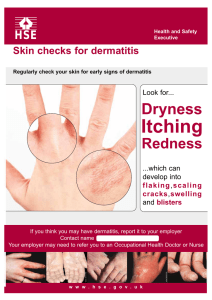
REVIEW SUM LAM DERM o o o o o o o o o o o o o o Lichenification – repeated rubbing of the skin makes it thick Pruritus reaction treated with antihistamine cream and if it's a large area you give a systemic CS Most common type of skin reaction = erythematous reaction o Stop abx and the drug goes away – exanthematic erythematous Angioedema = ACEI o More likely to be involved in the mouth, eyes, eyelid, tongue, uvula o Uvula caused by captopril / ramipril Fixed drug reaction – TARGET o Occurs at the same site, same size, and caused by medication ONLY and usually a specific type DRESS – allopurinol and abacavir o Eosinophil is elevated o Drug hypersensitivity syndrome is another term for DRESS o You see eosinophil inc AND you have to have a systemic presentation as well Contact Dermatitis o Nickel from the watch o Caine products o Rosin (the ankle strap rubber) o Neomycin o Allergic to PEG o Anything is possible- it doesn't have to be the active ingredient it can be the inactive ingredient o If they are allergic to something topically you cannot give it systemically TENS = most severe!! o Body surface area > 30% Blisters – SJS/TENS o Contact dermatitis can have blisters too o Fixed drug reactions can have blisters too o Small blisters = vesicles o Large blisters = bullae Type of drug you can do screening for o CBZ o Allopurinol o Abacavir o If you have the copy you have to avoid!! o If the patient has 2 copies = EVEN WORSE – AVOID!! One copy is bad two copies is really bad Hyperpigmentation o Quinidine o Minocycline o Amiodarone o Phenothiazine – for the treatment of anit-psychotic o Adrimycin o Bleomycin – flagellated – not painful just hyperpigmentation How can you tell its contact dermatitis – it mimics the object in which the patient is in contact with TENS Tx o Supportive care o Pain care o IV fluids o IV IG o Mucosal membrane – pulmonary doctor, eye doctor o Types of drug good for mucositis – magic mouthwash, peridex, lidocaine o If someone confirmed with TENS and SJS – AVOID sulfur based drug – silver sulfasalazine Erythema Nodous o Knees and Shins – lower extremities o Tender upon touch o Nodules o o o o o o Drugs that can cause this – ORAL CONTRACEPTIVE INC PHOTOSENSITIVITY o Stay away from the sun o Apply sun screen o Protective clothing o Sunglasses o Can have hypersensitivity of the eyes and the tongue Acne Form o OC o Testosterone o EGFR inhibitors o Treatment of Acne Form – treat is as acne o If its happening in the back and not seeing/cosmetic you can just ignore it and just have good hygiene practice and don't have to treat Initial presentation of Angioedema in patients that have urticaria so you have to monitor them that the hives don't become worse o If the hives become worse it can be angioedema o Swelling and itching – may need some sort of antihistamine on board Drug Hypersensitivity Syndrome o CBZ o Worry for cross reactivity and CBZ is cross reactive with VPA and phenobarbital Photoallergic is more severe o Anytime you see the immune system involved – it is more severe HEMATOLOGIC o Thromboemobolism o OC/HRT – stop 4 weeks prior and start again 2 weeks after o Raloxifene – stop 72 hours prior to sx and resume after becoming mobile o Chemotherapy induced anemia – Darbo/EPO- monitor the H/H HB - Make sure it doesn't go above 12 Does not rise more than 1 in 2 weeks o Thrombocytopenia o Chemo Agents o Heparin – emboli in toes- monitor for thrombosis HITT!! Decrease platelet count but you worry about thrombosis o HAT = anticipated – not life threatening and due to platelet aggregation effect o Anemia o MACROcylic give b12 and folic acid Chronic use metformin HIV drug - Zidovudine o MICROcylic – iron supplementation o Agranulocytosis o Clozapine BEN pts > 1000 Regular general patients >1500 o Definition of medical emergency for neutropenic fever o LEVAQUIN!!!!! o If the patient is allergic to b-lactam give them monobactam aztrenenum o High risk MRSA add on Vance or linezolid o Antifungal therapy for patients that are more than 96 hours and still have fever