been shown in several clinical trials to have only a minimal effect on blood lipids. In one such trial, when 640 mg of cholesterol from eggs was added to the daily diets of 91 healthy men and women, the additional cholesterol had no effect on blood cholesterol levels or LDL atherogenicity in hyporesponsive individuals. • In hyperresponsive participants (those who experienced >2.5 mg/dL increase in plasma cholesterol for every additional 100 mg of dietary cholesterol), as LDLcholesterol levels rose, the LDL subclass pattern shifted toward a larger, lessatherogenic particle type. • These findings led the study authors to conclude that limitations on egg intake may not be necessary for healthy person and that egg consumption does not increase the atherogenicity of LDL particles. • Studies have consistently indicated that there is no relationship between egg intake and plasma cholesterol levels or CHD risk. 1/29/2019 F.R.SIDDIQUEE 226 Question/Answer… Q5. Does egg intake increase the risk for heart disease? Ans: A number of these studies indicate that there is no relationship between egg consumption and CHD risk, they found that those who ate one egg per week had the same relative risk for CHD as did those who ate an egg a day. • These findings suggest that consumption of up to 1 egg per day is unlikely to have substantial overall impact on the risk of CHD or stroke among healthy men and women. • In fact, the countries with the highest per capita egg consumption (Japan, Mexico, France, and Spain) had the lowest rates of CHD mortality, indicating that egg consumption does not contribute to the development of CHD. Q6. How many eggs should my patients eat in a week? Ans: Although no official recommendation exists for egg intake, research suggests that heart disease risk does not increase in healthy adults consuming up to 7 eggs per week. • Because physiologic responses to dietary cholesterol are highly individual, making specific recommendations for egg intake for the general population would be impractical, at best. • This question is best addressed by an individual’s physician and/or dietitian, who can take into account individual lifestyle factors such as age, weight, physical activity, gender, family history, and typical eating habits before making recommendations regarding dietary intake. 1/29/2019 F.R.SIDDIQUEE 227 Question/Answer… Q. If olive oil is high in fat, why is it considered healthy? Ans: The main type of fat found in all kinds of olive oil is monounsaturated fatty acids (MUFAs). MUFAs are actually considered a healthy dietary fat. If your diet emphasizes unsaturated fats, such as MUFAs and polyunsaturated fats (PUFAs), instead of saturated fats and trans fats, you may gain certain health benefits. • MUFAs and PUFAs may help lower your risk of heart disease by improving related risk factors. For instance, MUFAs may lower your total cholesterol and low-density lipoprotein cholesterol levels. MUFAs may also help normalize blood clotting. And some research shows that MUFAs may also benefit insulin levels and blood sugar control, which can be especially helpful if you have type 2 diabetes. • But even healthier fats like olive oil are high in calories, so use them only in moderation. Choose MUFA-rich foods such as olive oil instead of other fatty foods — particularly butter and stick margarine — not in addition to them. And remember that you can't make unhealthy foods healthier simply by adding olive oil to them. 1/29/2019 F.R.SIDDIQUEE 228 Recommended Books • Understanding Nutrition. By Ellie Whitney and Sharon Rady Rolfes. 3rd Edition, Thomson Wadsworth, USA, 2005. • Nutrition: Concepts and Controversies. By Frances Sizer and Ellie Whitney. 10th Edition, Thomson Wadsworth, USA, 2005. • Discovering Nutrition. By Paul Insel, R. Elaine Turner and Don Ross. 2nd Edition, American Dietetic Association, Jones and Bartlett Publishers, Inc. USA, 2006. 1/29/2019 F.R.SIDDIQUEE 229 Energy Metabolism BMB 408: Human Nutrition Yearul Kabir, Ph.D. Handout # 5 Energy Metabolism Human beings requires enough energy to lead an active and healthy life. Energy fulfils the following functions: - Maintenance of basal body functions (basal metabolism) - Physical activity - Growth and development in infants and children and maintenance of pregnancy and lactation in women. • An adequate and constant amount of energy must be made available to the body for cell survival and maintaining the following vital functions at optimal levels. • Activity of the brain and the nervous system • Pumping of heart and distribution of blood to supply oxygen and nutrients • Liver function •1/29/2019 Excretory function of the kidneyF.R.SIDDIQUEE 231 Energy Balance • The balance between how much energy is consumed and how much is expended. • Positive balance is when intake exceeds expenditure and is associated with increases in body energy stores (weight gain). • During negative balance, as in periods of starvation, body energy stores are depleted. 1/29/2019 F.R.SIDDIQUEE 232 Components of energy balance • Energy intake • The caloric or energy content of food as provided by the major sources of dietary energy: carbohydrate, protein, fat and alcohol. • Energy storage • The energy that is consumed in the form of food or drinks can either be stored in the body in the form of fat (the major energy store), glycogen (short-term energy/carbohydrate reserves) or protein (rarely used by the body for energy) or be used by the body to fuel energy-requiring events. • Energy expenditure • The energy that is required by the body for metabolic, cellular and mechanical work. 1/29/2019 F.R.SIDDIQUEE 233 Measurement of Energy Expenditure • Calorimetry is the measurement of the body’s energy expenditure • Direct Calorimetry • Direct calorimeters have been designed for measuring total heat production in the body, • but this approach is technically demanding, especially in human studies, and is now infrequently used. • Indirect calorimetry measures energy production via respiratory gas analysis. • This approach is based on measuring oxygen consumption and carbon dioxide production that occurs during the combustion (or oxidation) of protein, carbohydrate, fat and alcohol, as shown in the example of glucose combustion. • Estimations of energy expenditure by indirect calorimetry have been shown to be practically identical to those derived from direct calorimetry. 1/29/2019 F.R.SIDDIQUEE 234 Bomb calorimeter 1/29/2019 F.R.SIDDIQUEE 235 1/29/2019 F.R.SIDDIQUEE 236 The Respiratory Quotient • Substances such as carbohydrates and fats, yield approximately the same amount of heat when oxidized in the body as when oxidized in a laboratory bomb calorimeter. • When foods are oxidized in the body, carbon dioxide, water, and heat are produced in direct proportion to the quantity of oxygen consumed in the process. • The proportion of CO2 produced to O2 consumed can furnish information as to the kind and quantity of food which is being metabolized. • The ratio of the volume of CO2 eliminated by the lungs to the volume of O2 consumed by the body is termed the respiratory quotient (RQ). 1/29/2019 F.R.SIDDIQUEE 237 The Respiratory Quotient… • When carbohydrates are oxidized, the reaction may be represented as: C6H12O6 + 6O2 6CO2 + 6H2O + 675 kcal (approx.) • Here RQ = 6 vol CO2/6 vol O2 = 1.0 • Fat contain less oxygen in their molecules than carbohydrates and thus require more oxygen from the atmosphere for complete oxidation: • 2 C51H98O6 + 145 O2 Tripalmitin 102 CO2 + 98 H2O + 15,314 kcal • Here RQ = 51 vol CO2/ 72.5 vol O2 = 0.7 • The RQ for proteins is derived indirectly since its oxidation in the body cannot be represented accurately by a chemical equation. When protein alone is metabolized, the RQ is 0.8. • Determining the RQ of an individual at any one time, it indicates the type of oxidative metabolism which takes place. 1/29/2019 F.R.SIDDIQUEE 238 The Respiratory Quotient… • When carbohydrates alone are burned, an RQ of 1.0 is obtained. • The lowest obtainable RQ under normal conditions is 0.71, representing the oxidative metabolism of fats only. • RQ intermediate between these figures indicates the combustion of a mixture of foodstuffs. • Normally, when a mixed diet is metabolized, the RQ is about 0.85. • Under abnormal conditions, the limits of 0.71 and 1.0 may be exceeded in both direction. • In uncontrolled diabetes the RQ will be close to 0.7, indicating that much of the combustion is derived from fats. (Normal utilization of carbohydrates would shift the RQ closer to 1.0). 1/29/2019 F.R.SIDDIQUEE 239 The Respiratory Quotient… • In severe uncontrolled diabetes, RQ as low as 0.63 have been reported. This indicates that some of the absorbed oxygen was not used for the production of CO2 and H2O and reflects the conversion of amino acids to glucose (for which oxygen is needed, since the glucose molecule contains more oxygen than the amino acid molecules) and the subsequent excretion and loss of this glucose in the diabetic’s urine. • One of the most striking results of insulin treatment is that the RQ increases, showing that carbohydrates are again being utilized for energy purposes. • RQ higher than 1.0 may be found in conditions where excessive amounts of carbohydrates are utilized, to the practical exclusion of fats and proteins, and where glucose is converted into fat and deposited as such in the body. • In this case a substance rich in oxygen is converted into one containing less, with a net release of oxygen which is available for the metabolic needs of the body 1/29/2019 F.R.SIDDIQUEE 240 without inhalation. The Respiratory Quotient… • In clinical practice, an RQ < 0.8 suggests that a patient may be underfed and an RQ < 0.7 suggests starvation or ingestion of a low-carbohydrate or high-alcohol diet, whereas an RQ > 1.0 suggests that lipogenesis is occurring. • The protein portion of the metabolized food may be computed from urinary nitrogen by assuming that each gram of nitrogen represents 6.25 g of original protein. • The oxidation of this quantity of protein requires the consumption of 5.92 liters of O2 and liberates 4.75 liters of CO2. From these figures one can compute the volume of these gases involved in the metabolism of protein alone. • Subtracting these figures from the total CO2 exhaled and oxygen absorbed yields the RQ for the fat and carbohydrate metabolism. • Once the amount of O2 consumed and of CO2 and N2 eliminated has been determined in the metabolic laboratory, it is thus possible to compute, for any given period, the exact amounts of carbohydrate, fat, and protein which were metabolized. 1/29/2019 F.R.SIDDIQUEE 241 Calculation of Energy Expenditure from RQ • Once the RQ has been computed from gaseous exchange, the calculation of energy expended is rather simple. Table below gives the caloric value for 1 L of O2 and for 1 L of CO2 given various RQs. • When the amount of O2 and/or CO2 in the exchange has been determined, the total caloric value represented by the exchange can be calculated. It is also possible to determine the amount of carbohydrate and fat being oxidized in the production of these calories. 1/29/2019 F.R.SIDDIQUEE 242 Energy Expenditure from RQ…. • For example, if under standard conditions for the determination of BMR a person consumed 15.7 L O2/hr and expired 12.0 L CO2, the RQ would be 12.0/15.7 = 0.7643. • From Table, the caloric equivalent for an RQ of 0.76 is 4.751 for 1 L O2 or 6.253 for 1 L CO2. Based on the caloric equivalent for O2, calories produced/hr are 15.7 x 4.751 = 74.59. Based on the caloric equivalent for CO2, calories produced/hr are 12.0 x 6.253 = 75.04. • If we then use 75 kcal/hr as the caloric expenditure, then under basal conditions the BMR for the day would be approx. 1,800 kcal (75 kcal/h x 24). At this RQ of 0.76, fat is supplying almost 81% of energy expended (Table). • Because under ordinary circumstances the contribution of protein to energy metabolism so small, the oxidation of protein is ignored the determination of the so-called RQ. 1/29/2019 F.R.SIDDIQUEE is in nonprotein 243 Measurement of Energy by Indirect calorimetry 1/29/2019 F.R.SIDDIQUEE 244 Total Energy Expenditure or Utilization • has three components: • BMR: energy expenditure at complete rest and without physical work. • Physical activity: for mechanical work. • Specific dynamic action or Thermogenic component: energy expenditure due to the physiological response following the ingestion of food, and exposure to cold or stimulants. 1/29/2019 F.R.SIDDIQUEE 245 Components of Energy Expenditure 1/29/2019 F.R.SIDDIQUEE 246 Energy Expenditure at Rest • Resting energy expenditure or basal energy expenditure: The minimum energy needed to maintain basic physiological functions. • The rate of energy expenditure at rest (kcal/hour) is measured as either the resting metabolic rate (RMR) or the basal metabolic rate (BMR). • BMR: the minimum level of energy expended by the body to sustain life in the awake state. – 12 to 18 hours after the ingestion of food – at complete rest, at a comfortable temperature – restful state of mind Under these basal conditions the energy output of the body is relatively constant and low. • BMR and RMR are almost same, except that RMR includes energy required for digestion, absorption, and distribution of ingested food (e.g., determinations are made in a nonfasting state). They are virtually interchangeable. 1/29/2019 F.R.SIDDIQUEE 247 1/29/2019 F.R.SIDDIQUEE 248 1/29/2019 F.R.SIDDIQUEE 249 Measurement of Basal Metabolic Rate (BMR) • BMR is defined as the number of calories given off by the body per square meter of body surface per hour. • The average BMR for normal adult males varies from 36 to 41 cal/m2/hr and for normal adult females, from 34 to 36 cal. • Any deviation of the individual BMR from the normal is expressed in terms of percent. For instance, if the BMR of a 40 year old male is found to be 43.7 cal/m2/hr, while the mean normal BMR for this age is 38.0, his BMR is said to be plus 15 percent. • In hyperthyroidism, the BMR is increased to +75% or more. In hypothyrodism, this is reduced to - 40%. Variations between -10% to +15% are considered within physiological range and hence normal. The BMR is also increased in Cushing’s syndrome and acromegaly (hyperfunction of adrenal cortex and anterior pituitary) and decreased in Addison’s disease (hypofunction of adrenal cortex). 1/29/2019 F.R.SIDDIQUEE 250 Basal Metabolic Rate (BMR)… • Apart from its use as a diagnostic aid, knowledge of BMR is essential in the calculation of calorie requirements and planning of nutrition for individuals as well as large communities & populations. • For the practical determination of the BMR a number of apparatuses have been developed. The simplest type (McKesson, Sanborn, or Benedict-Roth) measures the oxygen consumption of the individual while he is in the basal state. • BMR is calculated from oxygen consumption measured over a 6- to 12-minute period when the subject is in a post-absorptive state (after a 12 h fast) and rested quietly (physically and mentally) during the previous 30 minutes in a thermally neutral environment (room temperature). • Under the conditions of the experiment, each liter of oxygen consumed represents 4.8 kcal of heat generated by the body. 1/29/2019 F.R.SIDDIQUEE 251 Basal Metabolic Rate (BMR)… • Determined from the consumption of oxygen and excretion of carbon dioxide and urinary nitrogen, or from the heat production of the animal. Body size is a major factor in TEE and hence BMR. • BMR is calculated using the body weight in kg/surface area in meters. • The use of surface area of the body enables comparison of measurements of BMR in individuals of different size. • The surface area is calculated from height and weight using monograms (DuBois height-weight chart). • BMR is more closely related to lean body mass than to surface area. • The surface area of the individual can be determined from weight and height data according to the formula of DuBois: Area (cm2) = weight (kg)0.425 x height (cm)0.725 x 71.84 F.R.SIDDIQUEE 1/29/2019 252 Basal Metabolic Rate (BMR)… • Given the oxygen consumption during specific time and the height-weight data, the individual’s BMR can thus be obtained in terms of calories generated per square meter of body surface per hour. • The BMR is subject to variation by a number of physiological and pathological conditions. • A simple approach to calculate BMR is to use values of 1.0 and 0.9 kcal/hr/kg body weight for men and women, respectively. When calculated over 24 hr, this results in values of 1680 and 1173 kcal for an average 70 kg man or 58 kg woman, respectively. • More accurate values are obtained with the formulas. 1/29/2019 F.R.SIDDIQUEE 253 1/29/2019 F.R.SIDDIQUEE 254 Equations for estimated BMR from body weight • can be measured directly by indirect calorimetry, or can be calculated from the predicted equations (Table). • Age range (yr) • Men Under 3 • Prediction equation BMR (MJ/day) = [0.249 X weight (kg)] – 0.127 3-10 BMR (MJ/day) = [0.095 X weight 10-17 BMR (MJ/day) = [0.074 X weight 18-29 BMR (MJ/day) = [0.063 X weight (kg)] + 2.110 • (kg)] + 2.754 • (kg)] + 2.896 • Women Under 3 BMR (MJ/day) = [0.244 X weight (kg)] – 0.130 • 3-10 BMR (MJ/day) = [0.085 X weight (kg)] + 2.033 • 10-17 • BMR (MJ/day) = [0.056 X weight (kg)] + 2.898 18-29 BMR (MJ/day) = [0.062 X weight (kg)] + 2.036 • *I kcal = 4.184 kj, or 1 kj = 0.239 kcal 1/29/2019 F.R.SIDDIQUEE 255 Energy Expenditure for physical Activity • Once BMR has been measured or predicted, it is necessary to add on the energy required for physical activity and other thermogenic processes. • The energy cost of physical activity can also be measured directly by indirect calorimetry, although to do this for all the major activities of each subject is a painstaking task; the alternative is to estimate the energy cost of each activity from tables. • Physical activity is more than just exercise and sport. • It includes work, leisure activities, and other everyday activities. • The energy cost of an activity depends on its type, duration, and intensity. • Body size affects energy cost, too – a large person expends more calories per minute than a smaller person doing the same activity. 1/29/2019 F.R.SIDDIQUEE 256 • • • • • • • • • Estimates of the energy costs of selected activities. All values are expressed as a multiple of BMR. Activity Men Women Sitting 1.2 1.2 Standing 1.4 1.5 Walking 3.2 3.4 (normal pace) Each activity applied for all individuals of any body weight and any age group. If the duration of each activity is known, its energy cost can be determined from this multiple and BMR of the subject. In this way the body weight of the subject is taken into account in the estimation of energy expenditure in activity. • Studying = 1 or 2 kcal/minute 1/29/2019 F.R.SIDDIQUEE 257 1/29/2019 F.R.SIDDIQUEE 258 1/29/2019 F.R.SIDDIQUEE 259 Activity Pattern • If detailed information about the duration of different physical activities is not available, a crude estimation can be made from the knowledge of the subjects' lifestyle (Table). • • Non-occupational Occupational activity level • Light Moderate Heavy • M F M • Non-active 1.5 • Moderate active 1.8 1.6 • Very active 1.9 1.7 1/29/2019 F M F 1.4 1.4 1.6 1.7 1.5 1.5 1.5 1.6 1.6 F.R.SIDDIQUEE 1.7 1.6 1.8 1.7 260 Calculation of Energy Requirement from activity pattern • Example: Calculate the energy requirement of a male officer aged 25 yrs, weight 65 kg, predicted BMR = 6078 kj/day from activity pattern. • Activity expended Multiple of BMR Hours spent in activity • In bed kj 1.0 8 2340 • At work 1.7 6 • Discretionary • Household tasks 2970 3.0 2 1760 • Fitness training 0.33 • Remainder 7.67 • TOTAL 1/29/2019 6.0 580 1.4 3140 1.54 10,780 F.R.SIDDIQUEE 24 261 Energy Expenditure to Process Food • Our bodies expend energy to digest, absorb, and metabolize the nutrients we take in, and these process generate heat. • This energy output is collectively called the thermic effect of food (TEF) also known as diet-induced thermogenesis or the specific dynamic action of food.. • TEF peaks about one hour after eating and normally dissipates within five hours. • It is lowest for fat and highest for protein. • For a typical mixed diet, TEF accounts for approximately 10% of total energy expenditure. • Thermic effect of foods: • Carbohydrate: 5-10%; Fat: 0-5%; Protein: 20-30%. • The percentages are calculated by dividing the energy expended during digestion and absorption (above basal) by the energy content of the food. 1/29/2019 F.R.SIDDIQUEE 262 1/29/2019 F.R.SIDDIQUEE 263 Estimating Total Energy Expenditure • Resting energy expenditure (REE) : can be estimated using the following equations • For adult men: REE = weight (kg) X 1.0 kcal/kg X 24 hr • REE = weight (kg) X 1.0 X 24 • For adult women: REE = weight (kg) X 0.9 kcal/kg X 24 hr • REE = weight (kg) X 0.9 X 24 • The 1.0 and 0.9 factors for kcal/kg reflect the differences in body composition between men and women. • Man have proportionally more lean body mass and so burn more calories per kg of body weight. • This method underestimates children’s REE, and overestimates the REE of elders. 1/29/2019 F.R.SIDDIQUEE 264 Estimating Energy Expended in Physical Activity • Energy expended in physical activity can be estimated as a percentage of REE based on a person’s general activity level. % of REE Activity Level Description • 20-30% activity Sedentary • 30-40% activity Light Mostly resting with little or no Occasional unplanned (e.g., going for a stroll) • 45-65% such as brisk Moderate • 65-90% Heavy Daily planned activity, walks Daily workout routine requiring several hours of continuous exercise • 90-120% Exceptional Daily vigorous workouts for extended hours; training for competition 1/29/2019 F.R.SIDDIQUEE 265 Thermic Effect of Food (TEF) • The thermic effect of food can be estimated as roughly 10% of the sum of REE plus energy expended in physical activity. • Therefore, • Total Energy Expenditure (TEE) = REE + Physical activity + TEF 1/29/2019 F.R.SIDDIQUEE 266 How Many Calories Do a Person Burn? • Deena is a 54.5 kg adult female, has a light to moderate physical activity level. Calculate her total energy expenditure? • Step 1. Estimation of REE = weight (kg) X 0.9 X 24 • = 54.5 X 0.9 X 24 = 1,177 kcal • Step 2. Estimation of energy expenditure for • physical activity = Value from Table (%) X REE • = 0.45 X 1,177 = 530 kcal • Step 3. Estimation of • Thermic Effect of Food = 0.1 X (Energyphysical activity + REE) • = 0.1 X (530 + 1,177) = 171 kcal • Total Energy Expenditure = REE + Energyphysical activity + TEF • = 1,177 + 530 + 171 = 1,878 kcal 1/29/2019 F.R.SIDDIQUEE 267 Estimating Resting Energy Expenditure • Commonly used equations for predicting REE for healthy persons are those published by Harris and Benedict and those developed by an expert panel of the WHO. • Harris-Benedict equations’ derived the best predicted REE using the variables weight, stature, age and sex. • Because stature was not found to significantly improve the predictive ability of the equations, it was omitted from WHO equations. • Using measured energy expenditure based on the doubly labeled water technique, the National Academy of Sciences also developed a set of equations for estimating REE in healthy people. • The Harris Benedict Equation is a formula that uses your BMR and then applies an activity factor to determine your total daily energy expenditure. 1/29/2019 F.R.SIDDIQUEE 268 Harris Benedict Formula • To determine your total daily calorie needs, multiply your BMR by the appropriate activity factor, as follows: • If you are sedentary (little or no exercise) : Calorie-Calculation = BMR x 1.2 • If you are lightly active (light exercise/sports 1-3 days/week) : Calorie-Calculation = BMR x 1.375 • If you are moderatetely active (moderate exercise/sports 3-5 days/week) : Calorie-Calculation = BMR x 1.55 • If you are very active (hard exercise/sports 6-7 days a week) : Calorie-Calculation = BMR x 1.725 • If you are extra active (very hard exercise/sports & physical job or 2x training) : Calorie-Calculation = BMR x 1.9 1/29/2019 F.R.SIDDIQUEE 269 Estimation of Energy Requirements • Energy requirement can also be determined from energy expenditure, which can be estimated in a number of ways. • The most common approach is the factorial method, in which the different components of energy expenditure are separately determined. • A complete knowledge of the hours of activity, type of activity, hours of rest and sleep besides height, weight, age and sex are required to calculate the daily calorie requirements. 1/29/2019 F.R.SIDDIQUEE 270 Calculation of Total Energy Requirement • Calculate the total energy requirement of a Bangladeshi male medical student, aged 22 years, height 162 cm and weight 55 kg, the surface area is 1.55 sq. meters. His BMR is 41 Kcal/sq. m/hr. • 1) His basal requirement/day = 41 x 1.55 x 24 = 1525 kcal • 2) SDA. 10% of basal requirements kcal = 152 • 3a) 8 hours moderate work (walking, playing simple • games like badminton, shuttle etc.), extra 100 kcal/hr = 800 kcal • 3b) 8 hours sedentary activity like sitting, reading, • writing etc., Extra = 40 kcal/hr 320 kcal • ---------------------- • • Total 1/29/2019 F.R.SIDDIQUEE or say = 2797 kcal 2800 kcal 271 Estimated Energy Requirement Equations • Just as there are Dietary Reference Intakes (DRIs) for nutrients, there are also DRIs for energy, called Estimated Energy Requirements (EERs). • The Estimated Energy Requirement (EER) is defined as • the average dietary energy intake that is predicted to maintain energy balance in a healthy person of a defined • age, gender, weight, height, and level of physical activity consistent with good health. • A set of predicted equations have been developed to calculate the EER. 1/29/2019 F.R.SIDDIQUEE 272 DRIs for Energy : Estimated Energy Requirements • The EER equations for adults (below) predict TEE from age, height, weight, gender, and physical activity level. • For Males • EER = 662– 9.53 X age [yr] + PA X (15.91 X weight [kg] + 539.6 X height [m]) • PA = 1.0 (sedentary), 1.11 (low active), 1.25 (active), 1.48 (very active) • For Females • EER = 354 – 6.91 X age [yr] + PA X (9.36 X weight [kg] + 726 X height [m]) • PA = 1.0 (sedentary), 1.12 (low active), 1.27 (active), 1.4 (very active) • Separate equations have been developed for infants, children, and teens, and adjustments are made for pregnancy and lactation. • EER values have not been established for persons who are overweight or obese. 1/29/2019 F.R.SIDDIQUEE 273 Example: Estimation of Energy Requirements • Example: Calculate the estimated energy requirements of an active 30-year-old male who is 1.8 m tall and weights 80.9 kg. EER = 662 – 9.53 X 30 + 1.25 X [(15.91 x 80.9) + 539.6 x 1.8)] = 3199 kcal/day (about 3200 kcal/day) His actual requirement probably falls within a range 200 kcal above or below this estimate. For most people, the actual energy requirement falls within these ranges: For men, EER ± 200 kcal. For Women, EER ± 160 kcal. 1/29/2019 F.R.SIDDIQUEE 274 Energy Calculation • The fastest and easiest method for calculating your total daily energy expenditure, is by multiplying your total body weight by a certain amount of calories for each pound of body weight. If you have an average amount of muscle mass and body fat, this method can be quite accurate. • To maintain your current weight you multiply your current body weight by 15 calories per pound of bodyweight. • For example 200 pounds multiplied by 15 calories, would give you a maintenance level calorie intake of 3000 calories per day! • If you want to lose weight you would multiply your current body weight by 12 calories per pound of bodyweight. • This would be 200 pounds multiplied by 12 calories, which would give you 2400 calorie intake for weight loss. • This quick formula does not take into account your current body composition or your current activity levels. • But if you want to get a quick approximate figure of your optimum daily calorie intake...it does the job. 1 kilogram = 2.2 pounds 1/29/2019 F.R.SIDDIQUEE 275 Energy Calculation… • Using BMR will be even more accurate • Formulas for calculating your daily maintenance calorie intake based on your basal metabolic rate (BMR), that are multiplied by your activity level, will always be the more accurate. • YOUR FIRST OPTION... • The first formula The Harris-Benedict formula can be used if you have not calculated your lean body mass (LBM). • For this formula you use your age, sex, height and weight to determine your basal metabolic rate (BMR). • It is much more accurate than the quick formula above. Here is the formula: • -For Men to calculate BMR = 66 + (13.7 x weight in kg) + (5 x height in cm) – (6.8 x age in years) • -For Women to calculate BMR = 655 + (9.6 x weight in kg) + (1.8 x height in cm) – (4.7 x age in years) • The Harris-Benedict equation has a separate formula for men and women, because as we already mentioned, most men have higher muscle mass and larger bodies. 1/29/2019 F.R.SIDDIQUEE 276 Energy Calculation… Example #1: You are a male, 35 years old, 6 foot tall (182.88 cm), you weigh 200 pounds (91 kg). Your basal metabolic rate (BMR) will be 66 + 1246.7 + 914.4 – 238 = 1989.1 calorie intake per day! Example #2: You are a female, 35 years old, 5 feet 6 inches tall (170.69 cm), you weigh 132 pounds (60 kg). Your basal metabolic rate (BMR) will be 655 + 576 + 307.24 – 164.5 = 1373.74 calorie intake per day! • Once you know your BMR (basal metabolic rate) then use your daily activity factor to get your total daily energy expenditure (TDEE): • -Sedentary................BMR x 1.2 (little exercise) • -Lightly active...........BMR x 1.375 (light exercise) • -Moderately active.....BMR x 1.55 (moderate exercise) • -Very active.............BMR x 1.725 (hard exercise) • -Extremely active......BMR x 1.9 (hard exercise daily) For example #1... if you are a moderately active male…your TDEE will be 1989.1 calories times your activity level of 1.55 which equals 3083 calories per day. For example #2... if you are a moderately active female, your TDEE will be 1373.74 calories which equals 2129.30 calories per day. 1/29/2019times your activity level of 1.55 F.R.SIDDIQUEE 277 Energy Calculation…. • YOUR SECOND OPTION • The second formula Katch-McArdle, takes into account your lean body mass (LBM), and will be the most accurate formula that you can use, to get the most accurate total daily energy expenditure. • The formula is BMR = 370 + (21.6 x lean body mass in kg), for both men and women. • Example #1: You are a male, you weigh 200 pounds (91 kg). Your body fat percentage is 20% (40 pounds fat, 160 pounds lean body mass) Your lean body mass (LBM) is 72.72 kg. Your basal metabolic rate (BMR) will be 370 + (21.6 x 72.72) = 1940.75 calorie intake per day! • Example #2: You are a female, you weigh 132 pounds (60 kg). Your body fat percentage is 20% (26.4 pounds fat, 105.6 pounds lean body mass) Your lean body mass (LBM) is 48 kg. Your basal metabolic rate (BMR) will be 370 + (21.6 x 48) = 1406.8 calorie intake per day! 1/29/2019 F.R.SIDDIQUEE 278 Energy Calculation…. • Once you know your BMR then use your daily activity factor to get your total daily energy expenditure (TDEE): • -Sedentary................BMR x 1.2 (little exercise) • -Lightly active...........BMR x 1.375 (light exercise) • -Moderately active.....BMR x 1.55 (moderate exercise) • -Very active.............BMR x 1.725 (hard exercise) • -Extremely active......BMR x 1.9 (hard exercise daily) • For example #1... if you are a moderately active male…your TDEE will be 1940.75 calories times your activity level of 1.55 this will be 3088 calories per day. • For example #2... if you are a moderately active female, your TDEE will be 1406.8 calories times your activity level of 1.55 this will be 2180.54 calories per day. • As you can see the difference between the second and third formula is very minimal. • The Katch-McArdle formula is more accurate when you have an above average muscle mass or above average body fat. 1/29/2019 F.R.SIDDIQUEE 279 Obesity Obesity has become a global problem and has emerged as the most important contributor to ill health, displacing undernutrition and infectious disseases. Obesity is a normal response to an abnormal environment, rather than an abnormal response to an abnormal environment. Stimulation of physical activity and the promotion of healthy eating habits are essential. Modification of lifestyle habits should not rely on personal advice only, but should also address components of the physical, economic and sociocultural environments in which individuals live. 1/29/2019 F.R.SIDDIQUEE 280 Obesity: A Public Health Crisis • Obesity poses a major threat to public health due to the clear association between obesity and a variety of chronic diseases, such as type 2 diabetes, heart disease, cancer, stroke, and hypertension. • A number of factors influence overweight or obesity, including the following: • Behavior: eating too many calories while not getting enough physical activity. • Environment: Home, work, school, or community can provide barriers to or opportunities for an active lifestyle. • Genetics: Heredity plays a large role in determining how susceptible people are to overweight and obesity. Genes also influence how the body burns calories for energy or stores fat. Behavioral and environmental factors are the main contributors to overweight and obesity and provide the greatest opportunity for prevention and treatment. 1/29/2019 F.R.SIDDIQUEE 281 Factors in the Development of Obesity • At its simplest, obesity results from a chronic positive energy balance - energy intake regularly exceeds energy output, and weight is gained. • Obesity is a complex disorder that probably involves several regulatory mechanisms and the way they interact and response to biological factors such as heredity, age, and sex; social and environmental factors; and behavior and lifestyle choices. • Biological Factors • Heredity and Genetics • When both parents are morbidly obese (Body weight 100% above normal), the probability that their children will be obese is high (80%); when neither parent is obese, the probability that their children will be obese is relatively low (< 10%). • However, about 25-30% of obese individuals have normal-weight parents. 1/29/2019 F.R.SIDDIQUEE 282 Factors in the Development of Obesity … • Fat Cell Development • The number and size of fat cells in the body help determine how easily a person gains or loses fat. • Hypercellular obesity: an above-average number of fat cells. People may born with them or may developed them at certain critical times because of overeating. • Hypertrophic obesity: fat cells are larger than normal. Fat cells continue to expand as they fill with more fat; when their capacity is reached, the body generates more cell. • Even with weight loss, the number of fat cells does not decline. Fat cells do become smaller, but beyond a certain point, they resist further shrinking and the body strives to refill them with fat, making it difficult to maintain weight loss. 1/29/2019 F.R.SIDDIQUEE 283 Factors in the Development of Obesity … • Sex and Age • In general, males and females set different weight standards for themselves. Obesity is more prevalent in women than in men. • By early adulthood, about the same number of men want to loss or gain weight, whereas almost all women want to lose weight. • Adult women feel thin only when they weight < 90% of desirable body weight, whereas men rate themselves as thin even when they are above a healthy body weight. • Both men and women gain the most weight between 25 and 34 years of age. After that, we gain weight more slowly and then start to lose it after we reach age 55. 1/29/2019 F.R.SIDDIQUEE 284 Factors in the Development of Obesity … • Race and Ethnicity • The prevalence of obesity and attitudes about weight differ among racial and ethnic groups. • Black and Hispanic women are more likely to be overweight than white women. • Rates of overweight are similar for black and Hispanic, and white men. • Because of cultural factors, African Americans, Hispanic Americans, and Native Americans typically value thinness less than white Americans do. 1/29/2019 F.R.SIDDIQUEE 285 Factors in the Development of Obesity … • Social and Environmental Factors • Socioeconomic Status • Income: People are more likely to be obese if they have low socioeconomic status. Obesity is more prevalent in lower-income women. • Education: is another factor associated with body weight, but mainly for women. The prevalence of overweight among less educated women were higher than those of higher educated. • Occupational prestige: Obesity is more prevalent in women in less prestigious jobs. • Employment: Women who are not employed have a higher incidence of obesity. • Marriage: Married men have a higher incidence of obesity. • Residence: Rural women have a higher incidence of obesity. 1/29/2019 F.R.SIDDIQUEE 286 Factors in the Development of Obesity … • The Built Environment • Our immediate surroundings influence our behaviors, and have link with obesity. • The environments in which we live and work can either encourage or hinder physical activity and healthful eating. • When neighborhoods have low ‘walkability’, BMI s is tend to be higher. • Lower-income neighborhoods have fewer recreational facilities and healthful eating options. • Fast-food restaurants and convenience stores are more prevalent in low-income neighborhoods, whereas the number of supermarkets are more in wealthier neighborhoods. 1/29/2019 F.R.SIDDIQUEE 287 Factors in the Development of Obesity … • Social factors • Social factors also influence the development of obesity. • Abundant high-calorie, highly palatable foods, pervasive advertising promoting their consumption, and the social enjoyment of eating all create pressures to over eat. 1/29/2019 F.R.SIDDIQUEE 288 Factors in the Development of Obesity … • Lifestyle and Behavior Factors • Physical Activity • Lack of exercise is a major contributing factor to weight gain and obesity. • Some people may be obese, not because they eat too much, but because they move too little. • Inactivity is more common among women, older adults, and less affluence adults. • In both children and adults, research links excessive television viewing to obesity. • For many people, television watching, video games, and computer entertainment have all but replaced outdoor work and play as the major leisure time activity. 1/29/2019 F.R.SIDDIQUEE 289 Factors in the Development of Obesity …….. • Lifestyle and Behavior Factors • Psychological Factors • Some people adopt eating as a strategy for dealing with the stresses and challenges of life. Overeating also can occurs in response to complex human sensations such as entertainment, boredom, loneliness or depression. • Any kind of stress can cause overeating. • Certain obese people may be more prone to emotional eating than others. • Other people respond to other external stimuli such as the time of day (“I am not hungry, but it’s time for lunch”). 1/29/2019 F.R.SIDDIQUEE 290 Factors in the Development of Obesity … • People with a healthy lifestyle have more effective ways to meet their needs. They communicate assertively and manage interpersonal conflict effectively, so they don’t shrink from problems or over eat. • The person with a healthy lifestyle knows how to create and maintain relationships with others and has a solid network of friends and loved ones. • Food is used appropriately – to fuel life’s activities and gain personal satisfaction, not to manage stress. 1/29/2019 F.R.SIDDIQUEE 291 Health Risks Associated with Body Weight and Body Fat • Body weight and fat distribution correlated with disease risks and life expectancy. These risks indicate a greater likelihood of developing a chronic disease and shortening life expectancy. • Not all overweight and underweight people will get sick and die before their time nor will all normal-weight people live long healthy lives. These are correlations, not causes. • For the most part, people with a BMI falls between 18.5 and 24.9 have relatively few health risks; risks increase as BMI falls below or rises above this range, indicating that both too little and too much body fat impair health. • BMI, is a ratio of weight (kg) to height (m2), correlates reasonably well with body fatness and health risks. • Underweight: BMI<18.5 kg/m2; Normal weight: 18.5 to < 25; Overweight: 25 to < 30; Obese: 30 and over • Fat Distribution: More critical than the total amount of fat alone. Intra-abdominal fat that is stored around the organs of the abdomen is referred to as central obesity or upper-body fat (Apple shape) and, independently of total body fat, is associated with increased risks. Lower body fat (Pears Shape). 1/29/2019 F.R.SIDDIQUEE 292 Health Risks of Overweight and Obesity • Overweight and obesity are major public health challenges. • Among the health risks associated with obesity are diabetes, hypertension, cardiovascular disease*, some cancers, and complications in pregnancy and surgery. • Mortality increases as excess weight increases; people with a BMI greater than 35 are twice as likely to die prematurely as others. *Diseases of the heart and blood vessels collectively known as cardiovascular disease (CVD). Coronary heart disease (CHD) is the most common form of cardiovascular disease and is usually caused by atherosclerosis in the coronary arteries that supply blood to the heart muscle. 1/29/2019 F.R.SIDDIQUEE 293 Obesity and cardiovascular disease (CVD) • It is now well recognized that obesity, especially abdominal adiposity, is a risk factor for CVD. • Obesity is a risk factor for increased blood pressure and an unfavorable lipid profile which in turn are risk factors for CVD. • Similarly, weight loss has been shown to improve both blood pressure and lipid levels, at least in the short term. • However, obesity is also an independent risk factor for CVD. • Maintaining optimal weight causes 25% less CHD and 35% fewer strokes or episodes of heart failure. • A 20% weight reduction in the obese confers a 40% reduced risk of a coronary event. 1/29/2019 F.R.SIDDIQUEE 294 Obesity and Cardiovascular Disease… • The relationship between obesity and cardiovascular disease risk is strong, with links to both elevated blood cholesterol and hypertension. • Central obesity may raise the risk of heart attack and stroke as much as the three leading risk factors (high LDL cholesterol, hypertension, and smoking) do. • In addition to body fat and its distribution, weight gain also increases the risk of cardiovascular disease. • A person who is only mildly to moderately obese has an elevated risk of coronary heart disease. • However, even modest weight loss (about 10% of body weight) reduces risk. 1/29/2019 F.R.SIDDIQUEE 295 Obesity and type 2 diabetes mellitus • Besides being a major risk factor for CVD, obesity, and in particular abdominal obesity, is the most important risk factor in the onset of type 2 diabetes. • Diabetes is by far the most expensive public health consequence of obesity. • WHO has calculated that about 64% of type 2 diabetes in US men and 74% in US women could be avoided if BMI was maintained at or below 25 kg/m2. • Recent intervention studies in groups at high risk of type 2 diabetes show that moderate lifestyle changes and relatively minor weight loss may lower the risk of developing type 2 diabetes mellitus by as much as 60%. • Diabetes (type 2) is three times more likely to develop in an obese person than in a non-obese person. • Furthermore, the person with type 2 diabetes often has abdominal (central) obesity. • Diabetes, in turn, is a risk factor for heart disease. 1/29/2019 F.R.SIDDIQUEE 296 Obesity and cancer • There is sufficient evidence for a cancer-preventive effect of avoidance of weight gain (prevention of overweight). • The risk of some cancers increases with both body weight and weight gain, but researchers do not fully understand the relationships. • The same food pattern that contributes to obesity (a diet high in calories and fat, plus low in fiber, fruits, and vegetables) also may be a cancer risk. • Inactivity not only encourages obesity, but also increases cancer risk. 1/29/2019 F.R.SIDDIQUEE 297 Energy Balance • When more food energy is consumed than is needed, excess fat accumulates in the fat cells in the body’s adipose tissue where it is stored. • When energy supplies run low, stored fat is withdrawn. • For energy imbalance, too much or too little fat on the body does not necessarily required, small imbalances in the energy budget compound over time. • 450 g (1 lb) body fat = 3,500 kcal. • Pure fat is worth 9 kcal per g. 450 g, then would store 4,050 kcal. A pound of body fat is not pure fat, it contains water, protein, and other materials of living tissue – hence the lower kcal value. 1/29/2019 F.R.SIDDIQUEE 298 Recommended Books • Human Nutrition and Dietetics. Edited by J.S. Garrow and W.P.T. James, 9th Edition, Churchill Livingstone, UK, 1993. • A Textbook of Foods, Nutrition and Dietetics. By M. Raheena Begum. Sterling Publishers Pvt. Ltd., New Delhi, 1996. • Introduction to Human Nutrition. Edited by M.J. Gibney, H.H. Vorster and F.J. Kok. The Nutrition Society Test Book Series, Blackwell Publishing, UK, 2002. • Understanding Nutrition. By Ellie Whitney and Sharon Rady Rolfes. 3rd Edition, Thomson Wadsworth, USA, 2005. • Nutrition: Concepts and Controversies. By Frances Sizer and Ellie Whitney. 10th Edition, Thomson Wadsworth, USA, 2005. 1/29/2019 F.R.SIDDIQUEE 299 10. Role of Functional Foods in Human Health BMB 303 – HUMAN NUTRITION Yearul Kabir 1/29/2019 F.R.SIDDIQUEE 300 Functional Foods • Although there is not yet a legal definition for the term, a functional food is widely considered to be a food or food component that may provide a health benefit beyond those of the traditional nutrients. For examples: grains rich in dietary fibers, fish rich in omega-3 fatty acids, and fruits rich in phytochemicals. • "Functional Food is a Natural or processed food that contains known biologically-active compounds which when in defined quantitative and qualitative amounts provides a clinically proven and documented health benefit, and thus, an important source in the prevention, management and treatment of chronic diseases of the modern age". • A functional food is a food given an additional function (often one related to health-promotion or disease prevention) by adding new ingredients or more of existing ingredients. 1/29/2019 F.R.SIDDIQUEE 301 Functional Foods… • Functional foods may include whole foods, fortified foods, and modified foods. Fermented foods with live cultures are considered functional foods with probiotic benefits. • Functional foods are an emerging field in food science due to their increasing popularity with health-conscious consumers and the ability of marketers to create new interest in existing products. • Garlic contains sulfur compounds that may reduce heart disease risk, and tomato sauce is rich in lycopene, a compound that may reduce prostate cancer risk. The soy protein in tofu and the fiber in oatmeal can help reduce the risk of heart disease. • All the functional foods just mentioned get their health-promoting properties from naturally occurring compounds that are not considered nutrients but are called phytochemicals. 1/29/2019 F.R.SIDDIQUEE 302 Functional Foods… • Cranberries may help protect against urinary tract infections; garlic may lower blood cholesterol; and tomatoes may protect against some cancers. • Many processed foods become functional when they are fortified with nutrients or enhanced with phytochemicals or herbs (e.g., calcium-fortified orange juice). • Less frequently, an entirely new food is created, as in the case of a meat substitute made of mycoprotein – a protein derived from a fungus. This functional food not only provides dietary fiber, polyunsaturated fats, and high-quality protein, but it lowers LDL cholesterol, raises HDL cholesterol, improves glucose response, and prolongs satiety after a meal. • Such a novel functional food raises the question – is it a food or a drug? 1/29/2019 F.R.SIDDIQUEE 303 Functional Foods… • Not long ago, most of us could agree on what was a food and what was s drug. As functional foods come to market, this distinction is becoming less clear. • Consider the healing powers of yogurt, for example, yogurt contains Lactobacillus and other living bacteria that ferment milk into yogurt. These microorganisms, called probiotics, change the population of microbes in the GI tract, which improves defenses against GI disorders. • Like drugs used to treat chronic diseases, functional foods may need to be eaten several times a day for several months or years to have a beneficial effect. • Sporadic users may be disappointed in the results. 1/29/2019 F.R.SIDDIQUEE 304 Functional Foods… • When used four times a day for four weeks, margarine enriched with phytosterols reduces cholesterol by 8%, much more than regular margarine does, but not nearly as much as the 32% reduction seen with cholesterol-lowering drugs. • For this reason, functional foods may be more useful for prevention and mild cases of disease than for intervention and more severe cases. • Food and drugs differ dramatically in cost as well. Functional foods such as fruits and vegetables incur no added costs, of course, but foods that have been manufactured with added phytochemicals can be expensive, costing up to six times as much as their conventional counterparts. • The price of functional foods typically falls between that of traditional foods and medicines. 1/29/2019 F.R.SIDDIQUEE 305 Functional Foods… Phytochemicals Make Foods Functional A vitamin is a food substance essential for life, Phytochemicals, in contrast, are substances in plants that may promote good health, even though they are not essential for life. Phytochemicals are complex chemicals that vary from plant to plant. They include thousands of compounds, pigments, and natural antioxidants, many of which have been associated with protection from heart disease, hypertension, cancer, and diabetes. 1/29/2019 F.R.SIDDIQUEE 306 How do phytochemical work to prevent chronic diseases? • A number of phytochemicals, including those from soybeans and from the cabbage family, are able to modify estrogen metabolism or block the effect of estrogen on cell growth. Since levels of estrogen and other hormones are in turn closely linked to the development of breast, ovarian, and prostate tumors, it is apparent how phytochemicals might inhibit development of such cancers. • Other phytochemicals neutralize free radicals. Free radicals (active oxidants) are continually produced in our cell and over time can result in damage to DNA and important cell structures. • Eventually, this damage can promote both cancer and cell aging. Free radical oxidation of lipids contributes to heart disease risk. 1/29/2019 F.R.SIDDIQUEE 307 How do phytochemical work to prevent chronic diseases? • Many different plant chemicals, such as the pigments in grapes and red wine, are able to neutralize or reduce concentrations of free radicals, thus protecting us against the development of both cancer and heart disease. • Phytochemicals in fruits and vegetables have a number of other potential benefits. Lutein and zeaxanthin are carotenoids (plant pigments) found in dark-green leafy vegetables, corn, and egg yolks. Increased consumption of these compounds is associated with a lower incidence of age-related mascular degeneration, the leading cause of blindness in older people. The phytochemicals in whole grains are generally similar to those found in fruits and vegetables and are also important in prevention of both cancer and heart disease. • One class of grain phytochemicals, the terpenoids, produces a significant reduction in total and LDL cholesterol levels, thus reducing the risk of heart disease. 1/29/2019 F.R.SIDDIQUEE 308 Claims for Functional Foods When a functional food meets the appropriate FDA guidelines, it may make a nutrient content claims or health claim on the label. • For example, tofu containing at least 6.25 g of soy protein per serving may make a health claim about the role of soy protein in reducing the risk of heart disease. • Oatmeal with an adequate amount of beta-glucan fiber can highlight its benefit in reducing risk of heart disease. • Certain types of nuts (e.g., almonds, hazelnuts, peanuts, pecans, pistachio nuts, and walnuts) may make a qualified health claim on the label linking nut consumption with reduced risk of heart disease. • Under FDA guidelines, a functional food’s label may have a nutrient content claim, health claim, or structure/function claim. • A structure/function claim promotes a substance’s effect on the structure or function of the body. 1/29/2019 F.R.SIDDIQUEE 309 Strategies for Functional Food Use • Which ones would you buy? • The best course of action is to stick with what scientists have agreed upon so far. • First, fruits and vegetables promote health and reduce disease risk through a whole host of natural phytochemicals. • Second, consider nutrient-fortified products when a particular nutrient is lacking in your diet and you either do not like or cannot eat good food sources of that nutrient. • For example, if you are allergic to milk and dairy products, consider calcium-fortified orange juice as a nutritious way to get the calcium that you need. • Third, read, read, read about functional foods, and not just what’s on the Internet. Do your homework by looking at scientific articles – your instructor can help you find and interpret studies of functional food components. • Finally, be critical of advertising and hype – if it sound too good to be true, it probably is ! 1/29/2019 F.R.SIDDIQUEE 310 Role of Food Toxin in Human Nutrition BMB 303 – HUMAN NUTRITION Yearul Kabir 1/29/2019 F.R.SIDDIQUEE 311 Natural Toxins in Foods • Toxic substances in foods are generally those substances found in foods that produce harmful effects on ingestion by humans or animals. • Toxic substances present in foods can be natural or due to accidental chemical contamination. • Natural toxicants may be inherently present in food or arise due to abnormal environmental/improper storage conditions and when consumed in large quantities over long periods may prove toxic. • Examples of these include • Protease inhibitors mainly present in legumes that inhibit digestion of proteins. • Hemagglutinins that agglutinate blood cells. • Goitrogens that may cause hypothyroidism found in mustard, cabbage and such vegetables. • Cyanogenic glycosides that produce hydrocyanic acid, lathyrogens, saponins, oxalic acid, salanins and such others. 1/29/2019 F.R.SIDDIQUEE 312 Toxicants of Natural Origin • Plant Origin • Toxin containing seeds such as dhatura, agremone may enter grains and oilseeds rendering them unsafe for human consumption. • Marine Origin • Several syndromes are caused by ingestion of shellfish and finfish containing toxins. The toxins are not produced by the fish but by living creatures that the fish themselves eat. These are dinoflagellates, members of the algae family that carry out metabolism through photosynthetic reactions. • Microbial Origin • Foods with high moisture content are susceptible to contamination by bacteria and moulds. Some grow in the food and produce toxins. 1/29/2019 F.R.SIDDIQUEE 313 Toxicants of Plant Origin • Some of the important naturally occurring toxic substances in foods are: • Neurolathyrism is a disease characterized by gradually developing spastic paralysis of the lower limbs caused by Lathyrus sativus (Khesari dal). Diet containing more than 30% L. sativus for six months will cause the disease. • Toxin, an unusual amino acid (N) oxalyl amino–L-alanine (BOAA) also known as oxalyl diamino propionic acid (ODAP) isolated from L. sativus has been implicated as the causative agent of neurolathyrism and effected the nervous system. • Acute: in more than 50% the onset is sudden and severe. The person while at work may fall down even in field. • Sub-acute: it occurs after 15 to 20 days of spasm and is precipitated by sudden physical effort. Full fledged picture emerges in a period of one month. 1/29/2019 F.R.SIDDIQUEE 314 Toxicants of Plant Origin… • Toxic Alkaloids • Potatoes contain many natural poisons, including solanine, a powerful bitter, narcotic like substance. • The toxic action of solanine has been attributed to inhibition of serum cholinesterase. • The small amounts of solanine normally found in potatoes are harmless, but solanine can build up to toxic levels when potatoes are exposed to light during storage. • Cooking does not destroy solanine, but because most of a potato’s solanine is in a green layer that develops just beneath the skin, it can be peeled off, making the potato safe to eat. If the potato tastes bitter, however, throw it out. 1/29/2019 F.R.SIDDIQUEE 315 Toxicants of Plant Origin… • Goitrogens in Cruciferous Vegetables • Cruciferous vegetables such as broccoli, cauliflower, and brussels sprouts contain several compounds, some of which are harmful to health. Goitrogens are toxicants found in these products, responsible for the development of goiter in humans. • Thiocyanate is one of the most commonly found goitrogens in cabbage. Progoitrin, a goitrogen found in rapeseed, inhibits production of thyroid hormones in humans. • Cyanogenic Glycosides • Several plants produce compounds that contain cyanogenic glycosides (or glucosides). When ingested, these are converted to hydrogen cyanide (HCN), a powerful toxicant. This production of HCN is based on the breakdown of cyanogenic glycosides, either by enzymatic action of -glucosidase, or by a low pH. 1/29/2019 F.R.SIDDIQUEE 316 Toxicants of Plant Origin… • Although over 25 cyanogenic glycosides are known to occur in 2000 plant species, important among them are Linamarin and Lotaustralin in cassava and lima beans. Dhurrin in sorghum, Taxiphyllin in bamboo shoots and Amygdalin in almonds. • Acute toxicity at small doses can cause headache, tightness in the throat and chest, and muscle weakness. Exposure to cyanidecontaining foods has been linked to several conditions, such as anemia, degeneration of the optic nerve in people with a vitamin deficiency, and atrophy of the optic nerve. • Trypsin Inhibitors • In several plants, specially members of Leguminosae, some protein inhibitors, active against pancreatic protolytic enzymes of vertebrates occur in varying quantities. 1/29/2019 F.R.SIDDIQUEE 317 Toxicants of Plant Origin… • Among them, trypsin inhibitors are the most widely distributed, and reported to be present in redgram, bengalgram, cow pea, soybean, potato, sweet potato and sunflower. The trypsin inhibitors have been found to cause growth retardation and hypertrophy of pancreas. • Haemagglutinins • Some of the edible plant seeds belonging to Leguminosae and Euphorbiaceae families contain globulin type of protein component having the property of agglutinating red blood cells (RBCs) known as phytohaemagglutinins or haem-agglutinins. • These heat-labile agglutinins have isolated from field bean, white bean, double bean and horse gram. • Consumption of improperly processed beans have been reported to result in nausea, vomiting and diarrhoea. The agglutinins at low levels lead to growth depression, reduction of food intake and death. 1/29/2019 F.R.SIDDIQUEE 318 Toxicants of Plant Origin… • Herbs • The herbs balladonna and hemlock have reputations as deadly poisons, but few people know that the herb sassafras contains a cancer-causing agent and is banned from use in commercially produced foods and beverages. • Herbal extracts are considered by many as superior to synthetic medicines, because they believe that herbs are natural, and thus cannot be harmful. • Pyrrolizidine alkaloids are toxic compounds found in comfrey, Indian herbal teas, tomatoes, potatoes, and eggplant. They inhibit the enzyme cholinesterase, which serves to break down acetylcholine. Since acetylcholine is used by nerve cells to transmit signals to the rest of the body, stopping the action of cholinesterase prevent regulation of acetylcholine, resulting in over stimulation of nerve cells. 1/29/2019 F.R.SIDDIQUEE 319 Toxicants of Plant Origin… • Chamomile is an herb used by many people in an herbal tea for adults or to treat childhood illnesses. Some allergic reactions to the tea have been observed, and continued use over time can cause diarrhea and seizures. • Rosemary and sage are commonly used herbs. Plant extracts of these products have been found to be toxic to yeast cells, with eucalyptol being the main fungicidal component. • Small amounts of rosemary and sage constituents can cause a variety of symptoms, including nausea, severe headache, and vomiting, due to these bioactive components. 1/29/2019 F.R.SIDDIQUEE 320 Toxicants of Plant Origin… • Toxic Mushrooms • All mushrooms contain at least one toxicant (hydrazine), including those grown for food and including prized wild species such as Agaricus bisporus, Boletus edulis, and Gyromitra esculenta. Most of the toxicants cannot be eliminated by cooking, canning, freezing, or any means of processing. Thus, the only way to avoid the toxicants is to avoid eating the mushrooms. • The good news is that the toxin levels are low enough that there are no health effects from consuming normal amounts of edible mushrooms. • Mushroom poisoning occurs when people eat known poisonous species. The effects of the toxicants in mushrooms are acute. 1/29/2019 F.R.SIDDIQUEE 321 Toxicants of Marine Origin • There are at least five types of marine toxic poisonings: • • • • • Ciguatera Paralytic shellfish poisoning (PSP) Neurotoxic shellfish poisoning (NSP) Diarrhetic shellfish poisoning (DSP) Amnesic shellfish poisoning (ASP) • Ciguatera is caused by consumption of tropical herbivorous reef fish, such as grouper and red snapper, and the carnivorous fish that feed upon them. The source is the dinoflagellate Gambierdiscus toxicus. • Paralytic shellfish poisoning is caused by consumption of mussels, calms, and oysters. The source of the illness is toxin produced by the dinoflagellate Gonyaulax catenella. 1/29/2019 F.R.SIDDIQUEE 322 Toxicants of Marine Origin… • Neurotoxic shellfish poisoning results from ingestion of oysters and clams that have ingested dinoflagellate Ptychodiscus brevis. • Diarrhetic shellfish poisoning is caused by consumption of mussels, and calms contaminated with the dinoflagellate Dinophysis fortit, as well as species of the genus Prorocentrum. • Amnesic shellfish poisoning is caused by mussels harvested from the eastern shore of Canada that are infected with the dinoflagellate Nitschia. 1/29/2019 F.R.SIDDIQUEE 323 Toxicants of Marine Origin… • Mercury in Seafood • A number of people in Minamata, Japan, became ill with a disease (Minamata disease) due to toxicity of methylmercury. • Manufacturing plants in the region were discharging mercury into the waters of the bay (sea), and bacteria in the water were converting the mercury into a more toxic form, methylmercury. • The fish in the bay were accumulating this poison in their bodies and eating fish from the bay every day cause the disease. • Survivors of Minamata disease suffered progressive, irreversible blindness, deafness, loss of coordination, and severely impaired mental function. 1/29/2019 F.R.SIDDIQUEE 324 Toxicants of Microbial Origin • Microbial toxins are those produced by microorganisms, either by molds, in the case of mycotoxins, or by bacteria, in the case of bacterial toxins. • Exotoxins: generated and actively secreted. • Endotoxins: remain part of bacteria (usually outer membrane part). • Mycotoxins from Molds • Some molds associated with food are able to produce highly toxic substances known as mycotoxins. • Mycotoxins range in toxicity from causing typical food borne illness symptoms, such as vomiting, to more serious conditions such as gangrene, bone marrow destruction, renal disorders, and liver cancer. 1/29/2019 F.R.SIDDIQUEE 325 Toxicants of Microbial Origin… • Aflatoxicosis • These are a group of mycotoxins produced by certain fungi, i.e., Aspergillus flavus and A. parasiticus. • These fungi infest food grains such as groundnut, maize, parboiled rice under conditions of humidity and improper storage and produce aflatoxin of which B1 and G1 are the most potent hepatotoxins. These have been reported to be carcinogenic too. • Moisture level 16% and temperature ranging from 11 oC to 37 oC favor its formation. 1/29/2019 F.R.SIDDIQUEE 326 Toxicants of Microbial Origin… • Some Bacterial Toxins • Only three bacterial species are considered important causes of the intoxication type of food poisoning: • Clostridum botulinum • Staphylococcus aureus • Bacillus cereus • All of which are capable of causing illness by producing toxins in food. • The bacterial toxin, such as Botulium neurotoxins (Exotoxin), are the most potent natural toxins known and the causative agents of deadly food poisoning disease botulism by Clostridum botulinum. • Eight types of toxins have been identified that are allocated a letter (A–H), Only types A, B, E, F and H cause disease in humans. 1/29/2019 F.R.SIDDIQUEE 327 Toxicants of Microbial Origin… • Some Bacterial Toxins • Types A, B, and E are associated with food-borne illness, • The botulinum toxins are resistant to degradation by enzymes found in the gastrointestinal tract. • This allows for ingested toxin to be absorbed from the intestines into the blood stream. • However, all types of botulinum toxin are rapidly destroyed by heating to 100 °C for 15 minutes. 1/29/2019 F.R.SIDDIQUEE 328 Toxicants of Microbial Origin… • Staphylococcus aureus is a type of bacteria commonly found on the skin and hair as well as in the noses and throats of people and animals. • These bacteria are present in up to 25 percent of healthy people and are even more common among those with skin, eye, nose, or throat infections. • Staphylococcus can cause food poisoning when a food handler contaminates food and then the food is not properly refrigerated. • Staphylococcal Enterotoxins: produced by staphylococcus aureus. The cells produce seven enterotoxins – they affect the enteric, or intestinal, system. • All of the toxins are pyrogenic, able to cause fever, and can suppress the immune system of the person affected. 1/29/2019 F.R.SIDDIQUEE 329 Toxicants of Microbial Origin… • Bacillus cereus is becoming one of the more important causes of food poisoning in the industrialized world. It produces one emetic toxin and three different enterotoxins. • These toxins can cause two types of illness: one type characterized by diarrhea and the other, called emetic toxin, by nausea and vomiting. • These bacteria are present in foods and can multiply quickly at room temperature. • A variety of foods, particularly rice and leftovers, as well as sauces, soups, and other prepared foods that have sat out too long at room temperature. • The Bacillus cereus group comprises seven closely related species: B. cereus sensu stricto (referred to herein as B. cereus), B. anthracis, B. thuringiensis, B. mycoides, B. pseudomycoides, B. weihenstephanensis, B. cytotoxicus. 1/29/2019 F.R.SIDDIQUEE 330 Toxicants of Microbial Origin… • Other examples of bacterial toxins • Tetanus Toxin. Clostridum tetani produces tetanus toxin and the causative agent of tetanus. • Releasing the toxins: tetanolysin and tetanospasmin (also called "tetanus toxin") is one of the extremely potent neurotoxin known. • Shiga Toxin. Shigella dysenteriae produces Shigela toxin, causes dysentery. • Shiga toxins are a family of related toxins with two major groups, Stx1 and Stx2, • Diphtheria Toxin. is an exotoxin secreted by Corynebacterium diphtheriae, that causes diphtheria. • Not necessarily involving bacterial infection (e.g., when the bacteria have died, but have already produced toxin, which are ingested). 1/29/2019 F.R.SIDDIQUEE 331 Food Supplements in Human Nutrition BMB 303 – HUMAN NUTRITION Yearul Kabir 1/29/2019 F.R.SIDDIQUEE 332 Dietary Supplements: Vitamins and Minerals • Many people take supplements as dietary insurance – in case they are not meeting their nutrient needs from foods alone. Others take supplements as health insurance – to protect against certain diseases. • Arguments for Supplements • Vitamin-mineral supplements may be appropriate in some circumstances. In some cases, they can correct deficiencies; in others, they can reduce the risk of diseases. • Correct Overt Deficiencies • To correct an overt deficiency disease, a physician may prescribe therapeutic doses two to ten times the RDA (or AI) of a nutrient. At such high doses, the supplement is acting as a drug. 1/29/2019 F.R.SIDDIQUEE 333 Dietary Supplements: Vitamins and Minerals… • Improve Nutrition Status • In contrast to the classical deficiencies, which present a multitude of symptoms and are relatively easy to recognize, subclinical deficiencies are subtle and easy to overlook – and they are also more likely to occur. • People who do not eat enough food to deliver the needed amounts of nutrients, such as habitual dieters and the elderly, risk developing subclinical deficiencies. • Similarly, vegetarians who restrict their use of entire food groups without appropriate substitutions may fail to fully meet their nutrient needs. • If there is no way for these people to eat enough nutritious foods to meet their needs, the vitamin-mineral supplements may be appropriate to help prevent nutrient deficiencies. 1/29/2019 F.R.SIDDIQUEE 334 Dietary Supplements: Vitamins and Minerals… • Reduce Disease Risks • Few people consume the optimal amounts of all the vitamins and minerals by diet alone. Inadequate intakes have been linked to chronic diseases such as heart disease, some cancers, and osteoporosis. • For this reason, some physicians recommend that all adults take vitamin-mineral supplements. Others recognize the lack of conclusive evidence and the potential harm of supplementation and advise against such a recommendation. • Support Increased Nutrient Needs • Nutrient needs increase during certain stages of life, making it difficult to meet some of those needs without supplementation. For example, women who lose a lot of blood and therefore a lot of iron during menstruation each month may need an iron supplement. 1/29/2019 F.R.SIDDIQUEE 335 Dietary Supplements: Vitamins and Minerals… • Women of childbearing age need folate supplements to reduce the risks of neural tube defects. • Similarly, pregnant women and lactating mothers have exceptionally high nutrient needs and so usually need special supplements. • Improve the Body’s Defenses • Health care professionals may provide special supplementation to people being treated for addictions to alcohol or drugs and to people with prolonged illnesses, extensive injuries, or other severe stresses such as surgery. • Illnesses that interfere with appetite, eating, or nutrient absorption limit nutrient intakes, yet nutrient needs are often heightened by diseases or medications. • In all these cases, supplements are appropriate. 1/29/2019 F.R.SIDDIQUEE 336 Dietary Supplements: Protein and Amino Acid • Websites, health-food stores, and popular magazine articles advertise a wide variety of protein supplements, and people take these supplements for many different reasons, all of them unfounded. • • • • Athletes take to build muscle. Dieters take them to spare their bodies’ protein while losing weight. Women take them to strengthen their fingernails. People take individual amino acids, too – to cure herpes, to make themselves sleep better, to lose weight, and to relieve pain and depression. • Like many other magic solutions to health problems, protein and amino acid supplements don’t work these miracles. Furthermore, they may be harmful. • Muscle work build muscle; protein supplements do not, and athletes do not need them. Fingernails are not affected by protein supplements. 1/29/2019 F.R.SIDDIQUEE 337 Arguments against Supplements • Foods rarely cause nutrient imbalances or toxicities, but supplements can. The higher the dose, the greater the risk of harm. People’s tolerances for high doses of nutrients vary, just as their risks of deficiencies do. Amounts that some can tolerate may be harmful for others. It is difficult to determine just how much of a nutrient is enough – or too much. • Toxicity: The extent and severity of supplement toxicity remain unclear. • Life-Threatening Misinformation: Another problem arises when people who are ill come to believe that high doses of vitamins or minerals can be therapeutic. Not only can high doses be toxic, but the person may take them instead of seeking medical help. Furthermore, there are no guarantees that the supplements will be effective, e.g., herbal preparation. 1/29/2019 F.R.SIDDIQUEE 338 Arguments against Supplements… • Unknown Needs: Another arguments against the use of supplements is that no one knows exactly how to formulate the “ideal” supplement. • • • • What nutrients should be included? Which, if any, of the photochemical should be included? How much of each? On whose needs should the choices be based? • Surveys have repeatedly shown little relationship between the supplements people take and the nutrients they actually need. • False Sense of Security: Another argument against supple-ment use is that it may put people into a false sense of security. A person might eat irresponsibly, thinking, “My supplement will cover my needs.” • Or, experiencing a warning symptom of a disease, a person might postpone seeking a diagnosis, thinking, “I probably just need a supplement to make this go away.” such self-diagnosis is potentially dangerous. 1/29/2019 F.R.SIDDIQUEE 339 Dietary Supplements • Dietary supplements come in various forms – vitamins, minerals, amino acids, herbs, enzymes, and many others. • Moderate Supplementation • Health care practitioners often recommend moderate nutrient supplementation for people with elevated nutrient needs and people who may not always eat well enough. • Some example include the following: • • • • • • • Pregnant and breastfeeding women Women with heavy menstrual bleeding Children Infants People with severe food restrictions, either self-imposed or prescribed. Strict vegetarians who abstain from animal foods and dairy products Elders. 1/29/2019 F.R.SIDDIQUEE 340 Dietary Supplements… • Vitamin and mineral supplements are popular; however, it is better to obtain nutrients from food. Multivitamin/mineral supplements should be well balanced, with doses no greater than about 150% DV of each nutrient. • Some supplements are contraindicated during pregnancy or lactation; others should not be used with certain chronic illnesses. Supplements sometimes interfere with the action of medicines. Some slow blood clotting, which is a concern if surgery is planned. • Megadoses in Conventional Medical Management • High doses of vitamins and minerals have become so much a part of treating certain illnesses (colitis or cystic fibrosis) that when physicians prescribe these nutrients, many see themselves as following “standard medical practice” rather than as “practicing nutrition”. 1/29/2019 F.R.SIDDIQUEE 341 Dietary Supplements… • Megadosing Beyond Conventional Medicine • Megadoses of vitamin C cannot effectively prevent the common cold or treat cancer, but the vitamin may help prevent other conditions, such as cataracts. • Some studies do show a reduced duration of cold symptoms with high doses of vitamin C. A few studies found that colds were slightly less severe or less frequent in certain people, most studies found no beneficial effect. • The most controversial claim for vitamin C was its purported ability to prevent and treat cancer. Well-controlled studies have now disproved this claim. 1/29/2019 F.R.SIDDIQUEE 342 Drawbacks of Megadoses… • Megadose vitamins and minerals remain popular. But when taken without recommendation or prescription from a qualified health professional, they can cause problems. Since high doses of a nutrient can act as a drug, with a drug’s risk of adverse side effects, people who choose to take megadoses should always check first with their doctors. • Excesses of some nutrients can create deficits of other nutrients. It is easy to reach toxic levels if you use high doses of the fat-soluble vitamins A and D. • High doses of vitamin E can interfere with normal use of vitamin K and blood clotting. Megadoseing with water-soluble vitamin B6 at 50 to 100 times the DV can cause nerve damage. • Megadoses often are recommended for sick people, but sick people may be least able to tolerate them. 1/29/2019 F.R.SIDDIQUEE 343 Dietary Supplements: Natural Health Products • What are Natural Health Products? • Under the Natural Health Products Regulations, natural health products (NHPs) are defined as: • Vitamins and minerals supplements • Herbal and other plant-based health products • Homeopathic medicines • Traditional medicines such as traditional Chinese medicines • Probiotics and enzymes • Other products like amino acids and essential fatty acids • some personal care products like toothpastes that contain natural ingredients. 1/29/2019 F.R.SIDDIQUEE 344 Dietary Supplements: Natural Health Products… • NHPs must be safe to use as over-the-counter products and not need a prescription to be sold. Products needing a prescription and are regulated as drugs under the FAD regulations. • NHPs are naturally occurring substances that are used and marketed for a number of health reasons, like the prevention or treatment of an illness or condition, the reduction of health risks, or the maintenance of good health. • They are often made from plants, but can also be made from animals, microorganisms and marine sources. They come in a wide variety of forms like tablets, capsules, tinctures, solutions, creams, ointments and drops. 1/29/2019 F.R.SIDDIQUEE 345 Dietary Supplements: Natural Health Products… • Supplementation with herbal and other “natural” products is growing in popularity. • However, herbal therapy (phytotherapy) is nothing new. Most cultures have long traditions of using plants (and some animal products) to treat illness or sustain health. For centuries there were no other medicines. • Helpful Herbs, Harmful Herbs • The suggested benefits of herbs are based not on scientific study but on years of informal observation: Mint helps indigestion; ginger helps nausea and motion sickness; lemon perks appetite; chamomile helps insomnia. 1/29/2019 F.R.SIDDIQUEE 346 Dietary Supplements: Natural Health Products…. • If you are considering using an herb, remember that any herb that is strong enough to help you can be strong enough to hurt you. • Like any medicine, herbs can have side effects, and herbs can be contraindicated. Ginkgo biloba is a blood thinner and appears to help blood circulation, can cause harmful bleeding in some people. • Quality control is a big issue in herbal medicines. • To correct these problems, the FDA proposed new regulations in March 2003 to require Current Good Manufacturing Practices (CGMPs) in the manufacturing, packing, and storage of dietary supplements. These regulations would establish standards to ensure that dietary supplements and dietary ingredients are not adulterated with contaminants or impurities, and are labeled accurately to reflect active and other ingredients. 1/29/2019 F.R.SIDDIQUEE 347 Other Dietary Supplements • The supplement market used to include only vitamins, minerals, and a handful of other products such as brewer’s yeast and sea salt. Today there are hundreds more products, with new ones continuously popping up. Although some are useful, many are of dubious benefit. 1/29/2019 F.R.SIDDIQUEE 348