Gastric Sleeve: Patient Case Study & Procedure Overview
advertisement
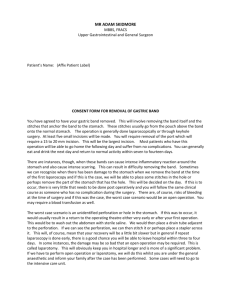
GASTRIC SLEEVE INITIAL CONSULT IN OFFICE (11/19/18) • 50 Year old female pt. presents for bariatric consult and a history of GERD referred by her PCP. Mrs. T states she has been struggling with weight loss since age 18. She states she has tried the cabbage soup diet, Nutrisystem, Weight Watchers, Sum Fast, HCG, Lean Cuisine and the most she could lose was 50 pounds. She states her highest weight she was 260 pounds. Today Mrs. T is 240.2 pounds with a BMI of 37.6. Pt. Denies binge eating, night eating or overeating. Factors she states contributes to weight gain are pregnancy and lack of activity. Pt. has a history of fatigue, difficultly sleeping and back pain that she attributes to weight gain. • Mrs. T states the onset of her heartburn was gradual and not changing. Pt. states there is a burning sensation in her chest but no radiation. Pt. States symptoms are constant and aggravated by eating. Pt. states nothing helps to relieving the reflux. Pt. Denies chronic cough, dental erosions, dysphagia, hoarseness, melena or vomiting. IN OFFICE HISTORY • PMH - GERD, Anxiety, Insomnia • PSH- 2 abdominoplasty C-sections 1987 & 1989, Tubal ligation with hysterectomy, Cholecystectomy 2008 • Family Hx- None provided • Social Hx- Married, unemployed, Smokes a vape pen for 2 years, Drinks 1-2 drinks per week, Denies illegal drug use • Meds- Lexapro10mg 1 tab daily, Trazadone 50mg tab as needed • Allergies- NKDA ROS-IN OFFICE (11/19/18) • Resp: Denies aspiration, stridor and wheezing • Cardio: Denies claudication, edema and palpitations • GI: Denies constipation, change in stool pattern, diarrhea, decreased appetite • GU: Denies Dribbling, dysuria, hematuria, urinary frequency, urinary incontinence and urinary retention • Endocrine: Denies cold intolerance, heat intolerance, polydipsia and polyphagia • Neruo: (+) headaches, Denies dizziness, memory impairment, numbness in extremities • Psych: (+) anxiety • MS: (+) joint pain • Heme/Lymph: Denies easy bleeding and lymphadenopathy PHYSICAL EXAM- IN OFFICE (11/19/18) • Vitals: BP 127/81, Pulse 86, Height 5’7”, Weight 240.2, BMI 37.6 • Gen: Obese female, alert and appropriate, No acute distress • Back/Spine: No kyphosis • Heart: RRR, no murmurs, rubs gallops • Lungs: CTA AF, no wheezes, rales, or rhonchi • Vascular: No Carotid bruits, normal doornails peds, capillary refill less than 2 seconds, no varicosities • Ab: obese, abdomen soft, nontender, nondistented, no hepatic enlargement, no splenic enlargement, no femoral or ventral hernias, no Murphy’s sign PHYSICAL EXAM CONT. • Skin: Warm and dry, no pallor • Head/Neck: No JVD, No Thyromegaly, • Eyes: PERRLA, no scleral icterus • Ears: TMs pearly grey, cone of light present • Nose: symmetrical, nares patent, non- erythematous, no septal deviation • Mouth/Throat: normal dentition and gums, no lesions, pink mucosa, no tonsil enlargement • MS: normal gait, no muscle atrophy • Neuro: CNs II-XII present B/L, DTRs +2/4, normal sensation • Psysh: appropriate mood, cooperative SURGICAL ASSESSMENT AND PLAN • Assessment: Unspecified abdominal pain and Morbid Obesity • Plan: Mrs. T meets the NIH guidelines for bariatric surgery. She has clinical risks of obesity including, back pain, suspected sleep apnea and suspected depression. Discussed the different bariatric procedures including lap band, gastric bypass and the sleeve as well as the risks and benefits of each procedure. Discussed risks in surgery including but not limited to: Bleeding, infection, bowel injury and need for open operation. Discussed possible hiatal hernia repair if one is identified on EGD . Pt. is asked to follow up after her EGD for repeat evaluation. The pt. expressed complete understanding, was agreeable to this plan, and will follow up as discussed. • Plan Orders: Avoid citrus, alcohol, coffee, chocolate, mints, eat smaller meals, no eating three hours prior to bedtime and elevate head prior to sleep. EDG WITH BIOPSY ( 12/11/12) • No gastric ulcerations or masses. Retroflexion view shows hiatal hernia. The distal antrum shows flattening of the rugal folds distally and some streaky erythema, no ulcerations. Duodenum showed no ulcerations. The distal third of the esophagus shows erythema consistent with reflux esophagitis.The rest of the esophagus appeared normal. FOLLOW-UP ( 12/12/18) • Mrs. T is presenting today for preoperative check. An EGD done 12/11/18 show hiatal hernia. Pathology is pending. Pt. has been following her diet and has lost 7 pounds since her initial visit, 240.2 to 233 pounds. Pt. has been given pre-and post-op diet instructions. Given the pt. symptomatic presentation, plan for laparoscopic hiatal hernia repair and partial gastrectomy. Discussed in detail all the risks, benefits and alternatives. Pt. understands and wishes to proceed with the operation. • Pre-operative and post-operative prescriptions were offered to minimize or alleviate the patient’s post-operative discomfort. Pt. has been asked to review the pre- and postop intrusions and contact the office with any questions. The pt. expressed complete understanding and agreed to do so. • Pt. scheduled for surgery 01/01/19 - to go home same day pending no complications PRE-OP LABS • EKG: Normal sinus rhythm • Rate 76 BPM • PR internal 142 ms • QRS duration 97 ms • QT/QTc 412/443 ms PRE-OP LABS • U/A • Specific Gravity -1.016 • pH -6.0 • Urine-Color -Yellow • Appearance -Clear • WBC Esterase/Protein/Glucose/Ketones/Occult blood/Bilirubin -Negative • Nitrate -Negative • Microscopic • WBC/RBC/Epithelial cells- None • Bacteria- few PRE-OP LABS BMP CBC 13.1 4.5 142 106 14 179 38.4 106 4.1 PT 10.8 PTT 28 INR 1.0 23 0.50 SURGICAL PROCEDURE • Needle is placed left to the umbilicus and abdomen insufflated to 15mmHg. Pt. placed supine and in Trendelenberg once ports are placed. Several ports are placed in several locations depending on the size and pannus of the patient. • Mobilization of the fundus, antrum and cardia with the energy device. The stomach is inspected and the blood vessels to the lateral side of the stomach are divided. • A bougies is inserted into the stomach and serves as a sizer for the new stomach. http://surgery.ucla.edu/bariatrics-gastric-sleeve SURGICAL PROCEDURE • The hiatal hernia defect was closed with interrupted suture intracorporeally. • The greater curvature of the stomach was amputated using successful firing of a stapling device. It was reinforced with individual clips and sealant. • The distal stomach was then occluded and proximal stomach was filled with 60 mL of methylene blue placing the proximal staple line under tension. There was no evidence of extravasation of the methylene blue and the closure appeared completely satisfactory. • The greater curvature of the stomach was in a bag and removed through the 15-mm port site. • Abdomen was deflated, all ports removed and all skin incision were closed. http://surgery.ucla.edu/bariatrics-gastric-sleeve BENEFITS OF THE GASTRIC SLEEVE • Removal of part of the stomach reduces stomach volume, causing people to feel fuller much quicker. Thus reducing intake of calories. There are also hormonal changes because there is reduced secretion of hunger hormones such as ghrelin. Food can pass the stomach to the intestine quicker which increases stomach motility. • People lose about 60-70% of their excess body weight. The success rate for the gastric sleeve is 80-90%. • Resolution or improvement of obesity related health problems such as: Diabetes type 2, hypertension, fatty liver disease, high cholesterol, sleep apnea, joint pain, depression, PCOS and gout. • Surgery offered to patients with a BMI greater than 40 kg/m2, or greater than 35 kg/m2 with serious comorbidities. WEIGHT LOSS PROGRESSION • 2 weeks- 10-20 pounds; one pound a day • 3 months- 35-45% weight loss • 6 months- 50-60% weight loss • First Year- 60-705 weight loss COMPLICATIONS AND RISKS • A staple line leak from where the part stomach was removed • Bleeding, blot clot • Nutrient or vitamin deficiency • GERD • Weight regain due to the stomach being overstretched thus increased volume intake allowed again • Excess skin ADVANTAGE OF GASTRIC SLEEVE VS. GASTRIC BYPASS • Simpler surgery, gastric sleeve takes 40-70mins while gastric bypass takes 2-3 hours. • No mal-absorption • More likely to develop complications such as bowel obstruction, marginal ulcer, and internal hernias with bypass. DISCUSSION QUESTIONS • What psychological effects does the gastric sleeve have on the patient in the long run? • What percent of people who have the gastric sleeve procedure return back to their pre-op weight? RESOURCES Cummings, David E and Ricardo V Cohen. “Beyond BMI: the need for new guidelines governing the use of bariatric and metabolic surgery” lancet. Diabetes & endocrinology vol. 2,2 (2014): 175-81. Dr. Shawn Stevenson. General Surgeon. Agave Surgery. “Gastric Sleeve.” Bariatrics, surgery.ucla.edu/bariatricsgasrtic-sleeve.