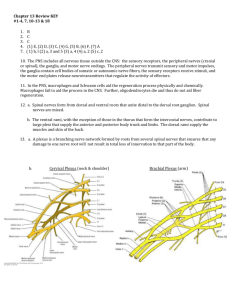
Brachial plexus notes Originates from the ventral rami of C5-C8 and T1 spinal nerves o Small contributions from C4 and T2 are known as “prefixed” and “postfixed” contributions. Dorsal rami travel posterior to innervate skin and muscles of the neck and upper back and are not part of the plexus. Ventral rami emerge between the anterior and middle scalenes o C5-8 descend toward the 1st rib o T1 must ascend over the 1st rib Motor cells of the nerve roots for the brachial plexus are located in the ventral horn of the spinal cord gray matter Sensory bodies are positioned outside the spinal cord within the dorsal root ganglia o Transfer afferent fibers to the spinal cord through the dorsal rootlets. Roots, Trunks, divisions, cord Ventral rami of C5-6 combine to form the upper trunk C7 continues alone to form the middle trunk C8-T1 unite to form the lower trunk Each trunk divides into anterior and posterior divisions and proceeds behind the clavicle. Divisions merge into 3 cords names in relation to the axillary artery. o Anterior divisions of the upper and middle trunk combine to form the lateral cord o The 3 posterior divisions of the upper, middle and inferior trunks converge to form the posterior cord. o The anterior division fo the lower trunk continues as the medial cord The cords proceed behind the pec minor muscle into the axilla. Each cord divides into two terminal branches. o Lateral cord: Musculocutaneous nerve Branch to the medial nerve o Posterior cord Axillary Radial nerves (largest branch of the brachial plexus Medial cord: Ulnar nerve Branch to the median nerve (majority of median motor fibers) Several branches arise from the roots, trunks, and cords. Can be helpful with diagnosis/location of nerve injury o Root level Dorsal scapular arises from C5 Levator scap, rhomboids Long thoracic from C5-C7 Serratus anterior Phrenic nerve from C3-C5 may be injured in nerve root injuries Diaphragm o Trunk level Upper trunk Suprascapular nerve o Infraspinatus and supraspinatus o Common sites of compression at the suprascapular notch which affects both muscles. o Spinoglenoid notch only affects infraspinatus o Division level has no branches o Cord level Lateral cord Lateral pectoral n. o Clavicular part of pec major Posterior cord Upper subscapular o Upper portion of subscapularis Thoracodorsal o Lats, Lower subscapular o Lower portion of subscapularis and teres major Medial cord (one motor and two sensory branches) Medial pectoral n. o Pec minor muscle o Sternocostal part of pec major Medial brachial (sensory) Medial antebrachial cutaneous (sensory) o Brachial plexus injuries Trauma, infection, entrapment Most common cause is traction o pulling the extremity, forcible head rotation from the shoulder, direct depression of the shoulder girdle o causes nerve to stretch beyond physiological limits o can cause temporary disruption or functional discontinuity of the nerve. o Upper plexus is taut when arm is dangling at the side Susceptible to injuries that increase distance between head and neck o Lower plexus is taut when arm is abducted and elevated Excessive arm abduction elevates the “coracoid pulley” and places tension across the cords of the brachial plexus. Infection is uncommon cause Brachila neuritis, neuralgic amyotrphy, parsonage-turner syndrome o Acute onset of intense pain about shoulder girdle without trauma o Weakness of muscles innervated by the affected nerves develops after p! subsides o Upper plexus is most commonly involved. Specifically the suprascapular and long thoracic nerves o EMG abnormalities are only apparent 3-4 wks after initial p! response. Positive sharp waves and fibrillation potentials indicate acute denervation Upper brachial plexus (Erb-Duchenne) o C5-C6 o Primary deficit: shoulder abduction, ER, elbow flexion Extended upper brachial plexus o C6-C7 o Primary deficit: above plus elbow and digital extension Lower brachial plexus (Dejerine-Klumpke) o C8-T1 o Hand intrinsic muscles, finger flexors Total brachial plexus lesion o C5-C8 +T1, entire plexus Seddon’s classification of nerve injury Neuropraxia: interruption of nerve conduction; some segmental demyelination; axon continuity intact, reversible Axonotmesis: axon continuity disrupted, neural tube intact; Wallerian degeneration distal to lesion Neurotmesis: complete disruption of nerve continuity; loss of axons and neural tube; no spontaneous recovery; sx required. o Transection is classic example of this but severe traction or contusion can produce similar injury with irreversible intraneurral scarring. Sometimes a brachial plexus can be a combined lesion with elements of all three. Diagnosis and Classification of brachial plexus injuries. Severe pain in an anesthetic extremity suggests deafferentiation and avulsion injuries. Adult brachial plexus injuries are often not evaluated in an acute setting, they are secondary to life-threatening injuries In sharp penetrating trauma (i.e. stabbing) the timing of neuro deficit is important. o Instantaneous deficit implies nerve laceration o Delayed onset indicates compressive neuropathy by an expanding hematoma or false aneurysm. Make sure to look at the limb’s posture Check sensation using Weinstein’s monofilaments Careful examination to find lesion level o Suggest avulsion: Dorsal rami – paraspinal muscles Dorsal scapular – rhomboids and levator scap Long thoracic Horner’s syndrome, drooped eyelid, constricted pupil, sunken globe, sweating deficit along the affected side of face usually implies avulsion of C8-T1 o Percussion of supraclavicular and infraclavicular plexus (+) Tinel sign indicates postganglionic lesion Tinel sign absent if link to spinal cord is disrupted in avulsion/pre-ganglionic injury. o Post-ganglionic lesions are further localized. Status of suprascapular nerve Thoracodorsal Upper and lower subscapular nerves Medial and lateral pectoral Pec major is REALLY helpful due to dual innervation from lateral and medial pectoral nerves from the lateral and medial cords. Also selective atrophy of the clavicular or sternocostal heads facilitate diagnosis. Complete atrophy implies global injury. Physical exam o Upper trunk (C5-C6) Shoulder (rotator cuff, deltoid), forearm supination (biceps, supinator), elbow flexion (biceps, brachialis), wrist extension (ECRL), median nerve sensibility of thumb and index finger Middle trunk (C7): elbow extension (triceps), forearm pronation (PT), wrist ext (ECRB), digital extension (MCP joints), digital flexion (FDS), wrist flexion (FCR), medial nerve sensibility long Lower trunk C8-T1: forearm pronation (PQ), extrinsic finger and thumb flexors (FPL, FDP), intrinsic muscle wrist flexion (FCU), ulnar nerve sensibility. Electrodiagnostic studies EMG o Records electrical activity of muscle fiber at rest and during activity o Normal muscle is silent at rest and active during contraction with progressive recruitment of motor units o Denervated muscle will exhibit spontaneous electrical discharge (fibrillations and + sharp waves) Not present until 2-4 weeks after denervation. o A reinnervated muscle will begin to show reinnervation or nascent potentials (polyphasic, low amplitude recordings) o Importantly this stuff shows on EMG before clinical signs that the muscle is coming back!! o EMG evaluation to assess level of brachial plexus injury Fibrillations and sharp waves of paraspinal muscles implies avulsion Or of serratus anterior If normal signal preserved suggests more distal lesion o Neuropraxia can be differentiated by absence of fibrillation potentials and + sharp waves o Axonotmesis or neurotmesis will both show fibrillation and + sharp waves 2-4 weeks later. o Serial EMG evals can infer axonotmesis by the spontaneous return of nascent units or reinnervation potentials that preceded clinical signs of recovery. o Neuotmesis will not show these signs of recovery. Nerve conduction velocity o Integrity of peripheral nerve o Motor or sensory latency can be measured using Compound motor action potential (CMAP) Or sensory nerve action potential (SNAP) o A severed nerve will lose its capability to conduct a sensory or motor AP distal to lesion as the nerve degenerates…but distal segment might be able to conduct for several days after injury prior to degeneration Early measurement of conduction velocity can produce false-positive reading for nerve continuity. Usually delay for 3 weeks to allow for loss of conduction and denervation changes in muscle o SNAP and corresponding sensory nerve conduction velocity is helpful in differentiating preganglionic avulsion injuries from post-ganglionic lesions Presence of normal sensory conduction velocity in an anesthetic part of the arm indicates pre-ganglionic injury because the nerve is not separated from its cell body in the dorsal root ganglion. However, the sensory nerve is separated from the spinal cord and sensation cannot be processes within the CNS o CMAP of motor nerve conduction velocity is absent in both pre and postganglionic injuries and is not a distinguishing factor (think cell body is IN the spinal cord) Somatosensory-evoked potentials (SEPs) o SEPs and MEP (motor evoked potential) are commonly used during surgery. o Can be employed to assess conduction across the brachial plexus to define irreparable nerve root avulsions o Absence of MEPs or SEPs recorded over spinal cord suggest ventral root and dorsal root avulsions respectively and are contraindicated for sx. Nerve action potentials (NAPs)