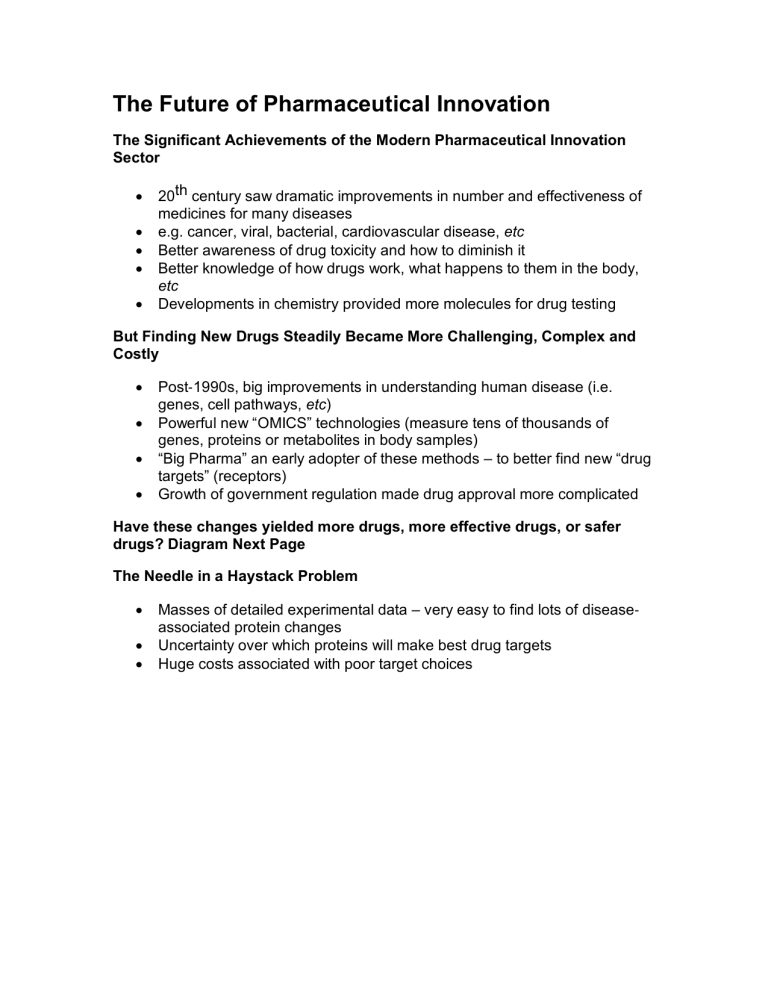
The Future of Pharmaceutical Innovation The Significant Achievements of the Modern Pharmaceutical Innovation Sector • • • • • 20th century saw dramatic improvements in number and effectiveness of medicines for many diseases e.g. cancer, viral, bacterial, cardiovascular disease, etc Better awareness of drug toxicity and how to diminish it Better knowledge of how drugs work, what happens to them in the body, etc Developments in chemistry provided more molecules for drug testing But Finding New Drugs Steadily Became More Challenging, Complex and Costly • • • • Post‐1990s, big improvements in understanding human disease (i.e. genes, cell pathways, etc) Powerful new “OMICS” technologies (measure tens of thousands of genes, proteins or metabolites in body samples) “Big Pharma” an early adopter of these methods – to better find new “drug targets” (receptors) Growth of government regulation made drug approval more complicated Have these changes yielded more drugs, more effective drugs, or safer drugs? Diagram Next Page The Needle in a Haystack Problem • • • Masses of detailed experimental data – very easy to find lots of disease‐ associated protein changes Uncertainty over which proteins will make best drug targets Huge costs associated with poor target choices Is There a Productivity Crisis in Pharmaceutical Innovation? Long‐term R&D Trends in the Industry • Eroom’s Law- The number of new drugs approved by the US‐FDA per billion US dollars (inflation‐ adjusted) spent on research and development (R&D) has halved roughly every 9 years. R&D Expenditure by Big Pharma in USA The Drug Development Phase of Pharmaceutical Innovation (“Human Testing”) has Gotten Expensive Most Classic Drugs Covered in PHAR1101 are “Small Molecules” (Absorbed from GI‐tract) • • • • Aspirin- MW = 180 g/mol Chlorpromazine- MW = 319 g/mol Ibuprofen- MW = 206 g/mo Modern Therapies can be Enormous What is a Drug ? Older versus Newer Concepts Some Examples of Biopharmaceuticals Produced by the Biotechnology Industry (1990s & Beyond) • Therapeutic Proteins • Growth factors & cytokines • Haemopoietic factors (stimulate white blood cell growth after chemotherapy) • Erythropoietin (EPO, stimulates red blood cell growth) • Hormones (e.g. insulin, human growth hormone, etc) • Coagulation factors & antithrombotic factors • Therapeutic Antibodies (e.g. Remicade) • Antisense Nucleic Acids (e.g. Fomiversen) Areas of Medicine Where “Biologics” Have Had a Key Impact in the Past 20 Years • • • • Hormone deficiencies “Blood tumours” Autoimmune diseases Solid tumours Two Classic Problems with Protein‐Based Drugs Options for Administering Large Molecule Drugs • • • • Oral Route – not very effective (proteins broken down by proteases in GI‐ tract) Lung Route – quite effective if proteins delivered deep as micron‐sized particles Nasal Route – reasonably effective for some proteins, but often low absorption Skin Route – may work if skin barrier transiently disrupted (sonic energy, electric current) An Example of a Pioneering Modern Biopharmaceutical: Infliximab (“Remicade”) • • • Approved by US‐FDA in 1998 Belongs to “TNF Inhibitor” class of Anti‐inflammatories (many now) A therapeutic antibody that neutralises role of tumour necrosis factor‐α (TNF) • • Developed by Drs Jan Vilcek and Junming Le (NY University) Changed the treatment of RA Sales ≈US$5 billion/p.a. Rheumatoid Arthritis (RA) • A serious and disabling “autoimmune” disease (affects ≈1% of population) • 2-3 × more common in women • Painful inflammation and swelling in joints (e.g. hands, knees, feet, etc) • Involves “self-reacting” antibodies, loss of cartilage and bone, destroyed joints • Morning stiffness & fatigue • Probably caused by imbalance between pro- & anti-inflammatory T-cells (immune cells made in thymus gland) • Patients often die from infections, heart disease, strokes, etc Role of TNF‐α in RA Inflammation • • • TNF- is a powerful molecule made in body by immune cells (a “cytokine” - mainly made by macrophages) o TNF has strong tissue damaging properties High TNF levels occur in synovial fluid in RA joints o Causes permanent cartilage damage and bone loss Blocking its effects with antibodies can slow RA progression The Development of Infliximab • • • • 1933, Jan-Vilcek born in Slovakia o Received M.D. and PhD o 1964, defected to USA Worked at NYU School of Medicine Developed interest in cytokines 1989 with Junming Le, created a monoclonal antibody against TNFo Collaborated with the biotechnology company Centocor (now Janssen) o Led to first anti-TNF drug Remicade How TNF Inhibitors Suppress Inflammatory Joint Damage... How Infliximab is Used Clinically • • • Given via intravenous infusions (“IV”) over 2 hr period o Repeat at 2 and 6 weeks, then every 8 weeks Doses increased if response suboptimal after 12 weeks o Very effective in rheumatoid arthritis (usually combined with methotrexate) Also used against other chronic inflammatory disorders E.g. Crohn’s disease, ulcerative colitis, psoriasis, ect Problems with Infliximab 1) Potential for Toxic Effects: • E.g. unpleasant allergy symptoms during infusion (vary in severity) • • Risk of liver damage (rare) Makes some diseases worse (e.g. MS) 2) Reduced Ability to Fight Infections • • Activation of “dormant” tuberculosis Nasty fungal infections 3) It is Expensive • • >$20K per year per RA patient (US) Social access concerns Other Immunomod ulatory Biopharmaceuticals • • • • • There are now many “TNF Inhibitors” available for use Significant successes in many patients All must be given by injection All face similar problems with allergies, TB, cost, etc Challenge for the Future: Can we make cheaper, small molecular weight TNF blockers? Conclusion • • • The pharmaceutical industry is in a prolonged state of flux o More success in making large protein‐ based drugs than traditional small, orally‐administered drugs What sort of drugs will be made in future decades remains unknown Still lots of ongoing health challenges needing drug innovation! o Latest trend sees small molecules being made after the success of protein‐based therapies is proven